INTRODUCTION
Infantile esotropia (IET) is a common type of infantile strabismus affecting 0.5% to 1% of children and usually occurs within thefirst 6mo of their life[1-3].
Most IET cases should undergo surgery to achieve ocular alignment, and 20% to 40% of them require reoperation, due to residual or recurrent esotropia[1-2,4-5]. These surgical procedures impose psychological and financial pressure on patients’families. According to different reports, some factors have been introduced as known predisposing risk factors of reoperation like surgical age younger than 15mo[6]and higher angle of deviation [values of esotropia >30[1]and >50[7]prism diopters(PD)]. Hyperopia less than 3.00 D, amblyopia, positive family history, nystagmus, inferior oblique overaction (IOOA),dissociated vertical deviation (DVD) and abduction deficit have also been considered as accompanying factors in this regard, whereas there is no consensus among practitioners on all of them[6,8-10]. Some IET subjects show different severities of abduction deficit which is due to contraction of their medial rectus (MR) muscles or lateral rectus (LR) underaction, or lack of nasotemporal pursuit development in IET patients after 6mo of age that should be recognized from 6thnerve paresis and Duane’s syndrome[9].
Doll’s head maneuver can distinguish true 6thnerve paresis from pseudoparalysis of LR muscle by stimulation of vestibular system in young children with abduction deficit[11].Also, lack of any changes in the size of eyelidfissure or globe retraction in lateral gazes, highly exclude Duane’s syndrome diagnosis.
According to the literature review, abduction deficit[1], preoperative angle of esotropia about 40 to 60 PD[3]and nystagmus[5]have been suggested as the probable risk factors of reoperation in these patients and should be attended before surgery.
In addition, the effective role of motor dysfunction especially when there is loss of LR in IET monkeys has been reported in another study[4]. They also reported that larger horizontal rectus muscles, can be considered as another etiologic factor.
As it was mentioned, a few authors have studied the role of clinical abduction deficit on the reoperation rate in IET cases,therefore we aimed to focus on the relationship of this factor and the reoperation rate in IET patients.
SUBJECTS AND METHODS
This retrospective study included records of 216 patients (432 eyes) with IET who had a history of surgery either at Torfeh Eye Hospital or Imam Hossein Medical Center, Tehran, Iran,from 2010 to 2015. This study was approved by the Ethic Committee of Ophthalmic Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Patients with a history of esotropia up to age of 6mo,preoperative stable deviation in two examinations with at least 2wk apart, and a minimum three months of postoperative follow up were included in the study. Those patients with a history of previous strabismus surgery, variable deviations,early onset accommodative esotropia (age of deviation from 6mo to 2y and hyperopia >+4.00 D[12]), congenital cataract,retinopathy of prematurity (ROP), manifest nystagmus, fundus lesions, neurological problem or ophthalmic anomalies, 6thnerve palsy, preoperative negative Doll’s head maneuver and abduction deficit of -4, Duane’s syndrome and lost records were excluded from this study.

Figure 1 Drawing and designation in different grades of abduction deficit No abduction deficit (0): Complete movement from primary position towards lateral canthus; Abduction deficit (-1):Completed 3/4 of distance towards lateral canthus; Abduction deficit(-2): Completed 2/4 of distance towards lateral canthus; Abduction deficit (-3): Completed 1/4 of distance towards lateral canthus;Abduction deficit (-4): No movement from primary position towards lateral canthus.
The epidemiologic factors such as parents consanguinity,prematurity (birth age less than 36wk[13], sex and age at the first operation were recorded. Also complete eye examinations including fixational status [center, steady,maintenance (CSM)], amblyopia (fixation preference of one eye comparing to the other eye or difference of two lines of best corrected visual acuity (BCVA) between two eyes in children over 3y)[14], cyclorefraction (30-45min after instillation of one drop cyclopentolate 1% and tropicamide 1% for 5min apart),extraocular muscle function (ocular version and duction using the scale of -4 to +4, if the case had -4 abduction limitation,the case would be excluded due to possibility of 6thpalsy),eye deviation tests (Krimsky method or alternate prism cover test), pattern of deviation (difference of horizontal deviation between up and down gazes ≥10 and ≥15 PD diagnosed as A and V pattern, respectively)[15], latent nystagmus, and DVD were recorded from patients’ files. If there was abduction deficit, it was graded from -1 to -4 on duction and version ocular motility test similar to Jampolsky ranking scale[12]. The ocular area from primary position towards lateral canthus was divided into 4 parts and the LR function was graded according to its limitation, which illustrated in Figure 1. Only cases with abduction deficit of -1 to -3 were included in our study.
Doll’s head maneuver was checked in all patients to distinguish true 6thnerve palsy from underaction of the LR muscle. If the result of Doll’s test was positive, 6thnerve paralysis was rejected. In addition, patients with typical eyelidfissure changes in horizontal gaze or globe retraction were also excluded due to the possibility of Duane’s syndrome.
Hyperopia, myopia and astigmatism were prescribed according to the Guideline for Refractive Correction in Infants and Young Children presented by the American Academy of Ophthalmology (AAO)[16]. Ocular patching of the dominant eye was recommended if amblyopia was diagnosed byfixation preference test or assessment of BCVA. Routinely, the first surgical procedure was bimedial rectus recession (BMR Rec), while in cases with significant fixation preference or amblyopia, recession-resection (R&R) method was also performed, all based on the standard surgical table[17]. Force duction test (FDT) was performed before the surgery on extraocular muscles under general anesthesia.
Three months after operation, children were classified into the two groups based on their post-surgical deviation: no-need reoperation group (deviation ≤15 PD), and need-reoperation group (deviation >15 PD).
Statistical Analysis All statistical analyses were performed by SPSS software version 22.0. (IBM Corp. Armonk, NY,USA). To check the normal distribution of continuous data,Shapiro-Wilks test and Q-Q plot were used. To present data we used mean, standard deviation, median and range. Chi-square,Fisher's exact test, t-test and Mann-Whitney U test were used to compare the groups in subject variables. The correlations between two eyes of the same person were considered by generalized estimating equation (GEE) analysis. P-value less than 0.05 was considered statistically significant.
RESULTS
Table 1 Epidemiologic characteristics of patients
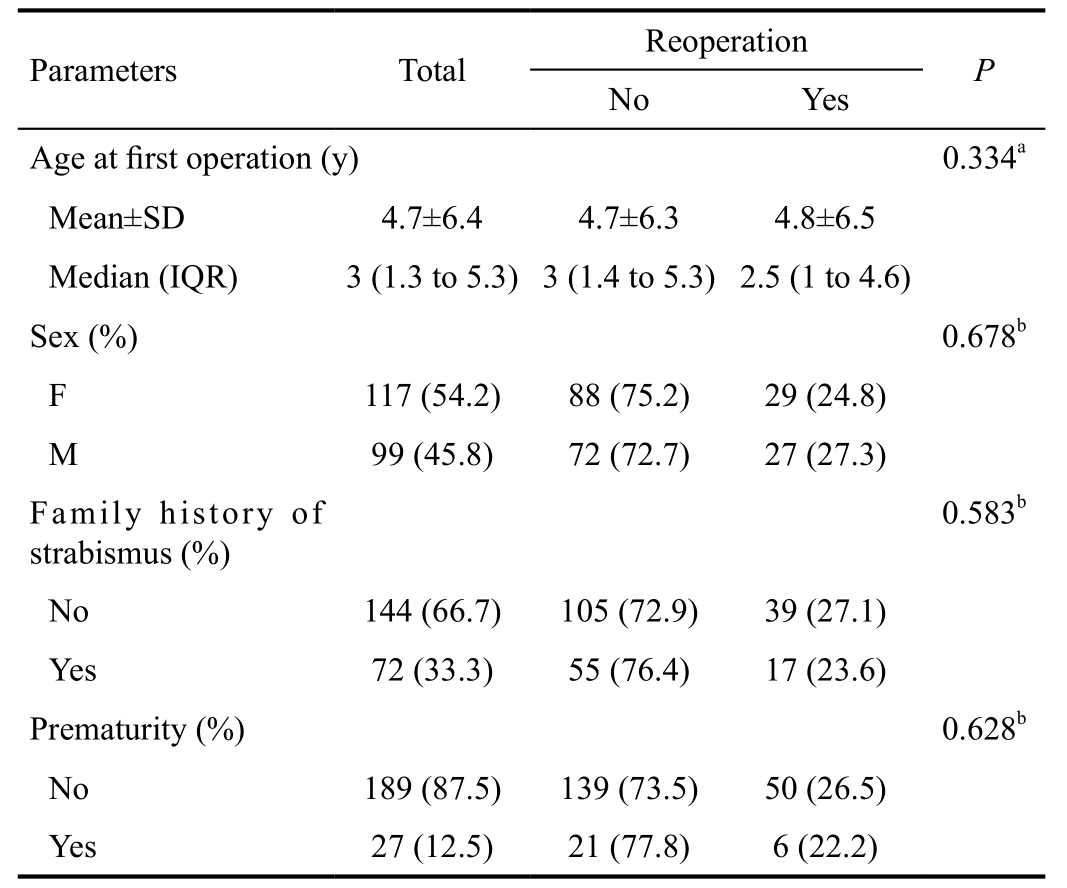
IQR: Inter-quartile range; SD: Standard deviation.aBased on Mann-Whitney U test;bBased on Chi-square test.
The epidemiologic characteristics of IET patients were shown in Table 1. There were no statistically significant difference between the no-need reoperation and need-reoperation groups regarding their surgical age, sex, family history of deviation,and prematurity.
Preoperative refractive errors and visual results were presented in Table 2. There were no differences between these groups regarding to myopia, astigmatism, anisometropia, amblyopia and spherical equivalent.
The surgical characteristics of our patients were shown in Table 3. There was not any statistically significant difference regarding the age between no-need reoperation and needreoperation groups in different surgical ages.
The mean preoperative angle of deviation was higher in needreoperation group in comparison with the no-need reoperation group (P<0.001). More reoperation rate was observed in need-reoperation group with preoperative larger esotropia(39.6%) compared to smaller esotropia (27.1%; P=0.043).There was not any difference between the types of surgery and reoperation rate, and 25% of all subjects were followed at least 4mo (IQR: 4 to 23mo). FDT under general anesthesia revealed that MR muscle had +1 restriction in 90% of our patients.
Generally, three months after surgery, 61.10%, 32.90% and 6%of the patients had orthophoria (≤10 PD), residual esotropia(under-correction of >10 PD) and consecutive exotropia (overcorrection of >10 PD), respectively.
The preoperative abduction deficit was -0.46±0.77 and it improved to -0.04±0.17 after surgery (P<0.001). A case of IET with improved abduction after BMR Rec surgery was shown in Figure 2.
The rate of reoperation was increased in cases with abduction deficit and late surgery (>2 years old, P=0.021; Table 4,Figure 3). Using logistic regression analysis, after adjusting for preoperative angle of deviation that was another risk factor of reoperation, this difference was also remained significant.Abduction deficit increased the odds of reoperation by 82%[OR=1.82, 95% confidence interval (CI)=1.05 to 3.19,P=0.003].
In addition, patients with no abduction deficit and early surgery (<2 years old) also showed higher rate of reoperation compared to the late surgery (>2 years old; P=0.019).
DISCUSSION
In this study, we focused on the relationship between abduction deficit and reoperation rate in IET patients. According to ourfindings, the rate of reoperation was increased with abduction deficit (from 16.0% to 33.3%) in patients who had a history of late surgery (>2 years old; Table 4). Abduction deficit increased the odds of reoperation by 82%.
Abduction deficit was found to be an accompanying factor of reoperation among IET cases in our previous study[1], but a few reports have previously indicated similar results[3-5],and the rate of reoperation was also raised by increasing the preoperative angle of deviation (Table 3), which is in line with other studies[6,8].
Both abduction deficit and preoperative angle of deviation showed a significant relationship with reoperation in the present study. After adjusting for preoperative angle of deviation, using logistic regression analysis, there was still a statistically significant relationship between abduction deficit and reoperation in patients with late surgery.

Figure 2 Pre- and postoperative function of LR muscle in IET patient Preoperative IET at primary position (B) with bilateral abduction deficit in both sides (A, C), orthophoria at 3mo after BMR recession surgery (E), postoperative normal LR function in both sides (D, F).
Table 2 Preoperative refractive and visual results of the eyes of IET patients

SE: Spherical equivalent; BCVA: Best corrected visual acuity; Diff: Difference; SD: Standard deviation.aBased on Fisher exact test.bBased on GEE analysis.
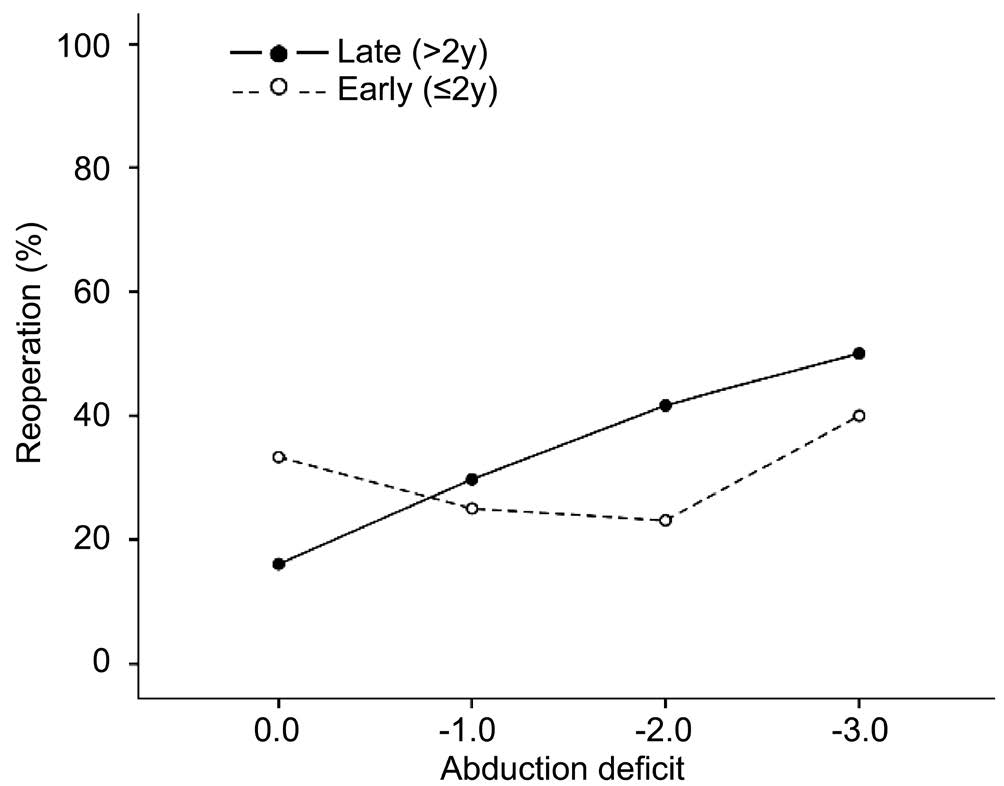
Figure 3 Percentage of reoperation according to the preoperative abduction deficit in patients with early and late surgery.
Interpretation of these results attracted our attention to the duration of esotropia. In early surgeries (<2 years of age), MR contracture has short duration while in late surgeries (>2 years of age), duration of MR contracture is longer, which may result in MR shortening. Therefore, even with equal MRs recession in both groups, reoperation may be still needed in late surgeries as it has been reported in literature that the best result of operation would be achieved within 2mo of the onset of esotropia[9].
Positive Dolls’ head maneuver before surgery and achieving all or some function of the LR muscle after BMR Rec, are two evidences to show etiological role of MR contracture. Few reports indicated similar results while Simonsz et al[17]found that abduction deficit was not related to the surgical outcomes in early versus late strabismus surgery.
Table 3 Operational characteristics of patients
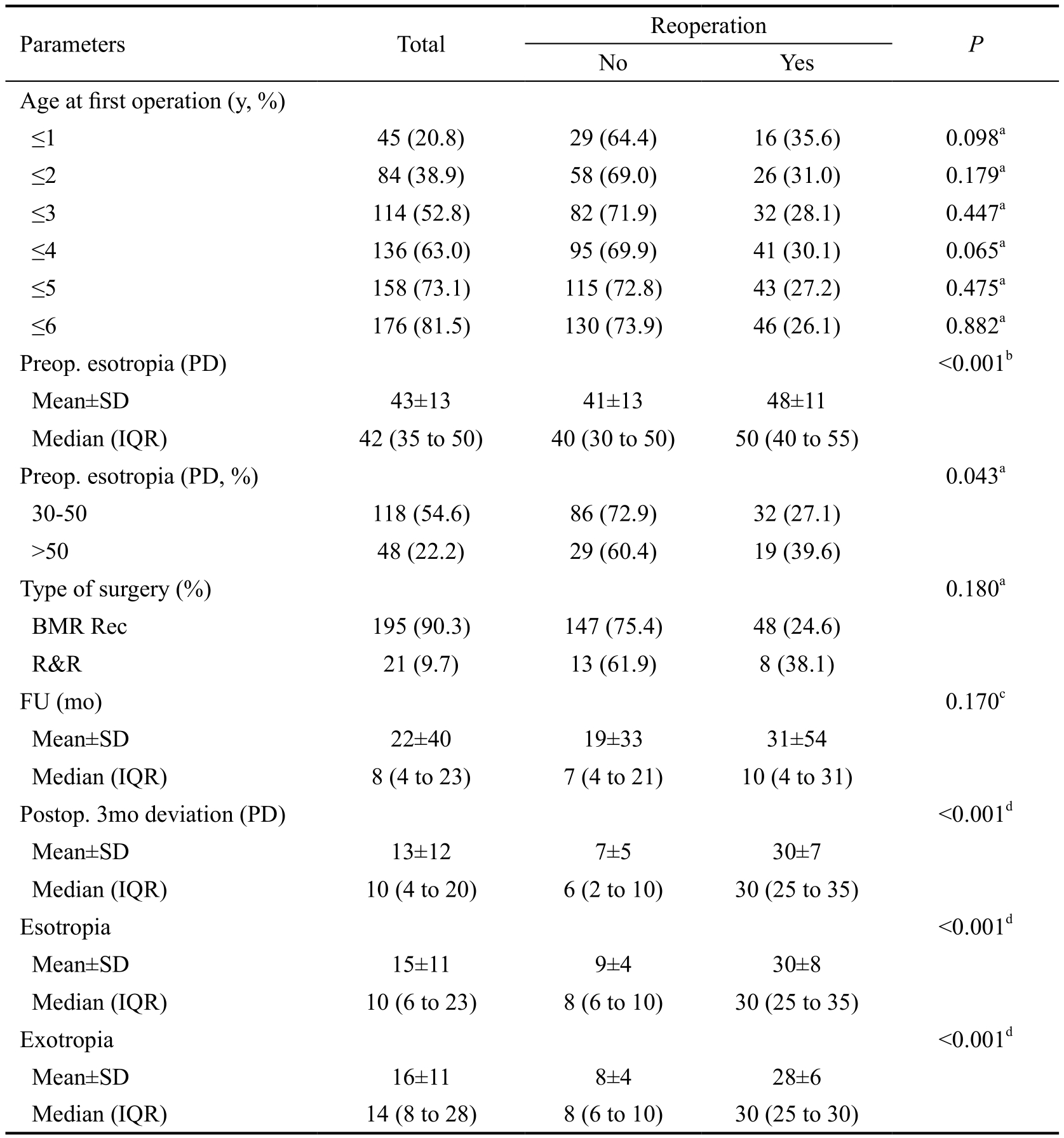
BMR Rec: Bimedial rectus recession; R&R: Recession-resection; FU: Follow up; IQR: Inter-quartile range; SD:Standard deviation; PD: Prism diopter.aBased on Chi-square test;bBased on t-test;cBased on Mann-Whitney U test;dAdjusted for the baseline value, based on analysis of covariance (ANCOVA).
Table 4 The rate of reoperation in cases with and without abduction deficit by consideration of early and late surgery

aBased on Chi-square test.
The higher rate of reoperation among IET cases with normal LR function and early surgery (33.3%, P=0.019) can be due to the lack of child’s cooperation for measurement of their deviation which has also been emphasized in literature as the higher reoperation rate with age of surgery less than 15mo of age[6].In our study, the rate of reoperation was 31.0% and 30.1%in IET cases who was operated at less than 2 and 4 years of age, respectively which was approximately in line with the European Early vs Late Infantile Strabismus Surgery Study(ELISSS) that were 28.7% and 24.6%, respectively[9]. The mean age of surgery of IET were 12-18mo for early and 24-36mo for late surgery according to the American and European standards[9], which are close to our criteria.
BMR Rec has been considered as an initial and routine type of operation in IET patients[7], in literature and our study. Due to the possibility of postoperative asymmetry and limitation of extraocular muscles in R&R surgery, we applied this method only in IET patients withfixation preference even after patching.
Our study has advantages of having large sample size,appropriate follow-up and attention to abduction deficit as a new reoperation risk factor which is only recently introduced in a few reports.
Our limitations were the less number of patients in different grades of abduction deficit (-1, -2 and -3) and early surgery group. Performing R&R surgical method on some IET patients withfixation preference can make heterogeneity of the surgical techniques that can be considered as another limitation of our study.
Based on our results, abduction deficit could be considered as a risk factor of reoperation in IET patients who were operated at the age more than 2y.
ACKNOWLEDGEMENTS
The authors would like to thank all the children and their families who participated in this study.
Conflicts of Interest:Rajavi Z, None; Sabbaghi H, None;Torkian P, None; Behradfar N, None; Yaseri M, None; Feizi M, None; Faghihi M, None; Sheibani K, None.
REFERENCES
1 Rajavi Z, Ferdosi AA, Eslamdoust M, Yaseri M, Haftabadi N, Kroji S,Sheibani K. The prevalence of reoperation and related risk factors among patients with congenital esotropia. J Pediatr Ophthalmol Strabismus 2013;50(1):53-59.
2 Rajavi Z, Ghadim HM, Ramezani A, Azemati M, Daneshvar F. Lateral rectus resection versus medial rectus re-recession for residual esotropia:early results of a randomized clinical trial. Clin Exp Ophthalmol 2007;35(6):520-526.
3 Magli A, Carelli R, Matarazzo F, Bruzzese D. Essential infantile esotropia: postoperative motor outcomes and inferential analysis of strabismus surgery. BMC Ophthalmology 2014;14:35.
4 Simonsz HJ, Eijkemans MJ. Predictive value of age, angle, and refraction on rate of reoperation and rate of spontaneous resolution in infantile esotropia. Strabismus 2010;18(3):87-97.
5 Wang T, Wang LH. Surgical treatment for residual or recurrent strabismus. Int J Ophthalmol 2014;7(6):1056-1063.
6 Trigler L, Siatkowski RM. Factors associated with horizontal reoperation in infantile esotropia. J AAPOS 2002;6(1):15-20.
7 Hug D. Management of infantile esotropia. Curr Opin Ophthalmol 2015;26(5):371-374.
8 Keenan JM, Willshaw HE. Outcome of strabismus surgery in congenital esotropia. Br J Ophthalmol 1992;76(6):342-345.
9 Magli A, Rombetto L, Matarazzo F, Carelli R. Infantile esotropia: risk factors associated with reoperation. Clin Ophthalmol 2016;10:2079-2083.
10 Von Noorden GK. Binocular vision and ocular motility: theory and management of strabismus. 6thedition. Mosby. St. Louis London Philadelphia Sydney Toronto; 2002:70-71.
11 Griffin JR, Grisham JD. Binocular anomalies: diagnosis and vision therapy. 4thedition. USA, OEP Foundation, Butterworth-Heinemann;2007:102-120.
12 Schalij-Delfos NE, de Graaf ME, Treffers WF, Engel J, Cats BP. Long term follow up of premature infants: detection of strabismus, amblyopia,and refractive errors. Br J Ophthalmol 2000;84(9):963-967.
13 Rajavi Z, Sabbaghi H, Baghini AS, Yaseri M, Moein H, Akbarian S,Behradfar N, Hosseini S, Rabei HM, Sheibani K. Prevalence of amblyopia and refractive errors among primary school children. J Ophthalmic Vis Res 2015;10(4):408-416.
14 Yam JC, Wu PK, Chong GS, Wong US, Chan CW, Ko ST. Long-term ocular alignment after bilateral lateral rectus recession in children with infantile and intermittent exotropia. J AAPOS 2012;16(3):274-279.
15 American Academy of Ophthalmology. Guideline for Refractive Correction in Infants and Young Children. Available at: https://www.aao.org/asset.axd?ID=4ca1be65-9339-4b95-882d-9e07cd625902; Accessed on 20 Jan. 2017.
16 Ansons AM, Davis H. Diagnosis and management of ocular motility disorders. 4thedition. New Jersey, United States: Wiley & Sons, Ltd;2014. Appendix: Surgical (Dose) Tables.
17 Simonsz HJ, Kolling GH, Unnebrink K. Final report of the early vs late infantile strabismus surgery study (ELISSS), a controlled, prospective,multicenter study. Strabismus 2005;13(4):169-199.