Episcleral brachytherapy as an effective alternative in vasoproliferative tumors
Marta Para Prieto, Maria Antonia Saornil, Jesús María de Frutos Baraja, Ciro García Álvarez,Patricia Diezhandino García, Francisco López Lara
Intraocular Tumors Unit, Ophthalmology & Radiotherapy departments, Hospital Clínico Universitario, Valladolid 47005,Spain
Abstract● The aim of this study is to assess the results of episcleral brachytherapy as treatment of retinal vasoproliferative tumors (RVTs) in a referral lntraocular Tumors Unit (lTU).A retrospective review of all patients diagnosed with vasoproliferative tumors of the retina and treated with episcleral brachytherapy in the lTU, University Hospital of Valladolid between 2009 and 2015 was done. Five patients accomplished the inclusion criteria. All of them presented associated exudation and secondary retinal detachments(RD). Four patients had received prior treatments.Decreased tumor size and exudation regression was found in all cases after treatment. Visual acuity remained stable or increased in all patients. No recurrences have been found after twelve-months follow up. The results of the present study suggest that episcleral brachytherapy is an efficient and safe option in the management of vasoproliferative tumors, especially when large tumor or extensive subretinal fluid is present. ln these cases episcleral brachytherapy could be considered as a first line treatment.
INTRODUCTION
Retinal vasoproliferative tumors (RVTs) are uncommon vascular masses firstly named “presumed acquired retinal hemangiomas”, to differentiate them from capillary hemangiomas. They are most frequent in middle-aged people and clinically appears as a solitary yellow-red-pink mass, with ill-defined borders in the retinal periphery, being the inferotemporal quadrant the most commonly involved[1]. Study of lesions obtained by endoresection or from enucleated eyes suggests a benign and reactive nature rather than neoplastic,composed of glial cells and blood vessels, but the exact origin of these tumors remains controversial[2-3]. RVTs can be primary (idiopathic) or secondary to other ocular diseases such as retinitis pigmentosa, previous surgery, uveitis or other ocular in flammations. These tumors used to produce massive intraretinal and subretinal exudation, detachment, which may be extensive and occurs in over than 80% of cases leading to a severe visual loss[4]. Other common complaints are floaters,photopsias and metamorphopsias.
There is no standard approach to the management. Different type of treatments can be used to cease or to reduce the retinal exudation for these patients. Observation is an option in asymptomatic patients with small tumors and limited exudation; other alternatives are used in symptomatic patients or with visual acuity (VA) risk (growing tumor or progressive exudation). Therapeutic options successfully employed include: intravitreal anti-vascular endothelial growth factor(VEGF), cryotherapy, laser photocoagulation, photodynamic therapy, surgery (resection or vitreoretinal surgery) or intravitreal dexametasone implant[5-7], but recurrences are common and collateral effects of multiple treatments can worsen vision loss. One alternative is plaque brachytherapy,and some authors recommend it especially in tumors thicker than 2.5 mm as an initial treatment[4-5,8-10].
The purpose of this study was to report the results of episcleral brachytherapy as treatment of RVTs in a Referral Intraocular Tumor Centre and compare with other treatments regarding regression of tumor, retinal exudation detachment visual function and recurrences.
SBUJECTS AND METHODS
A retrospective review of the Intraocular Tumors Unit (ITU)database was performed from 2009 to 2015. Ethical Approval an informed consent was done. Inclusion criteria were patients diagnosed of RVT, treated with episcleral brachytherapy with at least 12mo of follow up.
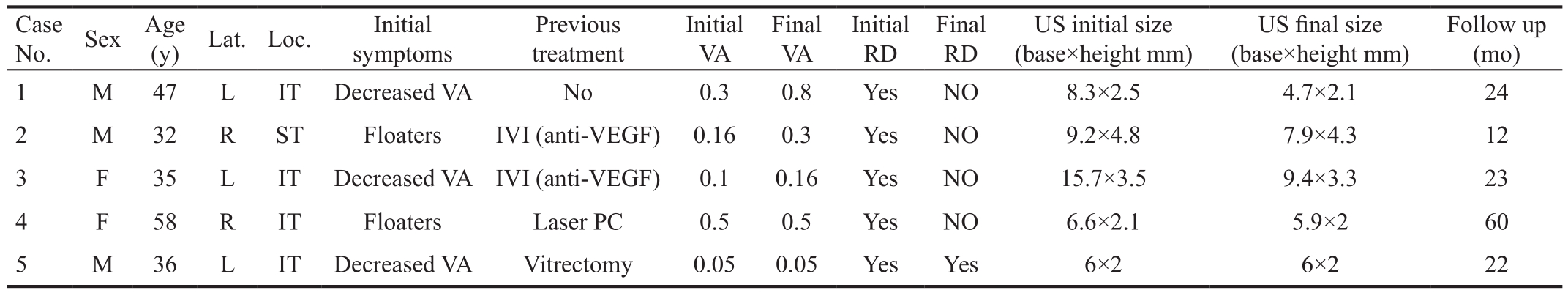
Table 1 Preoperative and postoperative patients and tumors characteristics
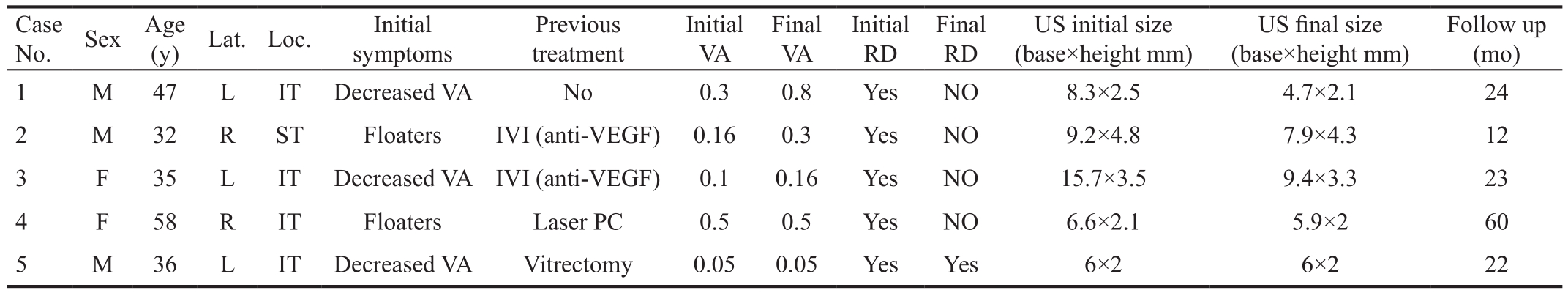
M: Male; F: Female; L: Left; R: Right; Lat.: Laterality; Loc.: Location; IT: Inferotemporal; ST: Superotemporal; VA: Visual acuity; IVI:Intravitreal injection; VEGF: Vascular endothelial growth factor; Laser PC: Laser photocoagulation; US: Ultrasound; RD: Retinal detachment.
Follow up(mo)1 M 47 L IT Decreased VA No 0.3 0.8 Yes NO 8.3×2.5 4.7×2.1 24 2 M 32 R ST Floaters IVI (anti-VEGF) 0.16 0.3 Yes NO 9.2×4.8 7.9×4.3 12 3 F 35 L IT Decreased VA IVI (anti-VEGF) 0.1 0.16 Yes NO 15.7×3.5 9.4×3.3 23 4 F 58 R IT Floaters Laser PC 0.5 0.5 Yes NO 6.6×2.1 5.9×2 60 5 M 36 L IT Decreased VA Vitrectomy 0.05 0.05 Yes Yes 6×2 6×2 22 Case No. Sex Age(y) Lat.Loc. Initial symptoms Previous treatment Initial VA Final VA Initial RD Final RD US initial size(base×height mm)US final size(base×height mm)
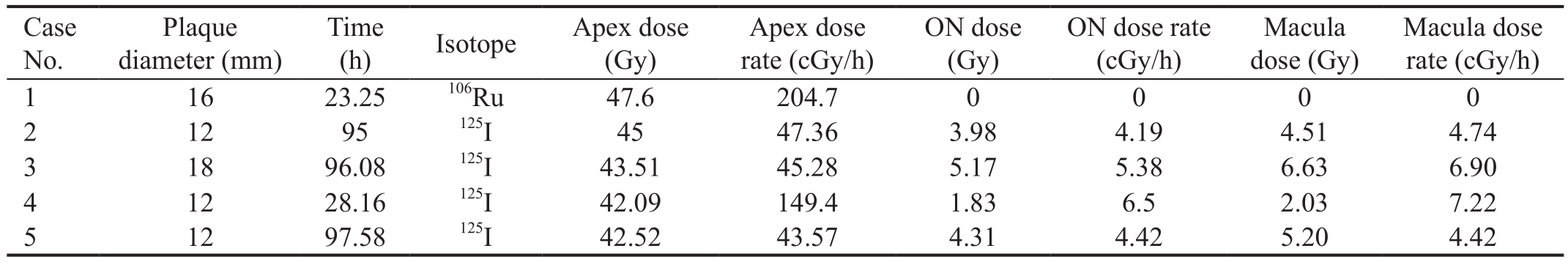
Table 2 Brachytherapy characteristics
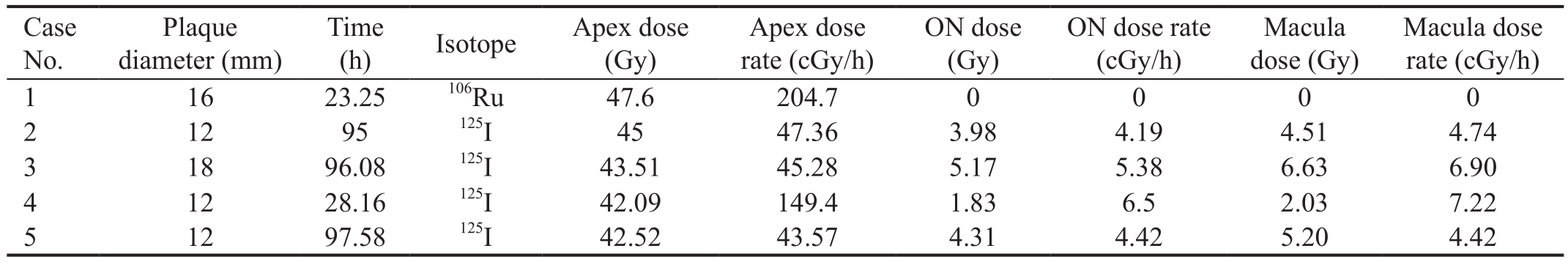
Gy: Gray; cGy/h: Centigray/hour; ON: Optic nerve.
Case No.Macula dose rate (cGy/h)1 16 23.25106Ru 47.6 204.7 0 0 0 0 2 12 95125I 45 47.36 3.98 4.19 4.51 4.74 3 18 96.08125I 43.51 45.28 5.17 5.38 6.63 6.90 4 12 28.16125I 42.09 149.4 1.83 6.5 2.03 7.22 5 12 97.58125I 42.52 43.57 4.31 4.42 5.20 4.42 Plaque diameter (mm)Time(h) Isotope Apex dose(Gy)Apex dose rate (cGy/h)ON dose(Gy)ON dose rate(cGy/h)Macula dose (Gy)
All patients underwent a complete ophthalmologic examination at their first visit, including VA, biomicroscopy of the anterior segment, intraocular pressure measurement, indirect ophthalmoscopy [exudation, retinal detachment (RD)],ultrasonography (measurement of tumor) and angiography.Treatment was decided in those patients with visual impairment caused by the progressive exudation of the tumor or extensive RD.
Dosimetry was performed in all the patients using the Bebig Plaque Simulator 5.37 Software and the Excel Spreadsheet Software with TG 43 parameters[11-12]. The planification was performed using the main measures (longitudinal,circumferential and apical diameters of the tumor), the exact location and distance from the mass to the optic disc and fovea.The calculated apex dose was 45 Gy. Episcleral brachytherapy was administered with125I (COMS plaques loaded with IsoSeed®I25.S16, both Eckert & Ziegler BEBIG, Germany)or106Ru plaques (Ru-106 Eye Applicators, Eckert & Ziegler BEBIG, Germany), with diameters between 12 to 18 mm and always with at least 2 mm of safety margin.
Fixation and removal of the plaques was done under general anesthesia and the location of the tumor was previously marked using scleral transillumination and indirect binocular ophthalmoscopy. Follow up was performed at one, three and every six months up to the third year and yearly thereafter.All the examinations were done by the same ophthalmologists and the following baseline parameters were assessed: sex, age,laterality and location of the lesion, initial symptoms, previous treatments, initial and final VA (specified in decimal form),initial and final RD, and initial and final size of the tumor.Regarding plaque diameter, time of brachytherapy, isotope,apex dose and rate, optic nerve (ON) dose and rate, and macula dose and rate were registered.
RESULTS
Among a total of 861 intraocular tumor patients, 38 were vascular origin and 9 RVTs (1%). Four patients were asymptomatic and underwent observation. Five patients met the inclusion criteria for the study and were treated with episcleral brachytherapy. Table 1 shows patients and tumor main characteristics.
Three patients (60%) were male and two female (40%). Median age at the time of diagnosis was 36 (mean 41, range 32-47). Two(40%) appeared in the right eye and three on the left (60%).
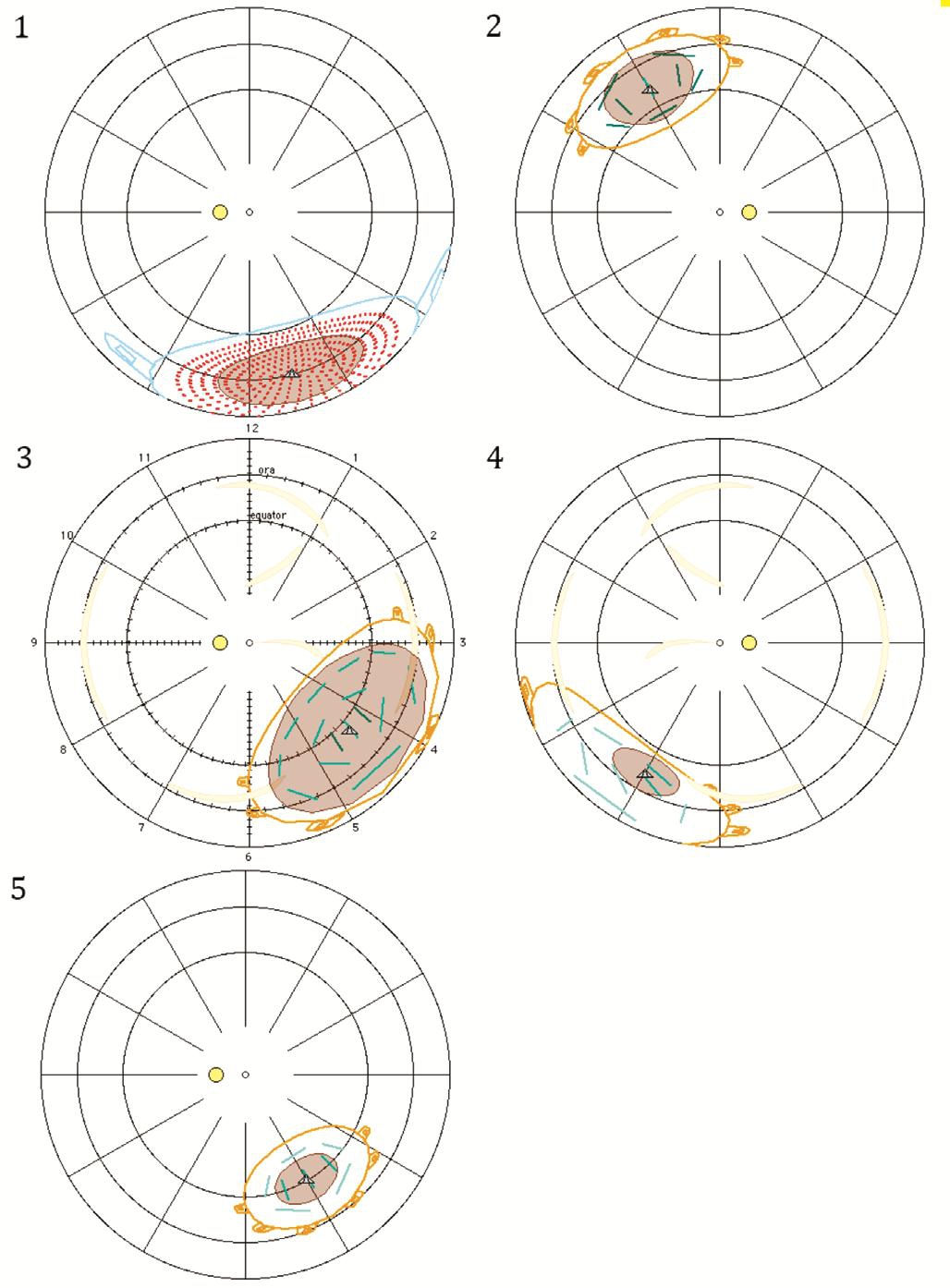
The tumor was located in peripheral temporal retina in all of them; one (20%) supero-temporal and the other four (80%)infero-temporal (Figure 1).
All of them presented visual symptoms at the moment of diagnosis: three (60%) decreased VA and two (40%) floaters.Four patients (80%) were previously treated with other alternatives: two with anti-VEGF intravitreal injections(IVIs; cases 2 and 3, treated with two and three bevacizumab injections respectively), one with laser photocoagulation (case 4)and one with vitrectomy (case 5). Brachytherapy was the first line treatment only in one case (case 1).
Four patients were treated with125I plaque and one of them with106Ru plaque. Figure 1 and Table 2 show main brachytherapy characteristics.
Brachytherapy time ranges from 23.25 to 97.58h and apex dose from 42.09 to 47.6 Gy with a dose rate between 43.57 to 204.7 cGy/h. Mean doses to the ON was 3.82 Gy and 4.59 Gy to the macula.
Median VA before treatment was 0.16 (range 0.05-0.5)improving up to 0.3 after brachytherapy treatment (range 0.05-0.8). All patients presented RD at the time of diagnosis;in cases 1 to 4 disappeared after treatment and in case 5 there was a marked improvement. Median thickness before treatment was 2.5 mm (range 2-4.8) decreasing to 2.1 mm after brachytherapy.
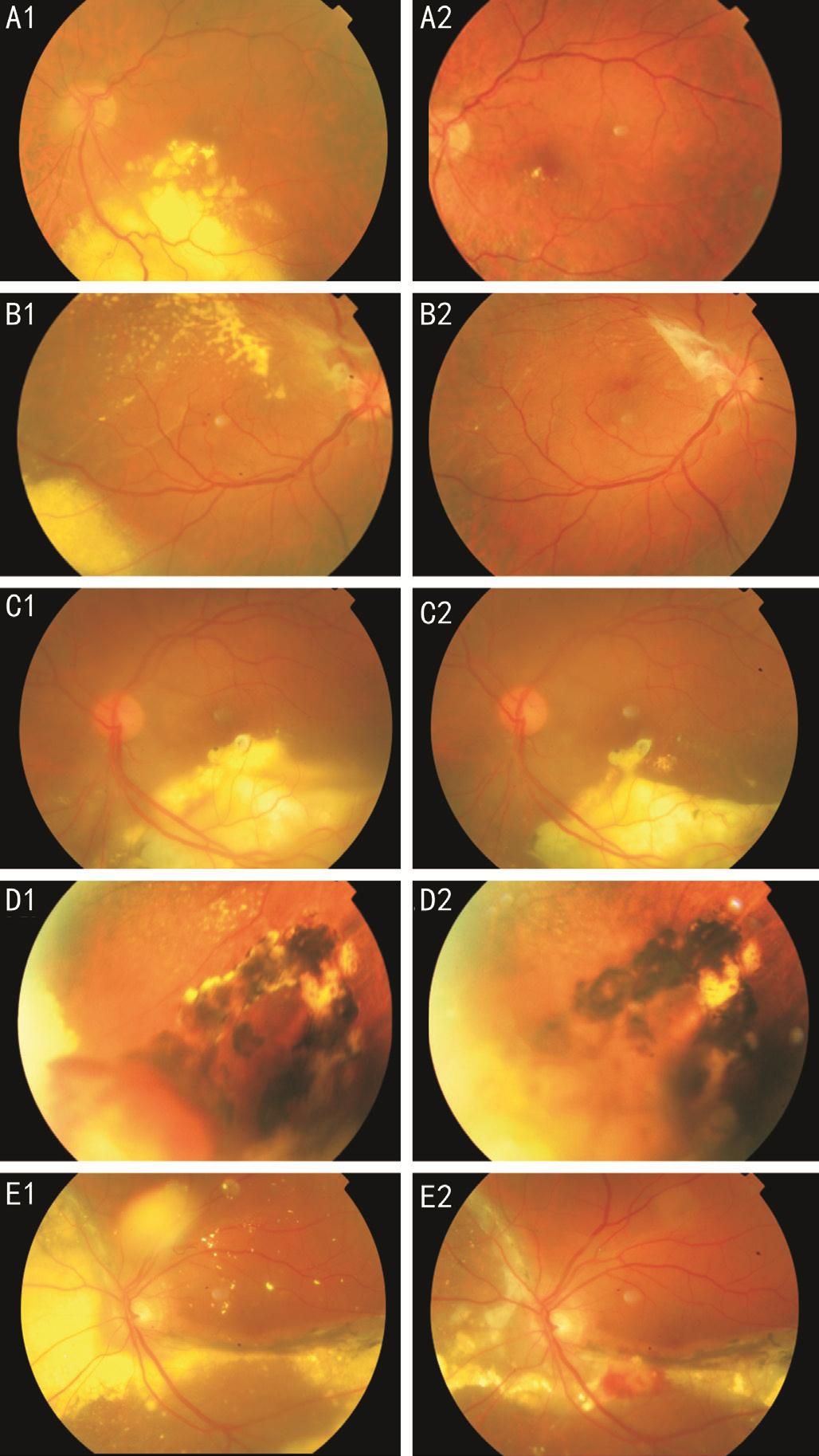
The median follow-up interval was 30mo (range 15-67)and there was no loss of follow-up. Neither progression nor recurrences were observed during this period. Sequelae of long standing disease or prior treatments appear in case 2 (preretinal membrane), 3 (subretinal fibrosis), preventing greater visual improvement. No complications related to radiation therapy appeared in the follow up time with the exception of mild cataract in case 4, no removed by the time of the study. Figure 2 shows the eye fundus of the five patients before and after treatment.
DISCUSSION
The present study shows the rarity of RVTs even in a referential clinic unit representing 1% of intraocular tumors. Other series previously published, agreed on the fact that these tumors are rare,but they didn’t present incidence or prevalence estimations[4,8-9].Shieldset al[4]showed in 2013 the largest series of RVTs,with 334 tumors in 295 eyes of 275 patients in a retrospective review of patients diagnosed in 36y, from 1975 to 2011.
RVTs are a well-recognized entity that can lead to severe visual loss and ocular complications such as exudative RD[13]. Therefore,some authors propose treatment, even in the early stages of the disease[5,13]. The indications of the different modalities in RVTs are not yet well defined and various methods have been reported, including brachytherapy, cryotherapy, surgery,photocoagulation, photodinamic therapy, anti-VEGF IVIs or,most recently, intravitreal dexamethasone implant[5-6,8-9,13].
However, the majority of these treatments have limited effectiveness in causing long-term regression and more than one therapy is required in severe cases. Recurrences are frequently reported thus none of these treatments seems to be definitive for RVTs. The lack of protocol makes many patients receive multiple treatments, developing complications that are possibly caused both by the therapies and the natural history of the tumor, especially fibrosis and gliosis that hinder VA improvement despite good control of exudation and RD associated. In the present study, the case with better evolution and greater visual recovery is the one who not received previous treatment (case 1).
Not many cases treated with plaque radiotherapy have been reported. Heimannet al[5]showed in 2000 a series of 22 eyes with vasoproliferative tumors, 16 of them treated with brachytherapy using106Ru/106Rho and a mean apex dose of 81 Gy. They recommended the use of this type of treatment in tumors larger than 2 mm and they demonstrated the ef ficacy in the tumor regression and the associated telangiectasias,improving or remaining stable the VA in most of the patients.Anastassiouet al[8]reported in 2006 their experience with106Ru plaque in VPTs. They treated 35 patients using106Ru eye applicators and the main applied dose at the apex was 108 Gy.The results were good control of the tumor activity but slight decrease the mean VA after treatment, probably due to a chronic maculopathy related with the brachytherapy dose and the development of epiretinal gliosis. In 2008, Cohenet al[9]reported the ef ficacy of125I treatment in 30 eyes, and reported a tumor regression in 97% of eyes and a signi ficant exudative RD reduction in 91% with a lower apex dose (mean apex radiation of 40 Gy). In this series VA improved or remained stable in 73%.
The present study showed improvement or stabilization of VA in all patients, with regression of tumor size and RD. Two patients (cases 3 and 4) developed macular gliosis, probably related with the natural history of the tumor or previous treatments. Both of them were previously treated with IVIs of bevacizumab. Scleral thickening was observed in one patient(patient 4). We saw the better results in the patient with no previous treatments (patient 1) and treated with106Ru plaque,which is a beta radiation source. This kind of radiation was not used in other patients because of the limited availability in our unit, nevertheless we think that beta radiation could be better to treat VPTs, because of the advantageous steep dose fall-of resulting from the limited range of electrons. The dose distribution allows delivering a suf ficient dose to a very restricted volume while minimizing damage to the healthy structures in the eye[8].
No patients suffered from radiation retinopathy, maculopathy,papillopathy or cataract. A possible explanation was the peripheral location, and the low dose of radiation received by the central retina.
In conclusion, our results support the previous literature and suggest that plaque brachytheraphy, with a low dose of radiation (mean apex dose around 40-45 Gy) should be considered as an efficient and safe alternative in VPTs,especially in large tumors or cases with important RD. We know the limitations of this study, especially the small sample size and the limited follow up, but we propose brachytherapy as a first treatment option in this group of patients, where complications of other previous treatments could get worse final results, and beta radiation in VPTs (106Ru plaques),because of the advantages in protecting healthy structures.
ACKNOWLEDGEMENTS
Foundation:Supported by BEBIG Co.
Conflicts of Interest: Para-Prieto M, None;Saornil MA,None;de Frutos-Baraja JM, None; García Álvarez C,None;Diezhandino García P, None; Lopez-Lara F,None.
REFERENCES
1 Shields CL, Shields JA, Barrett J, De Potter P. Vasoproliferative tumors of the ocular fundus. Classification and clinical manifestations in 103 patients. Arch Ophthalmol1995;113(5):615-623.
2 Irvine F, O’Donnell N, Kemp E, Lee WR. Retinal vasoproliferative tumors: surgical management and histological findings.Arch Ophthalmol2000;118(4):563-569.
3 Poole Perry LJ, Jakobiec FA, Zakka FR, Reichel E, Herwing MC, Perry A, Bratt DJ, Grossniklaus HE. Reactive retinal astrocytic tumors (so-called vasoproliferative tumors): histopathologic, immunohistochemical and genetic studies of four cases.Am J Ophthalmol2013;155(3):593-608.
4 Shields CL, Kaliki S, Al-Dahmash S, Rojanaporn D, Shukla AY, Reilly B, Shiels JA. Retinal vasoproliferative tumors. Comparative clinical features of primary vs secondary tumors in 334 cases.JAMA Ophthalmol2013;131(3):328-334.
5 Heimann H, Bornfeld N, Vij O, Coupland SE, Bechrakis NE, Kellner U, Foerster MH. Vasoproliferative tumors of the retina.Br J Ophthalmol2000;84(10):1162-1169.
6 Cebeci Z, Oray M, Tuncer S, Tugal Tutkun I, Kir N. Intravitreal dexamethasone implant (Ozurdex) and photodynamic therapy for vasoproliferative retinal tumours.Can J Ophthalmol2014;49(4):e83-e84.
7 Garcia-Arumi J, Diestefano LN, Fonollosa A, Quijano C, Corcostegui B. Management of vision-threatening complications of vasoproliferative tumors of the retina.Ophthalmic Res2015;54(1):34-40.
8 Anastassiou G, Bornfeld N, Schueler AO, Schilling H, Weber S, Fluehs D, Jurklies B, Vij O, Sauerwein W. Ruthenium-106 plaque brachytherapy for symptomatic vasoproliferative tumors of the retina.Br J Ophthalmol2006;90(4):447-450.
9 Cohen VM, Shields CL, Demirci H, Shields JA. Iodine I 125 plaque radiotherapy for the treatment of vasoproliferative tumors of the retina in 30 eyes.Arch Ophthalmol2008;126(9):1245-1251.
10 Astrahan MA, Luxton G, Jozsef G, Kampp TD, Liggett PE, Sapozink MD, Petrovich Z. An interactive treatment planning system for ophthalmic plaque radiotherapy.Int J Radiat Oncol Biol Phys1990;18(3):679-687.
11 Saw CB, Seidel M, Pawlicki T, Wu A, Karasek K. Seed strength determination for eye plaque therapy.Med Dosim1993;18(1):33-37.
12 Rivard MJ, Coursey BM, de Werd LA, Hanson WF, Saiful Huq M,Ibbott GS, Mitch MG, Nath R, Williamson JF. Update of AAPM Task Group No. 43 Report: A revised AAPM protocol for brachytherapy dose calculations.Med Phys2004;31(3):633-674.
13 Krivosic V, Massin P, Desjardins L, Le Hoang P, Tadayoni R, Gaudric A. Management of idiopathic retinal vasoproliferative tumors by slit-lamp laser or endolaser photocoagulation.Am J Ophthalmol2014;158(1):154-161.
Citation:Para-Prieto M, Saornil MA, de Frutos-Baraja JM, García Álvarez C, Diezhandino García P, Lopez-Lara F. Episcleral brachytherapy as an effective alternative in vasoproliferative tumors.Int J Ophthalmol2018;11(12):2017-2020
DOl:10.18240/ijo.2018.12.23
● KEYWORDS:episcleral brachytherapy; retinal vasoproliferative tumors
Received:2018-03-09 Accepted: 2018-05-16
Correspondence to:Marta Para Prieto. Hospital Clínico Universitario, C/Ramón y Cajal 3, Valladolid 47005, Spain. marta_para@hotmail.com