INTRODUCTION
In all over the world, cataract is the leading cause of blindness. Phacoemulsification and intraocular lens (IOL)implantation are routinely utilized as standard cataract surgical procedures[1]. Nowadays with the improved quality of people’s life, cataract surgery has developed from a procedure for removing the cloudy lens safely to that for refining to acquire the greatest extent of postoperative refractive status[2]. In spite of IOL materials and designs as well as surgical technique have improved obviously, the emphasis currently is improving functional vision and visual quality provided by IOL[3]. Glasses for near vision are usually needed after implantation of a monofocal IOL, whereas bifocal IOLs, also called multifocal IOLs, provide better uncorrected near visual acuity (UNVA)with lowering spectacle dependence.
Bifocal IOLs drops shadow multiple images on the retina,which may generate unfavorable visual symptoms such as glare, halos and contrast reduction. Since the majority of bifocal IOLs have merely two focal points, near and far, the quality of intermediate visual acuity (VA) might be inadequate for functioning perfectly in daily routine life. Then trifocal IOLs appeared to improve vision acuity at intermediate distances[4]. In recent years, despite several studies were performed to compare visual outcomes with trifocal IOLs, it remains controversial whether trifocal IOLs truly have better intermediate visual acuity than bifocal IOLs. Wefind that the majority of the literatures did not describe any statistically significant differences in comparison with bifocal IOLs, or,if present, these differences were most likely small. Besides,these primary studies generally had small sample sizes and showed conflicting results, which greatly hindered researchers drawing correct conclusions.
The objective of this study was to integrate the data from as many published prospective comparative clinical trials as possible into a Meta-analysis for a comparison of the visual outcomes achieved with trifocal IOLs and bifocal IOLs.
MATERIALS AND METHODS
Literature Search Strategy The systematic review and Metaanalysis were performed without data restriction according to the recommendations of the Cochrane Collaboration and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses statement. We specified all steps and methods of this Meta-analysis in advance in a predetermined review protocol.
We searched a systematic literature review through EMBASE and PubMed databases. The title or abstract included “trifocal”and “bifocal” as keywords. Limit was placed so as to retrieve only English-language studies. We removed duplicates.Records were screened firstly by scanning the titles and abstracts to exclude the apparent irrelevant studies, secondly by reading the full texts of the remaining articles to determine whether they met the eligibility criteria. Two reviewers (Yang JJ, Li JM) independently performed these searching steps, and if agreement could not be achieved by discussion between the two reviewers, a third reviewer (Qin L) was consulted.
Inclusion Criteria and Exclusion Criteria We used the following inclusion criteria to choose published studies for this Meta-analysis: 1) study design: prospective, clinical and randomized controlled trials (RCTs), or prospective,nonrandomized, consecutive and comparative study; 2) groups and interventions: patients underwent cataract surgery with trifocal and bifocal IOL implantation in one or both eyes; 3)outcome indicators: variable quantity of the study containing whole or part information on uncorrected and corrected near, intermediate and distance VA, contrast sensitivity (CS)and subjective perception of vision quality as the primary outcomes, refractive as a secondary outcome. The exclusion criteria were as follows: other ocular diseases, past history of refractive surgery, absence of VA comparison, lack of baseline data and statistical results. When one study had multiple trials from the same team, only the most complete data set was included.
We used the logarithm of the minimum angle of resolution(logMAR) scale as the VA measurements. On this scale, lower scores indicate better vision. However, all literature only reported the CS by graph or P value. The means and standard deviations cannot be calculated through part of the data in reports. Though we tried to contact the authors to provide sufficient information, the detailed data were still not obtained.So we failed to pool analysis. Besides, questionnaires about patients’ subjective perception of vision quality differed. Thus we could not combine these outcomes in a Meta-analysis.Instead, we conducted a descriptive analysis for CS and patients’ subjective visual quality perception.
We defined postoperative refraction as a secondary outcome.We recorded cylinder, sphere and spherical equivalents in diopters for both the trifocal and the bifocal group and carried out a Meta-analysis on these results.
Data Extraction Two reviewers (Yang JJ, Li JM) independently extracted all available data from the selected articles prudently.The following categories of information were extracted: each study’s first author, study location, publication year, study design, number of eyes at final follow-up, IOL type, the last follow-up point, quality control. Inconsistencies between two reviewers were double checked by discussion until a consensus was made, and if agreement could not be achieved between the two reviewers, a third reviewer (Qin L) was consulted.
Statistical Analysis The statistical analysis was performed by Review Manager analysis software [Review Manager(RevMan) Version 5.0; Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2008, USA)]. The uncorrected and corrected near, intermediate and distance VA results were expressed as mean difference (MD) and 95%confidence interval (CI), which were presented by forest plots. The statistical significance in the level of difference was defined as P<0.05. The size of the square showed percent weight proportionally that each study contributed to the pooled estimates, and the center of the square indicated the MD. The 95%CI for the MD is represented by the horizon bisecting each square. The Chi-squared statistic was used to test heterogeneity among studies. Fixed-effects model was used if the significant evidence of statistical heterogeneity or clinical diversity was not found (P≥0.10, I2≤50%). Otherwise, random-effects model was used to account for inter-study heterogeneity (P<0.10,I2>50%). A funnel plot about the primary outcome of CDVA was used to observe the publication bias of included studies,and asymmetry plot implied probable existence of publication bias.
Heterogeneity Management We supposed that the different designs of the different IOL types would explain a part of heterogeneity of the Meta-analysis. Eight studies including monocular vision performances were divided into two subgroups according to trifocal IOL type: one for Fine Vision(Phys IOL), and one for AT Lisa tri 839MP (CZM).
RESULTS
Search Results After removing duplicates, 92 studies were identified from original electronic search. Of these studies,24 studies were excluded after first-pass review of titles, 32studies were eliminated on the basis of their abstracts for not meeting the primary selection criteria as specified earlier.After reading the full text of the remaining 36 articles in more detail, 27 studies were excluded for the following reasons: 15 studies did not provide primary outcomes and 12 studies did not fulfill the predefined inclusion criteria. Finally, 9 studies(four RCTs andfive prospective cohorts) that reported on 265 eyes with trifocal IOL implantation and 264 eyes with bifocal IOL implantation met all eligibility criteria and provided comprehensive data for our Meta-analysis (Figure 1). Eight studies including monocular vision performances could be divided into 2 subgroups: one for trifocal Fine Vision IOL (5 studies) and one for AT Lisa tri 839MP (CZM) (3 studies). One study contains only binocular data.
Table 1 Characteristics of included studies in the Meta-analysis

RCT: Randomized controlled trial; IOL: Intraocular lens.
Study Characteristics and Quality The main characteristics of included studies are recorded in Table 1, and their quality is assessed. We used the Jadad method[5]to assess the methodological quality of eligible studies. A checklist containedfive items:1) with or without randomization; 2) with or without a doubleblind design; 3) the appropriateness of the randomization methods if used; 4) the appropriateness of double-blinding design if used; 5) the analysis and reasons for withdrawals and dropouts. The scale of each item is assigned 0 or 1. Therefore,poor quality of studies can gain a Jadad score of no more than 2, good quality if the score was 3 or 4, and excellent quality if the score was 5.
Meta-analysis Results
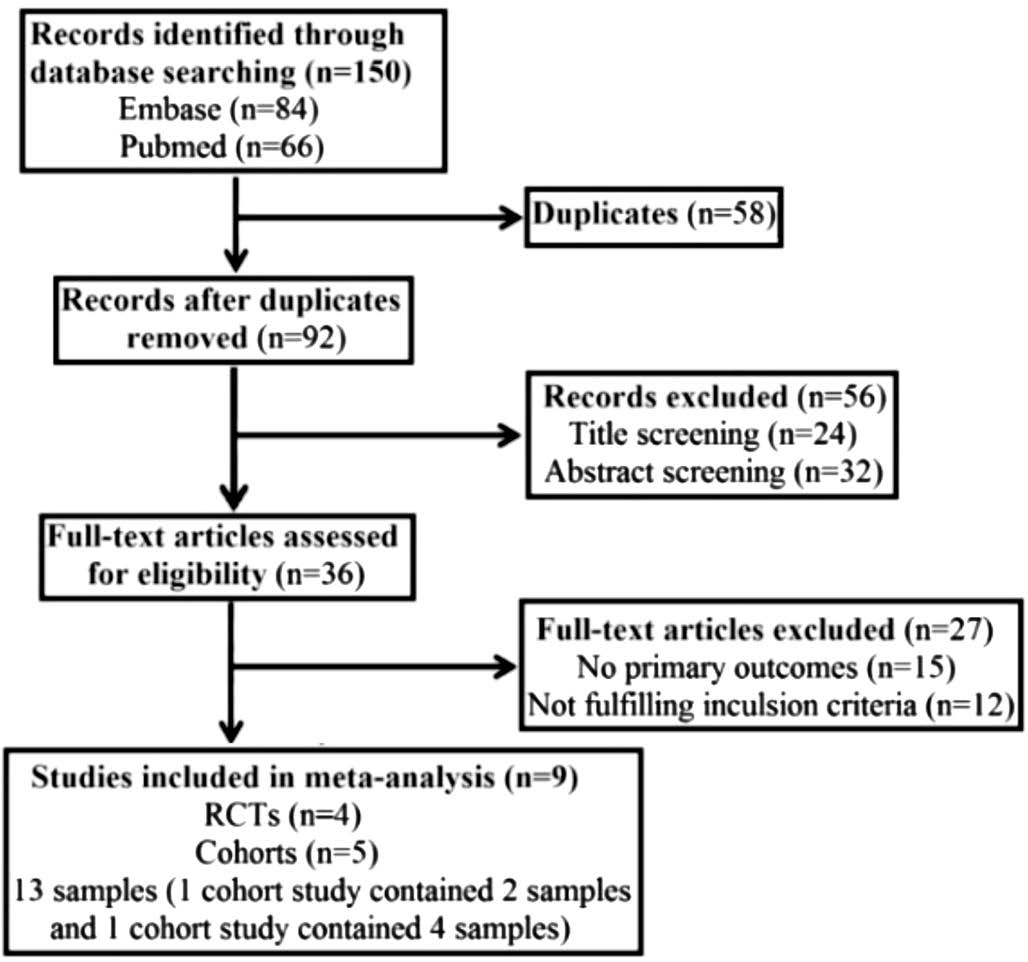
Figure 1 Flow diagram of study selection process RCTs: Randomized controlled trials.
Visual acuity Six studies reported monocular uncorrected distance visual acuity (UDVA) and eight studies reported monocular corrected distance visual acuity (CDVA) as outcomes, and each analysis results were presented in a forest plot (Figure 2A and 2B). There was a statistically significant but small difference in the overall effect that favored trifocal IOLs with better vision (MD=-0.06; 95%CI, -0.10 to -0.02;Z=2.90, P=0.004 for UDVA, and MD=-0.02; 95%CI, -0.03 to 0.00; Z=2.02, P=0.04 for CDVA). The quality of the evidence was low because not all studies were RCTs and characterized by high heterogeneity (I2=65%, τ2=0.00 for UDVA and I2=69%, τ2=0.00 for CDVA). But the studies in Fine Vision lens subgroup were characterized by low heterogeneity (I2=38%,τ2=0.00 for UDVA and I2=0%, τ2=0.00 for CDVA) and only one study was not RCT for analysis, which showed a small difference (MD=-0.04; 95%CI, -0.08 to 0.00; Z=2.13, P=0.03)
for UDVA but not for CDVA (MD=0.00; 95%CI, -0.01 to 0.01;Z=0.43, P=0.67). The quality of the evidence was moderate to high.
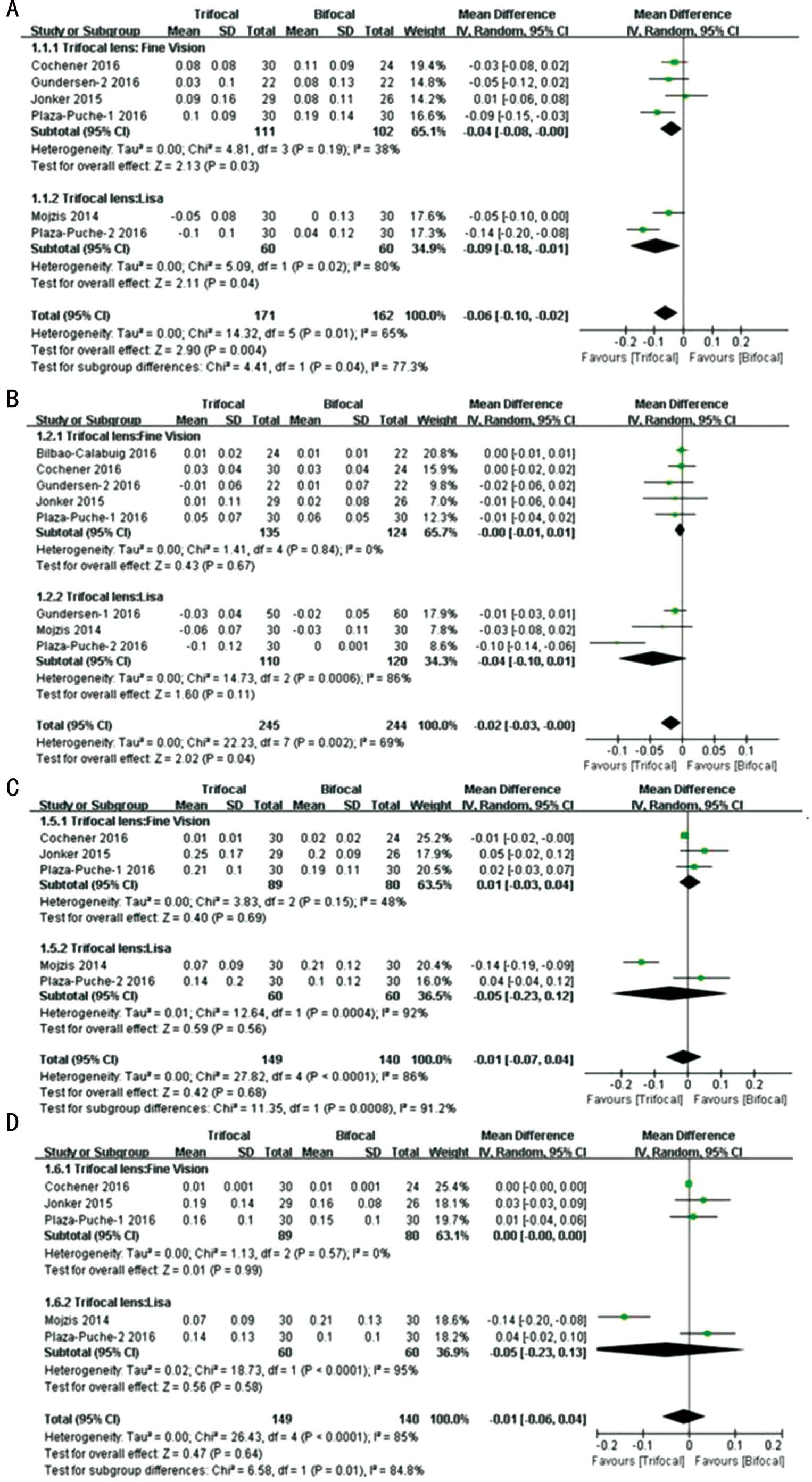
Figure 2 Subgroup analysis of postoperative monocular UDVA, CDVA, UNVA, DCNVA This forest plot showed the mean difference in visual acuity (logMAR) along with associated 95% CI, comparing the implantation of trifocal with bifocal IOLs. A: Forest plot showing the MD of UDVA; B: Forest plot showing the MD of CDVA; C: Forest plot showing the MD of UNVA; D: Forest plot showing the MD of DCNVA; In bold: subgroup and totalfinding of effect size calculation with the random effect model; the diamond shows the mean effect size and its standard deviation. CI: Confidence interval; df: Degrees of freedom; IOL: Intraocular lens; IV: Inverse variance; SD: Standard deviation.
Five studies reported postoperative monocular uncorrected near visual acuity (UNVA) and distance-corrected near visual acuity (DCNVA) as outcomes (Figure 2C and 2D). There was no significant difference between trifocal and bifocal groups in the overall effect (MD=-0.01; 95%CI, -0.07 to 0.04; Z=0.42,P=0.68 for UNVA, and MD=-0.01; 95%CI, -0.06 to 0.04;Z=0.47, P=0.64 for DCNVA). The quality of the evidence was low. All studies were characterized by high heterogeneity(I2=86%, τ2=0.00 for UNVA and I2=85%, τ2=0.00 for DCNVA). We made analysis again after excluding one trial (Mojzis et al[6]) because of its significant problems of comparability with other studies, low heterogeneity was gotten(I2=41%, τ2=0.00 for UNVA and I2=0, τ2=0.00 for DCNVA).But the results still did not show significant difference between the two groups.
Two studies reported postoperative monocular uncorrected intermediate visual acuity (UIVA) and distance-corrected intermediate visual acuity (DCIVA) as outcomes (Figure 3A and 3B). There was no significant difference between trifocal and bifocal groups in the overall effect (MD=-0.10; 95%CI,-0.36 to 0.17; Z=0.71, P=0.48 for UIVA, and MD=-0.12;95%CI, -0.36 to 0.13; Z=0.93, P=0.35 for DCNVA). Both were characterized by high heterogeneity (I2=96%, τ2=0.03).The quality of the evidence was low.
Three studies reported postoperative binocular UDVA, UIVA and UNVA as outcomes (Figure 4A-4C). There was no significant difference between trifocal and bifocal groups in the overall effect (MD=-0.04; 95%CI, -0.08 to 0.00; Z=1.91,P=0.06 for UDVA and MD=-0.04; 95%CI, -0.09 to 0.02;Z=1.39, P=0.16 for UIVA, and MD=-0.03; 95%CI, -0.10 to 0.05;Z=0.69, P=0.49 for UNVA). All studies were characterized by high heterogeneity (I2=51%, τ2=0.00 for UDVA and I2=65%,τ2=0.00 for UIVA and I2=95%, τ2=0.00 for UNVA). The quality of the evidence was low.
Contrast sensitivity Six studies evaluated the CS of trifocal IOLs and bifocal IOLs after implantation (Table 2).These studies differed between light conditions and spatial frequencies. Under photopic conditions, Mojzis et al[6]reported that there was a significantly higher level of CS at a frequency of 3 cycles per degree (cpd) in the trifocal group than in the bifocal group. Vilar et al[13]reported that the trifocal group showed better results for CS at 6, 12 and 18 cpd without glare,and at 18 cpd with glare. However, no significant difference between the two groups was seen in Jonker et al’s[4]and Cochener’s[8]studies. Under mesopic conditions, Jonker et al[4]reported that CS value was significantly better for 6 cpd in the bifocal group compared to the trifocal group. Vilar et al[13]reported that the bifocal group showed better results for CS at 3, 6 and 12 cpd, but the trifocal group showed better CS at 1.5 cpd with glare. However, no significant difference in CS between the two groups was reported in Bilbao-Calabuig et al’s[7]and Plaza-Puche et al’s[12]studies.
Subjective visual quality and complications Four studies used questionnaires to record complications and compare visual quality of trifocal IOLs versus bifocal IOLs. Because these studies used different questionnaires and these outcome measures were not consistent, it was impossible to make comparisons directly regarding complications or the visual quality, such as glare, reading speed and spectacle independence. So we carried out a descriptive analysis with results shown in Table 3. There was no statistically significant difference with respect to visual disturbances and glare between two groups in most studies.However, Jonker et al[4]and Cochener[8]reported that more frequently complete spectacle independence was achieved in the trifocal subjects than bifocal subjects. Visual disturbances was fewer bothersome with bifocal than trifocal implants in Gundersen and Potvin’s[9]study (P=0.045).
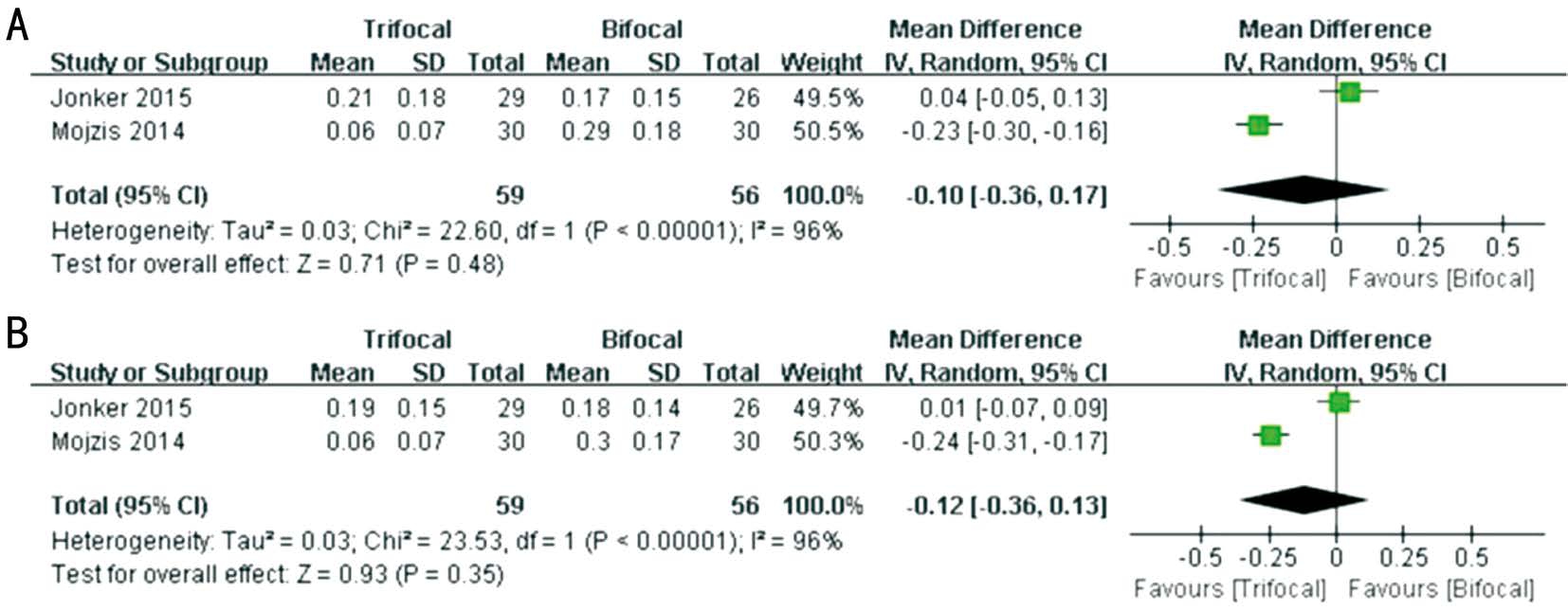
Figure 3 Random effects pooled estimates of postoperative monocular UIVA and DCIVA This forest plot showed the mean difference in visual acuity (logMAR) along with associated 95% CI, comparing the implantation of trifocal with bifocal IOLs. A: Forest plot showing the MD of UIVA; B: Forest plot showing the MD of DCIVA.

Figure 4 Random effects pooled estimates of postoperative binocular UDVA, UIVA and UNVA This forest plot showed the mean difference in visual acuity (logMAR) along with associated 95%CI, comparing the implantation of trifocal with bifocal IOLs. A: Forest plot showing the MD of UDVA; B: Forest plot showing the MD of UIVA; C: Forest plot showing the MD of UNVA.
Table 2 Comparison of postoperative mean contrast sensitivity in two groups
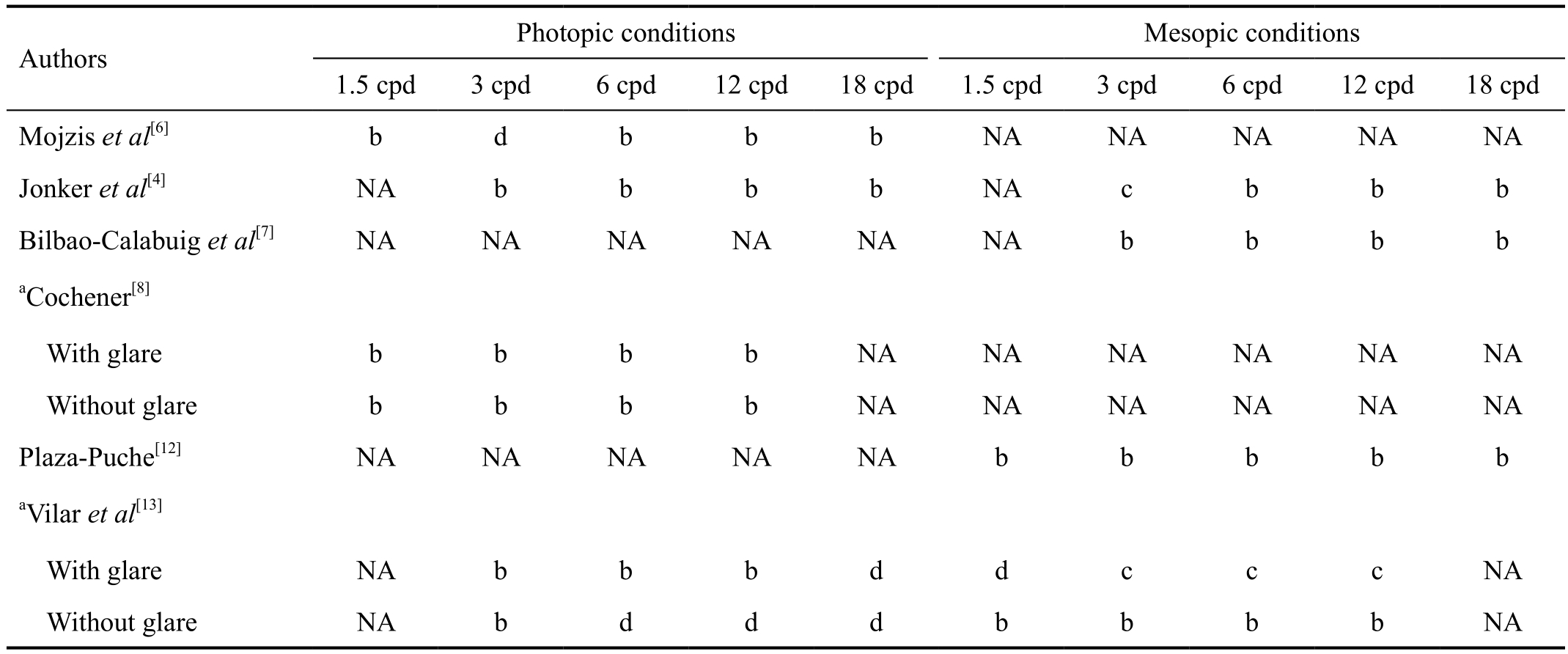
awith and without glare;bNo statistically significant difference;cSignificantly higher in bifocal group;dSignificantly higher in trifocal group. NA: Not available; cpd: Cycles per degree.
Refraction Postoperative refraction was reported in 6 studies (Figure 5A-5C). There was no significant difference between trifocal and bifocal groups in the overall effect(MD=0.09; 95%CI, -0.05 to 0.23; Z=1.29, P=0.20 for cylinder, MD=0.12; 95%CI, -0.13 to 0.37; Z=0.95, P=0.34 for sphere, and MD=0.03; 95%CI, -0.06 to 0.13; Z=0.73, P=0.47 for spherical equivalent). All studies were characterized by high heterogeneity (I2=67%, τ2=0.02 for cylinder, and I2=74%, τ2=0.04 for sphere), except for spherical equivalent characterized by low heterogeneity (I2=0). A subgroup analysis showed that there was no significant difference between Fine Vision IOL with a bifocal IOL in cylinder (MD= -0.04;95%CI, -0.30 to 0.22; Z=0.30, P=0.76 for cylinder, and MD=0.01; 95%CI, -0.14 to 0.17; Z=0.17, P=0.87 for spherical equivalent).
Publication Bias Funnel plot was performed to assess the publication bias of literatures (Figure 6). The symmetrical funnel plots provide no evidence for publication bias in the eight publications.

Figure 5 Random effects pooled estimates of postoperative cylinder (D), sphere (D) and spherical equivalent (SE; D) This forest plot showed the mean difference in visual acuity (logMAR) along with associated 95% CI, comparing the implantation of trifocal with bifocal IOLs. A: Forest plot showing the MD of cylinder; B: Forest plot showing the MD of sphere; C: Forest plot showing the MD of SE.
Table 3 Summary of subjective visual quality perception and complications as reported in questionnaires
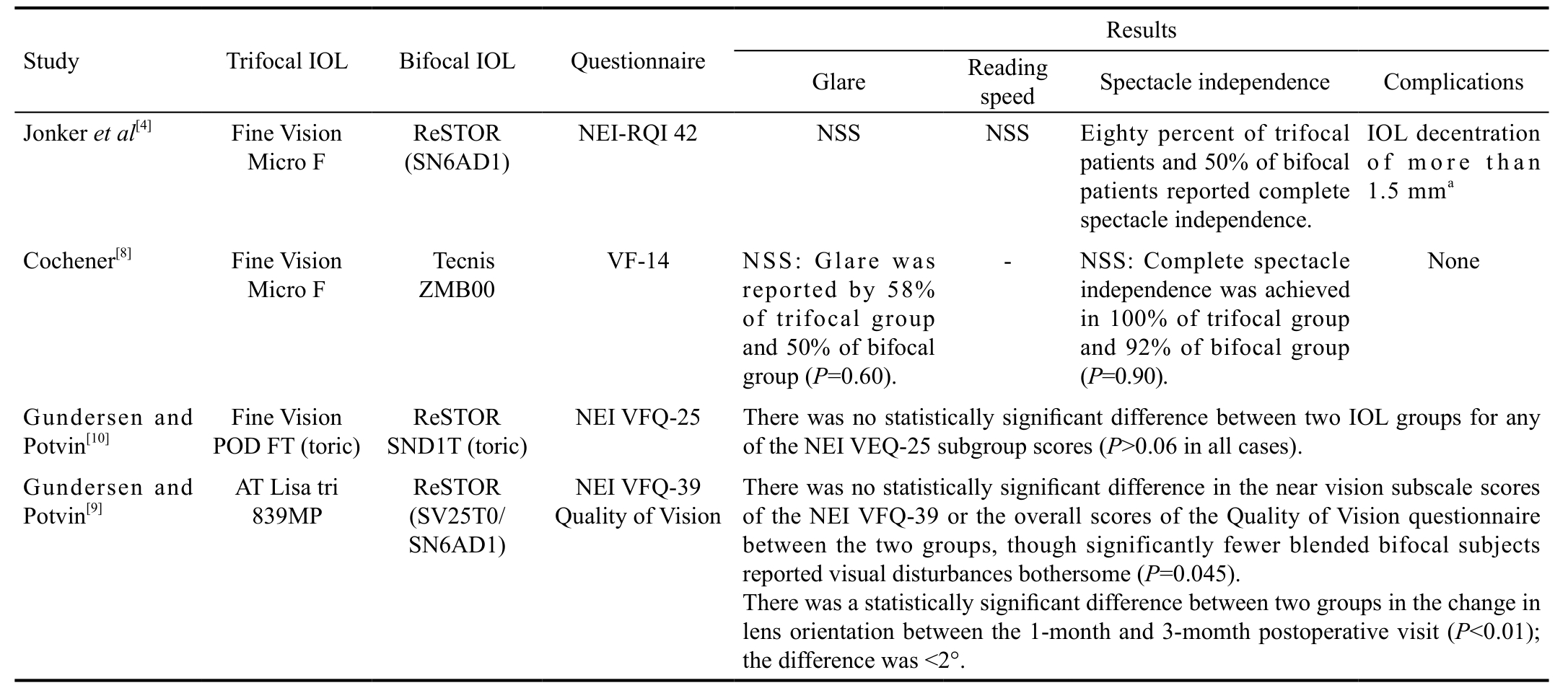
aBoth eyes of 1 patient (6.6%) in the trifocal group, 1 eye (3.8%) of 1 patient in the bifocal group. NSS: Not statistically significant; IOL: Intraocular lens; NEI RQL 42: National Eye Institute Refractive Error Correction Quality of Life Instrument-42; VF-14: Visual Function Index-14; NEI VFQ: National Eye Institute Visual Function Questionnaire.
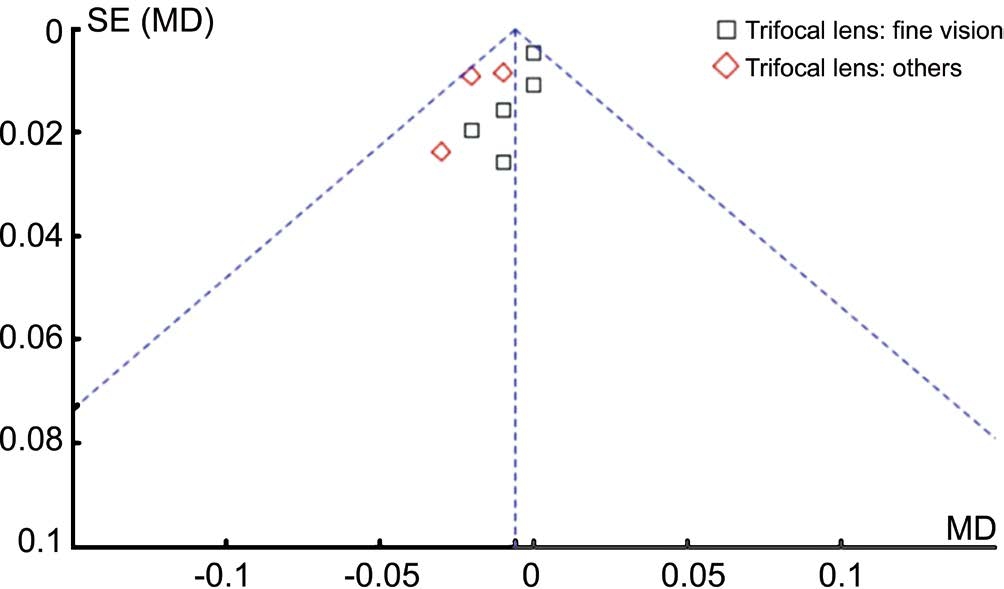
Figure 6 Funnel plot for the results between trifocal and bifocal IOLs.
DISCUSSION
In our study, we determined whether and to what extent trifocal IOL perform superior to bifocal IOL at several aspects including VA, refraction, CS and visual quality questionnaire results (including complications). No statistically significant difference were found in monocular UIVA, DCIVA, UNVA,DCNVA, refraction and binocular UDVA, UIVA, UNVA between two groups, whereas statistically significant difference in monocular UDVA and CDVA, that favored trifocal IOLs with better vision. However, the studies were similar infinding no difference in monocular CDVA between Fine Vision trifocal IOL and bifocal IOL by subgroup analysis. CS and visual quality questionnaire results were recorded but could not make definitive conclusions.
Data based on monocular UDVA and CDVA showed that trifocal IOL implantation provided better vision but small difference in the overall effect. However, when subgroup analysis with regard to trifocal IOL types performed, only 2 studies from Fine Vision subgroup and 1 study from Lisa subgroup demonstrated a statistically significant advantage in trifocal IOL implantation. So the data on monocular UDVA and CDVA do not suggest that the effect of trifocal IOL implantation would clinically outperform bifocal IOL implantation. The results confirmed that the additional intermediate focal point in trifocal IOLs did not result in a decline of the distance focal point[6].
The result with regard to monocular UIVA and DCIVA would not be credible because of only 2 studies available with high heterogeneity. In terms of monocular UNVA and DCNVA,there was no significant difference between two groups. But the quality of the evidence was low due to the study design and high heterogeneity. At least, we should note that the generation of a third focal point with trifocal IOLs was not harmful to the near vision[10]. We found in Mojzis et al’s[6]study, some important factors including the preoperative CDVA, DCIVA,IOL power and age differed significantly between two groups.Thus this study’s potential limitation of comparability was the main reason of high heterogeneity for the effect estimates.However, the result did not change after excluding this study.Different from the published review by Shen et al[14], we conducted a Meta-analysis on binocular vision performance by adding one included study by Vilar et al[13]. In terms of postoperative binocular uncorrected distance, intermediate,and near vision, there was no significant difference between trifocal and bifocal groups, but the result would not be reliable due to high heterogeneity.
It is important to analyze refraction and CS to understand the visual quality obtained with multifocal IOLs. No significant difference was found in terms of refraction,however, characterized by high heterogeneity for cylinder and sphere, while spherical equivalent was characterized by low heterogeneity. A decrease in CS is well-known side effect of multifocal IOLs[4]. Our study found that CS with trifocal IOLs was not lower than bifocal IOLs in most studies. It is may a possible explanation that a smaller percentage of energy is allocated to intermediate vision than to distance and near vision[15].
Except for the clinical measurements of visual function(VA and CS), questionnaire such as National Eye Institute Refractive Error Correction Quality of Life Instrument-42 (NEI RQL 420), the Visual Function Index-14 (VF-14) and National Eye Institute Visual Function Questionnaire (NEI VFQ) were used to evaluate subjective visual quality. It was the high scores for almost all implants that suggested both trifocal and bifocal groups were satisfied with postoperative vision.Although Gundersen and Potvin’s[9]reported that bifocal implants experienced fewer bothersome visual disturbances than trifocal implants, the authors explained that in partly because more patients in the trifocal group were younger than the bifocal group, as the younger may had relatively higher visual demands or expectations. The outcomes also demonstrated high rates of spectacle independence in both subject groups, particularly in the trifocal group.
As far as we know, this is the second Meta-analysis of comparing the trifocal IOL with the bifocal IOL. In this Metaanalysis, it should be paid attention that almost half of included trials were RCTs, the other half were prospective cohorts.We retained cohorts to replenish randomized trial evidence in consideration of the insufficient number of RCTs. In order to decrease the heterogeneity of the Meta-analysis, we conducted subgroups analysis according to trifocal IOL types, which was absent in the previous review by Shen et al[14]. Thus, these Meta-analysis results provided the moderate level of evidence.Nevertheless, this Meta-analysis has its own limitations. For instance, the examination of visual outcomes between trifocal IOL and bifocal IOL was based on merged data from trails of different follow-up durations. We chose the data reported at the last follow-up point for comparison. Besides, numbers of studies included are not greatly sufficient to show the true difference between trifocal IOL and bifocal IOL. Despite this Meta-analysis has several limitations as described above,it is noted that this study confirms that trifocal IOL doesn’t decrease distance and near vision by dedicating some energy to intermediate vision. Also, our research lays useful evidence for future large scale patients-based prospective controlled trials. Further well-designed studies with a larger sample size are required.
In conclusion, trifocal IOL and bifocal IOL had similar levels of distance and near VAs. Besides, CS and subjective visual quality had no conclusive results.
ACKNOWLEDGEMENTS
Foundations:Supported by National Natural Science Foundation of China (No.81741058; No.81460163; No.81400427; No.81300786);Fundamental Research Funds for the Central Universities(No.xjj2015015); Research Grants from Shaanxi Provincial Department of Science and Technology (No.2016KJXX-12;No.2016JM8029); Specialized Research Fund for the Doctoral Program of Higher Education (No.20133601120012); Research Grants from Jiangxi Provincial Department of Science and Technology (No.20142BAB215029; No.20132BAB205024;No.20142BDH80005); Research Grants from Education Department of Jiangxi Province (No.GJJ14094; No.GJJ13175).
conflicts of Interest:Yang JJ, None; Liu QP, None; Li JM,None; Qin L, None.
REFERENCES
1 Liu JP, Zhang F, Zhao JY, Ma LW, Zhang JS. Visual function and higher order aberration after implantation of aspheric and spherical multifocal intraocular lenses: a meta-analysis. Int J Ophthalmol 2013;6(5):690-695.
2 Liu J, Zhao J, Ma L, Liu G, Wu D, Zhang J. Contrast sensitivity and spherical aberration in eyes implanted with AcrySof IQ and AcrySof Natural intraocular lens: the results of a meta-analysis. PLoS One 2013;8(10):e77860.
3 Olawoye O, Ashaye A, Bekibele C, Ajuwon AJ. Quality-of-life and visual function after manual small incision cataract surgery in South Western Nigeria. West Afr J Med 2012;31(2):114-119.
4 Jonker SMR, Bauer NJC, Makhotkina NY, Berendschot TTJM, Van Den Biggelaar FJHM, Nuijts RMMA. Comparison of a trifocal intraocular lens with a +3.0 D bifocal IOL: results of a prospective randomized clinical trial presented at the XXXI Congress of the European Society of Cataract and Refractive Surgeons, Amsterdam, the Netherlands, October 2013. J Cataract Refract Surg 2015;41(8):1631-1640.
5 Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996;17(1):1-12.
6 Mojzis P, Kukuckova L, Majerova K, Liehneova K, Pinero DP.Comparative analysis of the visual performance after cataract surgery with implantation of a bifocal or trifocal diffractive IOL. J Refract Surg 2014;30(10):666-672.
7 Bilbao-Calabuig R, González-López F, Amparo F, Alvarez G, Patel SR,Llovet-Osuna F. Comparison between mix-and-match implantation of bifocal intraocular lenses and bilateral implantation of trifocal intraocular lenses. J Refract Surg 2016;32(10):659-663.
8 Cochener B. Prospective clinical comparison of patient outcomes following implantation of trifocal or bifocal intraocular lenses. J Refract Surg 2016;32(3):146-151.
9 Gundersen KG, Potvin R. Comparison of visual outcomes and subjective visual quality after bilateral implantation of a diffractive trifocal intraocular lens and blended implantation of apodized diffractive bifocal intraocular lenses. Clin Ophthalmol 2016;10:805-811.
10 Gundersen KG, Potvin R. Comparison of visual outcomes after implantation of diffractive trifocal toric intraocular lens and a diffractive apodized bifocal toric intraocular lens. Clin Ophthalmol 2016;10:455-461.
11 Plaza-Puche AB, Alio JL. Analysis of defocus curves of different modern multifocal intraocular lenses. Eur J Ophthalmol 2016;26(5):412-417.
12 Plaza-Puche AB, Alio JL, Sala E, Mojzis P. Impact of low mesopic contrast sensitivity outcomes in different types of modern multifocal intraocular lenses. Eur J Ophthalmol 2016;26(6):612-617.
13 Vilar C, Hida WT, de Medeiros AL, Magalhães KRP, Tzelikis PFM,Chaves MAPD, Pimenta Motta AF, Carricondo PC, Alves MR, Nosé W. Comparison between bilateral implantation of a trifocal intraocular lens and blended implantation of two bifocal intraocular lenses. Clin Ophthalmol 2017;11:1393-1397.
14 Shen Z, Lin Y, Zhu Y, Liu X, Yan J, Yao K. Clinical comparison of patient outcomes following implantation of trifocal or bifocal intraocular lenses: a systematic review and meta-analysis. Sci Rep 2017;7:45337.
15 Vryghem JC, Heireman S. Visual performance after the implantation of a new trifocal intraocular lens. Clin Ophthalmol 2013;7:1957-1965.