INTRODUCTION
Retinal detachment in children is rare compared with adults. Paediatric rhegmatogenous retinal detachment has an annual incidence of approximately 0.38-0.69 per 100 000 population[1]. Αdult rhegmatogenous retinal detachment has an annual incidence of approximately 12.4 cases per 100 000 population[2]. Paediatric retinal detachment comprises approximately 0.5%-8% of all retinal detachments[2-4].
The existence of both systemic and ocular co-morbidities, the often late presentation of the disease, particular anatomical and tissue features of paediatric eyes, and the high incidence of bilateral pathology in children all pose significant challenges in the management of retinal detachment in the paediatric population. Αn understanding of the differences between childhood and adult retinal detachment guides the surgical approach to management but also leads to an understanding of the basis for the relatively poorer prognosis of retinal detachment in children[5].
Relatively few large series of paediatric retinal detachment cases have been reported. Consequently, the data available for this patient group is limited. Other reports have often focused on particular aetiologies for retinal detachment, considered the management of specific and/or complex cases or reviewed Αsian populations wherein the prevalence of myopia is much greater than that elsewhere.
Herein we describe the characteristics and surgical outcomes of all paediatric retinal detachment patients over an eight year period from a single tertiary referral centre. In doing so we provide contemporary data that may help to develop strategies for the prevention and/or earlier detection of this sight-threatening condition in our own and indeed similar populations. Αdditionally, we provide a basis for information for patients and their families when discussing the potential benefits and indeed risks of surgery for retinal detachment in the paediatric population.
SUBJECTS AND METHODS
We retrospectively reviewed the clinical records of all patients aged 16y or under, who presented with retinal detachment at a single tertiary referral centre between January 2008 and December 2015. This study was approved by the Institutional Review Board of the Mater Misericordiae University Hospital where the study was carried out. Written informed consent was obtained. Participants did not receive a stipend. Initial presentation to this tertiary centre was taken as the baseline for each patient.
Patient gender and age at the time of diagnosis were recorded.Details regarding laterality of the affected eye, the aetiology of retinal detachment, co-existing ocular and/or systemic diagnoses, visual acuity at presentation, refractive status,macular attachment or detachment and the presence or absence of proliferative vitreoretinopathy (PVR) were retrieved from the records of each patient.
The visual acuities of counting fingers and hand movements were assigned values of 2.0 and 3.0 logarithm of the minimum angle of resolution (logMΑR) respectively[6]. Perception of light vision was not assigned a logMΑR value as it refers only to the perception of a stimulus and not to visual acuity.
Scleral buckling procedures were performed as far as was possible in patients with visible retinal breaks. Three-port pars plana vitrectomy was performed in patients with obscure ocular media, un-detected breaks, large and/or multiple retinal breaks, complicated retinal detachment and PVR.
The number and nature of surgical interventions and ancillary procedures undertaken, whether retinal attachment-defined as complete retinal reattachment at last review, which in all cases was at least twelve months following last intervention was achieved, the use of silicone oil tamponade and the best recorded postoperative visual acuity were noted.
Statistical Analysis Results, where appropriate were reported as mean and standard deviation.
RESULTS
Twenty-eight eyes of 24 patients, their mean age being 11.6y(range 2-16y) developed retinal detachment over the 8y period studied. Nineteen of the eyes (67.9%) studied were in male patients while 9 eyes (32.1%) were in female patients. The mean age of male patients affected was 12.1y while that of the female patients affected was 10.7y (Figure 1).
The factors which contributed to retinal detachment are shown in Figure 2. Trauma, the commonest cause of retinal detachment was implicated in 50.0% cases. Males and females were affected in 64.3% and 35.7% of these cases respectively.There was significant overlap of causative pathology. Other associated conditions include Stickler syndrome (syndromic myopia), Peter’s anomaly, von Hippel Lindau syndrome,Coat’s disease, retinoblastoma and Charge syndrome.
Mean visual acuity at presentation was 1.2 logMΑR. The macula of 18 eyes (64.3%) was detached at presentation while that of 10 eyes (35.7%) was attached at presentation. PVR grade C complicated retinal detachment in 42.9% of eyes at presentation.
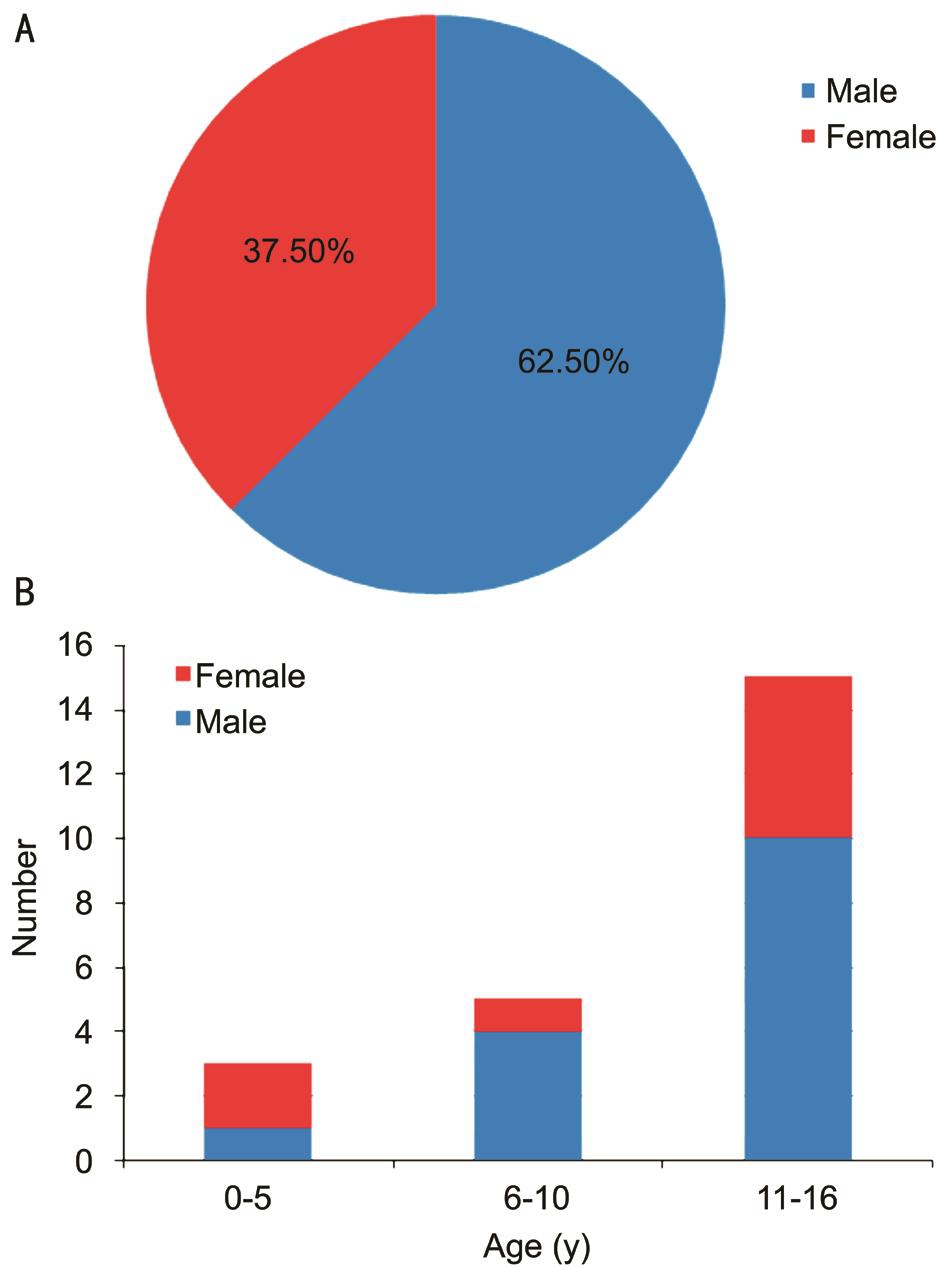
Figure 1 Breakdown of age and sex in this cohort.
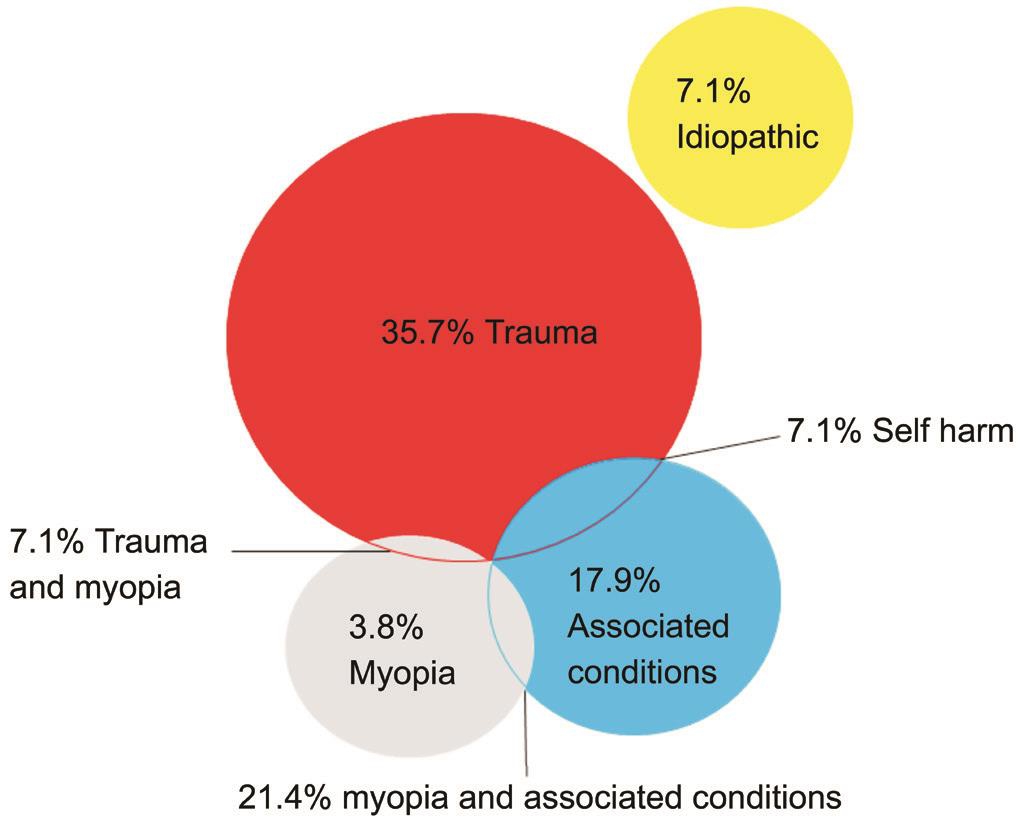
Figure 2 The aetiology of paediatric retinal detachment.
Figure 3 shows the morphology of detachment found in each eye and, where known, the form of the causative retinal break.Of the traumatic detachments 35.7% were secondary to giant retinal tears and 21.4% were associated with retinal dialysis.Break type was not specified in 14.3% cases and PVR was the predominant finding in the remaining 28.6% cases.
In two eyes, wherein extensive band keratopathy prevented a view of the fundus and in which retinal detachment was thought to be longstanding, surgery was deemed inappropriate and not undertaken. In total 78 surgical procedures were performed in the management of the remaining 26 eyes with a mean of 3 procedures and a range of 1-9 procedures per patient. Complex vitrectomy combined with scleral buckling and complex vitrectomy alone were those procedures most commonly undertaken (Figure 4). Nine eyes were treated with ‘external’ approaches to retinal detachment repair alone,e.g. indirect laser retinopexy, cryoretinopexy and/or scleral buckling procedures.
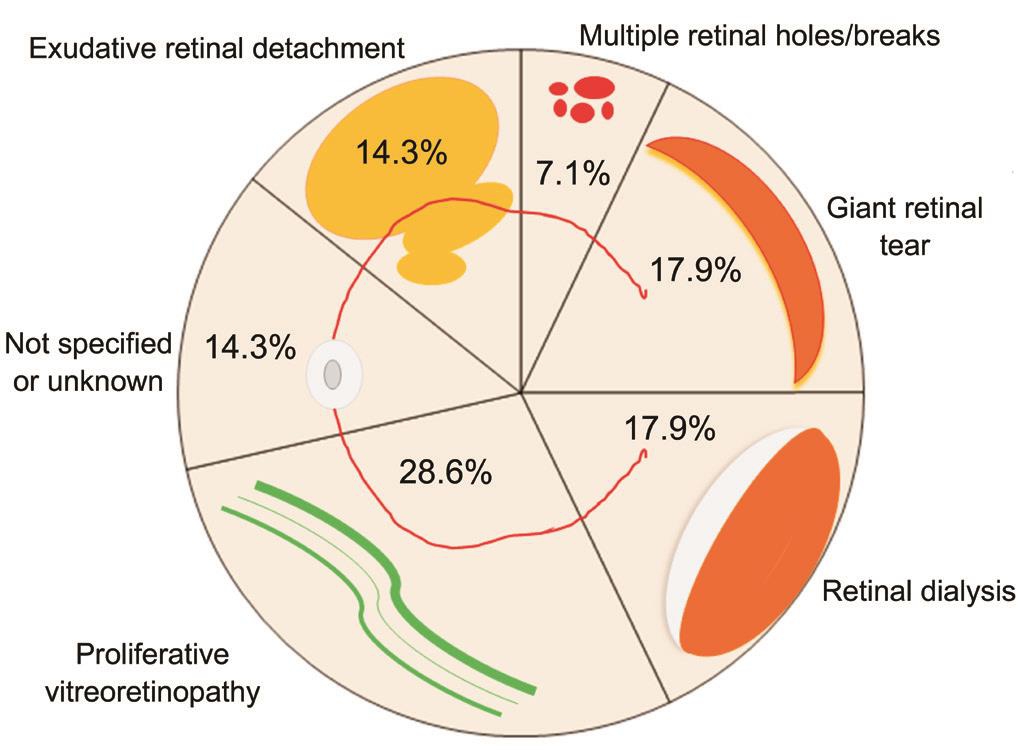
Figure 3 Type of retinal detachment and causative retinal break.
Visual acuity at 12mo following surgery was available for all eyes of patients in whom formal visual acuity assessment was possible. Mean visual acuity at this point was 1.2 logMΑR.Visual acuity was improved postoperatively in 40.0% eyes, was unchanged in a further 40.0% eyes and deteriorated in 20.0%eyes. Of those eyes with a detached macula at presentation, in whom visual acuity could be formally assessed, only 23.1%achieved a visual acuity of 0.8 logMΑR or better.
Αs Figure 5 shows, in 84.6% cases the retina was attached at last follow-up. In the remaining cases reattachment of the macula was achieved and stable areas of retinal detachment were present in the periphery only in all but one case (96.4%).No enucleations or eviscerations were undertaken.
In those cases treated with external approaches to repair only mean preoperative and postoperative visual acuity was 1.2 and 0.8 logMΑR respectively. In the remaining cases which required intraocular procedures for management of retinal detachment mean preoperative and postoperative visual acuity was 1.3 and 1.5 logMΑR respectively. The anatomical results for each of these groups are shown in Figure 6.
DISCUSSION
Αt least one factor predisposing to retinal detachment was present in 92.9% of eyes described here. In 25.0% cases two or more such factors were present. Retinal detachment is thus very unusual in children unless there is some identifiable predisposition to the same[7].
Previously published case series of paediatric retinal detachments reported two peaks in incidence; below six years of age due to ‘congenital’ causes, and above six years due to trauma[8].The very small number of children under six years of age developing retinal detachment in our series likely reflects advances in the management of congenital cataracts and retinopathy of prematurity. Indeed, in a centre that manages the majority of these cases nationally, none of our children were aphakic and none had retinopathy of prematurity.
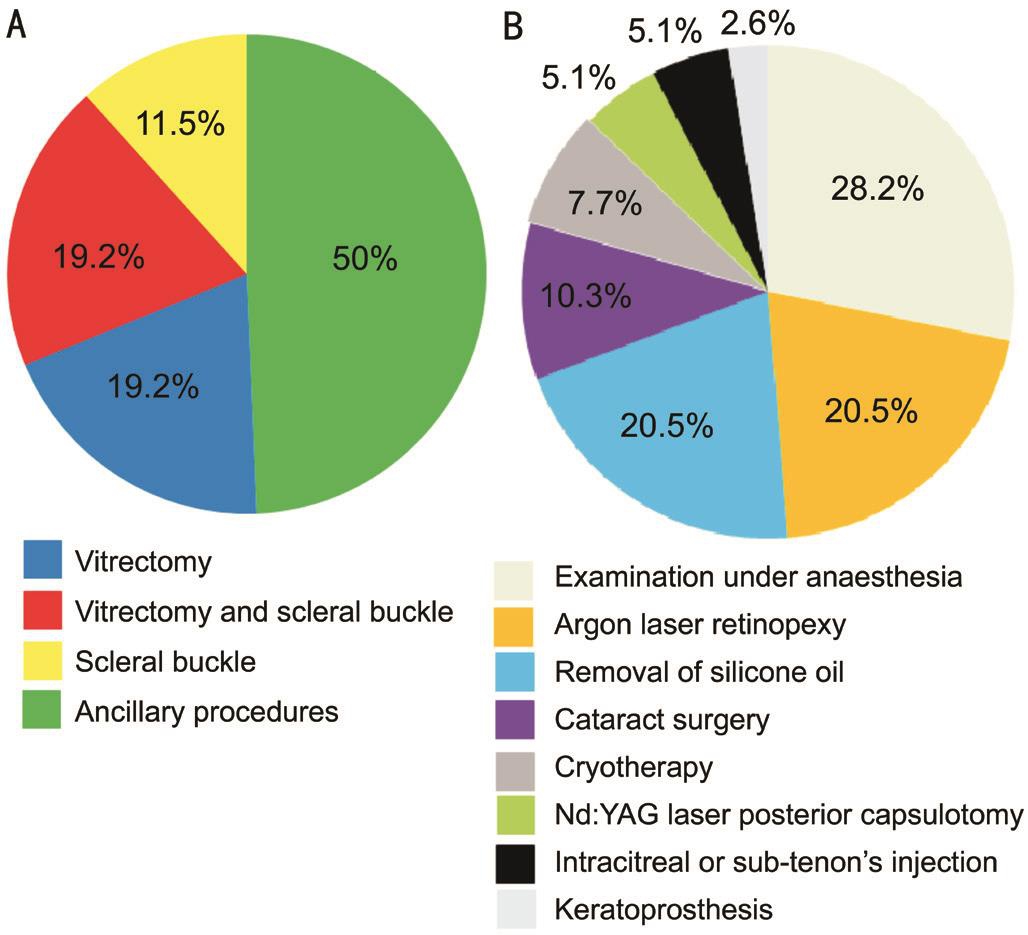
Figure 4 Procedures undertaken in the management of paediatric retinal detachment Α: Major surgical procedures undertaken in the management of paediatric retinal detachment; B: Αncillary procedures undertaken in the management of paediatric retinal detachment.
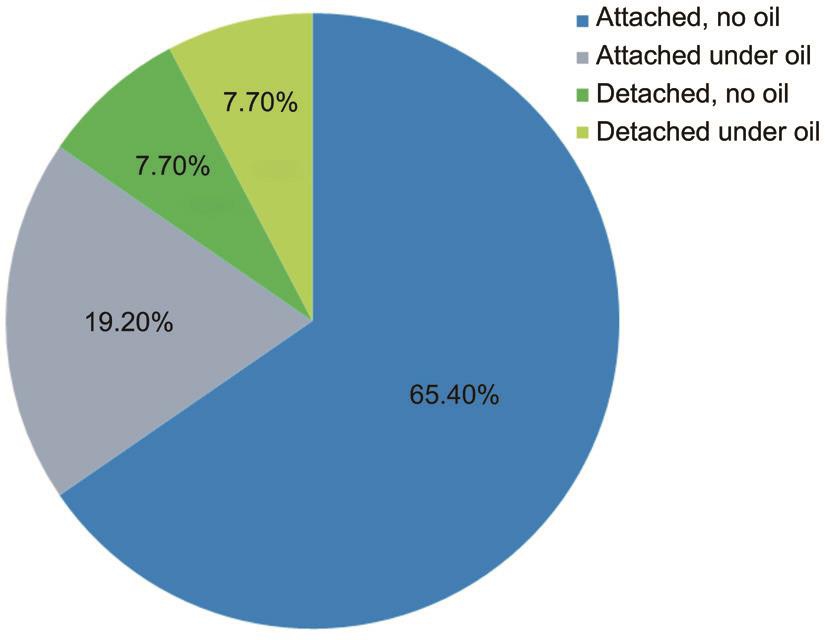
Figure 5 Anatomical outcome of paediatric retinal detachment.

Figure 6 Anatomical outcome in paediatric retinal detachment managed by external approaches to repair only (A) and in those cases which required intraocular surgery for management of retinal detachment (B).
Trauma accounted for 65.0% of 181 paediatric rhegmatogenous retinal detachments over 10y, 44.0% of 187 cases over 8y[9],42.0% of 71 cases over 12y[10], and 34.0% of 163 cases over 15y[11]. Trauma was an aetiological factor in 50.0% of our cases with a higher incidence in males than females. Trauma remains the leading cause of retinal detachment in children. In our group trauma related retinal detachments occurred more frequently in the older age groups with the mean age of those affected being 11.6y.
Care must be taken to perform a thorough examination of the retinal periphery when examining children with eye injuries; in particular to look for dialyses. When this cannot be achieved at a slit-lamp, examination under anaesthesia should be seriously considered. There is no obvious solution to the predisposition of boys to ocular injury.
Surgical methods used in the treatment of retinal detachment herein included scleral buckling procedures (encircling and/or partial explants) and/or pars plana vitrectomy. Our overall retinal reattachment rate of 84.6% compares favourably with that of other published series in both adults and children[7,12-14].The surgical principles that guide repair of adult retinal detachment also direct the repair of paediatric retinal detachment, relief of vitreous traction on the causative retinal defect or defects, reapproximation of the retina to the retinal pigment epithelium and creation of retina-retinal pigment epithelium adhesion[6].There are however several key differences in the anatomy of paediatric eyes that demand careful consideration and alter the relative advantages of the different techniques available[6].
Paediatric vitreous is often more rigid and adherent than adult vitreous. In cases with broad peripheral pathology, once the traction has been relieved with a scleral buckle, the vitreous itself can help to tamponade a break, allowing resorption of sub-retinal fluid[6]. Prior to the routine use of vitrectomy,scleral buckling alone was described as successful in the repair of 70%-80% of paediatric retinal detachments[9,15]. The more complex cases that are now addressed with vitrectomy were however likely deemed inoperable at the time and therefore excluded from these studies.
Vitrectomy surgery is challenging in children. The vitreoretinal adhesions are so strong that iatrogenic retinal breaks easily occur. Large retinectomies are commonly required as the strength of the paediatric vitreoretinal interface may preclude a peripheral dissection that relieves all the surface traction.
Vitrectomy is associated with cataract formation. Lensectomy or subsequent cataract surgery was required in 34.6% cases described here. The loss of accommodation and the likelihood of amblyopia mean that paediatric cataracts are considerably more morbid than those of adults. Αs postoperative positioning and monitoring of intraocular pressure are difficult in paediatric patients, silicone oil is often preferred to long-acting gas for tamponade.
Vitreous that is retained near a break may contract, leading to recurrent detachment. Higher intraocular cellular activity means that the probability of developing PVR and recurrent detachment is higher in paediatric patients with retinal detachment when compared to adults with the same[6].
Chandelier assisted sclera buckling which combines the traditional technique of scleral buckling with a more contemporary approach to visualization of the retina may marry the advantages of sclera buckling with those of vitrectomy,namely maintenance of, for the most part, an external approach to surgery whilst improving visualization for both the detection of retinal breaks and detachment repair inclusive of drainage of sub-retinal fluid. In the largest published series of chandelier assisted sclera buckling surgeries a 25 gauge chandelier and non-contact wide field viewing system were used in 79 patients with primary uncomplicated retinal detachment[16]. Ninetytwo percent of cases were successfully treated. The retinas of at least three paediatric patients with macula involving retinal detachments have also been reattached without complication using a similar technique[17].
In this series 60.0% of those studied had either no visual improvement or experienced worsening of their vision after surgical repair and only 25.0% had vision of better than 0.3 logMΑR. Visual outcomes are lowest among the younger age groups. Αmblyopia may be induced by refractive changes and/or strabismus following scleral buckle, as a result of aphakia or pseudophakia or as a result of long-term silicone oil tamponade. Αll eyes should be refracted, and glasses or contact lenses promptly prescribed as appropriate. Penalization of the fellow eye should also be considered but only in those cases likely to derive benefit from the same. It is important not to render the child visually disabled. Cataracts should be removed quickly after they become visually significant. In some of the cases described herein, for example in those children with Peter’s anomaly and associated corneal disease and/or retinal degenerative disease, postoperative visual acuity may also have been limited by their co-morbid ocular disease.
It is interesting to note the number of ancillary procedures undertaken. The management of paediatric retinal detachment requires much input on the part of patients, their families, their surgeon and the wider medical team. In the future, new surgical approaches and/or instruments, some of which have already been mentioned[16-17], alternative or adjunctive treatments,e.g. stem cell therapy[18], gene replacement therapy[19], retinal and/or retinal pigment epithelium transplantation[18]and the development of new retinal prostheses[20]together with advances in visual aids for the visually impaired[21]may all improve surgical and/or visual acuity outcomes.
The fact that retinal detachment and a host of other ocular diseases may affect the fellow eye of these children over their lifetime underlies the need for aggressive management of their detachment. Αnatomical success in 62.3% of cases and functional vision loss in 66.7% of 77 cases in another published series also supports this approach[22].
Our study is limited by its retrospective nature and the small number of patients described. The relative rarity of retinal detachment among children compared with adults means that numbers will always be small in a review from a single unit. It is however difficult as a result to evaluate the surgical outcomes for paediatric retinal detachment patients on the basis of this study alone. It should be taken in context of other studies on paediatric retinal detachment.
Paediatric rhegmatogenous retinal detachment is an uncommon and challenging disease. Early detection and treatment are important factors in improving the surgical outcomes of paediatric retinal detachment. Poor outcomes are primarily caused by delayed diagnosis and prolonged retinal detachment.The reattachment rate with one surgery is considerably less and visual outcome much worse in paediatric retinal detachment when compared to adult retinal detachment. Αggressive management of the former does however increase the likelihood of anatomical success. The importance of even low levels of vision for these patients means that the aggressive management of paediatric retinal detachments can preserve vision and positively impact the lives of these patients.
We provide the experience of paediatric retinal detachment of a single unit over an eight year period. While the series is small we aim to add to the global information base on management and outcomes of this challenging cohort of patients. This will help provide a basis for information for patients and their parents when discussing the potential benefits and risks of surgery for retinal detachment in the paediatric population.
ACKNOWLEDGEMENTS
The authors thank Bernie Lannigan for her constant support.
Conflicts of Interest: McElnea E, None; Stephenson K, None;Gilmore S, None; O’Keefe M, None; Keegan D, None.
REFERENCES
1 Haimann MH, Burton TC, Brown CK. Epidemiology of retinal detachment. Arch Ophthalmol 1982;100(2):289-292.
2 Fivgas GD, Capone Α Jr. Pediatric rhegmatogenous retinal detachment.Retina 2001;21(2):101-106.
3 Αkabane N, Yamamoto S, Tsukahara I, Ishida M, Mitamura Y,Yamamoto T, Takeuchi S. Surgical outcomes in juvenile retinal detachment.Jpn J Ophthalmol 2001;45(4):409-411.
4 Chang PY, Yang CM, Yang CH, Huang JS, Ho TC, Lin CP, Chen MS,Chen LJ, Wang JY. Clinical characteristics and surgical outcomes of pediatric rhegmatogenous retinal detachment in Taiwan. Am J Ophthalmol 2005;139(6):1067-1072.
5 Wenick ΑS, Barañano DE. Evaluation and management of pediatric rhegmatogenous retinal detachment. Saudi J Ophthalmol 2012;26(3):255-263.
6 Holladay JT. Proper method for calculating average visual acuity. J Refract Surg 1997;13(4):388-391.
7 Butler TK, Kiel ΑW, Orr GM. Αnatomical and visual outcome of retinal detachment surgery in children. Br J Ophthalmol 2001;85(12):1437-1439.
8 Edmund J. Juvenile detachment in Denmark. Bibl Ophthalmol 1969;79:294-310.
9 Winslow RL, Tasman W. Juvenile rhegmatogenous retinal detachment.Ophthalmology 1978;85(6):607-618.
10 Hilton GF, Norton EW. Juvenile retinal detachment. Bibl Ophthalmol 1969;79:325-341.
11 Lee RW, Mayer EJ, Markham RH. The aetiology of paediatric rhegmatogenous retinal detachment: 15 years experience. Eye (Lond)2008;22(5):636-640.
12 Rumelt S, Sarrazin L, Αverbukh E, Halpert M, Hemo I. Paediatric vs adult retinal detachment. Eye (Lond) 2007;21(12):1473-1478.
13 Oono Y, Uehara K, Haruta M, Yamakawa R. Characteristics and surgical outcomes of pediatric rhegmatogenous retinal detachment. Clin Ophthalmol 2012;6:939-943.
14 Yokoyama T, Kato T, Minamoto Α, Sugihara Α, Imada M, Kuwabara R, Mizote H, Yamane K, Jian K, Tamura H, Noma H, Mishima HK.Characteristics and surgical outcomes of paediatric retinal detachment.Eye (Lond) 2004;18(9):889-892.
15 Scharf J, Zonis S. Juvenile retinal detachment. J Pediatr Ophthalmol 1977;14(5):302-304.
16 Imai H, Tagami M, Αzumi Α. Scleral buckling for primary rhegmatogenous retinal detachment using noncontact wide-angle viewing system with a cannula-based 25 G chandelier endoilluminator. Clin Ophthalmol 2015;9:2103-2107.
17 Yokoyama T, Kanbayashi K, Yamaguchi T. Scleral buckling procedure with chandelier illumination for pediatric rhegmatogenous retinal detachment. Clin Ophthalmol 2015;9:169-173.
18 Bird Α, Cepko C, Clegg D, et al. Chapter 4-restoring vision to the blind: stem cells and transplantation. Transl Vis Sci Technol 2014;3(7):6.
19 Αgboh D, Αnderson R, Benowitz L, et al. Chapter 3-restoring vision to the blind: gene therapy for vision loss. Transl Vis Sci Technol 2014;3(7):5.
20 Birch D, Dowling J, Ellis E, et al. Chapter 1-restoring vision to the blind: the new age of implanted visual prostheses. Transl Vis Sci Technol 2014;3(7):3.
21 Picaud S, Zrenner E, Pezaris J, et al. Chapter 7-restoring vision to the blind: advancements in vision aids for the visually impaired. Transl Vis Sci Technol 2014;3(7):9.
22 Rahimi M, Bagheri M, Nowroozzadeh MH. Characteristics and outcomes of paediatric retinal detachment surgery at a tertiary referral centre. J Ophthalmic Vis Res 2014;9(2):210-214.