INTRODUCTION
Small-incision lenticule extraction (SMILE) is a relatively commonly used all-in-one procedure for correcting refractive errors[1-2]. It involves the creation of an intrastromal lenticule, which is manually extracted through a 2- to 4- mm side incision. SMILE is known to be superior to surface refractive surgery because of its need for only a minor incision and less invasive nature[3-4]. However, impaired optical quality after SMILE remains a challenge for surgeons. Several factors are known to in fluence optical quality, such as corneal aberration[5],mesopic pupil size[6], corneal wound healing[7], and centration of the treatment zone[8].
SMILE is characterized by the absence of a flap; however,a corneal cap is associated with vision quality[9-10]. Previous studies have explored corneal caps with different thicknesses created using femtosecond laser[11-12]; however, the longitudinal changes in cap morphology after surgery as well as its relationship with intraocular scattering have seldom been reported. This inspired us to further study this subject.
Fourier-domain optical coherence tomography (FD-OCT)is superior to other imaging modalities owing to its noninvasiveness, speed, and repeatability for mapping corneal thickness, and these features have been applied in several clinical studies[13-14]. FD-OCT, also allows easy measurement of cap thickness in different meridians and areas of the central cornea, thereby allowing an overall analysis of the shape of caps. Moreover, because of the improper matching between the cap and the interface stroma after lenticule extraction, twisted segments of Bowman’s layer defined as microdistortion can also be observed using FD-OCT[10]. Thus, the present study utilized a double-pass system to objectively quantify optical quality, and FD-OCT to perform non-contact measurement of corneal caps after SMILE. The variability, uniformity, and accuracy of the cap as well as its relation with intraocular scattering, were assessed.
SUBJECTS AND METHODS
Informed consents were obtained from the patients to participate in the research. All performance was approved by the Ethics Committee of Eye and ENT Hospital of Fudan University.
Subjects Myopic patients scheduled for SMILE surgery at Refractive Surgery Centre of the Department of Ophthalmology, Eye and ENT Hospital of Fudan University between June 2016 and September 2016 were included in this prospective, non-randomized study. The inclusion criteria were as follows: spherical refraction less than -10 D,astigmatism less than -5 D, corrected distance visual acuity(CDVA) equaling to or better than 20/25, no use of contact lenses within the last 2wk and stable refraction for 2y at least.Individuals with following diseases were excluded: suspicious or diagnosed keratoconus, acute eye diseases, systemic connective tissue disease, and menstrual phase in female patients prior to surgery. Twelve female patients (23 eyes) and 21 male patients (42 eyes) with a mean age of 25.75±7.82y(range, 18 to 48y) were included in this study. The mean preoperative spherical equivalent was -5.32±1.57 D. The mean preoperative corneal keratometry and corneal thickness were 42.86±1.10 D and 540.14±26.57 μm, respectively.
Surgical Technique All SMILE treatments were conducted by the same surgeon (Yu ZQ) using a VisuMax 500 kHz femtosecond laser (Carl Zeiss Meditec AG, Germany) with a pulse energy of 130 nJ. Details of the SMILE procedures have been described previously[15]. In current study, a 2-mm incision was created superotemporally (right eye) or superonasally(left eye). In all cases, the intended cap thickness was 120 μm with a diameter of 7.5 mm, a refractive lenticule diameter of 6.5 mm, and a side-cut angle of 90°. All caps were created uneventfully and no intraoperative complications occurred.
Postoperative Treatment and Follow-up The postoperative treatment regimen included 0.3% tobramycin (Alcon Co. Inc.,USA) four times daily for a week, 0.1% fluorometholone(Santen, Japan), and artificial tears (Polyethylene Glycol Eye Drops, Alcon Co. Inc., USA) four times daily for a month.Patients returned for postoperative examination at 1d, 1wk,1 and 3mo after surgery. Uncorrected distance visual acuity(UDVA), CDVA, subjective refraction, slit-lamp microscopy,Optical Quality Analysis System (OQAS), Pentacam HR imaging, and anterior segment FD-OCT were performed at every follow-up. No patient dropped out of the study.
OCT Imaging FD-OCT (RTVue, software version 6.2,Optovue Inc., USA) was used to measure the cap thickness in all cases, with a wide-angle adaptor lens offering an 8-mm long scan width, an axial resolution of 5 μm, and a transverse resolution of 15 μm (focused spot size). A line-scan pattern centered at the pupil was used to image the cornea along the 0°, 45°, 90°, and 135° meridians. All measurements were performed by the same examiner (Fu D) who was blinded to the intended cap thickness.

Figure 1 Optical coherence tomography line-scan image Three months after small-incision lenticule extraction, the interface is still detected with high reflectivity; microdistortions are indicated by white arrows.
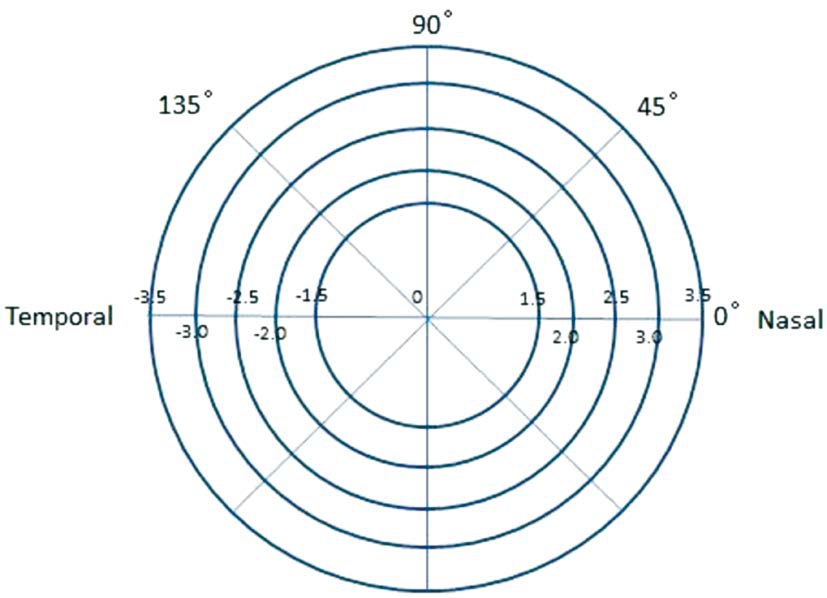
Figure 2 Schema graph of corneal cap measurements (right eye).
Each eye was scanned several times in a single meridian until one image with valid interface detection evaluated by the examiner was obtained. Thus, four consecutive scans from each eye with the best centration and quality were acquired.The anterior and posterior boundaries of the cornea were automatically lined, and the interface was adjusted manually by using calipers according to the increased signal intensity on the image provided by the software (Figure 1). The morphology of the cap was generated using 41 points (center 0 mm, ±1.5 mm,±2 mm, ±2.5 mm, ±3 mm, and ±3.5 mm) along the four meridians and the vertex. The corneal vertex was defined as 0 mm with a negative value on the temporal side and a positive value on the nasal side (left eyes were mirrored to the right eye) (Figure 2). The cap measurements at 0 mm and ±1.5 mm positions were averaged to calculate the mean central cap thickness; measurements at ±2 mm and ±2.5 mm positions were averaged to calculate the mean paracentral cap thickness; and measurements at ±3 mm and ±3.5 mm positions were averaged to calculate the mean peripheral cap thickness.Range of the thickness was acquired as the difference between the maximum value and the minimum value.
Simultaneously, the total number of microdistortions in Bowman’s layer was counted on the four meridians and was defined as index N (Figure 1).
Optical Quality Measurement Using an OQAS based on the double-pass technique (OQASTMII,Visiometrics, Terrassa,Spain), we obtained the optical quality parameters, including MTF cutoff frequency, Strehl ratio (SR), objective scattering index (OSI), and OQAS values (OVs; 100%, 20%, and 9%)at 1d, 1wk, 1 and 3mo after surgery. All measurements were performed in a dark room by the same examiner (Fu D), with a 4.0 mm pupil in mesopic condition. All the patients were asked to sit in a comfortable position and minimize eye’s movement;the patients rested each eye by closing it for 2s after each measurement. In this way, 3-5 consecutive measurements were acquired in each eye.
Table 1 Values of OQASTMmean ±SD
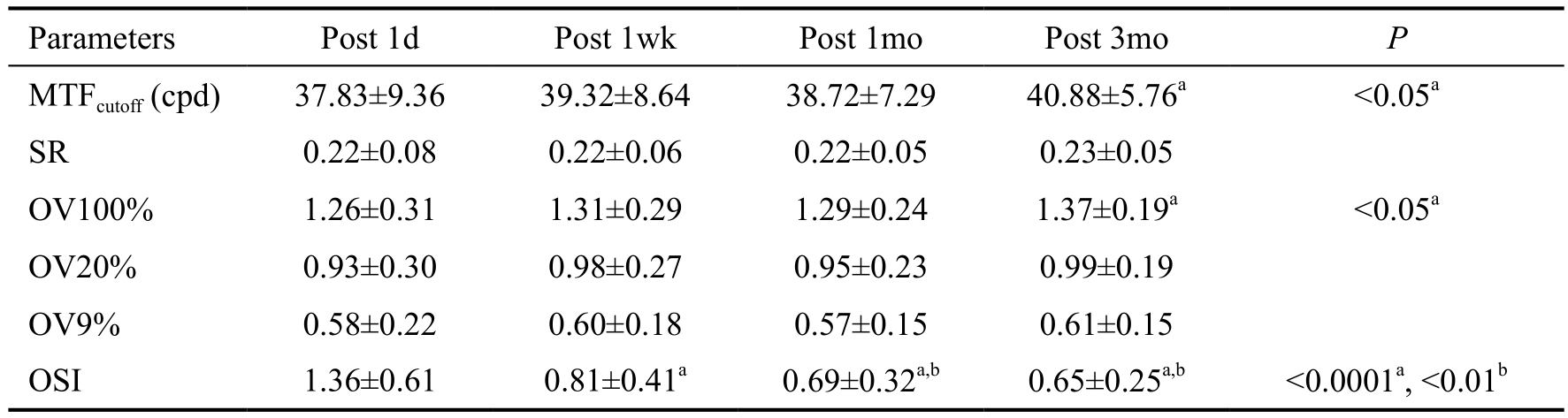
MTFcutoff: Modulation transfer cutoff frequency; cpd: Cycles per degree; SR: Strehl ratio in two dimensions; OV: Optical quality analysis system values; OSI: Objective scatter index.aStatistically significant compared with 1d after surgery;bStatistically significant compared with 1wk after surgery.
Table 2 Changes in corneal cap thickness after SMILE mean±SD, μm
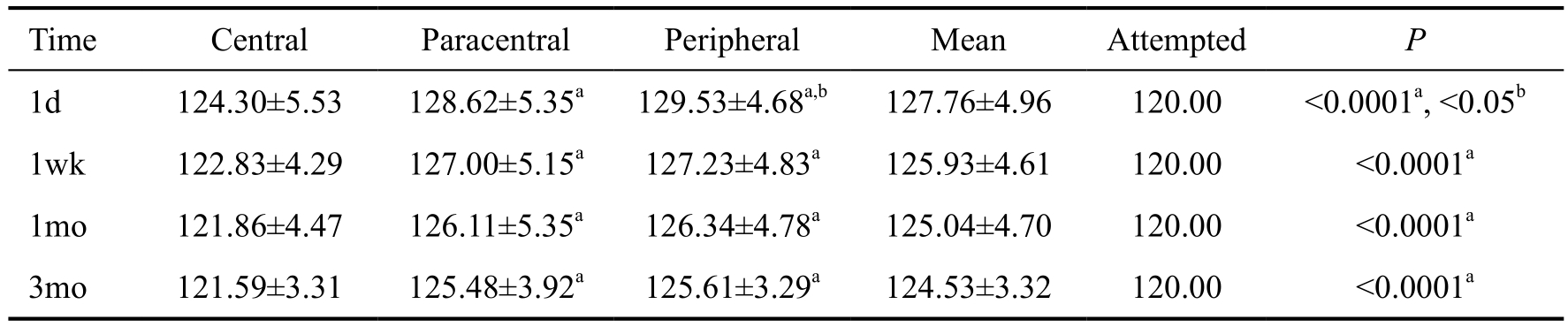
aStatistically significant compared with central area;bStatistically significant compared with paracentral area.
Statistical Analyses Statistical analysis was performed using SAS software (V.9.4, Cary, NC, USA). A linear mixed model was used to assess the postoperative variability of corneal cap thickness and optical values by OQAS, and their relationships were analyzed using Pearson analysis after performing Kolmogorov-Smirnov tests. The P values were adjusted using the Bonferroni correction for multiple comparisons and P<0.05 was considered significant level for all tests.
RESULTS
Refractive Outcomes Three months after surgery, 98.5%(n=64) of all eyes had a CDVA that was the same or better than the preoperative CDVA. Although a CDVA loss of 1 line was observed in 1 eye (1.5%), no CDVA loss of 2 lines or more occurred. The CDVA improved significantly from -0.07±0.03 logarithm of the minimum angle of resolution before surgery to -0.10±0.05 logarithm of the minimum angle of resolution 3mo after surgery (P<0.05, paired t-test).
After surgery, the UDVA was 20/20 or better in 87.7% (n=57)and 100% (n=65) of the eyes at 1d and 1wk after surgery,respectively. As for the spherical equivalent, all eyes fell within±1 D since 1mo after surgery, and 83.1% (n=54) and 90.8%(n=59) of eyes fell within ±0.25 D and ±0.5 D respectively at 3mo follow-up. The achieved refraction results were related to target refraction (R=0.96, P<0.001) at 3mo after surgery.
Concerning stability, the mean spherical equivalent improved from 1d (-0.20±0.41 D) to 1wk (0.05±0.36 D) after surgery(P<0.001), but there was a slight but significant regression from 1wk to 3mo (-0.03±0.41 D) (P=0.019). There was no significant regression from 1mo (0.00±0.41 D) to 3mo(P=0.177).
Optical Quality As shown in Table 1, MTFcutoffand OV100%were highest at 3mo and statistically differed from those at 1d after surgery. OSI showed a downtrend and significant differences were found between 1d and the remaining three time points (P<0.0001) as well as between 1wk and the latter two time points (P<0.01). No significant difference was found in SR, OV20% and OV9% during the follow-up period.
Changes in Cap Thickness As shown in Table 2, the cap thickness decreased significantly (P<0.001) from 1d to 1wk after SMILE, and no significant longitudinal difference was found at the following time points. Over the 3-month follow-up period, the central cap thickness was persistently and significantly thinner than that in other two areas. No statistically significant difference was found between peripheral and paracentral areas except on 1d after surgery.The mean cap thicknesses were always thicker than intended thickness of 120 μm (P<0.001), even though the deviations decreased over time (9.92±5.31 μm, 8.08±5.35 μm, 7.19±6.10 μm, and 6.62±4.82 μm, P<0.001).
Microdistortion Microdistortion in Bowman’s layer was found in 90.77% (59 of 65 eyes), 84.62% (55 of 65 eyes), 81.54%(51 of 65 eyes) and 73.85% (48 of 65 eyes) respectively at 1d,1wk, 1 and 3mo after surgery. After Kolmogorov-Smirnov test,total number of microdistortion (N) was 5.43±4.19, 4.80±4.09,4.15±4.01, and 3.31±3.67 respectively at 1d, 1wk, 1 and 3mo after surgery. A significant difference was found between 1d and 1mo (P=0.021), 1d and 3mo (P<0.0001), and 1wk and 3mo (P<0.0001).

Figure 3 Correlation analysis of morphology and objective scattering index OSI: Objective scattering index; Range: Range of cap thickness (maximum value minus minimal value among all points); SD: Standard deviation of all points’ cap thickness; N: Total number of microdistortions; r: Correlation coefficient.
Correlations Between Morphology and OSI The standard deviation of corneal cap thickness was related to the OSI at 1d and 1mo after surgery (P=0.034, and P=0.009 respectively).Moreover, a weak but significant correlation was found between the range of cap thickness and OSI at 1mo after surgery (P=0.010). Furthermore, a negative correlation existed between N and range of cap thickness at 1d and 1wk after surgery (P<0.001, and P=0.018, respectively), and correlation coefficient decreased over time (Figure 3). No significant correlation was found between OSI and microdistortion (not shown infigure).
DISCUSSION
Creating a regular cap is one of the most crucial steps to ensure an accurate lenticule. Many studies have demonstrated that a regular and accurate corneal cap is available in SMILE[16].However, longitudinal changes in cap morphology after SMILE are seldom reported. The present study aimed tofind whether a relationship exists between cap morphology as well as microdistortion in Bowman’s layer and intraocular scattering.
Our study confirmed previous results that SMILE can yield excellent visual outcomes[17-18]. Since a newly developed OQAS based on the double-pass technique came into clinical use, its excellent, repeatable, and reliable assessment of optical quality in both adults and children has been identified[19-21].In the present study, the OSI showed a significant downtrend after surgery, but these changes gradually stabilized with time. This result is in agreement with that of Miao et al[21],who has showed that the highest mean OSI appeared at 20d after SMILE and decreased to the preoperative level at 3mo.Although a significant difference was found in OV100%and MTFcutoff, the SR, OV20%, and OV9% did not change significantly. The SR is a global optical quality parameter that takes all the frequencies into account, whereas the OVs are related to specific values. Although the lowest values all appeared at post 1d, we speculated that the worsening of optical quality was more serious at high contrast values (100%)as demonstrated by Ondategui et al[22].
In the present study, a statistically significant reduction in corneal cap thickness was found between 1d and 1wk after surgery, but it remained stable after 1wk in the central,paracentral and peripheral areas. However, in the study by Zhao et al[9], no significant changes in cap thickness were found between 1d and 1wk. The absence of area delineation may amplify the measurement errors. As shown in Figure 1, the contrast was insensitive near corneal vertex where the interface reflections are overwhelming. This was the reason why we defined the central 1.5-mm radius area to reduce possible errors. Apart from that, the peripheral area, especially the 3.75 mm radius circle in Zhao et al’s[9]study, where the hinge and lid shadowing is usually located, may yield inferior outcomes. Furthermore, the healing response after surgery may be the prominent reason for significant changes in cap thickness. Considering the biomechanics of the cornea,edema is unavoidable after removal of stromal lamellar[23];besides, nerve damage that could regulate epithelial integrity,proliferation, and wound healing has been revealed in other studies. Although better preservation of corneal nerve in SMILE than in LASIK was demonstrated, it still takes at least 1mo for nerve recovery[24]. Not only the wound healing responses mentioned above, but several processes are also in paly during the early postoperative period: resorption of fluid introduced by intraoperative irrigation, biomechanical hydration shift and interface reflectivity changes[24]. Further studies are warranted to determine which among these factors plays the dominant role.
In line with the finding of a previous study[9], an increasing trend in the cap thickness from central to peripheral area was observed in our study. Among these, corneal cap thickness in central area was significantly thinner than that in the other two areas regardless of time. Meanwhile, the changes in cap thickness between 1d and 1wk after surgery increased,showing the same trend. Therefore, we speculate the thicker cap in paracentral and peripheral areas leads to greater degree of variations in cap thickness. Increased tensile strength towards the peripheral area[25]and system errors inherent to OCT may partly explain the difference in thickness. We think that slower dissection in the peripheral area, with cavitation overworked on collagen fibers at the interface, may shed light on this larger variation. In this study, laser was fired from periphery in at lenticule’s posterior surface and from the center out at the anterior surface, thus the delay between the creation of posterior and anterior surface in central area versus the peripheral area was less. This delay may allow increased displacement and distortion of the anterior stromal collagen lamellae, leading to the coalescence of cavitation bubbles, as demonstrated by Shah et al[26]. Last but not the least, taking the physiologic morphology of cornea into account, it’s reasonable for a thinner central cap suited to thinner central cornea to ensure enough residual stromal bed thickness.
On average, the cap thickness in this study was persistently thicker than intended thickness of 120 μm, even though it tended to be more accurate overtime, especially in the central area; nevertheless, all patients achieved excellent visual outcomes 3mo after surgery. Supported by Reinstein et al’s[27]findings that mean cap thickness accuracy was between -2.3 and 6.5 μm and was -0.7 μm centrally, our results were within the reasonable range. In addition, based on the findings of previous studies, no difference in visual acuity was found with different cap thicknesses[12]; therefore, we speculate that regularity and not accuracy of cap in fluences optical qualities.In previous studies, the OQAS was reportedly related with ages and spherical equivalent[21], but no studies to date have reported any correlation with microdistortion and cap morphology.Optical quality after SMILE has been determined to a major extent in terms of visual acuity, higher-order aberration or contrast sensitivity[28]. However, Kamiya et al[29]assumed it was corneal scattering rather than higher-order aberration resulting from surface irregularity that played a vital role in visual performance after SMILE. The standard deviation and range of cap thickness, which served as indicators of cap morphology, showed a correlation with the OSI at 1mo after surgery. A previous study has revealed that OSI is in fluenced by refractive degrees[21]and cataract opacities , while in our study, these factors can be excluded cause all patients targeted to be emmetropia after SMILE and went through preoperative assessment. To our best knowledge, it is thefirst time to put forward relationship between cap morphology and intraocular scattering after SMILE. Microstructural changes, dry eye symptoms and a relatively small sample size may explain the weak but significant relationship. Further studies on cap morphology can help shed light on this relationship.
In line with the findings of Yao et al[10], the number of microdistortions decreased with time and most of them were located in the central area. A previous study proposed that microdistortions can disrupt corneal transparency and cause increased scattering of light[30], but we did notfind a correlation between microdistortion and OSI during the follow-up period.This may be attributed to epithelial growth that covered the irregular surface of Bowman’s layer. Interestingly, we found a negative correlation between the number of microdistortions and range of cap thickness until 1wk after surgery. In our analysis, the range of cap thickness was obtained by subtracting the value of the thinnest point from the thickest point. A larger range may aid more proper adhesion at the interface, because a more steeply curved surface accompanied with larger area. Other factors such as surgical order, refractive lenticule thickness, and preoperative corneal curvature also influence appearance of microdistortions[10]. No effects of microdistortions on visual outcomes have ever been found,and our results provided new evidence in terms of intraocular scattering. Whether microdistortion plays a protective role in corneal biomechanics and irregular cap morphology deserves further investigation.
In summary, the corneal cap is variable in the early phase and tends to stabilize 1wk after surgery. The morphology of corneal cap is weakly correlated with intraocular scattering. Despite this, microdistortion decreased with time and did not in fluence intraocular scattering; however a correlation with the range of corneal cap thickness was found until 1wk after surgery.
ACKNOWLEDGEMENTS
Authors' contributions:Yu ZQ conducted the conception and design of the study, acquisition and interpretation of data,and final approval of the version to be published. Fu D conducted acquisition and interpretation of data, analysis and interpretation of data, writing and revising the article, and final approval of the version to be published. Wang L conducted acquisition of data and final approval of the version to be published.
Conflicts of Interest:Fu D, None; Wang L, None; Zhou XT,None; Yu ZQ, None.
REFERENCES
1 Fernández J, Valero A, Martínez J, Piñero DP, Rodríguez-Vallejo M.Short-term outcomes of small-incision lenticule extraction (SMILE) for low, medium, and high myopia. Eur J Ophthalmol 2017;27(2):153-159.
2 Xu Y, Yang Y. Small-incision lenticule extraction for myopia: results of a 12-month prospective study. Optom Vis Sci 2015;92(1):123-131.
3 Sinha Roy A, Dupps WJ Jr, Roberts CJ. Comparison of biomechanical effects of small-incision lenticule extraction and laser in situ keratomileusis: finite-element analysis. J Cataract Refract Surg 2014;40(6):971-980.
4 Shen Z, Shi K, Yu Y, Yu X, Lin Y, Yao K. Small incision lenticule extraction (SMILE) versus femtosecond laser-assisted in situ keratomileusis (FS-LASIK) for myopia: A systematic review and Metaanalysis. PLoS One 2016;11(7):e158176.
5 Wu W, Wang Y. Corneal higher-order aberrations of the anterior surface,posterior surface, and total cornea after SMILE, FS-LASIK, and FLEx surgeries. Eye Contact Lens 2016;42(6):358-365.
6 Schallhorn S, Brown M, Venter J, Hettinger K, Hannan S. The role of the mesopic pupil on patient-reportedoutcomes in young patients with myopia 1mo after wavefront-guided LASIK. J Refract Surg 2014;30(3):159-165.
7 Dong Z, Zhou X, Wu J, Zhang Z, Li T, Zhou Z, Zhang S, Li G. Small incision lenticule extraction (SMILE) and femtosecond laser LASIK:comparison of corneal wound healing and in flammation. Br J Ophthalmol 2014;98(2):263-269.
8 Lazaridis A, Droutsas K, Sekundo W. Topographic analysis of the centration of the treatment zone after SMILE for myopia and comparison to FS-LASIK: subjective versus objective alignment. J Refract Surg 2014;30(10):680-686.
9 Zhao J, Yao P, Li M, Chen Z, Shen Y, Zhao Z, Zhou Z, Zhou X. The morphology of corneal cap and its relation to refractive outcomes in femtosecond laser small incision lenticule extraction (SMILE) with anterior segment optical coherence tomography observation. PLoS One 2013;8(8):e70208.
10 Yao P, Zhao J, Li M, Shen Y, Dong Z, Zhou X. Microdistortions in Bowman's layer following femtosecond laser small incision lenticule extraction observed by Fourier-Domain OCT. J Refract Surg 2013;29(10):668-674.
11 He M, Wang W, Ding H, Zhong X. Comparison of two cap thickness in small incision lenticule extraction: 100μm versus 160μm. PLoS One 2016;11(9):e0163259.
12 Güell JL, Verdaguer P, Mateu-Figueras G, Elies D, Gris O, El Husseiny MA, Manero F, Morral M. SMILE procedures with four different cap thicknesses for the correction of myopia and myopic astigmatism. J Refract Surg 2015;31(9):580-585.
13 Alberto D, Garello R. Corneal sublayers thickness estimation obtained by high-resolution FD-OCT. Int J Biomed Imaging 2013;2013: 989624.
14 Li Y, Tan O, Brass R, Weiss JL, Huang D. Corneal epithelial thickness mapping by Fourier-domain optical coherence tomography in normal and keratoconic eyes. Ophthalmology 2012;119(12):2425-2433.
15 Moshirfar M, McCaughey MV, Reinstein DZ, Shah R, Santiago-Caban L, Fenzl CR. Small-incision lenticule extraction. J Cataract Refract Surg 2015;41(3):652-665.
16 Ozgurhan EB, Agca A, Bozkurt E, Gencer B, Celik U, Cankaya KI,Demirok A, Yilmaz OF. Accuracy and precision of cap thickness in small incision lenticule extraction. Clin Ophthalmol 2013;7:923-926.
17 Reinstein DZ, Carp GI, Archer TJ, Gobbe M. Outcomes of small incision lenticule extraction (SMILE) in low myopia. J Refract Surg 2014;30(12):812-818.
18 Kamiya K, Shimizu K, Igarashi A, Kobashi H. Visual and refractive outcomes of femtosecond lenticule extraction and small-incision lenticule extraction for myopia. Am J Ophthalmol 2014;157(1):128-134.e2.
19 Tian M, Miao H, Shen Y, Gao J, Mo X, Zhou X. Intra- and intersession repeatability of an optical quality and intraocular scattering measurement system in children. PLoS One 2015;10(11):e142189.
20 Iijima A, Shimizu K, Kobashi H, Saito A, Kamiya K. Repeatability,reproducibility, and comparability of subjective and objective measurements of intraocular forward scattering in healthy subjects.Biomed Res Int 2015;2015:925217.
21 Miao H, He L, Shen Y, Li M, Yu Y, Zhou X. Optical quality and intraocular scattering after femtosecond laser small incision lenticule extraction. J Refract Surg 2014;30(5):296-302.
22 Ondategui JC, Vilaseca M, Arjona M, Montasell A, Cardona G, Güell JL, Pujol J. Optical quality after myopic photorefractive keratectomy and laser in situ keratomileusis: comparison using a double-pass system. J Cataract Refract Surg 2012;38(1):16-27.
23 Cheng X, Petsche SJ, Pinsky PM. A structural model for the in vivo human cornea including collagen-swelling interaction. J R Soc Interface 2015;12(109):20150241.
24 Mohamed-Noriega K, Riau AK, Lwin NC, Chaurasia SS, Tan DT,Mehta JS. Early corneal nerve damage and recovery following small incision lenticule extraction (SMILE) and laser in situ keratomileusis(LASIK). Invest Ophthalmol Vis Sci 2014;55(3):1823-1834.
25 Dawson DG, Grossniklaus HE, McCarey BE, Edelhauser HF.Biomechanical and wound healing characteristics of corneas after excimer laser keratorefractive surgery: is there a difference between advanced surface ablation and sub-Bowman's keratomileusis? J Refract Surg 2008;24(1):S90-S96.
26 Shah R, Shah S. Effect of scanning patterns on the results of femtosecond laser lenticule extraction refractive surgery. J Cataract Refract Surg 2011;37(9):1636-1647.
27 Reinstein DZ, Archer TJ, Gobbe M. Accuracy and reproducibility of cap thickness in small incision lenticule extraction. J Refract Surg 2013;29(12):810-815.
28 Vestergaard AH, Grauslund J, Ivarsen AR, Hjortdal JØ. Efficacy,safety, predictability, contrast sensitivity, and aberrations after femtosecond laser lenticule extraction. J Cataract Refract Surg 2014;40(3):403-411.
29 Kamiya K, Shimizu K, Igarashi A, Kobashi H. Effect of femtosecond laser setting on visual performance after small-incision lenticule extraction for myopia. Br J Ophthalmol 2015;99(10):1381-1387.
30 Yadav R, Kottaiyan R, Ahmad K, Yoon G. Epithelium and Bowman's layer thickness and light scatter in keratoconic cornea evaluated using ultrahigh resolution optical coherence tomography. J Biomed Opt 2012;17(11):116010.