Treatment controversies in a rare case of a simultaneous branch retinal artery and vein occlusion secondary to hyperhomocysteinemia and hypertension
Panayiotis Christodoulou, Ioannis Katsimpris
General Hospital of Patras “ Agios Andreas”, Ophthalmology Clinic, Kalavriton 37, Patras 26335, Greece
Dear Editor,
C ombined vascular occlusions involving retinal arteries and veins have been reported in the past. Combined occlusion of the central retinal vein (CRVO) and artery (CRAO)is well described[1]. Cilioretinal artery occlusion along with CRVO is frequently reported and is well characterized[2-3].A few cases of branch retinal artery occlusion (BRAO) has been reported to coexist with CRVO[4-5]. These vascular occlusions have been related to systemic comorbidities such as dyslipidemia, diabetes, systemic lupus erythematosus(SLE), hypertension, hyperhomocysteinemia, coagulation disturbances, and immunological diseases[6]. Combined branch retinal vein (BRVO) and BRAO affecting the same hemisphere or retinal quadrant has rarely been reported previously. A study of 308 eyes of BRVO, illustrated 56 eyes with simultaneous arterial insufficiency but not frank obstruction[5]and most other reports describe single cases[6-11]. We present a case of combined BRAO and BRVO affecting both temporal quadrants and describe the clinical, angiographic, and optical coherence tomographic (OCT) features along with systemic associations and visual outcomes. The study was conducted by the ethical standards stated in the Declaration of Helsinki and was approved by an institutional review board; written consent was obtained from the participant.
A 54-year old man attended the vitreoretinal services of our clinic due to an uncorrectable visual reduction in the right eye (OD). At first assessment, best corrected visual acuity(BCVA) was 6/10 in the OD and 10/10 in the left eye (OS).
The patient was followed for twelve months. At baseline and every follow-up visit, BCVA was recorded; gonioscopy was performed to detect anterior chamber angle neovascularization;biomicroscopic evaluation to identify iris neovascularization;fundus examination was done to confirm findings associated with BRAO and BRVO such as macular status and neovascularization at disc (NVD) or elsewhere (NVE).
Fundus fluorescein angiography (FFA) and indocyanine green angiography (ICGA) was performed at baseline examination.FFA was repeated at first follow-up visit four months later.OCT was done at every visit (baseline, at four, eight and twelve months).
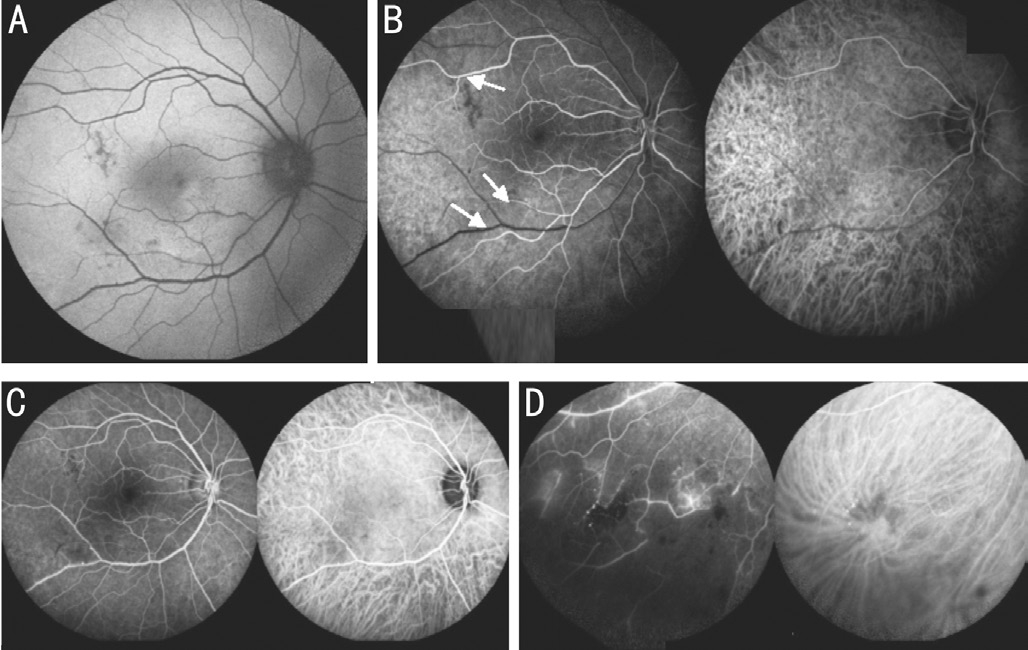
Auto fluorescence of the OD was typical (Figure 1A) of areas with a decreased intensity corresponding to hemorrhages and occluded vessels. FFA-ICGA (Figure 1) revealed significant delayed (22s) arterial filling and prolonged arterio-venous transit time (Figure 1B). Retinal vein and artery branches were occluded simultaneously in the inferior and superior temporal quadrants and extended areas of capillary drop out were displayed.Retinal veins were enlarged and tortuous (Figure 1C, 1D).
Fundus examination documented findings associated with BRAO and BRVO. OS fundus examination was unremarkable.The patient underwent a thorough systemic evaluation,including measurements of blood fasting and postprandial sugar levels, renal profile, lipid profile, and hemostasis markers including serum homocysteine levels. Inflammatory markers tested were rheumatoid factor (RF), autoantibody to nuclear antigen (ANA), double-stranded deoxyribonucleic acid (ds-DNA), cytoplasmic antineutrophil cytoplasmic antibodies (c-ANCA). The patient also underwent cardiologist’s consultations to investigate the underlying cardiovascular disease. Our patient was found to have hyperhomocysteinemia and hypertension.
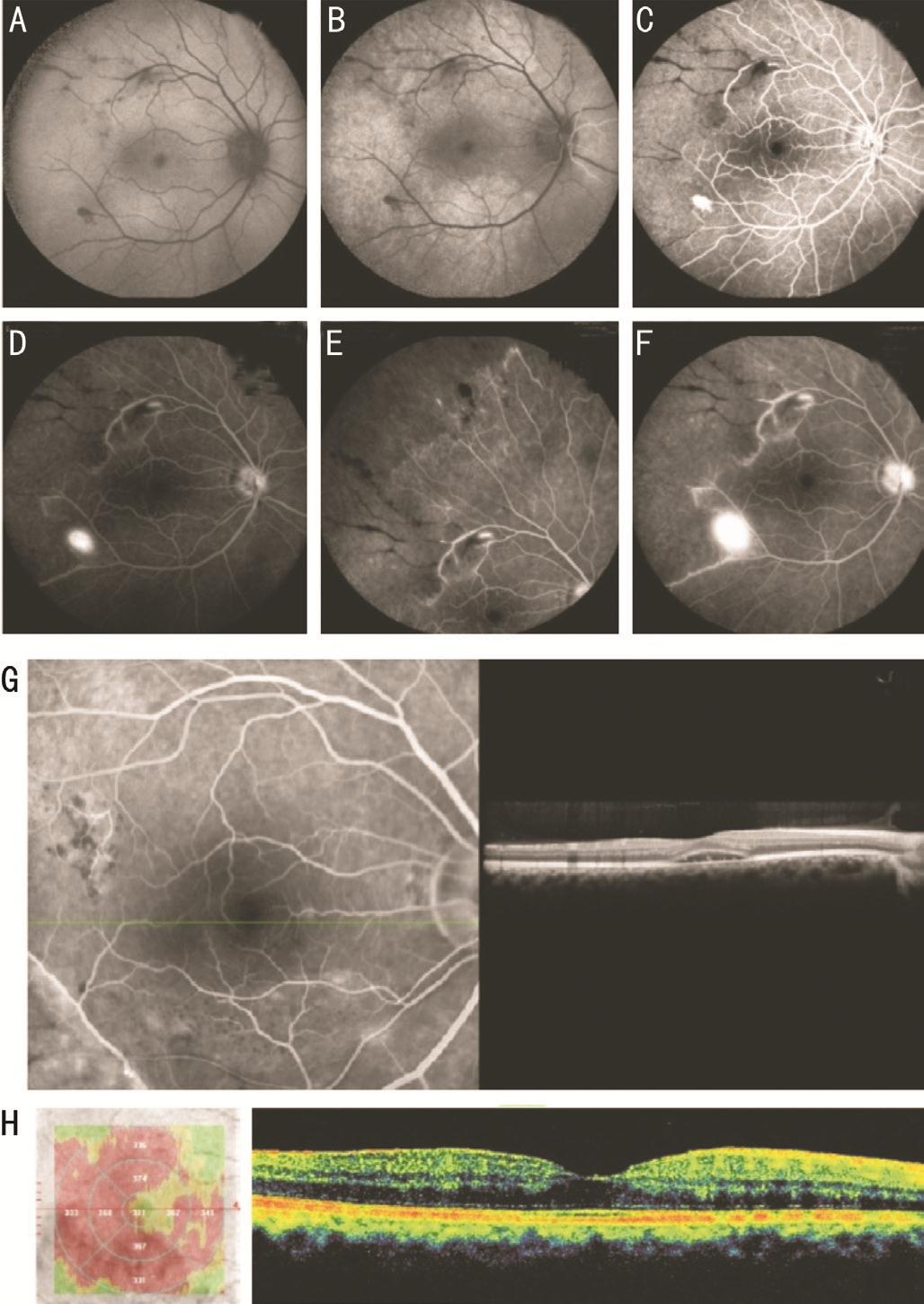
Autofluorescence and FFA (Figure 2) at first follow-up visit showed that occlusion deteriorated dramatically with a clear demarcation zone between the ischemic and perfused retina,NVD and NVE evolved. BCVA was unchanged. OCT revealed neuroretinal detachment and inner retinal opaci fication typical of arterial occlusion (Figure 2G). At this stage, the patient received scatter subthreshold diode laser micropulse (SDM)photocoagulation.
At the second follow-up visit, OCT image of macular edema and BCVA was unchanged. Intravitreal aflibercept (1.25 mg/0.05 mL)was administered, and the following day supplementary argon green laser scatter photocoagulation was performed after which BCVA reached 10/10 Snellen’s. Retina and functional status were stable for the next eight months (Figure 2H).
We describe a rare case of combined BRAO and BRVO involving both temporal quadrants. Six single cases[6-11]and a series of six cases[6]were previously reported in literature affecting the same retinal quadrant or hemisphere.
Perfusion status of the macula determines vision at presentation and visual recovery after treatment.
Pathogenetic mechanisms by which combined BRVO and BRAO occur are not precise. It was theorized[7,12]that BRVO may be the initial event. First, compression of the vein by atherosclerotic arteries at arterio-venous crossing sites leads to turbulent blood flow and dynamic obstruction or thrombus formation and mechanical blockage. Second, the severity of venous obstruction might affect arterial obstruction according to high hydraulic pressure. A sudden rise in intravenous pressure to levels above the systolic blood pressure may result in transmission of “back pressure” to the arterial circulation and subsequent compromise in arterial perfusion which manifests as BRAO. The perfusion pressure in arterial insuf ficiency can be reduced in severe venous obstruction. Third, a myogenic mechanism regulates automatically retinal blood flow, while retinal metabolic factors affect the retinal arterial tone. BRVO experimentally induced with impairment in nitric oxide (NO)release contributed to the arterial constriction[12]. Venous stasis caused by these mechanisms worsens arterial insufficiency which in turn leads to tissue hypoxia as perfusion pressure is lowered. Therefore neovascularization is not determined by the status of the arterial problem. Fourth, even though the severity of venous obstruction can induce neovascularization; reducing capillary perfusion pressure is the most potent causative factor.Laser photocoagulation at the time of initial presentation or a later stage may be controversial. We believe that due to high ischemic index and consequent vascular endothelial growth factor load eyes are at high risk for retinal and iris neovascularization. It was reported[5]neovascularization rate of 21.4% in cases of BRVO with arterial insuf ficiency. Of the cases listed in literature, NVD occurred in one case and NVG in two[6,8-9]. In our case, NVD occurred within four months despite early SDM laser application. A thorough systemic evaluation and close monitoring of cardiovascular events are critical in all cases of combined occlusion.
In conclusion, combined BRAO and BRVO are extremely rare.It is related to systemic comorbidities and may have a better visual outcome if identified early and treated appropriately.Patient with extended occlusion and ischemia should be treated promptly even without neovascularization. The ischemic index is a cardinal sign of treatment initiation[2].
ACKNOWLEDGEMENTS
Conflicts of Interest: Christodoulou P,None;Katsimpris I, None.
REFERENCES
1 Brown GC, Duker JS, Lehman R, Eagle RC Jr. Combined central retinal artery-central vein obstruction.Int Ophthalmol1993;17(1):9-17.
2 Hayreh SS, Fraterrigo L, Jonas J. Central retinal vein occlusion associated with cilioretinal artery occlusion.Retina2008;28(4):581-594.
3 Sengupta S, Pan U. Combined branch retinal vein and branch retinal artery occlusion-clinical features, systemic associations, and outcomes.Indian J Ophthalmol2017;65(3):238-241.
4 Schmidt D. Comorbidities in combined retinal artery and vein occlusions.Eur J Med Res2013;18(1):27.
5 Lee YJ, Kim JH, Ko MK. Neovascularization in branch retinal vein occlusion combined with arterial insufficiency.Korean J Ophthalmol2005;19(1):34-41.
6 Sengupta S. Combined branch retinal artery and vein occlusion in hyperhomocysteinemia.JAMA Ophthalmol2014;132(10):1255.
7 Conway MD, Tong P, Olk RJ. Branch retinal artery occlusion (BRAO)combined with branch retinal vein occlusion (BRVO) and optic disc neovascularization associated with HIV and CMV retinitis.Int Ophthalmol1995;19(4):249-252.
8 Nicolo’ M, Artioli S, La Mattina GC, Ghiglione D, Calabria G. Branch retinal artery occlusion combined with branch retinal vein occlusion in a patient with hepatitis c treated with interferon and ribavirin.Eur J Ophthalmol2005;15(6):811-814.
9 Kaur S, Sachdev N. Unilateral branch retinal arterial occlusion following administration of bevacizumab for branch retinal vein occlusion.Int Ophthalmol2013;33(5):549-552.
10 An TS, Kwon SI. Neovascular glaucoma due to branch retinal vein occlusion combined with branch retinal artery occlusion.Korean J Ophthalmol2013;27(1):64-67.
11 Okamoto N, Matsumoto C, Shimomura Y. Sequential occlusion of the branch retinal artery and branch retinal vein in a patient with hypertension:an interventional case report.Clin Ophthalmol2014;8:2121-2123.
12 Pournaras CJ, Riva CE. Retinal blood flow evaluation.Ophthalmologica2013;229(2):61-74.
Citation:Christodoulou P, Katsimpris I. Treatment controversies in a rare case of a simultaneous branch retinal artery and vein occlusion secondary to hyperhomocysteinemia and hypertension.Int J Ophthalmol2018;11(12):2024-2026
DOl:10.18240/ijo.2018.12.25
Received:2018-02-27 Accepted: 2018-07-09
Correspondence to:Panayiotis Christodoulou. 62 Ellispontou Street, Patras 26224, Greece. panayiotischristodoulou33@gmail.com