INTRODUCTION
Cataract surgery has gone through the three stages of intracapsular cataract extraction, extracapsular cataract extraction, and phacoemulsification. With the evolution of cataract surgery techniques, microincision-based cataract surgery has emerged as a safe and efficient technique as it reduces surgical damage to the eyeball structure. In this study,we performed phacoemulsification using a Bausch & Lomb Stellaris phacoemulsification system and compared the surgical efficacy of three incisions of different lengths.
SUBJECTS AND METHODS
General Information In this prospective, randomized study,we enrolled patients who underwent phacoemulsification and intraocular lens (IOL) implantation from May 2011 to February 2012. Ninety patients were categorized into three groups according to the type of IOL chosen of their own volition, i.e. 1.8-mm group, 3.2-mm group, and 5.5-mm group.The 1.8-mm group, which received Bausch & Lomb MI60 foldable IOL implantation (n=30), included 16 males and 14 females, with a mean age of 68y. When stratified by nuclear hardness according to the Lens Opacities Classification System II (LOCS II), there were 6 patients with grade II nuclear hardness, 15 with grade III nuclear hardness, and 9 with grade IV nuclear hardness. The 3.2-mm group, which received Bausch & Lomb Akreos AO foldable IOL implantation,included 15 men and 15 women, with a mean age of 70y.There were 5 patients with grade II nuclear hardness, 17 with grade III nuclear hardness, and 8 with grade IV nuclear hardness. The 5.5-mm group, which received Alcon TYPE 05 IOL implantation, included 14 men and 16 women, with a mean age of 71y. There were 4 patients with grade II nuclear hardness, 17 with grade III nuclear hardness, and 9 with grade IV nuclear hardness. Patients with glaucoma, iritis, corneal disease, diabetic eye disease, and other related eye diseases were excluded from the study. No statistical difference was found among the three groups with respect to age, gender,or preoperative examinations (i.e. visual acuity, lens nuclear hardness, corneal astigmatism, and corneal endothelial cell count; P>0.05).
Surgical Procedures The surgery was performed with a Bausch & Lomb Stellaris phacoemulsification system. Allprocedures were conducted by a single surgeon. The patients were operated on in a supine position, and operated eyes were sterilized with fortified iodine solution. Block anesthesia of ciliary ganglion behind the eye was induced with 2% lidocaine,after which an eye speculum was used to open the eyelid.A 1.8-mm tunnel knife was thrust into the anterior chamber in the 10 o’ clock position in the corneoscleral limbus, and a side cutter was introduced into the anterior chamber in the 2 o’ clock position. Subsequently, 0.2 mL of viscoelastic agent was injected into the anterior chamber. Circular capsulorhexis was performed with a diameter of about 6.0 mm, and the lens nucleus was hydrodissected, disintegrated with ultrasound emulsification, and removed. Balanced salt solution was used for irrigation/aspiration of the cortex lentis, after which 0.2 mL of viscoelastic agent was injected into the anterior chamber. According to the type of lens chosen before surgery,the 1.8-mm group was implanted with a Lomb MI60 IOL.In the 3.2-mm group, the incision was lengthened to 3.2 mm and a Lomb Akreos AO IOL was implanted. In the 5.5-mm group, the incision was lengthened to 5.5 mm and an Alcon TYPE 05 IOL was implanted. Subsequently, the viscoelastic agent in the anterior chamber was aspirated. Then, 0.2 mL of diluted carbachol was injected into the anterior chamber and retrobulbar injection of triamcinolone acetonide (20 mg) was performed. Tobradex eye ointment was applied within the conjunctival sac, and the operated eyes were covered with gauze.
Table 1 Comparison of ultrasonic energy and ultrasound time of the three groups mean±SD
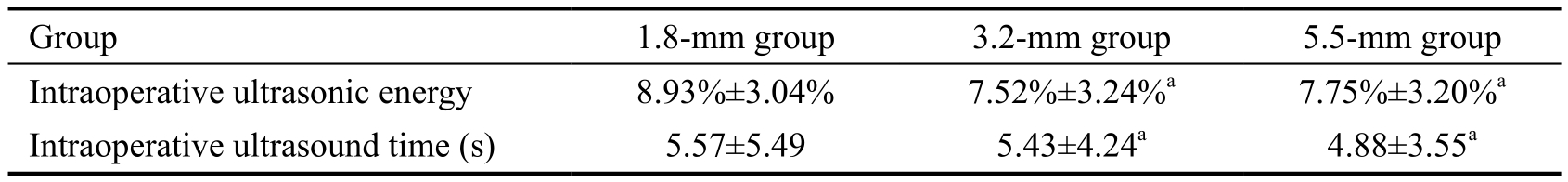
aP>0.05.
Preoperative and Postoperative Measurements Visual acuity, Oculyzer-based anterior segment analysis, and corneal endothelial cell count before surgery, and three days, one week, one month, and three months after surgery were recorded and compared. Pseudophakic accommodation three days, one week, one month, and three months after surgery was determined. Intraoperative ultrasound time and ultrasonic energy were recorded.Statistical Analysis Statistical analysis was performed using SPSS software. All observation indexes of patients were compared with the Chi-square test, whereas visual acuity, corneal astigmatism, corneal endothelial count, and pseudophakic accommodation were compared using the variance analysis.P<0.05 were considered statistically significant.
RESULTS AND DISCUSSION
Comparison of Intraoperative Uultrasound Energy and Ultrasound Time Among the Three Groups No significant differences in the ultrasonic energy and effective ultrasound time were noted across the three groups (P>0.05; Table 1).
Table 2 Comparison of mean uncorrected visual acuity among the three groups mean±SD
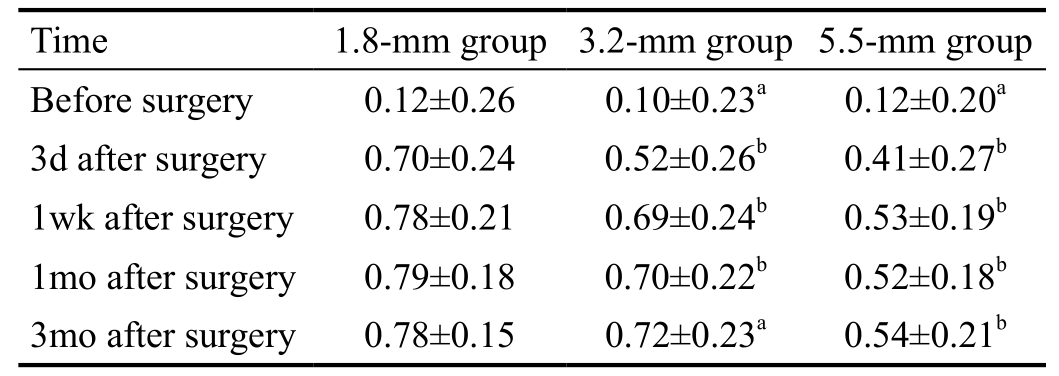
aP>0.05,bP<0.05.
Table 3 Comparison of average corneal astigmatism among the three groups mean±SD; D
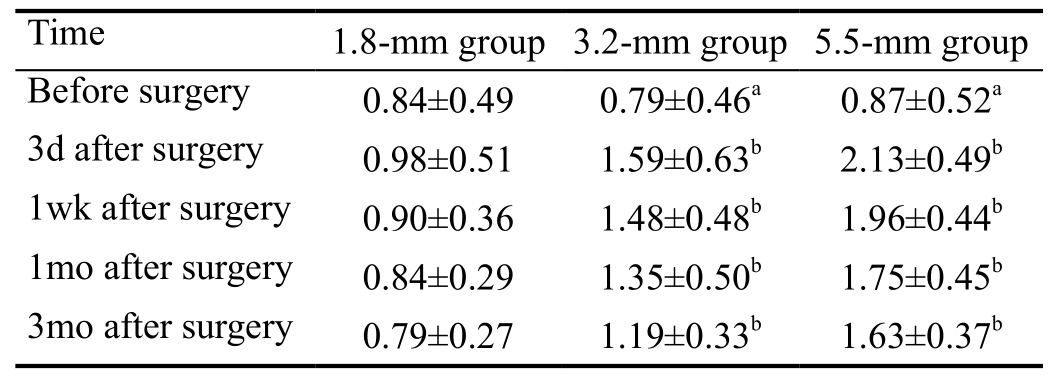
aP>0.05,bP<0.05.
Uncorrected Visual Acuity Preoperative visual acuity showed no statistically significant difference among the three groups (P>0.05). Visual acuity three days, one week, and one month after surgery showed significant difference among the three groups (P<0.05); however, the difference decreased over time. No significant difference in visual acuity was observed between the 1.8-mm group and the 3.2-mm group three months after surgery (P>0.05). In contrast, the 1.8-mm group and the 3.2-mm group showed significant differences in visual acuity from the 5.5-mm group (P<0.05). The results are presented in Table 2.
Astigmatism K1-K2 in the Oculyzer results refers to the degree of corneal astigmatism. No significant difference in corneal astigmatism was found among the three groups before surgery (P>0.05). Postoperative corneal astigmatism exhibited significant differences among the three groups (P<0.05), but the difference gradually decreased over time (Table 3).
Corneal Endothelial Cells No significant differences were noted with respect to preoperative and postoperative corneal endothelial count among the three groups (P>0.05). The results are presented in Table 4.
Pseudophakic Accommodation No significant difference was noted between the 1.8-mm group and the 3.2-mm group with respect to pseudophakic accommodation at three days,1wk, 1 and 3mo after surgery (P>0.05). Pseudophakic accommodation in the 1.8-mm group and the 3.2-mm groupdiffered significantly from that in the 5.5-mm group (P<0.05).The results are presented in Table 5.
Table 4 Comparison of average corneal endothelial cell count among the three groups mean±SD; cell/mm2
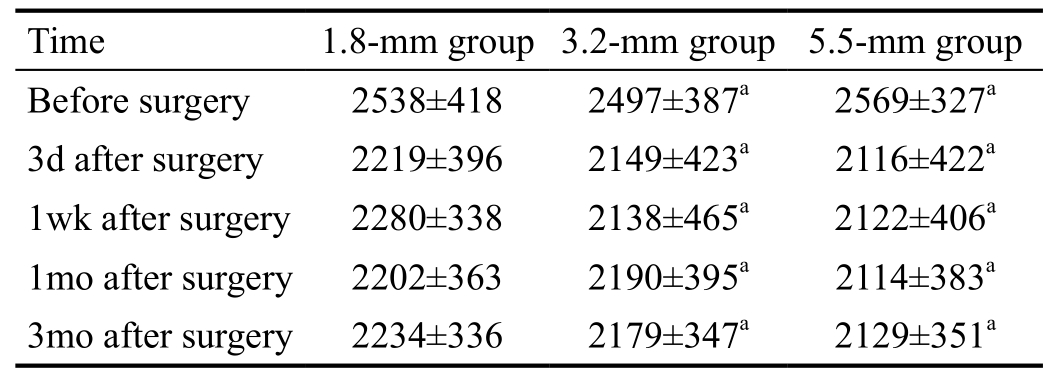
aP>0.05.
Correlation of Incision Length with Corneal Astigmatism and Refractive Stability Previous studies and clinical observations suggest that the size of the surgical incision correlates with surgically induced corneal astigmatism and time to refractive stability[1]. Complications aside, corneal astigmatism caused by a surgical incision is the major factor affecting visual acuity after cataract surgery[2]. The Oculyzer system for anterior segment analysis presents an accurate and comprehensive picture of the morphology of the entire cornea. Observation and comparison of anterior segment analysis results can aid in understanding corneal astigmatism before and after surgery. This study shows that postoperative corneal astigmatism increased and visual acuity decreased with increasing incision length. This difference was particularly notable in the early stage. However, the differences among the three groups decreased over time. Furthermore, no significant difference in visual acuity was observed between the 1.8-mm and 3.2-mm groups three months after surgery, whereas a marked difference in corneal astigmatism was still present across the three groups three months after surgery. In a case series study,Agarwal et al[3]showed that only surgical incisions greater than 2 mm in length will produce changes in corneal curvature.Accordingly, compared with the other two groups, the 1.8-mm group achieved a relatively stable refractive state and better visual acuity in a shorter period of time.
Correlation of Surgical Incision Length with Corneal Endothelial Cell Count Previous studies have shown that mechanical damage from emulsified particles and energy generated from high-frequency vibration of ultrasound probes during phacoemulsification can affect the structure,quantity, and physiological functions of corneal endothelial cells[4]. Endothelial cell loss, once a certain degree is reached,will cause corneal edema and decompensation, leading to devastating damage to the cornea. As such, the rate of corneal endothelial cell loss is used as one of the important indicators of surgical safety. Another study showed that the rate of corneal endothelial cell loss correlates with the size of corneal incisions and that a smaller incision in phacoemulsification has a milder impact on corneal endothelial cells[5]. In the presentstudy, we found that the number of corneal endothelial cells diminished in all three groups, and smaller incisions were associated with milder loss. However, no significant differences were observed between the three groups. We hypothesize that several reasons may explain this phenomenon. First, a number of factors determine the rate of corneal endothelial loss, such as nuclear hardness, patient age, position of ultrasound plane,and ultrasound incision location[6]. Second, the study involved an inadequate sample size, which means more data are needed.
Table 5 Comparison of pseudophakic accommodation among the three groups mean±SD; D
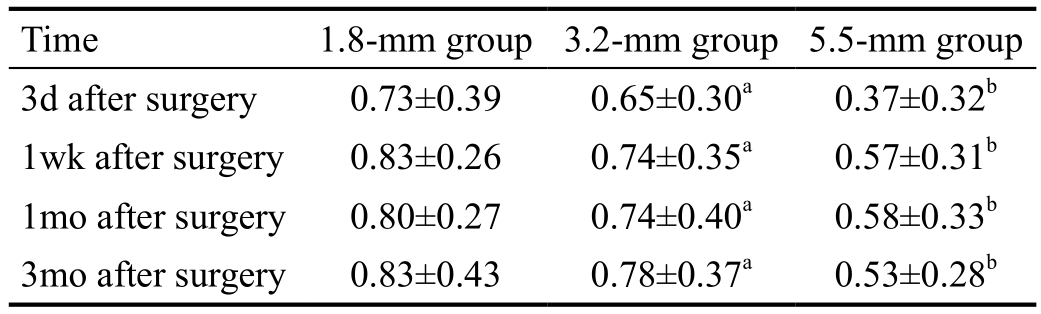
aP>0.05,bP<0.05.
Correlation of Surgical Incision Length with Pseudophakic Accommodation Previous research[7-9]confirmed that pseudophakic eyes exhibit some accommodation after cataract surgery, which is related to a small pupil, multifocal cornea,myopic astigmatism, or spherical aberration. In this study,all IOLs in the three groups achieved a certain degree of pseudophakic accommodation, and the 1.8-mm group showed significantly better pseudophakic accommodation than the 5.5-mm group. However, the 1.8-mm group had no significant advantage in this regard compared with the 3.2-mm group.According to the sac regulation theory, when normal eyes are adjusted, the contraction of the ciliary muscle moves the lens,suspensory ligament, and vitreous body forward, resulting in a shallower anterior chamber. Therefore, we propose that the following factors may account for the fact that microincisions lead to higher pseudophakic accommodation than conventional incisions. First, microincision-based surgery causes milder disturbance to the ciliary muscle and suspensory ligament around the incision and hence offers greater protection of ciliary muscle contractility. Second, microincisions enhance wound closure, alleviate intraoperative and postoperative inflammation, and reduce ciliary muscle congestion and edema. Third, the Baushe & Lomb MI60 IOL used together with the microincision is a foldable monofocal, one-piece IOL.When implanted in the eye, it causes little tissue disturbance,preserves sac integrity, and shows good biocompatibility,offering significantly better pseudophakic accommodation than a monofocal non-foldable IOL[10]. This study showed that the average pseudophakic accommodation after surgery was 0.83±0.43 D in the 1.8-mm group and 0.78±0.37 D in the 3.2-mm group. Our results are largely consistent with those of a study by Dong et al[11]but lower than the results of Yu et al[7](2.35±1.14 D). This discrepancy may be due to the following factors. First, the subjects differed in age, with the study population in our current study being relatively older.Second, the studies were performed over different time frames.Our study followed patients within three months after cataract surgery, whereas Yu et al[7]followed patients for more than six months after cataract surgery. Third, visual acuity may have differed among the subjects. Our study did not set any limitation on visual acuity when enrolling patients, whereas Yu et al[7]included only patients with a vision of 4.6 or greater in their study. Fourth, our study may be limited by an inadequate sample size, which means more data are needed.
The 1.8-mm coaxial microincision for phacoemulsification offers the advantages of minimizing the surgical wound while avoiding any change in conventional techniques, hence shortening the surgical learning curve. Smaller incisions can effectively prevent the over flow of balanced salt solution during surgery and therefore ensure higher anterior chamber stability during surgery. Moreover, 1.8-mm coaxial ultrasound features a unique Attune energy management system. The handle has a cavity effect and is capable of achieving higher operation efficiency, allowing fast treatment of grade IV nucleus in the study, resulting in milder corneal endothelium damage and less edema. Compared with conventional coaxial incisions for phacoemulsification, the 1.8-mm microincision features several advantages for phacoemulsification by reducing surgically induced astigmatism, enhancing wound closure, reducing intraoperative and postoperative in flammation, and shortening the time to visual acuity recovery[12]. Taken together, the results of the present study indicate that the 1.8-mm microincision can contribute to lower astigmatism, milder corneal endothelial loss, and higher postoperative pseudophakic accommodation,and help cataract patients recover visual acuity faster than conventional incisions.
ACKNOWLEDGEMENTS
Conflicts of Interest:Song E, None; Li X, None; Bi MC,None; Ren H, None; Wang D, None; Cui ZH, None; Yang W, None; Shi H, None; Sun YB, None.
REFERENCES
1 Hashemi H, Khabazkhoob M, Soroush S, Shariati R, Miraftab M, Yekta A. The location of incision in cataract surgery and its impact on induced astigmatism. Curr Opin Ophthalmol 2016;27(1):58-64.
2 Kim H, Whang WJ, Joo CK. Corneal astigmatism in patients after cataract surgery: a 10-year follow-up study. J Refract Surg 2016;32(6):404-409.
3 Agarwal A, Agarwal A, Agarwal S, Narang P, Narang S. Phakonit:phacoemulsification through a 0.9 mm corneal incision. J Cataract Refract Surg 2001;27(10):1548-1552.
4 Ho JW, Afshari NA. Advances in cataract surgery: preserving the corneal endothelium. Curr Opin Ophthalmol 2015;26(1):22-27.
5 Jin C, Chen X, Law A, Kang Y, Wang X, Xu W, Yao K. Differentsized incisions for phacoemulsification in age-related cataract. Cochrane Database Syst Rev 2017;20(9):CD010510.
6 Hong Y, Zhang C, Wang W. The effect of phacoemulsification on eyes with preexisting functionalfiltering blebs. Zhonghua Yan Ke Za Zhi 2009;45(10):898-902.
7 Yu AY, Zhao YE, Jin WQ. Accommodative facility of pseudophakic eyes after phacoemulsification. Chinese Journal of Practical Ophthalmology 2006;3:267-269.
8 Yamamoto T, Hiraoka T, Oshika T. Apparent accommodation in pseudophakic eyes with refractive against-the-rule, with-the-rule and minimum astigmatism. Br J Ophthalmol 2016;100(4):565-571.
9 Dewey S, Beiko G, Braga-Mele R, Nixon DR, Raviv T, Rosenthal K. ASCRS Cataract Clinical Committee, Instrumentation and IOLs Subcommittee. Microincisions in cataract surgery. J Cataract Refract Surg 2014;40(9):1549-1557.
10 Tong Y, Wu P, Zhang XG. Comparison of pseudophakic accommodation between foldable monofocal and non- foldable pseudophakic eyes.Journal of Injuries and Occupational Diseases of the Eye with Ophthalmic Surgeries 2006;1:6-8.
11 Dong Z, Wang NL, Zhu SQ. Relationship between ciliary muscle contraction and pseudophakic accommodation of foldable pseudophakic eyes. Zhonghua Yan Ke Za Zhi 2007;43(2):99-103.
12 Yang J, Wang X, Zhang H, Pang Y, Wei RH. Clinical evaluation of surgery-induced astigmatism in cataract surgery using 2.2 mm or 1.8 mm clear corneal micro-incisions. Int J Ophthalmol 2017;10(1):68-71.