INTRODUCTION
Pterygium is defined as a fibrovascular triangular encroachment of the epithelial tissue onto the cornea,usually at the nasal side, which leads to visual disturbance in severe case. It is associated with multiple risk factors such as chronic sunlight exposure, high altitude, lower latitude, and occupations such as commercial motorbike riders, outdoor workers and sand and sawmill workers[1-5]. Pterygium can cause visual disturbance due to encroachment in the visual axis or due to irregular astigmatism.
Pterygium surgery can be elucidated with diverse approach.Bare sclera technique, which was initially popular among surgeons, is now considered as an unacceptable method due to a high recurrence rate[6-8]. To address this, a variety of adjunctive methods have been developed with the aim of reducing the recurrence after surgery. Among those, the use of conjunctival autograft transplantation (CAT), amniotic membrane transplantation (AMT), and the combined conjunctival autograft transplantation and overlay Amniotic membrane transplantation (CAT with AMT) are in common practice. Each of these methods has its own pros and cons,and there is no gold standard for pterygium surgery. Studies show 97% of all recurrence occurs within 1styear of excision.Thus it is suggested 1y follow up is required to identify the recurrence[9]. The optimal method should have preferably no or low recurrence, have minimal adverse events, and with cosmetically acceptable appearance after pterygium surgery[10].Pterygium excision with CAT is popular in some surgeons for the fact that it has comparatively low recurrence rate and complications[10-14]. Other studies have shown that the AMT for pterygium surgery facilitates epithelialization, maintains normal epithelial phenotype, and reduces inflammation,scarring and vascularization[12,15-16]. The safety and effectiveness of combined use of CAT with AMT have also been emphasized by others[17-18]. However, there has been no study comparing pterygium surgery techniques by CAT with AMT to CAT and AMT alone.
Herein, we retrospectively reviewed the records of the patients who underwent pterygium surgery by those three different techniques and compared them.
SUBJECTS AND METHODS
The Ethical Committee of Zhongda Hospital, Affiliated Hospital of Southeast University, approved this study in accordance with the Ethical Standards laid down in the Declaration of Helsinki (Seventh revision, October 2013,Fortaleza, Brazil).
We retrospectively reviewed the medical records of patients with primary or recurrent pterygia in one eye who had undergone excision followed by intraoperative application of either CAT (group A), AMT (group B), or CAT with AMT(group C) between July 2013 and July 2015 in outpatient operation room and had completed minimum 12-month follow up at the Department of Ophthalmology, Zhongda Hospital, Nanjing, China. We excluded those with ocular trauma or a history of ocular surgery within the previous year other than pterygium surgery, the use of 5-Flurouracil (FU)and the use of mitomycin C (MMC) in pterygium surgery.We also excluded the patients with contact lens wearing or under treatment with any topical medications other than nonpreserved artificial tears. Prior to the surgery, all patients had undergone Schirmer’s test and tear break-up time (TBUT),and the patients already diagnosed as dry eye (the Schirmer’s test <10 mm or TBUT <10s) before surgery were not enrolled.Additional exclusion criteria consisted of those with pregnancy,systemic diseases (hematologic, respiratory, rheumatologic)and systemic infection.
The total patient numbers having regular follow-up and good documentations after exclusion were 51 (primary 37, recurrent 14, the same description below), 47 (34, 13) and 44 (33, 11)for CAT, AMT and CAT+AMT respectively. Medical records showed that patients had undergone detailed ocular evaluation using slit-lamp examination, measurement of best-corrected visual acuity and assessment of intraocular pressure.
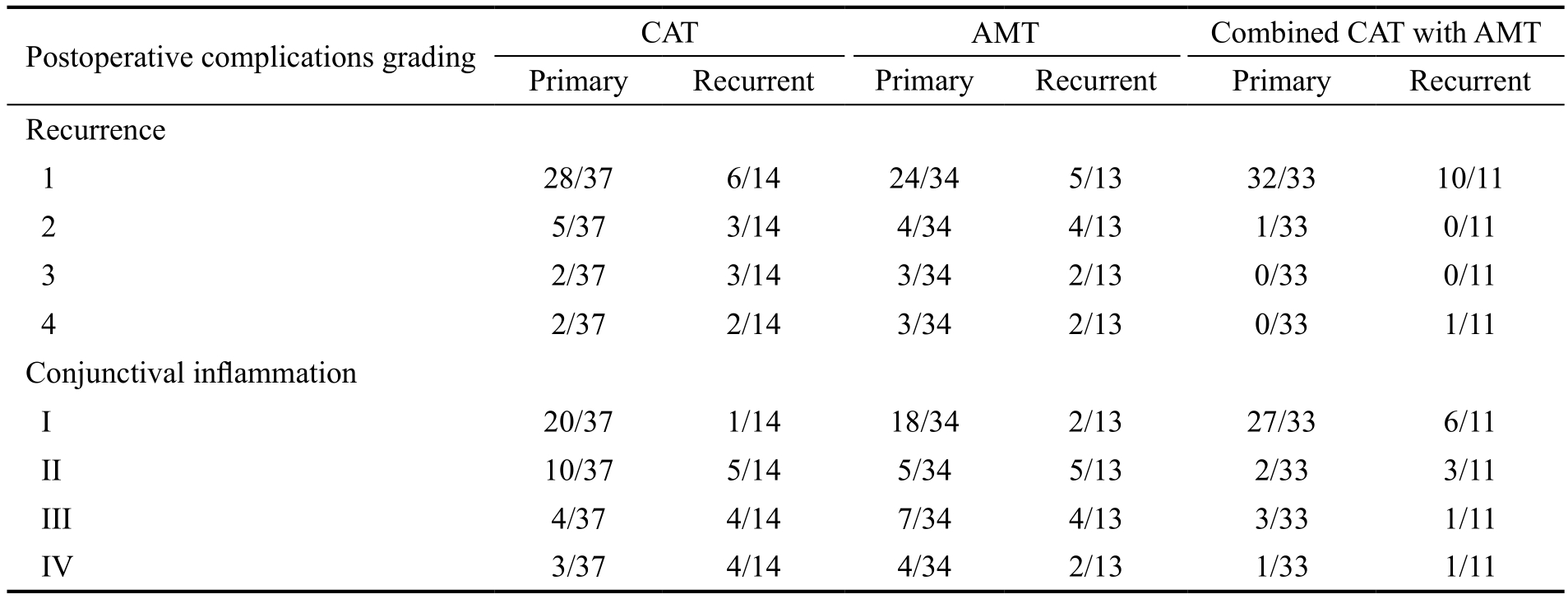
The recurrence status of pterygium preoperatively or at 12mo post-surgery was reviewed using a grade system previously reported: grade 1, no recurrence; grade 2, presence of fine episcleral vessels without fibrous tissue in the surgical areas; grade 3, the presence of fibrovascular tissue in the surgical areas without invasion onto the cornea (conjunctival recurrence)[12]; and grade 4,fibrovascular tissue invaded onto the cornea (cornea recurrence). Preoperatively, 38 cases were recurrent cases. Among them, 14 cases had undergone CAT(grade 2:2; grade 3:4; grade 4:8), 13 had undergone AMT(grade 2:2; grade 3:2; grade 4:9), and 11 had undergone CAT+AMT (grade 2:2; grade 3:2; grade 4:7).
We also reviewed the results of Schirmer’s test and TBUT at 6mo post-surgery.
Postoperative conjunctival inflammation data at 1mo postsurgery was reviewed. It had been reported using a grade system described as[19]: grade I (no in flammation), grade II(mild), grade III (moderate), and grade IV (severe), according to the degree of blood vessel injection. All cases of surgery were uneventful and there were secured attachment of conjunctival autograft or amniotic membrane or both in all eyes after surgery. No complications developed during the surgeries.Surgical Techniques All surgeries were performed by a single surgeon (Hu K) under retrobulbar anesthesia. Firstly, the head and neck of pterygium were dissected from the cornea by a surgical blade, and then the head, neck and body were excised by a conjunctival scissor, with the excision edge approximate 4 mm from the limbus, and this was followed by the removal of subconjunctival fibrovascular tissue for 2 mm beyond the conjunctival edge. Following the excision of pterygium, eye surface was washed with 100 mL balanced salt solution and patients had received either CAT or AMT or combined CAT and overly AMT (CAT with AMT) (Figure 1A-1D). Sutures were used in all groups.
In group A, conjunctival autograft was harvested from the superior bulbar conjunctiva, and then attached to the tissueexcised bare sclera area without crossing corneal limbus usinginterrupted 8-0 absorbable vicryl sutures. In group B, human sterilized freeze-dried amniotic membrane (FD-AM) (Jiangxi Ruiji Bio-Engineering Technology, Ltd., China) was used as previously described[20], and attached to the tissue-excised bare sclera area by 8-0 vicryl sutures extending to the area of cornea from where pterygium was excised. In group C, CAT wasfirst done as described above followed by overly of AMT covering the CAT also extending to the area of cornea from where pterygium was excised by the same suturing.
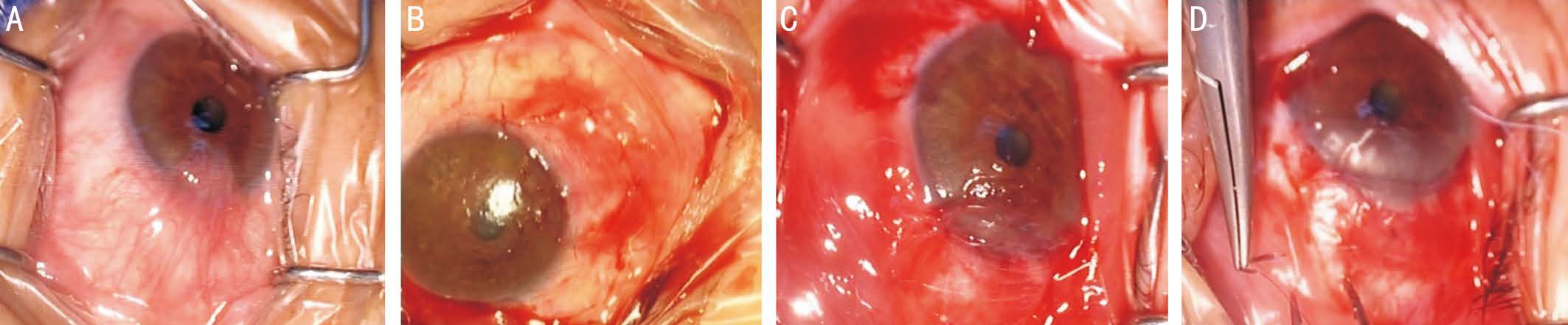
Figure 1 The representative clinical photographs of pterygium and different techniques of surgeries A: The representative photo of pterygium before surgery; B: The representative photo of conjunctival autograft transplantation in group A (CAT); C: The representative photo of human sterilized freeze-dried amniotic membrane transplantation in group B (AMT); D: The representative photo of combined use of CAT with AMT in group C.
Table 1 The characteristics of patients enrolled in the study
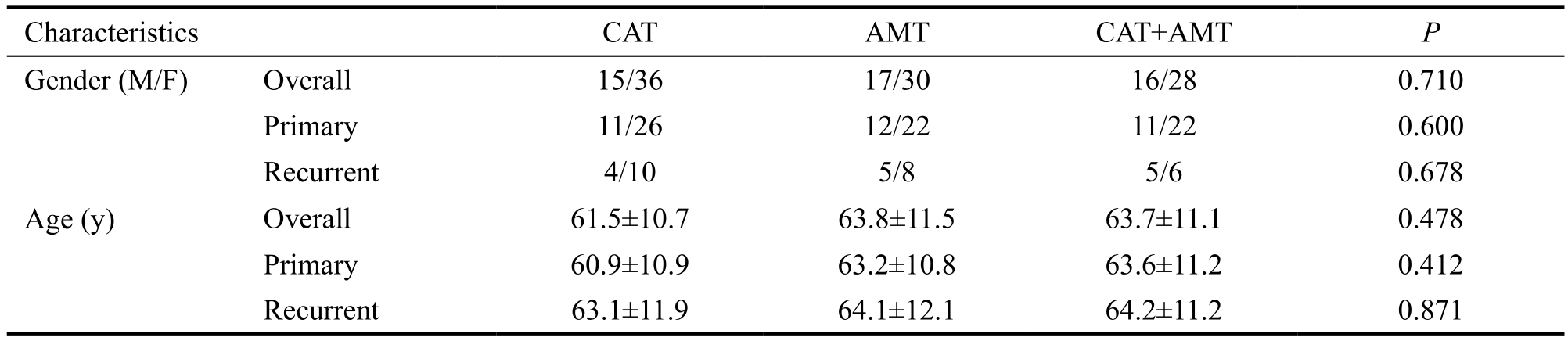
Table 2 The comparison between group C and group A, and between group C and group B
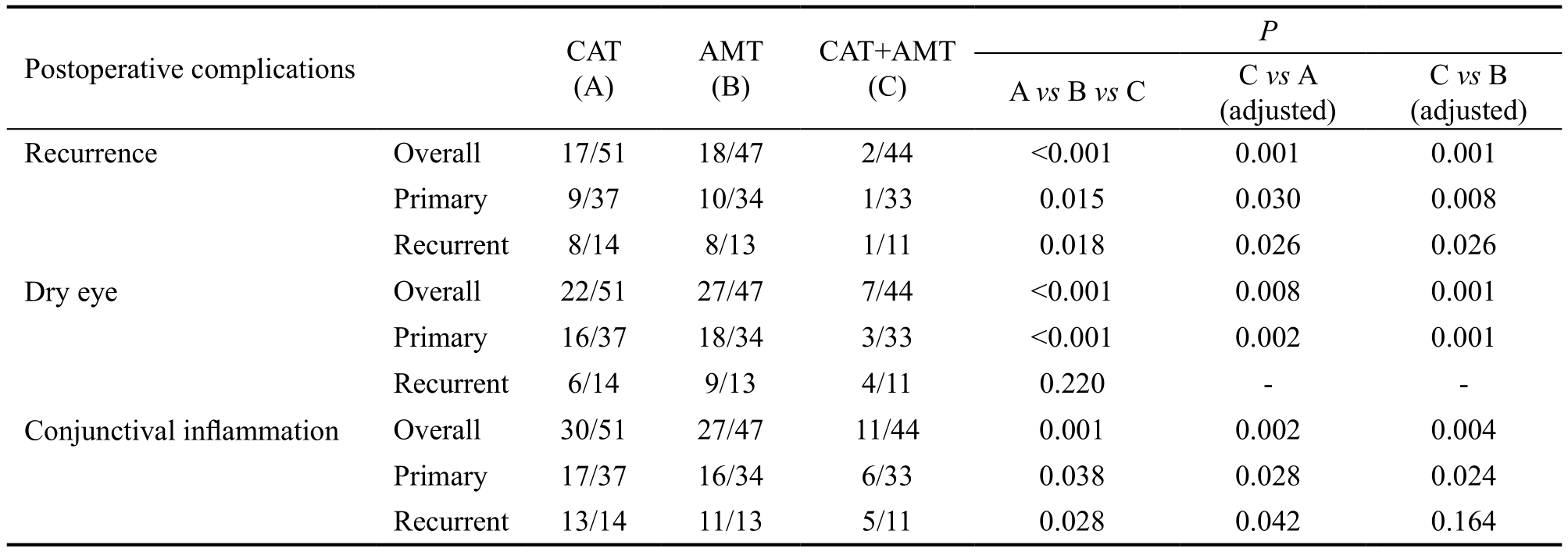
Overall, the occurrence of postoperative recurrence, dry eye and conjunctival in flammation is less in group C as compared to group A or B.
Postoperatively, all patients had received identical regimen of Pranoprofen eye drop (5 mL/5 mg) (Kotobuki Pharmaceutical Co., Ltd.) 3 times a day for 15d, Tobradex eye drop (Tobramycin and Dexamethasone) (S.A. ALCON-COUVREUR N.V) 3 times a day for 15d, Tobradex eye ointment (Tobramycin and Dexamethasone) (S.A. ALCON-COUVREUR N.V) 1 time at night for 15d.
Statistical Analysis Statistical analysis was performed using PASW Software version 20.0 (SPSS/IBM, Inc., Chicago, IL,USA). Chi-square and Fisher’s exact tests were used to analyze categorical variables such as gender and complication rate,whereas One-way ANOVA analysis was used, as appropriate,to analyze continuous numerical variables such as age. P<0.05 was considered to be statistically significant.
RESULTS
This study included 142 eyes (142 patients), with a mean age of 63.2±11.8y. Totally 66.2% were females and 33.8%were males. The gender and age were statistically consistent between groups (Table 1).
The pterygium recurrence post-surgery were 17 cases, 18 cases and 2 cases in groups A, B and C respectively; overall,group C had significant lower recurrence rate versus group A(P=0.001) and group B (P=0.001). Among them, both primary and recurrent cases of group C showed statistical differences as compared to group A (P=0.030 and 0.026) and B (P=0.008 and 0.026) (Table 2). In primary pterygium, groups A, B and C showed 9, 10 and 1 recurrence respectively, and regarding to recurrent pterygium, groups A, B and C had 8, 8 and 1 recurrence respectively. The detailed grades information is shown in Table 3.
Postoperative dry eyes occurred in 22, 27 and 7 cases in groups A, B and C respectively. The overall comparison of group C versus group A or B was statistically significant in either (P=0.008 or P=0.001) (Table 2). In primary pterygium,16, 18 and 3 patients developed dry eye in groups A, B and C respectively, and the average Schirmer’s test of them were 7.3 mm, 8.0 mm and 9.1 mm, and TBUT were 7.1s, 7.3s and 8.3s; the comparison between groups A and C (P=0.002),or between groups B and C (P=0.001) was statistically significant and dry eye was less in group C. In recurrent pterygium, 6, 9 and 4 patients developed dry eye in groups A,B and C respectively, with the least in group C, although the comparisons were not statistically significant, and the average Schirmer’s test were 7.4 mm, 7.0 mm and 7.5 mm, and TBUT were 7.1s, 7.4s and 7.3s (Table 2).
Postoperatively, conjunctival in flammations around the surgical sites were 30, 27 and 11 in groups A, B and C respectively.The overall comparisons between groups A and C (P=0.002)and between groups B and C (P=0.004) were statistically significant. In primary pterygium, conjunctival in flammations in groups A, B and C were 17, 16 and 6 cases respectively;the comparisons between groups A and C (P=0.028) and between groups B and C (P=0.024) were significant indicating that the fewer rate of conjunctival inflammation in group C. In recurrent pterygium, conjunctival inflammations were manifested 13, 11 and 5 respectively; the comparison between groups C and A (P=0.042) was statistically significant,although groups C and B was not statistically significant(P=0.164) (Table 2). The detailed grades information of them is shown in Table 3. Generally, group C presented with the fewest conjunctival in flammation.
Table 3 The overall view of grades of postoperative recurrence and conjunctival in flammation in primary and recurrent pterygium in groups A (CAT), B (AMT) and C (combined CAT with AMT)
DISCUSSION
The absolute treatment of pterygium is the surgical intervention.In contrast to small atopic pterygium which is rather left alone and treated with lubricant drops, progressive pterygium should undergo surgery. The method depends upon the choice of the surgeon. Following excision, the surgeons have many options to choose such as CAT alone, AMT alone, combined use of CAT with AMT, CAT plus MMC, beta-irradiation only, MMC only, etc[15,21-22]. However, the recurrence of pterygium is still the most common complication. So many surgeons make efforts to avoid it through different surgical techniques.
Primary and recurrent pterygium surgery treated with CAT have been reported occurring recurrences[23-25], and in this study, we also showed 17.6% clinically significant recurrences(grades 3 and 4). But studies have also shown that the recurrence is higher in those treated with AMT as compared to CAT[26-27]; further retrospective controlled studies stated lower recurrence in CAT versus AMT for primary and recurrent pterygium surgery[12,28]. However, some other studies reported that using AMT alone could also present good results[29-30], in addition, it can be used as an alternative choice, especially for advanced cases with bilateral heads or patients who might need glaucoma surgery later[11,30-31]. Ghanavati et al[17]documented low recurrence rate within the pterygium belt with use of combined CAT and overlay AMT. However, the detailed comparisons among the above-mentioned surgery techniques, especially the best option among them have not been reported. In this study, we compared CAT with AMT,CAT alone and AMT alone in postoperative recurrence,dry eye and conjunctival inflammation respects. The lower recurrence was demonstrated in both primary and recurrent pterygium with the use of combined CAT with AMT over CAT or AMT alone. Further, as mentioned previously[20],there is distinct relationship between dry eye and pterygium.In our study, we had already excluded the cases with dry eye preoperatively, but our result suggests dry eye could be one of the postoperative complications. It presented that there was significant difference between group C versus A or B,demonstrating combined CAT with AMT has lower incidence of dry eye than CAT or AMT alone. Postoperative conjunctival in flammation is prevalent after any ocular surface surgery and is regarded as a normal wound healing response, and further use of suture is known to cause conjunctival in flammation as reported in literature[32]. In our study, 3-4wk of postoperative period was given to allow normal in flammatory responses to subside, thus we reviewed the data at 1mo post-surgery. Our study showed that there were still some degree of conjunctival in flammations in 3 groups, but group C (CAT with AMT) had significantly less in flammations as compared to group A or B.Overall, we demonstrate that the combined CAT with AMT is a better option in primary and recurrent pterygium surgery.
The use of CAT covers tissue-excised bare area helping early epithelization and ocular surface reconstruction. The use of AMT also facilitates epithelization and decreases local inflammation leading to early recovery. In addition, it binds with the growth factors which promote wound healing,further, AMT provides a basement which aids the epithelial growth[33-34].
Our study has specified the amniotic membrane used, so it was identical among all the cases enrolled, whereas in other previously reported papers, the amniotic membrane used have not been specified[26,35-36]. We used standardized postoperative medication regimen which helped to compare the results among groups evenly. The cases showed no postoperative astigmatism, pyogenic granuloma, sclera thinning (ulceration),iritis, and symblepharon formation in either group during the period of study. The limitation of the study is that the subjects selected were limited to the single race or ethnicity (Chinese-Han).We have hypothesis that when combined use of CAT and overlay AMT (CAT with AMT) is done, it promotes individual advantage more and this further increases the process of epithelization. Our study confirms that hypothesis showing that CAT with AMT performs better in the rate of recurrence,dry eye and conjunctival inflammation as compared to CAT or AMT alone. So, we conclude that CAT and overlay AMT has better clinical outcome in primary and recurrent pterygium surgery versus CAT or AMT alone. This may potentially guide surgeons to select appropriate techniques in pterygium surgery in future.
ACKNOWLEDGEMENTS
Foundations:Supported by Natural Science Foundation of Jiangsu Province (No.BK20141346); Nanjing Science and Technology Development Plan (No.201402001).
Conflicts of Interest:Malla T, None; Jiang J, None; Hu K,None.
REFERENCES
1 Zhou WP, Zhu YF, Zhang B, Qiu WY, Yao YF. The role of ultraviolet radiation in the pathogenesis of pterygia (Review). Mol Med Rep 2016;14(1):3-15.
2 Shrestha S, Shrestha SM. Comparative study of prevalence of pterygium at high altitude and Kathmandu Valley. J Nepal Health Res Counc 2014;12(28):187-190.
3 Achigbu E, Ezepue UF. Prevalence and severity of pterygium among commercial motorcycle riders in south eastern Nigeria. Ghana Med J 2014;48(3):153-157.
4 Asokan R, Venkatasubbu RS, Velumuri L, Lingam V, George R.Prevalence and associated factors for pterygium and pinguecula in a South Indian population. Ophthalmic Physiol Opt 2012;32(1):39-44.
5 Njinaka I, Uhumwangho OM, Edema OT, Dawodu OA, Omoti AE. A comparison study of conjunctiva disorders in technical and administrative sawmill workers in Nigeria. Malays J Med Sci 2011;18(3):43-48.
6 Chan TC, Wong RL, Li EY, Yuen HK, Yeung EF, Jhanji V, Wong IY.Twelve-year outcomes of pterygium excision with conjunctival autograft versus intraoperative mitomycin C in double-head pterygium surgery. J Ophthalmol 2015;2015:1-6.
7 Otsuka J. Treatment of pterygium. Ganka 1970;12(1):65.
8 Sodhi PK, Verma L, Ratan SK. The treatment of pterygium. Surv Ophthalmol 2003;48(2):145-180.
9 Hirst LW, Sebban A, Chant D. Pterygium recurrence time. Ophthalmology 1994;101(4):755-758.
10 Fernandes M, Sangwan VS, Bansal AK, Gangopadhyay N, Sridhar MS, Garg P, Aasuri MK, Nutheti R, Rao GN. Outcome of pterygium surgery: analysis over 14 years. Eye (Lond) 2005;19(11)1182-1190.
11 Li M, Zhu M, Yu Y, Gong L, Zhao N, Robitaille MJ. Comparison of conjunctival autograft transplantation and amniotic membrane transplantation for pterygium: a meta-analysis. Graefes Arch Clin Exp Ophthalmol 2012;250(3):375-381.
12 Prabhasawat P, Barton K, Burkett G, Tseng SC. Comparison of conjunctival autografts, amniotic membrane grafts, and primary closure for pterygium excision. Ophthalmology 1997;104(6):974-985.
13 Lee JS, Ha SW, Yu S, Lee GJ, Park YJ. Efficacy and safety of a large conjunctival autograft for recurrent pterygium. Korean J Ophthalmol 2017;31(6):469-478.
14 Kim DJ, Lee JK, Chuck RS, Park CY. Low recurrence rate of anchored conjunctival rotation flap technique in pterygium surgery. BMC Ophthalmol 2017;17(1):187.
15 Kaufman SC, Jacobs DS, Lee WB, Deng SX, Rosenblatt MI, Shtein RM. Options and adjuvants in surgery for pterygium: a report by the American Academy of Ophthalmology. Ophthalmology 2013;120(1):201-208.
16 Sangwan VS, Burman S, Tejwani S, Mahesh SP, Murthy R. Amniotic membrane transplantation: a review of current indications in the management of ophthalmic disorders. Indian J Ophthalmol 2007;55(4):251-260.
17 Ghanavati S, Shousha M, Betancurt C, Perez V. Combined conjunctival autograft and overlay amniotic membrane transplantation; a novel surgical treatment for pterygium. J Ophthalmic Vis Res 2014;9(3):399-403.
18 Shimazaki J, Kosaka K, Shimmura S, Tsubota K. Amniotic membrane transplantation with conjunctival autograft for recurrent pterygium.Ophthalmology 2003;110(1):119-124.
19 Kheirkhah A, Casas V, Sheha H, Raju VK, Tseng SC. Role of conjunctival inflammation in surgical outcome after amniotic membrane transplantation with or without fibrin glue for pterygium. Cornea 2008;27(1):56-63.
20 Chen YH, Cui HG. Amniotic membrane transplantation for porous sphere orbital implant exposure. J Zhejiang Univ Sci B 2007;8(9):616-619.
21 Ang LP, Chua JL, Tan DT. Current concepts and techniques in pterygium treatment. Curr Opin Ophthalmol 2007;18(4):308-313.
22 Hovanesian JA, Starr CE, Vroman DT, Mah FS, Gomes JAP, Farid M, Shamie N, Davidson RS, John T, Holland EJ, Kim T; ASCRS Cornea Clinical Committee. Surgical techniques and adjuvants for the management of primary and recurrent pterygia. J Cataract Refract Surg 2017;43(3):405-419.
23 Ti SE, Chee SP, Dear KB, Tan DT. Analysis of variation in success rates in conjunctival autografting for primary and recurrent pterygium. Br J Ophthalmol 2000;84(4):385-389.
24 Kmiha N, Kamoun B, Trigui A, Jelliti B, Fourati M, Chaabouni M.Effectiveness of conjunctival autograft transplantation in pterygium surgery. J Fr Ophtalmol 2001;24(7):729-732.
25 Kwon SH, Kim HK. Analysis of recurrence patterns following pterygium surgery with conjunctival autografts. Medicine (Baltimore)2015;94(4):e518.
26 Tananuvat N, Martin T. The results of amniotic membrane transplantation for primary pterygium compared with conjunctival autograft. Cornea 2004;23(5):458-463.
27 Clearfield E, Hawkins BS, Kuo IC. Conjunctival autograft versus amniotic membrane transplantation for treatment of pterygium:findings from a cochrane systematic review. Am J Ophthalmol 2017;182:8-17.
28 Luanratanakorn P, Ratanapakorn T, Suwan-Apichon O, Chuck RS.Randomised controlled study of conjunctival autograft versus amniotic membrane graft in pterygium excision. Br J Ophthalmol 2006;90(12):1476-1480.
29 Hino T, Sotozono C, Inatomi T, Fukuoka H, Nakamura T, Nagata M,Koizumi N, Morio K, Yokoi N, Kinoshita S. Indications and surgical outcomes of amniotic membrane transplantation. Nippon Ganka Gakkai Zasshi 2012;116(4):374-378.
30 Morikawa K, Sotozono C, Inatomi T, Nakamura T, Yokoi N, Matsuo Y,Kinoshita S. Indication and efficacy of amniotic membrane transplantation performed under advanced medical healthcare. Nippon Ganka Gakkai Zasshi 2016;120(4):291-295.
31 Küçükerdönmez C, Akova YA, Altinörs DD. Comparison of conjunctival autograft with amniotic membrane transplantation for pterygium surgery: surgical and cosmetic outcome. Cornea 2007;26(4):407-413.
32 Kheirkhah A, Nazari R, Nikdel M, Ghassemi H, Hashemi H, Behrouz MJ. Postoperative conjunctival in flammation after pterygium surgery with amniotic membrane transplantation versus conjunctival autograft. Am J Ophthalmol 2011;152(5):733-738.
33 Dekaris I, Mravicić I, Barisić A, Draca N, Pauk M. Amniotic membrane transplantation in the treatment of persistent epithelial defect on the corneal graft. Coll Antropol 2010;34(Suppl 2):15-19.
34 Jirsova K, Jones GLA. Amniotic membrane in ophthalmology:properties, preparation, storage and indications for grafting-a review. Cell Tissue Bank 2017;18(2):193-204.
35 Ozer A, Yildirim N, Erol N, Yurdakul S. Long-term results of bare sclera, limbal-conjunctival autograft and amniotic membrane graft techniques in primary pterygium excisions. Ophthalmologica 2009;223(4):269-273.
36 Keklikci U, Celik Y, Cakmak SS, Unlu MK, Bilek B. Conjunctivallimbal autograft, amniotic membrane transplantation, and intraoperative mitomycin C for primary pterygium. Ann Ophthalmol (Skokie) 2007;39(4):296-301.