INTRODUCTION
The use of video display units (VDU) has become a huge part of daily life for working, studying and leisure activities with an increasing preference for smaller-screen devices, such as tablets, laptops and smartphones[1-2]. However,the increasing use of VDU has caused a high incidence of various eye problems[3-12], which are commonly presented in three areas: visual problems, disorders of the ocular surface(dry eye) and asthenopic problems[4]. Hayes et al[4]found that slight to mild eye symptoms were common in VDU users in their survey on university employees; moreover, between 10%and 20% experienced moderate to worse eye symptoms at the end of the day. In addition, previous studies have also reported that individual factors, along with environmental conditions,had significant influence on eye symptoms. These studies showed that eye symptoms were greater among females and increased with VDU use, notably rising when using a VDU for more than six hours in a typical day[6-7].
Accommodative and non-strabismic binocular vision dysfunctions refer to the inability of both eyes to coordinate properly. Subjects with these anomalies present abnormal clinical signs of accommodative and binocular vision tests and eye symptoms related to these dysfunctions. These eye symptoms may affect visual performance, hindering productivity due to decreased visual efficiency. Subjects with these dysfunctions can be treated to improve their visual performance[13-15].
Previous studies reported that VDU users present abnormal changes in accommodative and binocular vision status,most probably because such users make a great visual effort for extended periods[2]. Rosenfield[2]determined that inappropriate oculomotor responses can contribute to the symptoms associated with VDU use. However, it is not known to what extent these abnormal changes of accommodative and binocular vision status are related to the presence of Accommodative and non-strabismic binocular dysfunctions(ANSBD). In addition, there is a dearth of clinical studies in the literature on the presence of ANSBD in VDU users. Thus,the aim of the present study was to determine the presence of ANSBD in a non-presbyopic population of VDU users.
SUBJECTS AND METHODS
Subjects One hundred and one subjects, aged between 20 and 34y, using a VDU for at least two hours a day were initially included in the study. They were office workers,teachers and students at the University of Valencia, who were invited to participate through advertisements on public information boards. They were warned about the importance of eye examinations when using a VDU. Our study did not specifically target VDU users with eye symptoms. The age limit was 34y to avoid subjects who could potentially have pre-presbyopia, as they would bias the diagnosis of ANSBD.It also excluded contact-lens wearers and subjects who had undergone refractive surgery or had any given systemic or ocular disease. These subjects could present eye symptoms unrelated to ANSBD.
The study complied with the ethical requirements set by the University of Valencia and followed the tenets of the Declaration of Helsinki. Informed consent was obtained from all subjects once the nature and possible consequences of the study had been explained to them.
One qualified examiner performed the eye examination on all participants. A different examiner analysed the collected data.We conducted this study at the Eye Clinic of the Lluís Alcanyís Foundation (University of Valencia) between 2015 and 2016.
Clinical History Table 1 shows the questionnaire used in this study derived from Hayes et al[4]. The participants were asked about their eye symptoms (“How do you feel at the end of the workday using a VDU?”). It graded the intensity of eye symptoms like this: 4 (severe), 3 (moderate), 2 (mild), 1(slight) and 0 (none), thus allowing us to obtain the mean impact(in a 0-to-4 scale) of each symptom within the study population.
Eye Examination Two visits were needed to perform the eye examination. At thefirst visit, we carried out preliminary tests, such as visual acuity and the cover test at a distance and near, near point of convergence, ocular motility, pupils,fusion (Worth Four-Dot test), stereopsis (Randot stereo test)and the evaluation of ocular health (direct ophthalmoscopy,biomicroscopy, and visualfields). Cycloplegic evaluation was carried out when required (high decompensated esophoria,suspected latent hyperopia or accommodative spasm and indirect ophthalmoscopy).
In the second visit, we performed a refractive examination,which included objective (retinoscopy and autorefractometer)and subjective evaluation. The subjective examination was performed by means of monocular fogging with cross-cylinder followed by the binocular balance test to obtain the maximum positive for the best visual acuity of subjective refraction[14].This value was used as the baseline for evaluation of binocular and accommodative tests.
Table 1 Classification of eye symptoms related to VDU use

The questionnaire is derived from Hayes et al[4].
Subjects with a significant uncorrected refractive error regarding their habitual refraction (changes in the sphere or cylinder greater than 0.50 D; 8 subjects) or when they did not use a prescription but needed one (sphere or cylinder greater than 0.50 D; 2 subjects) were excluded. In addition, we also excluded those subjects with other problems, such as ocular motility disorders, vertical deviation, strabismus and any other ocular health problems (2 subjects). Finally, the remaining participants (89 subjects) underwent an exhaustive assessment of their accommodation and binocular vision status.
Evaluation of Accommodative and Binocular Vision Binocular and accommodative status were evaluated according to a standardised methodology used to perform these tests[14].The tests included in the examination were: far and near lateral phorias (cover test and von Gräfe’s techniques), near point of convergence (NPC), far and near lateral fusional vergence, vergence facility testing (using 12 Δ base-out / 3 Δ basein), monocular estimation method retinoscopy, positive and negative relative accommodation, monocular and binocular accommodative facility with ±2.00 D flipper lenses (the target for binocular testing was the Bernell #9 Vectogram) and accommodative amplitude (AA) using the push-up method.
An automatic phoropter for the tests at far and near distances(40 cm) was used. The exam test at a near distance was the Topcon NC3-3. Outside the phoropter, the accommodative and vergence facility tests, covert test, NPC and AA using a near test (gulden fixation stick that had 20/30 targets) were performed.
The findings of the accommodative and binocular vision tests in each subject were compared with the normal clinical values of the population for these tests; then thefindings that
Table 2 Clinical signs used for the diagnosis of accommodative and non-strabismic binocular dysfunctions
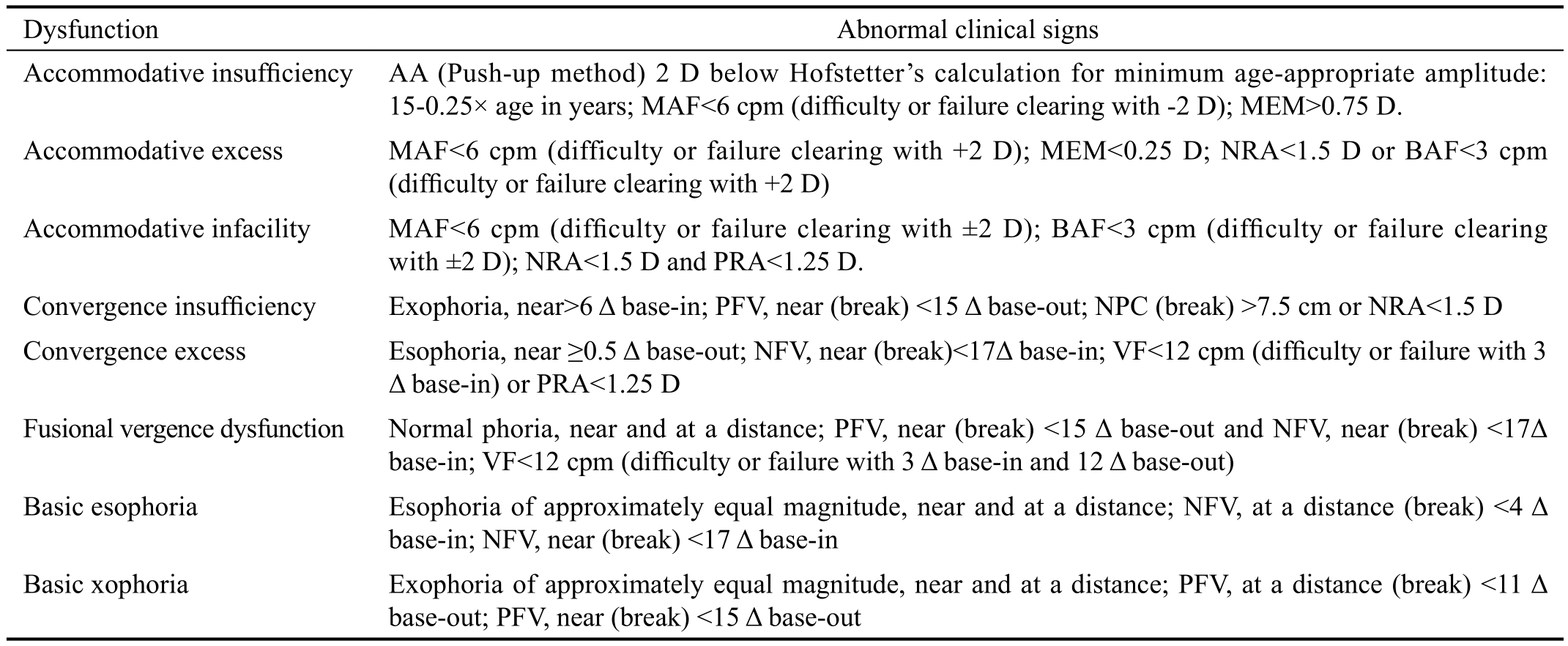
AA: Amplitude of accommodation; MAF: Monocular accommodative facility; cpm: Cycles per minute; MEM: Monocular estimation method retinoscopy; NRA: Negative relative accommodation; BAF: Binocular accommodative facility; PRA: Positive relative accommodation; PFV:Positive fusional vergence; NPC: Near point of convergence; NFV: Negative fusional vergence; VF: Vergence facility.deviated from normal values were grouped according to each dysfunction (Table 2); andfinally, the subjects who presented three abnormal clinical signs in some dysfunction, along with eye symptoms related to VDU use, were considered to have ANSBD[13-14].
Statistical Analysis The data collected from the questionnaire were analysed using SPSS software (version 15.0 for Windows,SPSS Inc., Chicago, IL, USA). It used nonparametric statistical tests to determinate the differences in eye symptoms between VDU users with and without ANSBD. A P-value <0.05 was regarded as statistically significant.
RESULTS
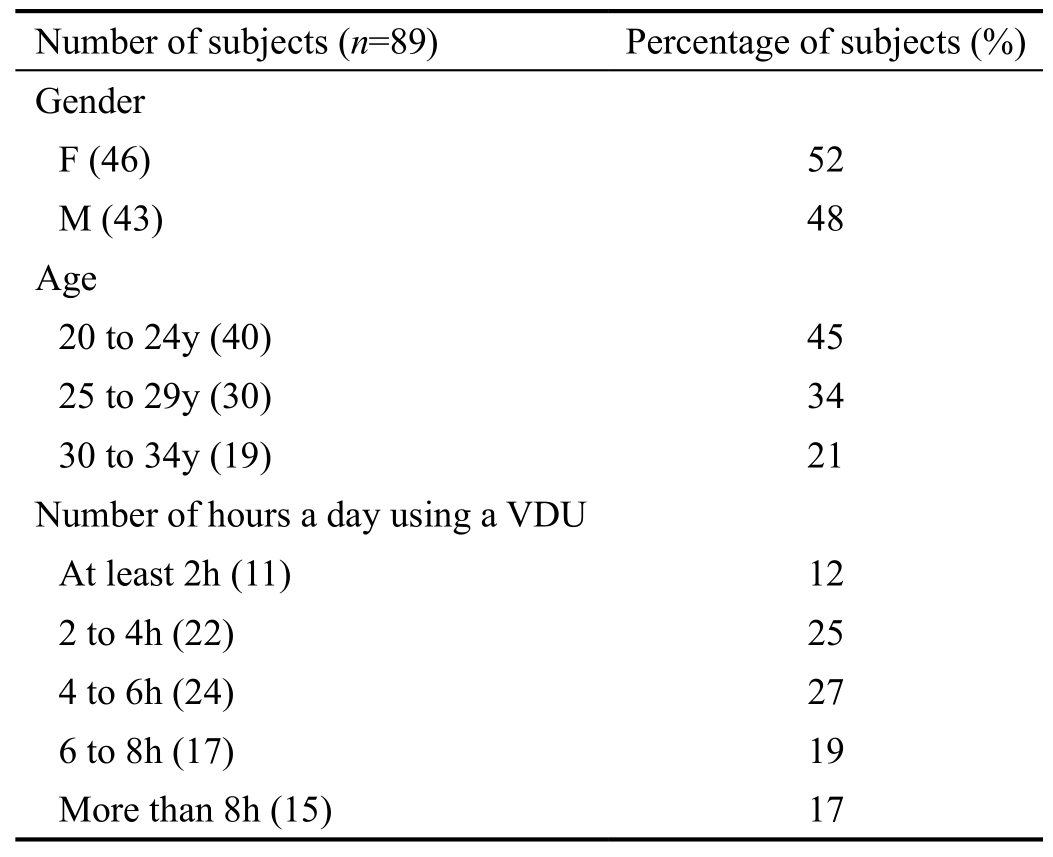
Eighty-nine VDU users (46 females and 43 males), aged between 20 and 34y, participated in the study (mean 25±4y).They were all Caucasians and had a monocular visual acuity of 20/20 or better in both eyes. The mean spherical equivalent refractive error was -0.90±1.35 D. They used flat-panel displays an average of 5±1.9h a day. Demographic information about the participants is summarised in Table 3. Subjects were classified by gender, in three age subgroups at fiveyear intervals and infive different subgroups according to the number of hours spent each day using a VDU.
Table 4 shows the results of clinical tests for abnormal signs of accommodative and binocular vision in the participants.The most predominant changes were in a difficulty to relax the convergence system (44 subjects presented reduced negative fusional vergence, 30 subjects had near esophoria, 18 subjects failed vergence facility with 3 Δ base-in and 15 subjects failed with positive relative accommodation)[14].
Table 5 shows the number of subjects (n=20; 22.5% of subjects) who presented ANSBD. Convergence excess was the most frequent binocular vision dysfunction (10% of subjects)and accommodative excess (4.5% of subjects) within the accommodative dysfunctions.
Table 3 Demographic data of participants
Seven of the participants with ANSBD (n=20) presented slight to mild eye symptoms at the end of the workday using a VDU; and 13 from moderate to severe in nature (at least one symptom of ten in the questionnaire used; Table 1). The median total score of eye symptoms was 9.5 [interquartile range (IQR)=8; overall range 3-23]. Eye symptoms were greater among females and increased with age and VDU use in a typical day (Figure 1). The median total score for subjects without ANSBD was 7.5 (IQR=7; overall range 0-27).No statistically significant differences were found between subjects with or without ANSBD (U=467.5; P=0.1).
DISCUSSION
The results of this study indicate that a large number of the participants presented eye symptoms related to VDU useand abnormal changes in their accommodative and binocular vision status, which is in agreement with previous studies[2].Table 4 shows that when clinical signs of accommodative and binocular vision tests were compared with normal values,the most predominant changes were in a difficulty to relax the convergence system[14]. Nine subjects (10% of VDU users) presented three abnormal clinical signs in relaxing the convergence system and eye symptoms related to VDU use,therefore this was consistent with the presence of convergence excess (Table 2). These findings show that VDU users with ANSBD were more prone to this dysfunction, which may be due to the high levels of visual effort made when using a VDU.The eye symptoms were evaluated with the aid of the questionnaire created by Hayes et al[4], because it has been used in previous studies to evaluate specific eye symptoms of VDU users. This questionnaire has proved to be reliable and repeatable[16-18]. The results showed that the median total score of eye symptoms (7.5 points) obtained in VDU users without ANSBD was similar to those of other previous studies[17-18],whilst VDU users with ANSBD showed higher scores (median total score 9.5 points) although no statistically significant differences were found. In addition, these eye symptoms were greater in females and increased with age and VDU use in a typical day, which concurs with previous studies[6-7]. More importantly, 13 subjects of 20 VDU users with ANSBD had moderate to severe eye symptoms, which represented 14.5%of the total participants. Indeed, these eye symptoms may lead to a decrease in visual efficiency with significant detriment to productivity when using a VDU, hence these subjects should be treated to improve their visual performance[13-14].
Table 4 Abnormal signs of accommodative and binocular vision clinical tests in the participants n=89
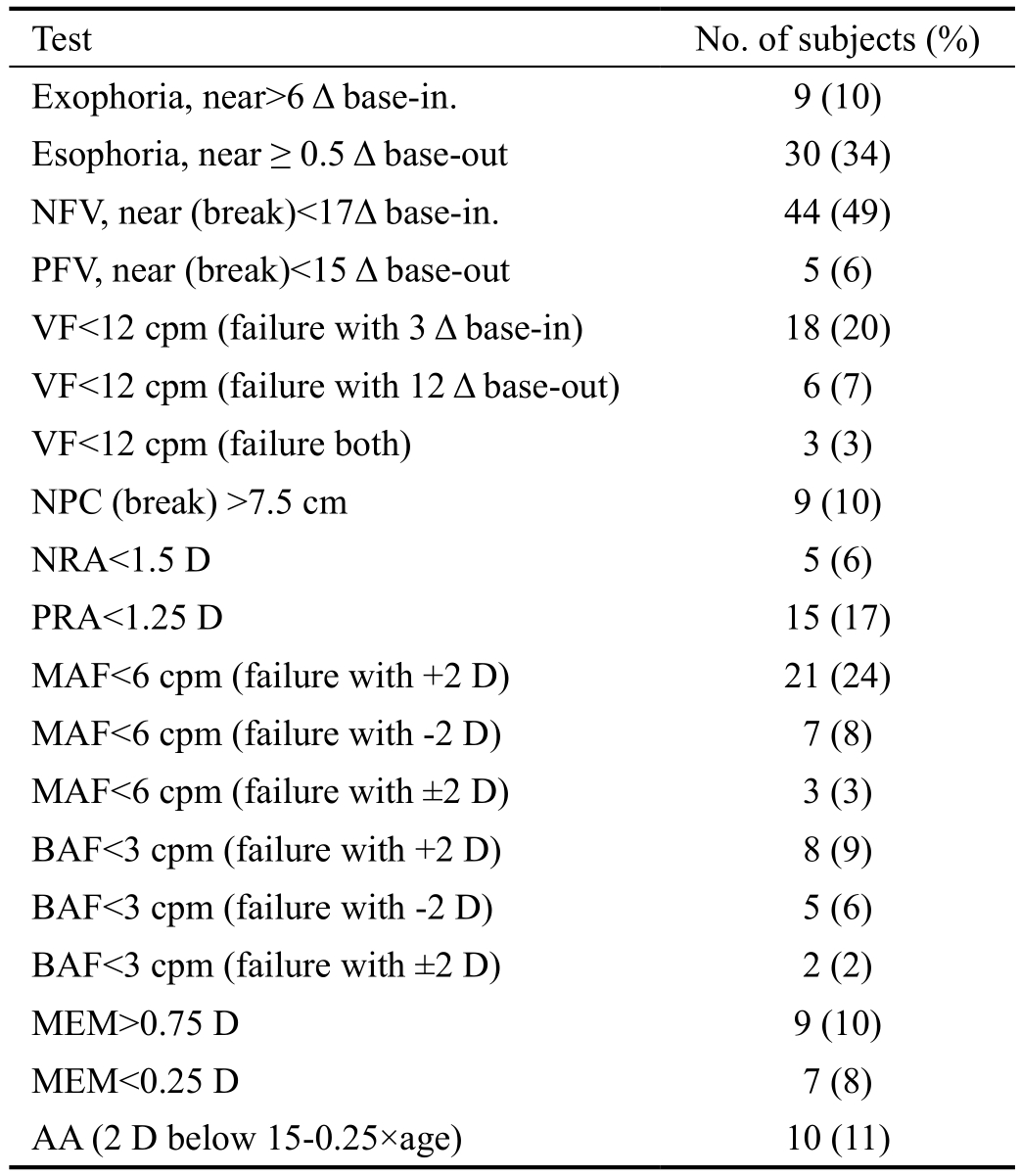
NFV: Negative fusional vergence; PFV: Positive fusional vergence;VF: Vergence facility; cpm: Cycles per minute; NPC: Near point of convergence; NRA: Negative relative accommodation; PRA:Positive relative accommodation; MAF: Monocular accommodative facility; BAF: Binocular accommodative facility; MEM: Monocular estimation method retinoscopy; AA: Amplitude of accommodation.
Table 5 Number of VDU users who presented accommodative and non-strabismic binocular dysfunctions along with eye symptoms related to VDU use
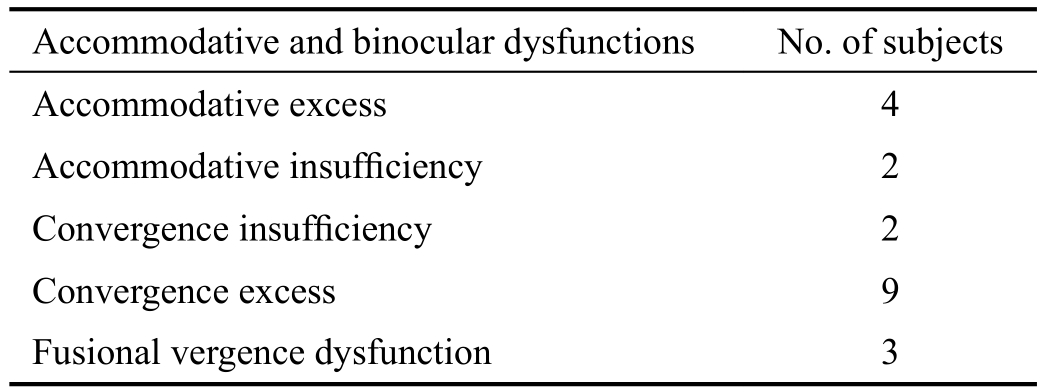
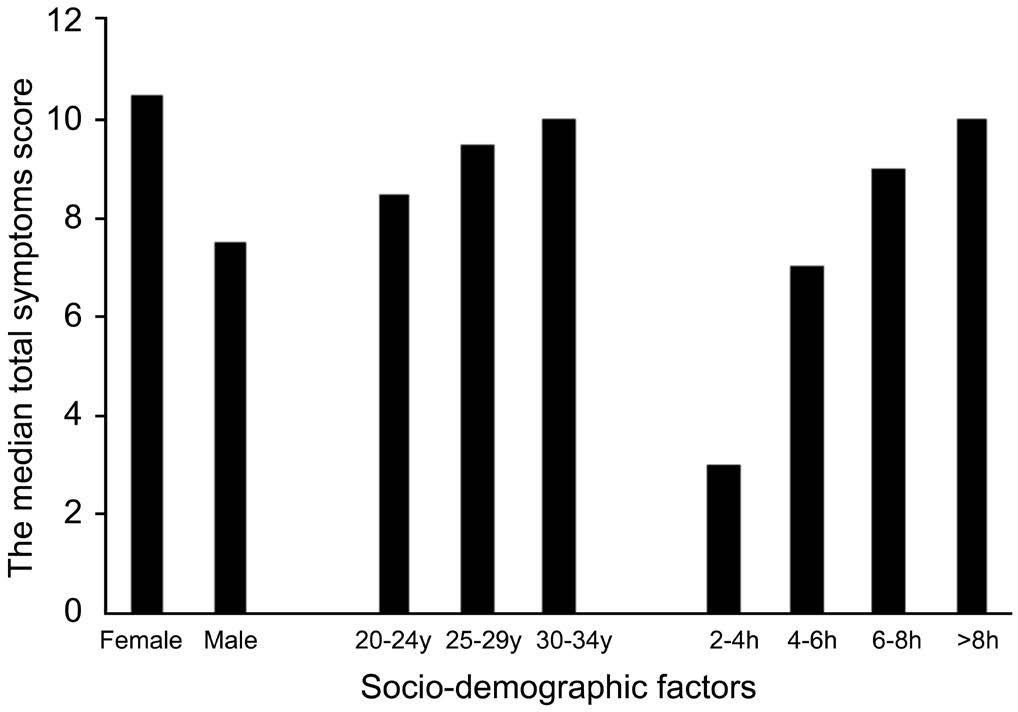
Figure 1 The median total score of eye symptoms in the VDU user participants, with accommodative and non-strabismic binocular dysfunctions (20 subjects), with regard to socio-demographic factors(gender, age and the number of hours spent each day using a VDU).
The presence of ANSBD in this study was 22.5% of VDU users (20 subjects). These findings are difficult to compare with the general population, since previous studies on ANSBD were performed on diverse populations (clinical population,mainly children, and university students)[19]. Another difficulty is the different diagnostic criteria and clinical tests used[19]. In fact, a problem that clinicians encounter when determining ANSBD is the lack of a gold standard for the diagnosis of each dysfunction. Therefore, previous studies based on scientific evidence have reported that a number of abnormal clinical signs associated with each dysfunction should be presented to determine the diagnosis of each ANSBD accurately[14,20-21]. This study followed this methodology and three abnormal clinical signs were considered in each ANSBD, in agreement with these previous studies.
In addition, previous studies have reported the influence of refractive errors when diagnosing ANSBD[14,20]. Significant degrees of uncorrected refractive errors should be correctedfirst, since they could affect the accommodative and binocular vision status. Re-evaluation after four or six weeks should be performed to analyse accommodative and binocular vision status[14]. However, with small degrees of uncorrected refractive errors, which are commonly found in subjects with ANSBD, the clinician should determine the relationship of eye symptoms with the presence of significant accommodative and binocular vision problems[14]. In the present study, VDU users with significant degrees of uncorrected refractive errors were excluded and those with small degrees of uncorrected refractive errors were considered to have ANSBD when their eye symptoms were related to these dysfunctions.
In summary, this study shows that the main abnormal changes in accommodative and binocular vision status in VDU users were found in a difficulty to relax the convergence system.These changes were related to the presence of convergence excess in 10% of VDU users. Finally, significant eye symptoms in VDU users with ANSBD often occur and should not be underestimated; therefore, such subjects should be treated for these dysfunctions to improve their visual performance.
ACKNOWLEDGEMENTS
Conflicts of Interest:Porcar E, None; Montalt JC, None;Pons AM, None; España E, None.
REFERENCES
1 Rosenfield M, Howarth PA, Sheddy JE, Crossland MD. Vision and IT displays: a whole new visual world. Ophthalmic Physiol Opt 2012;32(5):363-366.
2 Rosenfield M. Computer vision syndrome: a review of ocular causes and potential treatments. Ophthalmic Physiol Opt 2011;31(5):502-515.
3 Bali J, Neeraj N, Bali RT. Computer vision syndrome: a review. J Clin Ophthalmol Res 2014;2(1):61-68.
4 Hayes JR, Sheedy JE, Stelmack JA, Heaney CA. Computer use,symptoms, and quality of life. Optom Vis Sci 2007;84(8):738-744.
5 Thorud HM, Helland M, Aarås A, Kvikstad TM, Lindberg LG, Horgen G. Eye-related pain induced by visually demanding computer work.Optom Vis Sci 2012;89(4):E452-E464.
6 Agarwal S, Goel D, Sharma A. Evaluation of the factors which contribute to the ocular complaints in computer users. J Clin Diagn Res 2013;7(2):331-335.
7 Yoshioka E, Saijo Y, Kawaharada M, Kishi R. Association between duration of daily visual display terminal work and insomnia among local government clerks in Japan. Am J Ind Med 2008;51(2):148-156.
8 Uchino M, Yokoi N, Uchino Y, Dogru M, Kawashima M, Komuro A, Sonomura Y, Kato H, Kinoshita S, Schaumberg DA, Tsubota K.Prevalence of dry eye disease and its risk factors in visual display terminal users: the Osaka study. Am J Ophthalmol 2013;156(4):759-766.
9 Sa EC, Ferreira Junior M, Rocha LE. Risk factors for computer visual syndrome (CVS) among operators of two call centers in São Paulo, Brazil.Work 2012;41 Suppl 1:3568-3574.
10 Logaraj M, Madhupriya V, Hegde SK. Computer vision syndrome and associated factors among medical and engineering students in Chennai.Ann Med Health Sci Res 2014;4(2):179-185.
11 Han CC, Liu R, Liu RR, Zhu ZH, Yu RB, Ma L. Prevalence of asthenopia and its risk factors in Chinese collage students. Int J Ophthalmol 2013;6(5):718-722.
12 Soman Mani, Liji Menon M, Harishankar S, Anna Mathew. The prevalence of computer vision syndrome among information technology students in a rural engineering college. International Journal of Current Research 2016;8(12);43845-43848.
13 Cooper JS, Burns CR, Cotter SA, Daum KM, Griffin JR, Scheiman MM. Care of the patient with accommodative and vergence dysfunction.American Optometric Association; 2011. Available at: http://www.aoa.org/documents/optometrists/CPG-18.pdf. Accessed on March 20, 2016.
14 Scheiman M, Wick B. Clinical management of binocular vision:heterophoric, accommodative, and eye movement disorders. 4thedition.Philadelphia: Lippincott Williams & Wilkins; 2014.
15 Barnhardt C, Cotter SA, Mitchell GL, Scheirman M, Kulp MT; CITT Study Group. Symptoms in children with convergence insufficiency:before and after treatment. Optom Vis Sci 2012;89:1512-1520.
16 Rosenfield M, Hue JE, Huang RR, Bababekova Y. The effects of induced oblique astigmatism on symptoms and reading performance while viewing a computer screen. Ophthalmic Physiol Opt 2012;32(2):142-148.
17 Portello JK, Rosenfield M, Bababekova Y, Estrada JM, Leon A.Computer-related visual symptoms in office workers. Ophthalmic Physiol Opt 2012;32(5):375-382.
18 Porcar E, Pons AM, Lorente A. Visual and ocular effects from the use of flat-panel displays. Int J Ophthalmol 2016;9(6):881-885.
19 Cacho-Martinez P, Garcia-Muñoz A, Ruiz-Cantero MT. Do we really know the prevalence of accommodative and nonstrabismic binocular dysfunctions? J Optom 2010;3(4):185-197.
20 García-Muñoz Á, Carbonell-Bonete S, Cantó-Cerdán M, Cacho-Martínez P. Accommodative and binocular dysfunctions: prevalence in a randomised sample of university students. Clin Exp Optom 2016;99(4):313-321.
21 Hussaindeen JR, Rakshit A, Singh NK, George R, Swaminathan M, Kapur S, Scheiman M, Ramani KK. Prevalence of non-strabismic anomalies of binocular vision in Tamil Nadu: report 2 of BAND study.Clin Exp Optom 2017;100(6):642-648.