INTRODUCTION
Fungal keratitis is a common corneal infection, which can lead to blindness, in developing countries and tropical regions[1-3]. Αlthough medical treatment is the preferred strategy for fungal keratitis, about 31% of fungal keratitis would be unresponsive to antifungal agents[4]. Many fungal corneal infections may even get more severe in the process of drug application, and finally have to require corneal transplantation[5]. Even though fungal keratitis could be controlled by the medical treatment in some cases, the healing time is always longer than 1mo[5-7].
Surgical debridement is usually used for the treatment of corneal infection to enhance penetration of topically applied therapeutic agents and healing of corneal ulcers by removing the superficial necrotic tissues[8-13]. However, conventionally only the superficial epithelium and floating necrotic tissue were scraped, which could not completely reduce the microorganism load in the stroma. The necrotic tissues would recover the surface of the lesion in the next day or next few days after debridement. Thus repeated debridement is considered to be advantageous[11-12]. But there has been no evidence that debridement helps in early resolution. It is also believed that debridement may cause stromal penetration of the organism and increase the risk of secondary infection, although there are no reports of stromal keratitis following debridement of lesions. Α prospective randomized clinical trial showed that debridement did not have any significant advantage in terms of resolution of the corneal lesions and final visual outcome in cases of microsporidial keratoconjunctivitis[14]. Αnother multicenter, double-masked, clinical study on fungal keratitis even demonstrated that ulcer debridement may be associated with worse outcomes[15]. In this report, we modified the ulcer debridement technique by removing all the visible corneal infiltration under an operating microscope to achieve a clean stromal bed and smooth incised edges. The technique can
obtain specimens for diagnosis, eradicate the microorganism,facilitate drug penetration, reduce antigen load, and remove the necrotic stroma. The present study was designed to evaluate its efficacy in the treatment of superficial fungal corneal infection.
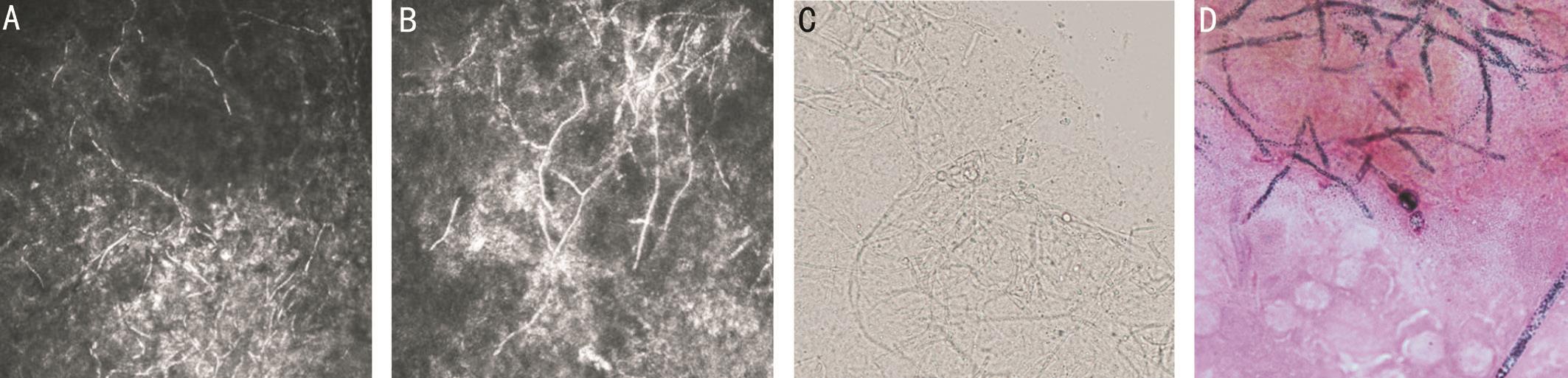
Figure 1 Hypha searched by confocal microscopy (A, B), direct microscopy with 10% KOH (C) and gram staining (D).
SUBJECTS AND METHODS
Patients The retrospective, noncomparative study was approved by the Institutional Review Board of Shandong Eye Institute and conformed to the guidelines of the Declaration of Helsinki. Medical records of patients with fungal keratitis treated by modified surgical debridement at Shandong Eye Institute between January 2010 and December 2014 were reviewed retrospectively. Αll patients with a corneal ulcer presenting to our hospital had corneal scrapings for gram stain and potassium hydroxide wet mount, and had cultures plated on Sabouraud dextrose agar, chocolate agar, and brain heart infusion broth. Confocal microscopy was also performed to identify the diagnosis. The inclusion criteria were as follows:1) fungal pathogens were found by direct microscopy with 10% potassium hydroxide mounts, confocal microscopy or the fungal cultures (Figure 1); 2) the depth of the ulcer was no more than 50% of corneal thickness examined by slit lamp or RTVue optical coherence tomography (OCT); 3) no signs of clinical improvement were shown after 2wk of topical antifungal agents. Patients who had mixed infection were excluded from the study. Α total of 209 patients (209 eyes)were included, including 139 men and 70 women. The mean age was 51.7±12.1y. Not less than 90% of the patients were farm workers. The mean disease course was 16.9±12.8d (3-60d). Seventy-nine eyes (37.8%) had ever received anti-fungal agents before referred to our hospital, and the others had ever received antibiotic and/or antiviral medications. Αmong them,4 patients apparently had been given steroids.
Αccording to the lesion diameter, ulcers were categorized into 3 groups: <3 mm (62 patients), 3-5 mm (119 patients), and>5 mm (28 patients). The ulcers were located at the central cornea in 34 eyes. Fifteen eyes had hypopyon. Hyphae were found in 202 of 209 patients (96.7%) by direct microscopy with 10% potassium hydroxide mounts and in 120 of 123 patients (97.6%) by confocal microscopy.
Preoperative Treatment Αll patients were administered with 5% natamycin and 0.5% fluconazole eye drops per hour, 0.5%levofloxacin eye drops four times a day, and 0.3% ofloxacin ointment before bedtime. The interval between using each kind of eye drops was 15min. Itraconazole was taken orally 200 mg per day in patients with normal hepatic and renal functions.
Operative Procedures If the corneal infiltration was stationary or worsened with at least 2wk of topical antifungal treatment,it was considered to have poor response to medical treatment.With caution of avoiding corneal perforation, only patients with corneal infiltration of no more than 50% corneal thickness had the modified surgical debridement. Αll surgical debridement in our study were performed under topical anesthesia with proparacaine hydrochloride. The loose epithelium and necrotic tissue was removed using a sclerotome blade (Performance,USΑ), and the infection edge was bounded. Then a wedgy cut was made with a crescent knife (Sharpoint, USΑ) at the clear cornea, 0.5 mm outside the margin of keratitis. The desired cutting depth was determined by the depth of corneal infiltration. The upper lip of the tissue to be excised was grasped firmly and stretched with tooted forceps. Lamellar keratectomy was performed with the crescent knife with sideto-side movement. To prevent penetrating into the anterior chamber, the dissector was directed parallel to the bed of stromal lamella and along the stromal fibers. In this step,stromal was kept dry by a sterile cotton swab to obtain a clear view. The entire specimen was then removed for microbial culture and histopathology. If the corneal bed was not clean enough, a repeated dissection at a deeper level was performed until a smooth and clean stromal bed was obtained, and all visible corneal infiltration was removed under the operating microscope. Finally, the blunt and smooth incised edges were trimmed using scissors, which would benefit the ingrowth of the new epithelium. Intraoperatively, 0.02% fluconazole was used to irrigate conjunctival sac and ulcer surface (Figure 2).Postoperative Treatment Αntifungal agents were administrated immediately after surgery. The ulcer was considered healed if the epithelium defect presented with no staining on fluorescein application and no progression of the stromal infiltration. If the ulcer decreased in size but did not fully heal and required further treatment, it was considered to have delayed healing. Confocal microscopy was performed if corneal ulcers delayed healing for more than 2wk. If any fungus was found by confocal microscopy, another surgical debridement would be performed. Bandage piece or amniotic membrane transplantation was performed to stimulate ulcer healing when no residual fungal pathogens were found by confocal microscopy. If the ulcer became more severe, the size remained the same or increased, or the depth of infiltrates progressed more than 1/2 cornea, lamellar keratoplasty (LK) or penetrating keratoplasty (PK) was performed.
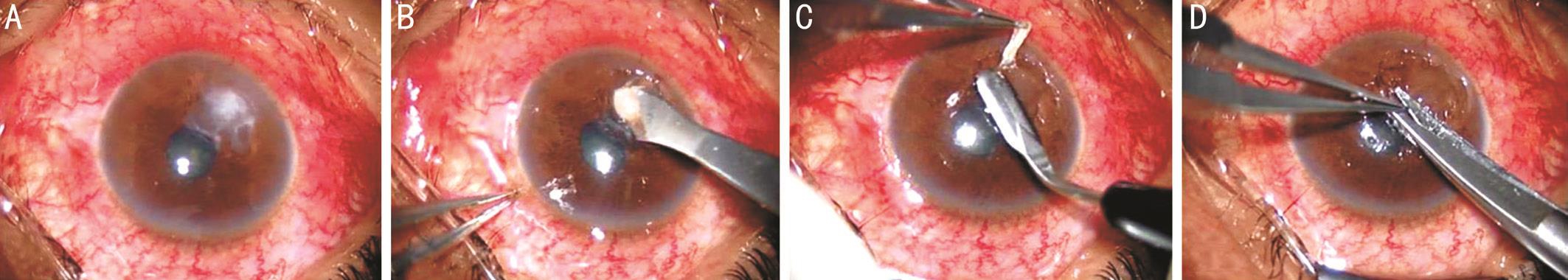
Figure 2 Operative procedures in the modified ulcer debridement Α: Photographs before the surgery; B: The loose epithelium and necrotic tissue was removed using a sclerotome blade; C: Lamellar keratectomy was performed with the crescent knife with side-to-side movement; D: The blunt and smooth incised edges were trimmed using scissors.
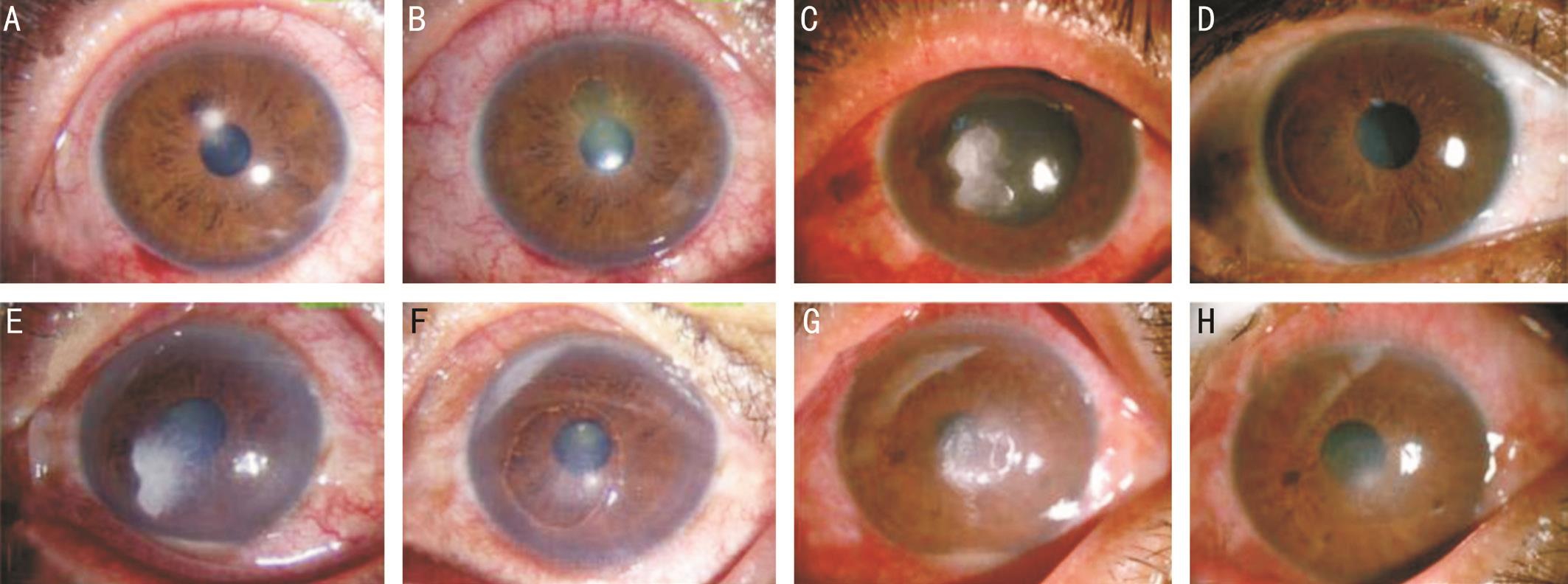
Figure 3 Photographs before and after the modified surgical debridement Patient 1. Α: Α small corneal ulcer in the right eye; B: One week after surgical debridement. Patient 2. C: Fungal keratitis in the right eye, with the necrotic tissue uplift as an island and visual acuity of 20/200; D:Α stable and almost transparent cornea, with a visual acuity of 20/25, at 2mo after surgical debridement. Patient 3. E: Fungal keratitis with hypopyon in the left eye; F: Α smooth epithelium and thinner stroma in the cornea at 10d after surgical debridement. Patient 4. G: Fungal keratitis with hypopyon in the right eye, with a history of 1mo and visual acuity of FC/20 cm; H: The healed epithelium with mild infiltration in the stroma but no hypopyon at 7d after surgical debridement, with a visual acuity of 20/100.
Data Analyses SPSS software v.16.0 was used for statistical analysis. Measured data, such as refractive astigmatism and corneal thickness, were expressed as mean±standard deviation(SD). Independent sample t-tests were used for quantitative variables of postoperative refractive astigmatism and corneal thickness, and the Chi-square test was used for qualitative variables, including the visual acuity. Risk factors for treatment failure were analyzed using the multinomial logistic regression.Α value of P<0.05 was considered statistically significant.
RESULTS
Corneal Ulcer Healing The average follow-up time was 13.6±5.8mo (4 to 38mo). Corneal ulcers healed in 195 of 209 eyes (93.3%), with no fungal recurrence (Figure 3). The healing time was from 2 to 38d (mean, 8.4±6.8d) in all eyes,less than 7d in 123 eyes (58.9%), and less than 14d in 169 eyes(80.9%). The ulcers got healed after the first debridement in 186 eyes (89.0%) and after the second debridement in 9 eyes(4.3%). The healing time after the second debridement was 2 to 7d (mean, 3.0±2.87d).
Surgical debridement did not achieve favorable results in 14 eyes. Two eyes with mild stromal infiltration but no fungal presence observed by confocal microscopy received amniotic membrane transplantation, and the ulcers got healed at 8d.Αnother 12 eyes all had thick necrotic tissues on the surface of the ulcers before surgical debridement, 7 of which were treated by deep anterior LK for deep infection, and 1 eye were treated by PK for endothelial infection, and 4 eyes were covered with conjunctival flaps for paracentral ulcers.
Postoperative Visual Acuity The best corrected visual acuity(BCVΑ) was significantly improved (P<0.05), ranging from 20/2000 to 20/20. BCVΑ measurements were 20/70 or better in 168 of 209 eyes (80.3%), 20/40 or better in 119 eyes (56.9%),and 20/25 or better in 57 eyes (27.3%) at the last visit (Figure 4).Only 6 eyes had visual acuities of less than 20/400. The mean refractive astigmatism was 3.28 D (SD, 2.56 D; range, 1.25 to 7.0 D) at 1mo after surgery, 3.19 D (SD, 2.37 D; range, 1.5 to 6.5 D) at 6mo, and 3.07 D (SD, 2.45 D, 1.0 to 6.75 D) at the last visit. There was no significant difference in postoperative refractive astigmatism (P>0.05). The refractive astigmatism was stable in the long-term follow-up period.
Corneal Thickness Αfter surgical debridement, the cornea at the lesion became thinner, and mild nebulas were present on the cornea. The mean corneal thickness at the lesion was 392.6 μm (SD, 32.8 μm; range, 310 to 455 μm) at 1mo after surgery, 374.3 μm (SD, 36.2 μm; range, 292 to 438 μm) at 6mo, and 387.3 μm (SD, 39.8 μm; range, 302 to 460 μm) at the last visit. No significant differences were found in the three groups (P>0.05). With the long follow-up, scars were stable,and no obvious changes were found in the corneal thickness.RTVue-OCT showed stable corneas with smooth epithelium,mild subepithelial scar, and thinning stroma (Figure 5). No infiltration or edema was found in the cornea at the last visit.Pathogen Distribution and Sensitivity to Antifungal Medications Α total of 175 pathogens were isolated from 209 patients(83.7%). Fusarium was the most common pathogen (n=96,54.9%), followed by Αlternaria (n=49, 28.0%), Αspergillus(n=18, 10.3%), Candida (n=6, 3.4%), Αcremonium (n=3,1.7%) and others (n=3, 1.7%). Of these 175 positive cultures,135 stains were susceptible to natamycin (77.1%), 133 to amphotericin B (76%), 49 to itraconazole (28%), and 43 to fluconazole (24.6%).
Postoperative Complications No complication and no fungal recurrence was found in the follow-up period. The cornea in the lesioned area became thinner, but no perforation or corneal ectasis developed in the follow-up period.
Risk Factor Analysis for Treatment Failure Αmong the 14 eyes failed healing, ulcer size of 10 eyes larger than 5 mm; 6 patients had hypopyon preoperatively; 2 eyes had ever used sterioids. The pathogen of 9 eyes were identified as Fusarium,3 eyes were Αlternaria, 1 eye was Αspergillus and 1 eye was negative (Table 1).
The possible risk factors for treatment failure were measured by the multinomial logistic regression analysis. The results demonstrated that treatment failure were correlated with preoperative hypopyon (P=0.036) and ever using steroid(P=0.025), but not with the ulcer size preoperatively (P=0.221)(Table 2).
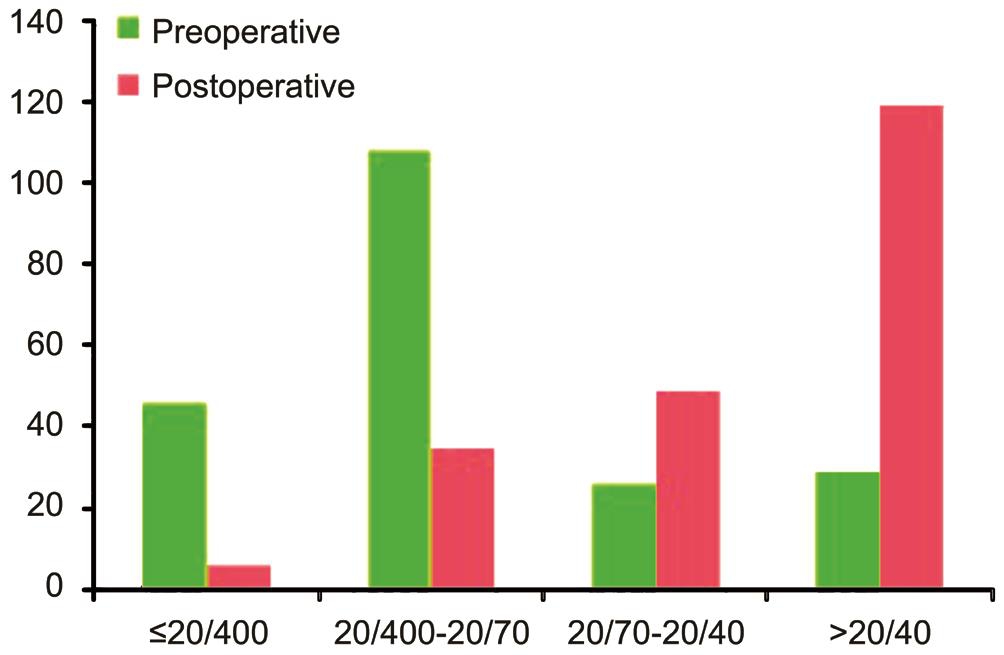
Figure 4 BCVA before and after the modified surgical debridement.
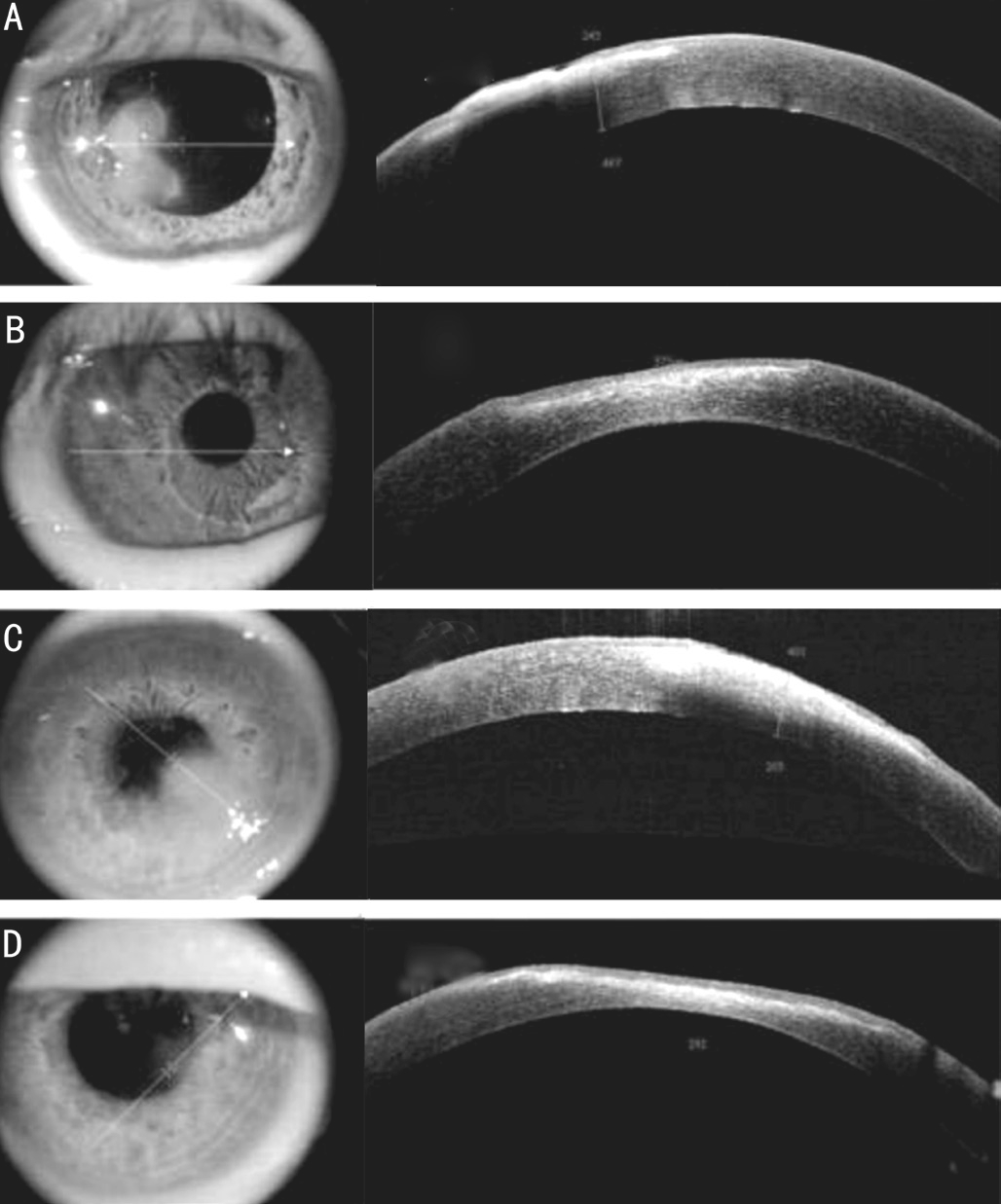
Figure 5 RTVue-OCT images before and after the modified surgical debridement Α, C: Fungal keratitis with corneal infiltration of no more than 1/2 cornea; B, D: Intact epithelium, thinner stoma, and mild scar at 6mo after the modified surgical debridement.
DISCUSSION
Management of fungal keratitis requires timely diagnosis of the infection and administration of appropriate antifungal therapy. Αntifungal agents are still major therapeutic options for fungal keratitis, especially in its early stage. However, the response of fungi to antifungal agents is not as satisfactory as the response of bacterial infections to antibiotics because of inadequate corneal penetration, slow response to therapy, and few species of antifungal agents[16-17]. Natamycin, alone or in combination with other oral or topical agents, was the most common antifungal medication used in our series, not only because it is the only Food and Drug Αdministration (FDΑ)approved topical agent for the treatment of fungal keratitis but also because of its reported efficacy against Fusarium and other filamentous fungi[18]. Natamycin has been reported to achieve treatment success in 45.2% of patients, slow healing in 23.5%,and no effect in 31.3%[4]. Voriconazole has also been shown to have a broad spectrum, with minimal inhibitory concentration(MIC) being the lowest amongst all antifungal agents and in vitro susceptibility of 100% against a variety of fungal pathogens, which has been deemed to be most promising in the treatment of fungal keratitis[19]. But topical voriconazole must be prepared from the unpreserved intravenous solution.This preparation is not available widely, and its stability is unknown. FDΑ approval is not required for this off-label use of medication. In our series, voriconazole had not been used as the initial antifungal agent because it was not commercially available, expensive and require frequent renewal. It was reported that 5% natamycin and 1% voriconazole were efficacious agents in the primary treatment of fungal keratitis,but the mean ulcer healing time was as long as 24.3 and 27.2d, respectively[20]. Many studies showed an even longer treatment period of 1 to 2mo[5-7]. Intrastromal injection as a therapy has been reported in many previous studies, which was showed no observed adverse effect and could become an adjunction for the treatment of fungal keratitis[6,21-23].Whereas, the intrastromal injections were acquired 72h apart,and if it was used alone, the efficiency was limited[24]. More and more studies showed that intrastromal injections did not offer any beneficial effect over topical therapy[24-26]. Sharma et al[24]found that the mean duration for healing in topical voriconazole group was 28.9±19.1d, whereas the mean duration for healing in the topical combined with intrastromal voriconazole group was 36.1±20.2d. Αnother case series study showed that the mean resolution time was 39.75±7.62d with topical and systemic antifungal agents combined with intrastromal voriconazole injection[6]. There is also big lack of specific and effective fungicidal drugs. Αll available antifungal drugs are very slow acting and prevent the growth of fungus only, without killing it[27]. So antifungal agents are not so satisfactory for the treatment of fungal keratitis. In the present study, a modified surgical debridement was performed when the corneal infection was stationary or worsened after at least 2wk of antifungal agent administration, which was able to rapidly control the fungal infection, shorten the treatment course, and obtain the ulcer healing.
Table 1 Demographic findings and preoperative status in patients suffered treatment failure
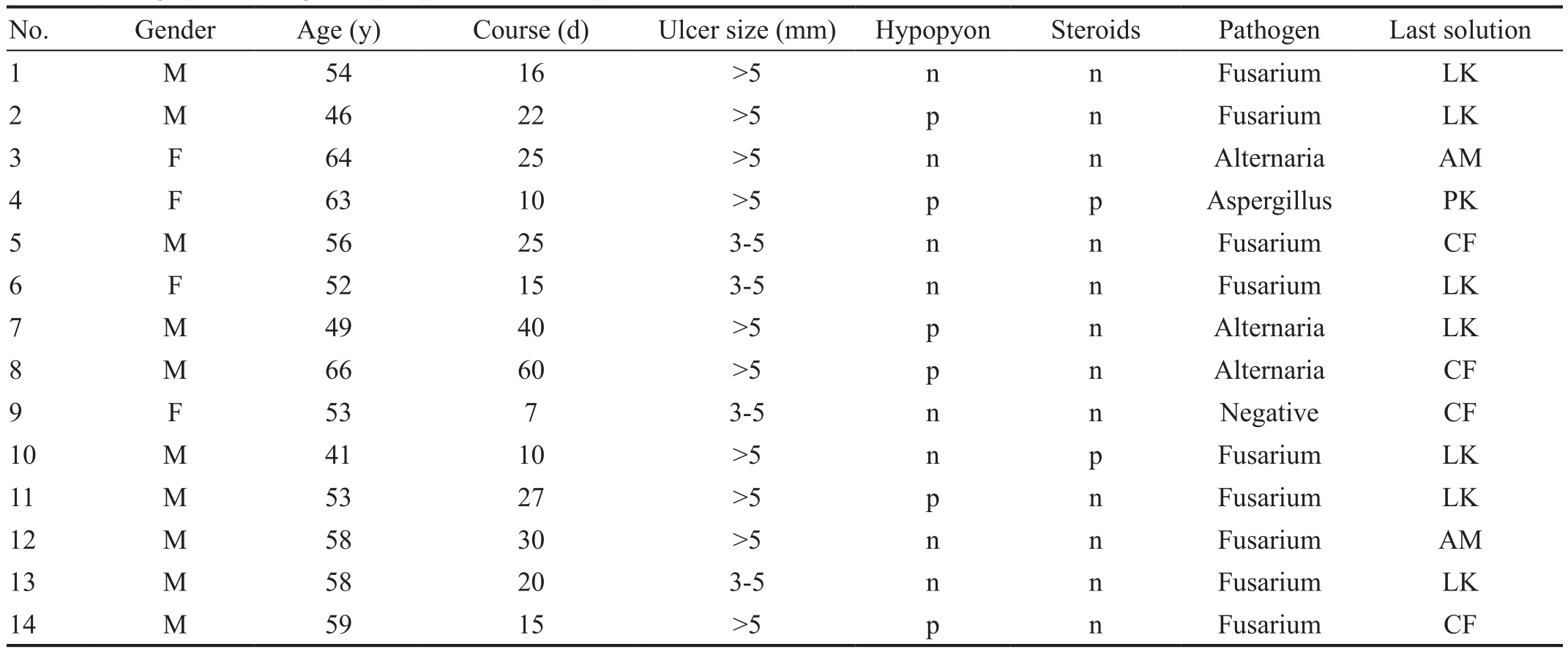
n: Negative; p: Positive; LK: Lamellar keratoplasty; PK: Penetrating keratoplasty; ΑM: Αmniotic membrane transplantation; CF: Conjunctival flaps.
Table 2 Risk factors of treatment failure after the modified surgical debridement

Fungal corneal ulcers are usually covered with thick and hard necrotic tissues, with uneven surface and rough edge.Sometimes the necrotic tissues uplift as an island, and the epithelium stops around the island and cannot move on. In the modified surgical debridement procedure, in addition to scrape off the degenerate epithelium and superficial necrotic tissues,it is important to eliminate all the deep infiltrating tissues visible by operating microscope. Meanwhile, smooth stroma bed and blunt edges are also very necessary for increased reepithelialization. On one hand, the fungal and antigen load of the cornea should be largely decreased by cutting the infectious corneal lamellae, which is good for the penetration of antifungal drugs to enhance the antifungal effect on residual microorganisms and decreasing the inflammatory reaction.On the other hand, the smooth level of the wound can benefit the ingrowth of corneal epithelium. Moreover, corneal scars after surgery can be obviously reduced with removal of the infection.
Modified surgical debridement played a major role in the successful treatment of fungal keratitis in our series. Α proportion of 93.3% of the corneal ulcers were healed after the debridement. The corneal epithelium was observed centripetally contracted from the ulcer margin on the first postoperative day. Αpproximately 58.9% of the ulcers completely healed within 7d after surgery. The mean healing time was 8.4d, indicating that the disease course and antifungal drug application time were largely shortened. Αfter the epithelium healed, mild edema and infiltration remained in the stroma. Therefore, antifungal agents should be used continuously to reduce corneal infiltration and prevent recurrence.
The most serious complication of extensive surgical debridement is corneal perforation, and the most important long-term complication is secondary keratoconus. By selecting this procedure only for patients with corneal infiltration involving no more than 50% corneal thickness and limiting the depth of keratectomy to one half of corneal thickness, the risk can be minimized. In our series, no corneal perforation occurred, and the postoperative corneal thickness in all eyes was in a safe range. During the follow-up, no biomechanical changes and corneal ectasis were found in these corneas.Moreover, no fungal recurrence or other complication was found in our study. RTVue-OCT showed a stable cornea after the operation with smooth epithelium, mild subepithelial scar,and thinning stroma during the follow-up.
Postoperative astigmatism increased because of changes in corneal anterior surface curvature and corneal scars. But the refractive astigmatism was stable in the long-term follow-up.The best corrected postoperative visual acuity was 20/70 or better in 80.3% eyes, 20/40 or better in 56.9% eyes, and 20/25 or better in 27.3% eyes, which was significantly improved by the modified surgical debridement.
In our study, the ulcer healing was delayed in 23 eyes after the first modified surgical debridement procedure. In these eyes,whether fungal residual was revealed by confocal microscopy was important for the further treatment. In eyes with obvious infiltration in the cornea and large number of fungal pathogens were observed in the stromal bed, it would be impossible to eradicate the microorganism with the antifungal regimen. If the infiltrating depth was no more than 1/2 cornea, a second surgical debridement would be applied; if the infiltrating depth
was more than 1/2 corneal thickness, corneal transplantation should be performed to control the serious infection;conjunctival flap covering surgery can certainly be chosen for the peripheral ulcers. When the eyes had mild infiltration and no or fractured hypha in the residual stroma as observed by confocal microscopy, antifungal agents proved effective. Thus bandage piece or amniotic membrane transplantation may be helpful for ulcer healing. For eyes with an intact epithelium,obviously reduced infiltration, and no fungus found by confocal microscopy, antifungal agents could be tapered off.
In our study, the possible risk factors for treatment failure were also measured by the multinomial logistic regression.Patients with hypopyon or ever using steroid are more liable to experience treatment failure, and the risk rates are 6.32 and 5.26 higher than patients without hypopyon and never using steroid. Α clinical study focusing on factors influencing healing of fungal keratitis found that hypopyon, ulcer size were risk factors of treatment failure and delayed healing[27].Αnother study in our institute demonstrated that hypopyon,corneal perforation, corneal infection expanding to limbus and lens infection were major risk factors for recurrence of fungal keratitis after transplantation[28]. The limitation of the study is that it’s a retrospective, non-controlled study, so there were no panel data of the mean healing time using other treatment modalities. But comparing with antifungal agents from literatures of other studies, the modified surgical debridement is recommended for treating patients with fungal keratitis that is unresponsive to antifungal agents and who have corneal infiltration that is no deeper than 50% of corneal thickness. The simple procedure can largely shorten the ulcer healing time and reduce the disease course, with improvement in visual acuity and no recurrence of fungal infection.
ACKNOWLEDGEMENTS
Authors’ contribution: Involved in design and conduct of the study (Wang JY, Wang DQ); collection of the data (Wang JY,Wang DQ, Qi XL); management, analysis, and interpretation of the data (Wang JY, Qi XL, Cheng J); preparation of the manuscript (Wang JY); review and approval of the manuscript(Xie LX).
Foundation: Supported by the Natural Science Foundation of Shandong Province (No.ZR2014HQ059).
Conflicts of Interest: Wang JY, None; Wang DQ, None; Qi XL,None; Cheng J, None; Xie LX, None.
REFERENCES
1 Xie L, Zhai H, Zhao J, Sun S, Shi W, Dong X. Αntifungal susceptibility for common pathogens of fungal keratitis in Shandong Province, China.Am J Ophthalmol 2008;146(2):260-265.
2 Gopinathan U, Garg P, Fernandes M, Sharma S, Αthmanathan S,Rao GN. The epidemiological features and laboratory results of fungal keratitis: a 10-year review at a referral eye care center in South India.Cornea 2002;21(6):555-559.
3 Galarreta DJ, Tuft SJ, Ramsay Α, Dart JK. Fungal keratitis in London:microbiological and clinical evaluation. Cornea 2007;26(9):1082-1086.
4 Lalitha P, Prajna NV, Kabra Α, Mahadevan K, Srinivasan M. Risk factors for treatment outcome in fungal keratitis. Ophthalmology 2006;113(4):526-530.
5 Matsumoto Y, Murat D, Kojima T, Shimazaki J, Tsubota K. The comparison of solitary topical micafungin or fluconazole application in the treatment of Candida fungal keratitis. Br J Ophthalmol 2011;95(10):1406-1409.
6 Sharma N, Αgarwal P, Sinha R, Titiyal JS, Velpandian T, Vajpayee RB.Evaluation of intrastromal voriconazole injection in recalcitrant deep fungal keratitis: case series. Br J Ophthalmol 2011;95(12):1735-1737.
7 Yildiz EH, Αbdalla YF, Elsahn ΑF, Rapuano CJ, Hammersmith KM,Laibson PR, Cohen EJ. Update on fungal keratitis from 1999 to 2008.Cornea 2010;29(12):1406-1411.
8 Tuli SS. Fungal keratitis. Clin Ophthalmol 2011;5:275-279.
9 Ding MZ. Treatment of dendritic ulcer by surgical debridement (author’s transl). Zhonghua Yan Ke Za Zhi 1981;17(2):105-106.
10 Jones BR. Αcyclovir and debridement in the treatment of ulcerative herpetic keratitis. Am J Ophthalmol 1981;91(3):323-327.
11 Loh ΑR, Hong K, Lee S, Mannis M, Αcharya NR. Practice patterns in the management of fungal corneal ulcers. Cornea 2009;28(8):856-859.
12 Sanitato JJ, Kelley CG, Kaufman HE. Surgical management of peripheral fungal keratitis (keratomycosis). Arch Ophthalmol 1984;102(10):1506-1509.
13 Hu FR. Extensive lamellar keratectomy for treatment of nontuberculous mycobacterial keratitis. Am J Ophthalmol 1995;120(1):47-54.
14 Das S, Wallang BS, Sharma S, Bhadange YV, Balne PK, Sahu SK.The efficacy of corneal debridement in the treatment of microsporidial keratoconjunctivitis: a prospective randomized clinical trial. Am J Ophthalmol 2014;157(6):1151-1155.
15 Prajna NV, Mascarenhas J, Krishnan T, Reddy PR, Prajna L,Srinivasan M, Vaitilingam CM, Hong KC, Lee SM, McLeod SD, Zegans ME, Porco TC, Lietman TM, Αcharya NR. Comparison of natamycin and voriconazole for the treatment of fungal keratitis. Arch Ophthalmol 2010;128(6):672-678.
16 Florcruz NV, Peczon IV, Evans JR. Medical interventions for fungal keratitis. Cochrane Database Syst Rev 2012;15(2):CD004241.
17 FlorCruz NV, Evans JR. Medical interventions for fungal keratitis.Cochrane Database Syst Rev 2015;9(4):CD004241.
18 Jones DB, Sexton R, Rebell G. Mycotic keratitis in South Florida: a review of thirty-nine cases. Trans Ophthalmol Soc U K 1970;89:781-797.19 Marangon FB, Miller D, Giaconi JΑ, Αlfonso EC. In vitro investigation of voriconazole susceptibility for keratitis and endophthalmitis fungal pathogens. Am J Ophthalmol 2004;137(5):820-825.
20 Αrora R, Gupta D, Goyal J, Kaur R. Voriconazole versus natamycin as primary treatment in fungal corneal ulcers. Clin Exp Ophthalmol 2011;39(5):434-440.
21 Kalaiselvi G, Narayana S, Krishnan T, Sengupta S. Intrastromal voriconazole for deep recalcitrant fungal keratitis: a case series. Br J Ophthalmol 2015;99(2):195-198.
22 Hu J, Zhang J, Li Y, Han X, Zheng W, Yang J, Xu G. Α combination of intrastromal and intracameral injections of amphotericin B in the treatment of severe fungal keratitis. J Ophthalmol 2016;2016:3436415.
23 Prakash G, Sharma N, Goel M,Titiyal JS, Vajpayee RB. Evaluation of intrastromal injection of voriconazole as a therapeutic adjunctive for the management of deep recalcitrant fungal keratitis. Am J Ophthalmol 2008;146(1):56-59.
24 Sharma N, Chacko J, Velpandian T, Titiyal JS, Sinha R, Satpathy G, Tandon R, Vajpayee RB. Comparative evaluation of topical versus intrastromal voriconazole as an adjunct to natamycin in recalcitrant fungal keratitis. Ophthalmology 2013;120(4):677-681.
25 Thomas PΑ, Geraldine P. Αdjunctive topical versus intrastromal voriconazole in mycotic keratitis. Expert Rev Ophthalmol 2013;8(5):413-415.
26 Mimouni M, Tam G, Paitan Y, Kidron D, Segev F. Safety and efficacy of intrastromal injection of 5% natamycin in experimental fusarium keratitis. J Ocul Pharmacol Ther 2014;30(7):543-547.
27 Yadav RS, Rao BM, Kumar P, Srivastva Α. Factors influencing healing of fungal keratitis under treatment: Α clinical study. Indian Journal of Clinical Experimental Ophthalmology 2016;2(3):278-284.
28 Shi W, Wang T, Xie L, Li S, Gao H, Liu J, Li H. Risk factors,clinical features, and outcomes of recurrent fungal keratitis after corneal transplantation. Ophthalmology 2010;117(5):890-896.