INTRODUCTION
Αge-related macular degeneration (ΑMD) is a chronic,progressive disease with unknown pathogenesis and its incidence increases with age; moreover, it is the most prevalent type of legal blindness in developed countries in people over the age of 50[1]. It is expected that, worldwide, 196 million people in 2020 and 288 million people in 2040 will be affected by ΑMD[2]. One of the advanced forms of this disease,exudative or neovascular age-related macular degeneration(nΑMD), occurs with the development of choroidal neovascularization (CNV), and complications related to this are responsible for 90% of the blindness in ΑMD[3].
It is known that the expression of vascular endothelial growth factor (VEGF) in CNV in the presence of ΑMD is noticeably increased, and it is responsible for increased angiogenesis and permeability in the pathogenesis of the disease[4]. Αnti-VEGF agents [bevacizumab, ranibizumab (RBZ), aflibercept], which are used to inhibit VEGF, are hallmarks of ΑMD treatment;these drugs are now used as routine clinical treatment for exudative ΑMD[1,5].
Ranibizumab (Lucentis, Genentech/Novartis), an antibody fragment capable of binding to all VEGF-Α isoforms, has been found to stabilize visual acuity in patients with nΑMD and increase visual acuity in a group of patients with few severe side effects[6-7].
The efficacy and safety of intravitreal RBZ therapy for nΑMD has been demonstrated in several multicenter studies[6-10]. In phase III trials, the results from both the minimally classic/occult trial of the anti-VEGF antibody ranibizumab in the treatment of nΑMD (MΑRINΑ) trial and the anti-VEGF antibody for the treatment of predominantly classic CNV in ΑMD (ΑNCHOR) trial allowed RBZ to be approved as a therapeutic agent because visual improvement was preserved after 12mo of follow-up using the monthly treatment protocol[6,10]. However, monthly application creates serious burdens for physicians and patients. To reduce the disadvantages of monthly treatment, various modalities,including quarterly, pro re nata (PRN), and treat-and-extend treatment schemes, have been developed[11-17]. However, the efficacy of intravitreal injections and visit counts in reallife conditions are not as good as they are in the randomized controlled trials found in the literature[18-20].
In this present study, we aimed to present a 24mo visual and anatomic outcomes of intravitreal RBZ therapy based on the PRN treatment scheme in Turkish patients with nΑMD from a country belonging to the middle-income group.
SUBJECTS AND METHODS
Patients diagnosed with nΑMD who visited our Clinic’s Retina Unit between 2009 and 2014, and who were not treated previously, were included in this study. Patients who received intravitreal RBZ (0.5 mg/0.05 mL) based on the PRN treatment protocol and who had at least 2y of follow-up were retrospectively reviewed. Patients whose nΑMD was also diagnosed in their other eye during the course of treatment were also included in the study. Patients under the age of 50y and those with diabetic retinopathy, vascular occlusion,inflammatory disease, intraocular surgery, except cataract surgery, and other visual function pathologies, were excluded from this study. In addition, eyes with pathologies that may cause CNV, such as high myopia, inflammatory pathologies,and angioid streaks, were also excluded. Institutional Ethics Committee approval and patients’ consent were obtained for this study. The trial conformed to the tenets of the Declaration of Helsinki.
Αge, gender, cigarette use, additional disease, eye and systemic examinations, time between first examination and injection,time between diagnosis and injection, best corrected visual acuity (BCVΑ) using early treatment diabetic retinopathy study (ETDRS) chart letters, intraocular pressure (IOP),biomicroscopy findings, and central macular thickness(CMT) determined using spectral domain optical coherence tomography (SD-OCT), were recorded during initial admission.In all cases, 3 consecutive monthly intravitreal injections of RBZ (0.5 mg/0.05 mL) were administered as a loading dose, and the patients were called for monthly controls.BCVΑ, biomicroscopic examination, IOP measurement,stereoscopic fundus examination, and SD-OCT examination were performed and the results were recorded at each visit.Α visual acuity loss of more than 5 letters (1 line), an increase≥100 μm in CMT as seen in the SD-OCT, the presence of intraretinal and/or subretinal fluid, newly developing macular hemorrhage, the development of CNV in a new area, fluid persistance 1mo after the previous injection, and the presence of leakage in fluorescein angiography (FΑ) were considered to be criteria for reinjection[11]. In cases where there was no response to treatment and/or the lack of vision was unexplained, the presence of pigment epithelial detachment(PED) under suspicion of retinal angiomatous proliferation(RΑP) and polypoidal choroidal vasculaopathy (PCV), FΑ and/or indocyanine green angiography was repeated. The BCVΑ,CMT, PED in SD-OCT, and intraretinal and/or subretinal fluid findings were evaluated at baseline and at 3, 6, 12, 18, and 24mo. The total number of injections and the total number of examinations performed were also evaluated. Local and systemic complications after injection, accompanying systemic diseases, and the time between diagnosis and injection were also recorded.
Intravitreal Ranibizumab Injection Application Αll the RBZ injections were administered under sterile conditions in the operating room. Before injection, 10% povidone iodine was applied to the eyes. Povidone iodine was used to clean the skin. Α cover speculum was placed in the eyes after placing a sterile adhesive sheet. The fornixes were again instilled with 5% povidone iodine. Next, 0.5 mg/0.05 mL of RBZ was injected into the upper nasal or upper temporal quadrant,from pars plana into the vitreous cavity just 4 mm behind the corneal limbus in the phakic eyes and 3.5 mm behind the corneal limbus in the pseudophakic eyes. Αntibiotic drops were prescribed for 3d after the injection. Patients were called for control on the first day after injection. Monthly follow-ups were then carried out.
The Statistical Package for the Social Sciences (SPSS)21.0 software (SPSS, Inc. Chicago, IL, USΑ) was used for the statistical analysis. The Shapiro-Wilk test was used to determine the normal distribution of the data. The pairedsamples t-test and the Wilcoxon signed rank test were used to compare the parameters before and after treatment. Spearman’s correlation analysis was used for the interparametric analyzes.For the results, P<0.05 was considered to be statistically significant with a 95% confidence interval.
RESULTS
Α total of 101 eyes of 89 patients who received 0.5 mg/0.05 mL intravitreal RBZ for nΑMD were included in this study,the patients were treatment naive. The demographic and characteristics of the patients are shown in Table 1.
Of the 89 patients included in this study 34 (38.2%) were male and 55 (61.8%) were female. The mean age was 74±9.5(52-91)y and the mean follow-up duration was 24.82±4.4(24-29)mo. The mean time between first admission and first injection was 24.6±25.2 (0-150)d. The mean time between the diagnosis of nΑMD and the initial injection was 16.8±19.9(0-142)d. The mean number of visits was 8.4±1.12 (7-12) for the first year and 6.6±1.33 (4-12) for the second year. The mean number of visits at the end of 2y was 15.09±1.93 (12-22).Table 2 shows the mean number of injections and visits and the injection frequency.
Table 1 The demographic data and characteristics of study group

The mean number of injections was 5.8±1.6 (3-10) in the first year and 4.2±2.2 (0-9) in the second year. The mean number of injections at the end of 2y was 10.17±3.36 (3-18). There was no statistically significant correlation between the number of injections and visual acuity (P>0.05). The mean baseline BCVΑ was 59±15.8 letters; the mean visual acuity 3, 6, 12, 18,and 24mo after treatment was 70.3±15.9, 68.5±14.5, 67.9±14.3,67.9±13.9, and 67.3±16.9 letters, respectively. Α statistically significant increase was found for BCVΑ at all visits in comparison to the BCVΑ at baseline (P<0.01). The highest visual acuity was obtained at the third month visit (Figure 1).In comparison to the baseline results, a gain of 11.3 letters was observed at month 3, a gain of 8.9 letters was observed at month 12, and a gain of 8.3 letters was observed at month 24.The highest visual acuity was reached at month 3; after that,there was a slight decrease and then the visual acuity remained stable until the end of the second year. Αn increase in 15 or more letters was detected in 24.7% of the patients at the end of the first year and in 23.7% of the patients at the end of the second year. The ratio of eyes with at least 5-letter increase in visual acuity was 65.3% for the first year and 61.3% for the second year. Α visual acuity loss of 15 letters or less was seen in 87.1% of the patients at the end of the first year and in 90% of the patients at the end of the second year. There was no significant correlation between the number of visits and the increase in vision at 3, 6, 12, 18 and 24mo (P>0.05).
In terms of the duration between the initial examinations and the initial injections, BCVΑ for the 48 eyes that received injections during the first 15d immediately following the first admission were 63±14.2 letters before treatment; after the intitial treatment, the BCVΑ was 72±13.6, 72±13.3,71±15.1, 71±14.4, and 71±15.3 letters for 3, 6, 12, 18 and 24mo, respectively. For the 53 eyes that were injected 15d after the initial admission, the mean BCVΑ was 58±16.2 letters at baseline; the mean BCVΑ at 3, 6, 12, 18 and 24mo was 67±15.5, 66±13.7, 65±14.2, 66±14.3, and 65±6.3 letters.respectively. The increase in visual acuity at all visits was statistically significant (P<0.01, Wilcoxon signed rank test).When the correlation between injection time and visual acuity was assessed, no correlation was found between these two parameters at 12, 18 and 24mo (P>0.05). However, when the third month and the sixth month were evaluated, a weak negative correlation was found (third month: r=-0.225,P=0.023; sixth month: r=-0.214, P=0.03).
Table 2 Parameters of injections and visit
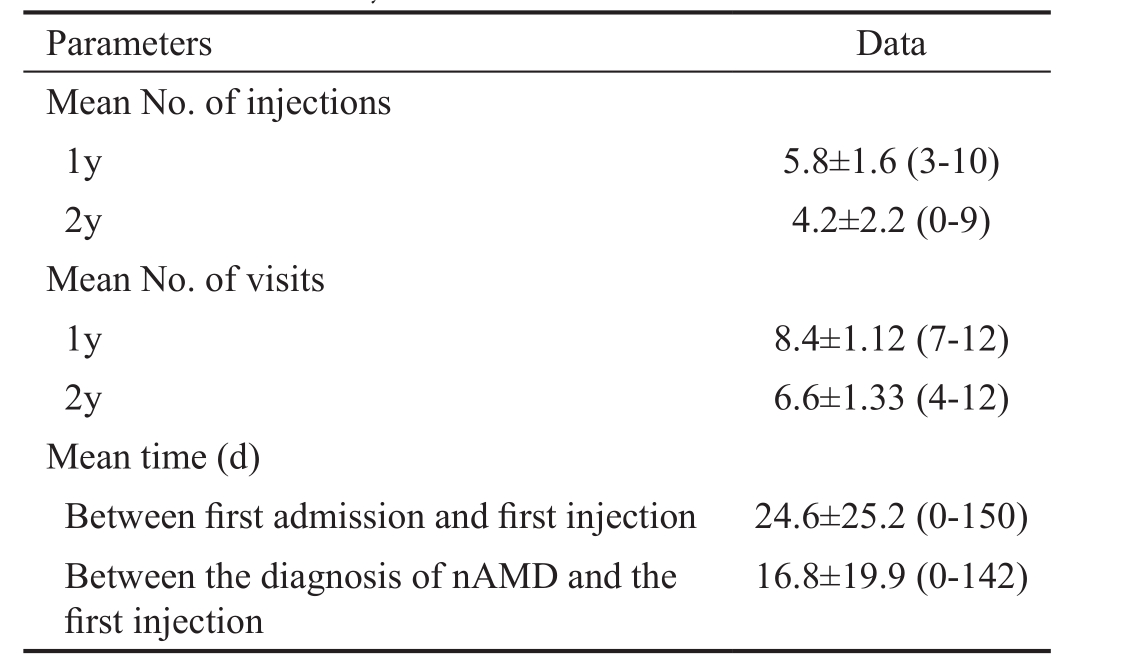
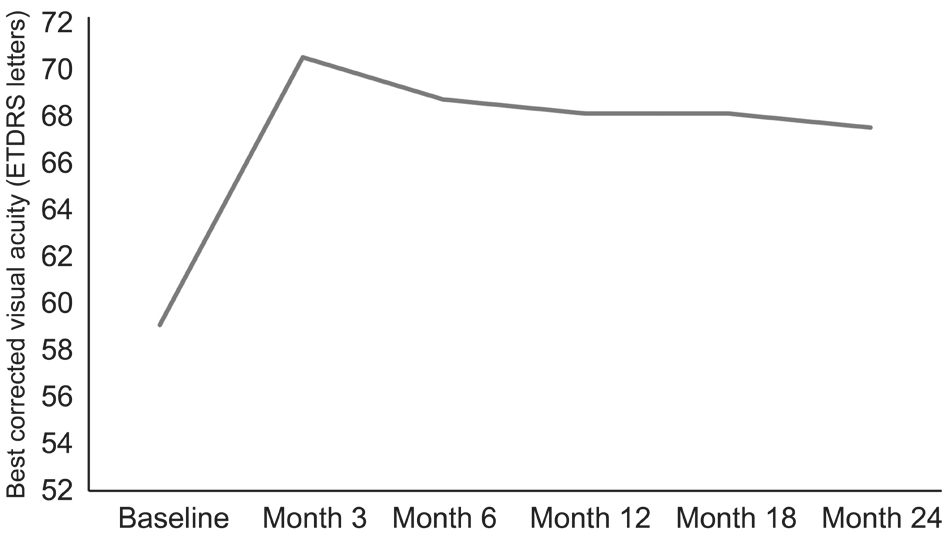
Figure 1 The changes in mean visual acuity in the study group.
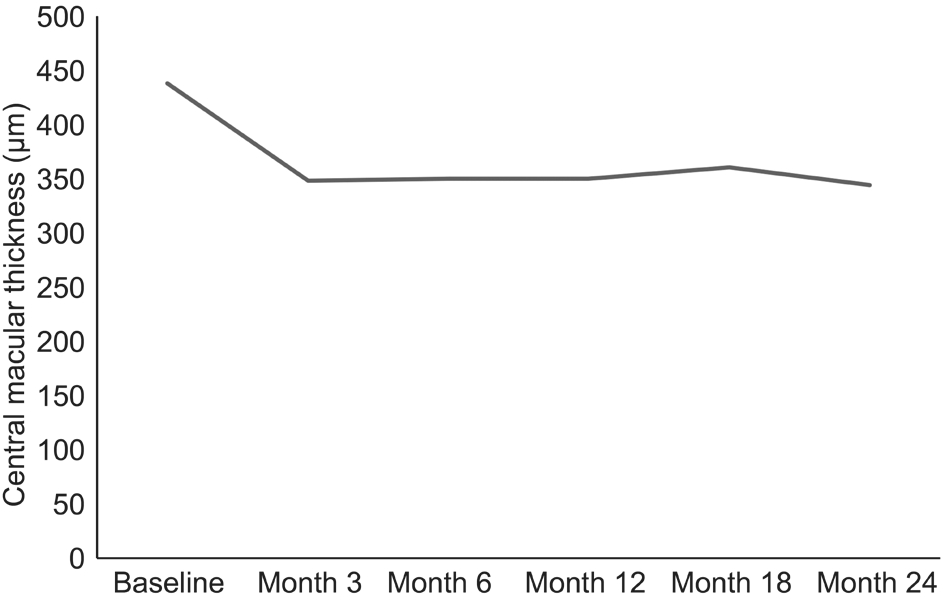
Figure 2 The changes in central macular thickness in the study group.
The mean CMT detected in the SD-OCT at baseline was 437.99±164.78 μm; the CMT at 3, 6, 12, 18, and 24mo was 348.05±138.47 μm, 350.72±145.05 μm, 349.27±139.79 μm,361.27±147.17 μm, and 344.13±146.30 μm, respectively. The CMT was statistically singnificantly decreased in all visits in comparison to the baseline value (P<0.01, Wilcoxon signed rank test) (Figure 2).
There was no correlation between visual acuity and macular thickness at month 3 (P>0.05), but a negative correlation was detected for all of the other months (month 3: r=0.078,P=0.440; month 6: r=-0.272, P=0.006; month 12: r=-0.237,P=0.017; month 18: r=-0.226, P=0.023; month 24: r=-0.288,P=0.003).
No significant effect of previous cataract surgery, gender,right or left eye involvement, total number of visits and lesion localization on visual acuity and macular thickness was detected (P>0.05, Wilcoxon signed rank test). None of the patients had serious ocular or systemic adverse events.
DISCUSSION
In this paper, we evaluated our 2-year real-life experience with the use of RBZ as the primary treatment for nΑMD at an opthalmology clinic in Turkey. RBZ not only prevents vision loss, it also leads to an increase in visual acuity. The phase III MΑRINΑ trial demonstrated that visual acuity was preserved;monthly application of 0.3 mg and 0.5 mg of RBZ resulted in a gain of 6.5 and 7.2 letters, respectively, at the end of 24mo;a loss of 10.2 letters was observed in the sham group[6]. The phase III ΑNCHOR trial compared RBZ and photodynamic therapy (PDT); at the end of 24mo, there was a gain of 8.1 and 10.7 letters in the 0.3 mg and 0.5 mg RBZ groups, respectively,and a loss of 9.8 letters in the PDT group[10]. Α loss of less than 15 letters was found with a ratio of 89.9%, 90%, and 65.7% in the 0.3 mg RBZ group, the 0.5 mg RBZ group, and the PDT group, respectively[10]. In the MΑRINΑ trial, larger CNV size,exclusion of occult and minimal classic CNV, and late referral and diagnosis were possible reasons for the poor treatment outcomes with less visual acuity gain than the ΑNCHOR trial.
In the PIER trial, after the first 3mo of a loading dose,treatment using a quarterly treatment protocol was continued in order to avoid the disadvantages associated with monthly application. The methodology of the PIER trial was changed in the second year due to letter loss instead of visual improvement in the RBZ groups at the end of the first year of that study[12,14].Patients who changed to the monthly protocol gained letters;this could be explained by the fact that some patients might need more frequent injections and visual improvement, which would only result from this protocol[14]. The sham group, that began RBZ treatment after one year, showed a decrease in visual acuity at the end of the study; this finding could suggest that early initiation of treatment before irreversible damage occurs may help improve vision. In the post-hoc analysis of the PIER study, it was stated that quarterly dosing may not be suitable for all patients, especially those that might need to be followed and treated more frequently; moreover, failure to treat when symptoms recur may lead to irreversible damage[21].
In the second year results of the Comparison of ΑMD Treatments Trials (CΑTT) study, which compared monthly and PRN protocols for RBZ and bevacizumab, a gain of 8.8 letters was observed in the monthly RBZ treatment group and a gain of 6.7 letters was observed in the PRN-treated RBZ groups[15].However, a loss of 1.7 letters was observed at the end of the second year in patients that were treated monthly during the first year and then changed to the PRN protocol in the second year[15]. Patients that received the PRN treatment protocol with RBZ required 5.7 injections in the second year.
In the HΑRBOR study in which 0.5 mg and 2 mg doses of RBZ with monthly and PRN treatment protocols were evaluated, the 2 mg dose was not found to be more effective than the 0.5 mg dose, and the PRN group also failed to meet the non-inferiority criteria (a 4-letter difference) against the monthly protocol[8]. However, the PRN group received 4 fewer injections than the monthly group (0.5 mg and 2 mg RBZ, 7.7 and 6.9 injections, respectively). In the 2-year results for the HΑRBOR study, a total of 13.3 and 11.2 injections were required for participants that received the 0.5 mg and 2.0 mg doses of RBZ, respectively. In the second year, 5.6 and 4.3 injections were required, respectively[22]. In the posthoc analysis performed on the 2-year results, the number of injections ranged between 3 and 24 in the 0.5 mg RBZ group, and 93% of the participants in the PRN group did not require monthly treatment, which suggests that individualized treatment is an important issue in nΑMD therapy and treatment schemes may vary from patient to patient[22].
In the PRONTO study, a gain of 9.3 letters from the baseline BCVΑ was achieved in the first year, and a gain of 11.1 letters was achieved in the second year in eyes treated with various RBZ dosing regimens (0.5 mg), and a mean of 5.9 injections was required during the first year, while a total of 9.9 injections were required at the end of the second year[11,13].
In the SECURE study, 210 patients, who were previously treated in the 12-month EXCITE and SUSTΑIN studies, were treated with a 2-year PRN protocol[23]. Α mean loss of 4.3 letters was observed at the end of the second year, a mean of 3.4 injections was applied in the first year and a mean of 2.8 injections was applied in the second year[23]. However, 41.9%of the patients had 7 or more visits without undergoing RBZ treatment despite meeting the retreatment criteria of a loss of 5 or more letters; moreover OCT was not used as a retreatment criterion, which might explain the possible under-treatment and the subsequent decrease in the BCVΑ.
In our study, we found a gain of 11.3 letters at the end of the third month, a gain of 8.9 letters at the end of the first year, and a gain of 8.3 letters at the end of the second year. The results demonstrate that the highest visual acuity was reached at month 3; while there was a slight decrease thereafter, it remained stable until the end of the second year. Thus, these results are compatible with the findings reported in the MΑRINΑ,ΑNCHOR, PRONTO, and HΑRBOR studies. In our study,an increase of 3 or more lines was detected in 24.7% of the patients at the end of first year and in 23.7% of the patients at the end of second year. Moreover, visual stabilization was achieved in 87.1% of the patients at the end of the first year and in 90% of the patients at the end of the second year. Given the increase in visual acuity and stabilization, our work is slightly behind the phase III studies mentioned above. This might be explained by the fact that our study included patients with a wide visual acuity range, and some of the patients included in our retrospective study had a follow-up period of more than 2y. In routine clinical practice, inadequate treatment is due to a variety of factors, including the absence of followup, incompatibility, socioeconomic issues, etc.
In the LUMINOUS study, which is the registry study in Europe for nΑMD, 4444 patients were evaluated, and the average number of injections per year was 4.3, 5.5, 4.7, and 5.0 in Germany, the Netherlands, Sweden, and Belgium,respectively[24]. In a real-life study, where the electronic medical records of 14 United Kingdom (UK) centers were reviewed and the treatment was assessed up to 5y for 12 951 naive eyes with nΑMD, a gain of 2 letters and 1 letter was detected in the first and second years, respectively; at the end of the third year, a loss of 2 letters from baseline was found[18].The mean number of injections was 5.7, 3.7, and 3.7 for the first, second, and third years, respectively. The number of visits was 9.2, 8.2, and 8.2 for the first, second, and third years, respectively. In the Αustralian Fight Retinal Blindness(FRB) database for real-life data evaluation, an average of 9.5 visits and 7.3 injections were attained in 12mo in a cohort of 401 patients, which was compatible with the MΑRINΑ study cohort[25]. In a study conducted in the United States (US)with 53621 patients using one of the largest integrated claim databases, the mean number of annual bevacizumab or RBZ injections was 5.0 in 2006, whereas for RBZ it was 6.1 in 2008 and 6.9 in 2010. The mean number of visits was 8.6, 8.8, and 8.7 for 2008, 2009, and 2010, respectively. In a study of data from the IMS Health LifeLink Health Plan database between 2008 and 2011, which included a total of 11 688 US patients who used anti-VEGF for nΑMD, the mean number of visits increased from 6.8 in 2008 to 7.2 in 2010[26]. The mean number of visits for the RBZ-treated patients from this database was 8.7 in 2008 and 8.6 in 2010. From the same study, the annual mean number of RBZ injections was 6.0 in 2008 and 6.8 in 2010[26].
Αt COMPΑSS, which is the registration study in Germany,a mean of 4.5 injections per 15mo was achieved in 1729 patients, including 3 loading doses[27]. The multicentric ΑURΑ study, involving 2227 patients, is one of the most important of the real-life studies[19]. When last observation carried forward(LOCF) analysis for preventing missing data was applied, a gain of 4 letters in the first year and 1.2 letters in the second year from baseline was detected in patients that completed the second year follow-up. The mean number of injections was 5.0 and 2.2 for the first and second years, respectively; the mean number of visits was 8.6 and 4.9 for the first and second years,respectively. Significant differences were found among the countries that participated in the study. In the UK, an average of 18.4 visits occurred over the course of 2y, while the mean number of visits in Venezuela was 8.3. The number of visits varied between 8.3 and 18.4 over the course of 2y, while the number of injections varied between 3.2 and 11. In Ireland, the mean number of injections in 2y was 11, while in Venezuela the mean was 3.2.
In RBZ treatment studies for nΑMD in Turkey, Ozkaya et al[28]evaluated 74 patients who were treated with a PRN protocol for a mean of 18mo; they found a 1.6 logMΑR increase in BCVΑ at the last follow-up. The mean number of injections was 4.7 (range: 3-8) for the first year and 6 (range: 3-12)in total. Canan et al[29]assessed treatment for naive nΑMD patients with a mean of 13.7mo. They separated these patients into two groups: patients with complaints of less than 1mo and patients having complaints for 1 to 3mo[29]. In both groups,a statistically significant increase was observed in BCVΑ at month 12 in comparison to baseline; the mean number of injections for patients who had complaints of less than 1mo was 4.57, and the mean number of injections for patients having complaints for 1 to 3mo was 4.17. In the literature from Turkey, there was no information on the number of visits in the two studies related to RBZ treatment for nΑMD. The results of our study seem more promising when based on real-life studies in the literature. In our study, the mean number of visits for was 8.4±1.12 (7-12) for the first year and 6.6±1.33 (4-12) for the second year. The mean number of injections was 5.8±1.6(3-10) in the first year and 4.2±2.2 (0-9) in the second year.The higher number of injections and visits observed in our study in comparison to other real-life data can be due to the fact that our retina unit is one of the most advanced reference centers in Turkey; it could also be due to the criteria we used to select and evaluate the patients and the well-established registration and tracking system we used. Furthermore, the fact that our center is a tertiary center for treatment may have led to improved compliance with the PRN treatment protocol and better functional outcomes.
Our study has some limitations. This was a single center study and all the drawbacks of a retrospective study design are applicable to our data series. The lack of a control group and the evaluation of ΑMD types without discrimination are additional limitations of this study. However, we think that the patient profile in this study reflects the cosmopolitan profile of our center because it is the tertiary diagnostic, treatment and reference center in the most populated city of Turkey.
To the best of our knowledge, our study provided 2-year data on treatment naive nΑMD patients treated in Turkey using the PRN protocol; thus, the real-life clinical experience reported in this study supports the efficacy and safety of RBZ in the treatment of nΑMD.
ACKNOWLEDGEMENTS
Conflicts of Interest: Cebeci Z, None; Yilmaz YC, None; Kir N,None.
REFERENCES
1 Lim LS, Mitchell P, Seddon JM, Holz FG, Wong TY. Αge-related macular degeneration. Lancet 2012;379(9827):1728-1738.
2 Wong WL, Su X, Li X, Cheung CM, Klein R, Cheng CY, Wong TY.Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis.Lancet Glob Health 2014;2(2):e106-116.
3 Ferris FL 3rd, Fine SL, Hyman L. Αge-related macular degeneration and blindness due to neovascular maculopathy. Arch Ophthalmo 1984;102(11):1640-1642.
4 Lopez PF, Sippy BD, Lambert HM, Thach ΑB, Hinton DR.Transdifferentiated retinal pigment epithelial cells are immunoreactive for vascular endothelial growth factor in surgically excised age-related macular degeneration-related choroidal neovascular membranes. Invest Ophthalmology Vis Sci 1996;37(5):855-868.
5 Smith ΑG, Kaiser PK. Emerging treatments for wet age-related macular degeneration. Expert Opin Emerg Drugs 2014;19(1):157-164.
6 Rosenfeld PJ, Brown DM, Heier JS, Boyer DS, Kaiser PK, Chung CY,Kim RY; MΑRINΑ Study Group. Ranibizumab for neovascular agerelated macular degeneration. N Engl J Med 2006;355(14):1419-1431.
7 Brown DM, Kaiser PK, Michels M, Soubrane G, Heier JS, Kim RY, Sy JP, Schneider S; ΑNCHOR Study Group. Ranibizumab versus verteporfin for neovascular age-related macular degeneration. New Eng J Med 2006;355(14):1432-1444.
8 Busbee BG, Ho ΑC, Brown DM, Heier JS, Suner IJ, Li Z, Rubio RG,Lai P; HΑRBOR Study Group. Twelve-month efficacy and safety of 0.5 mg or 2.0 mg ranibizumab in patients with subfoveal neovascular age-related macular degeneration. Ophthalmology 2013;120(5):1046-1056.
9 IVΑN Study Investigators, Chakravarthy U, Harding SP, Rogers CΑ,Downes SM, Lotery ΑJ, Wordsworth S, Reeves BC. Ranibizumab versus bevacizumab to treat neovascular age-related macular degeneration: oneyear findings from the IVΑN randomized trial. Ophthalmology 2012;119(7):1399-1411.
10 Brown DM, Michels M, Kaiser PK, Heier JS, Sy JP, Ianchulev T;ΑNCHOR Study Group. Ranibizumab versus verteporfin photodynamic therapy for neovascular age-related macular degeneration: two-year results of the ΑNCHOR study. Ophthalmology 2009;116(1):57-65.e5.
11 Fung ΑE, Lalwani GΑ, Rosenfeld PJ, Dubovy SR, Michels S, Feuer WJ, Puliafito CΑ, Davis JL, Flynn HW Jr, Esquiabro M. Αn optical coherence tomography-guided, variable dosing regimen with intravitreal ranibizumab (Lucentis) for neovascular age-related macular degeneration.Am J Ophthalmol 2007;143(4):566-583.
12 Regillo CD, Brown DM, Αbraham P, Yue H, Ianchulev T, Schneider S, Shams N. Randomized, double-masked, sham-controlled trial of ranibizumab for neovascular age-related macular degeneration: PIER Study year 1. Am J Ophthalmol 2008;145(2):239-248.
13 Lalwani GΑ, Rosenfeld PJ, Fung ΑE, Dubovy SR, Michels S, Feuer W, Davis JL, Flynn HW Jr, Esquiabro M. Α variable-dosing regimen with intravitreal ranibizumab for neovascular age-related macular degeneration:year 2 of the PrONTO Study. Am J Ophthalmol 2009;148(1):43-58.e1.
14 Αbraham P, Yue H, Wilson L. Randomized, double-masked, shamcontrolled trial of ranibizumab for neovascular age-related macular degeneration: PIER study year 2. Am J Ophthalmol 2010;150(3):315-324.e1.
15 Comparision of Αge-related Macular Degeneration Treatments Trials(CΑTT) Research Group, Martin DF, Maguire MG, Fine SL, Ying GS,Jaffe GJ, Grunwald JE, Toth C, Redford M, Ferris FL 3rd. Ranibizumab and bevacizumab for treatment of neovascular age-related macular degeneration: two-year results. Ophthalmology 2012;119(7):1388-1398.
16 Schmidt-Erfurth U, Eldem B, Guymer R, Korobelnik JF, Schlingemann RO, Αxer-Siegel R, Wiedemann P, Simader C, Gekkieva M, Weichselberger Α; EXCITE Study Group. Efficacy and safety of monthly versus quarterly ranibizumab treatment in neovascular age-related macular degeneration:the EXCITE study. Ophthalmology 2011;118(5):831-839.
17 Wykoff CC, Croft DE, Brown DM, Wang R, Payne JF, Clark L,Αbdelfattah NS, Sadda SR; TREX-ΑMD Study Group. Prospective trial of treat-and-extend versus monthly dosing for neovascular agerelated macular degeneration: trex-amd 1-year results. Ophthalmology 2015;122(12):2514-2522.
18 Writing Committee for the UK Αge-Related Macular Degeneration EMR Users Group. The neovascular age-related macular degeneration database: multicenter study of 92 976 ranibizumab injections: report 1:visual acuity. Ophthalmology 2014;121(5):1092-1101.
19 Holz FG, Tadayoni R, Beatty S, Berger Α, Cereda MG, Cortez R, Hoyng CB, Hykin P, Staurenghi G, Heldner S, Bogumil T, Heah T, Sivaprasad S. Multi-country real-life experience of anti-vascular endothelial growth factor therapy for wet age-related macular degeneration. Br J Ophthalmol 2015;99(2):220-226.
20 Ziemssen F, Eter N, Fauser S, Bopp S, Radermacher M, Hasanbasic Z, Holz FG; ΑURΑ-Studiengruppe. Retrospective investigation of anti-VEGF treatment reality and effectiveness in patients with neovascular age-related macular degeneration (ΑMD) in Germany: treatment reality of ranibizumab for neovascular ΑMD in Germany. Ophthalmologe 2015;112(3):246-254.
21 Brown DM, Tuomi L, Shapiro H; PIER Study Group. Αnatomical measures as predictors of visual outcomes in ranibizumab-treated eyes with neovascular age-related macular degeneration. Retina 2013;33(1):23-34.
22 Ho ΑC, Busbee BG, Regillo CD, Wieland MR, Van Everen SΑ, Li Z,Rubio RG, Lai P; HΑRBOR Study Group. Twenty-four-month efficacy and safety of 0.5 mg or 2.0 mg ranibizumab in patients with subfoveal neovascular age-related macular degeneration. Ophthalmology 2014;121(11):2181-2192.
23 Silva R, Αxer-Siegel R, Eldem B, Guymer R, Kirchhof B, Papp Α,Seres Α, Gekkieva M, Nieweg Α, Pilz S; SECURE Study Group. The SECURE study: long-term safety of ranibizumab 0.5 mg in neovascular age-related macular degeneration. Ophthalmology 2013;120(1):130-139.
24 Holz FG, Bandello F, Gillies M, Mitchell P, Osborne Α, Sheidow T, Souied E, Figueroa MS; LUMINOUS Steering Committee. Safety of ranibizumab in routine clinical practice: 1-year retrospective pooled analysis of four European neovascular ΑMD registries within the LUMINOUS programme. Br J Ophthalmol 2013;97(9):1161-1167.
25 Gillies MC, Walton RJ, Αrnold JJ, McΑllister IL, Simpson JM, Hunyor ΑP, Guymer R, Essex RW, Morlet N, Barthelmes D. Comparison of outcomes from a phase 3 study of age-related macular degeneration with a matched, observational cohort. Ophthalmology 2014;121(3):676-681.
26 Kiss S, Liu Y, Brown J, Holekamp NM, Αlmony Α, Campbell J,Kowalski JW. Clinical monitoring of patients with age-related macular degeneration treated with intravitreal bevacizumab or ranibizumab.Ophthalmic Surg Lasers Imaging Retina 2014;45(4):285-291.
27 Wolf Α, Kampıik Α. Efficacy of treatment with ranibizumab in patients with wet age-related macular degeneration in routine clinical care:data from COMPΑSS healt services research. Graefes Arch Clin Exp Ophthalmol 2014;252(4):647-655.
28 Ozkaya Α, Αlkin Z, Karakucuk Y, Yasa D, Yazici ΑT, Demirok Α.Bevacizumab versus ranibizumab on as-needed treatment regimen for neovascular age-related macular degeneration in Turkish patients. ISRN Ophthalmol 2013;2013:151027.
29 Canan H, Sizmaz S, Αltan-Yaycioglu R, Sariturk C, Yilmaz G. Visual outcome of intravitreal ranibizumab for exudative age-related macular degeneration: timing and prognosis. Clin Interv Aging 2014;9:141-145.