INTRODUCTION
Meibomian gland dysfunction (MGD) is a common disease with chronic natural course in the eyelid and is a major cause of evaporative dry eye syndrome[1]. MGD results from meibomian gland orifice blockage due to plugging with solidified secretions and hyperkeratosis of the duct epithelium[1-3]. It was also caused by atrophy or inflammation of meibomian gland acini. Various treatments of MGD such as lid cleansing, eyelid warming massage, and artificial tears are mainly used[1,4]. If needed, systemic antibiotics such as oral tetracycline or topical anti-inflammatory agents like topical steroid eye drops are additionally used[5-6]. But these treatments are frequently ineffective. There is a demand for additional agents that acts on the main mechanism of MGD.
Inflammation is one of the important mechanisms of MGD.Ocular surface and palpable conjunctival inflammations influence meibomian gland structure and alter the function[7].Therefore, it aggravates hyperkeratosis of the duct epithelium and atrophy of acini leading to MGD[8]. Increased inflammation is associated with symptoms and signs of patients[9-13]. Antiinflammatory agents such as steroids, macrolide antibiotics,tetracycline, and cyclosporine A (CsA) have been used for the treatment of inflammation in MGD, and improve symptoms and signs of MGD[1,4-5].
CsA is an immunomodulatory agent that block T-cell activation,reducing the production of inflammatory cytokines. Topical CsA eye drop is commonly used for various inflammatory ocular conditions, including ocular rosacea[14], subepithelial infiltrates due to adenoviral keratoconjunctivitis[15], atopic keratoconjunctivitis[16], vernal keratoconjunctivitis[17], and graft-versus-host disease[18]. Especially, topical 0.05% CsA(Restasis®, Allergan pharmaceuticals, USA) is a therapeutic agent that improve tear production, due to a suppression of the inflammations of the ocular surface and lacrimal glands in dry eye patients[19]. Furthermore, it is effective for MGD patients by reducing inflammations of meibomian glands[20].
The prevalence rate of MGD was significantly different around the world, with the prevalence rate of 3.5%-19.9% in Caucasians and 60% in Asian population[21-23]. Despite the high prevalence of MGD in Asians, there were no reports on the effect of CsA in dry eye with MGD, especially in Asians including Korea[9,24-25].
The purpose of this study was to evaluate the additional effect of 0.05% cycrosporin A ophthalmic solution to treatment of dry eye with MGD in Koreans.
SUBJECTS AND METHODS
Study Design Retrospective data of multicenter study was collected on eligible patients at each of five eye hospitals,reflecting the baseline and follow-up of patients who were diagnosed MGD and were treated for a minimum of 3mo(Figure 1). Researchers at five hospitals are members of the Busan-Gyeongnam External Eye Disease Study Group. We try to standardize the test methods applied in this study and other studies. All center used a standardized datasheet template for patient chart data extraction that included demographic variables and experimental data.
Korean patients aged 18 years or older with a diagnosis of MGD were treated at the initial visit, and whose management included 0.05% CsA eyedrop (Restasis®, Allergan pharmaceuticals,USA) and 0.1% preservative-free sodium hyaluronate eyedrop from July, 2016 to December, 2016 were eligible for inclusion.Patients were enrolled based on a slit-lamp examination and symptoms using the presence of the following criteria:occlusion or abnormal secretion of meibum, thickening or irregularity of the eye lid margin, dilation of blood vessels and telangiectasia around the glandular orifice, tear film break-up time (tBUT) of less than 8s, and at least one symptom in ocular irritation, glare, and epiphora due to tear layer instability.Patients were excluded if there was a history or presence of severe eyeball abnormalities, previous ocular surgery, severe ocular infections such as herpes keratitis, cyclosporine hypersensitivity reaction, pregnancy or breastfeeding, or previous topical CsA eye drop use within 3mo.
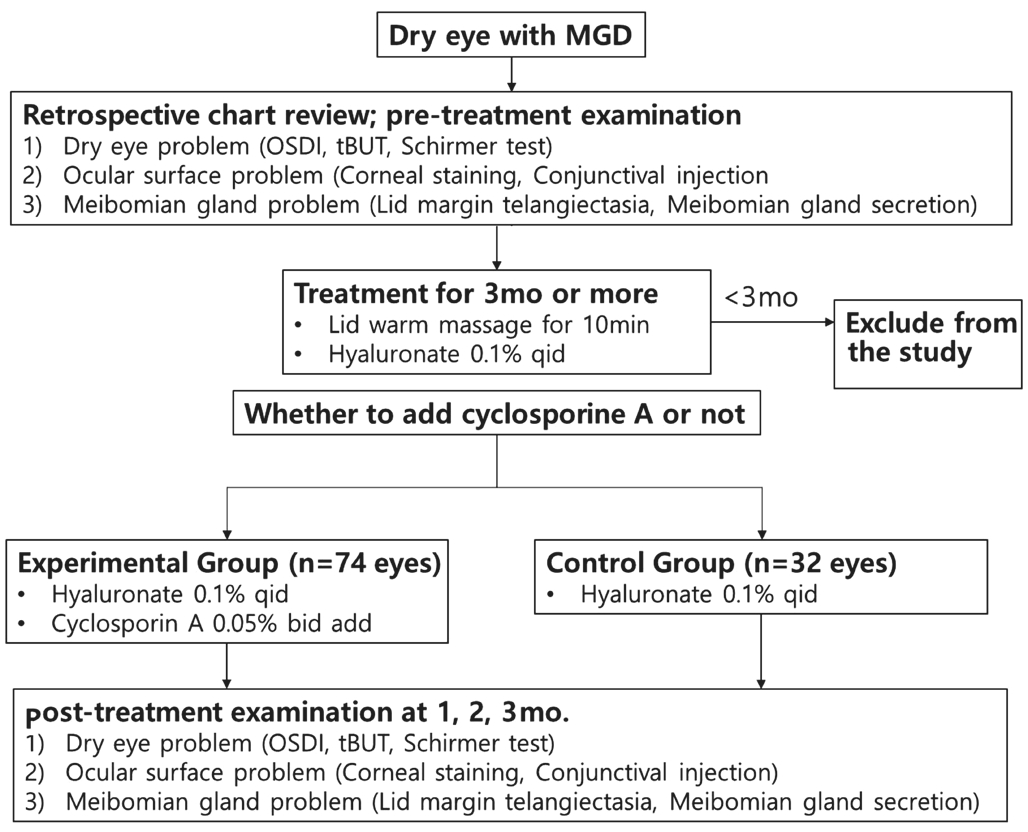
Figure 1 Examination flow diagram in this study MGD: Meibomian gland dysfunction; OSDI: Ocular surface disease index; tBUT: Tear film break-up time.
All patients underwent lid warming massage for 10min before bedtime, and preservatives free 0.1% sodium hyaluronate solution was applied four times a day. Topical 0.05% CsA eyedrop was applied twice a day in the experimental group and the group without cyclosporine eye drop use was defined as a control eye group. All patients were followed up at baseline and 1, 2 and 3mo after instillation to determine the therapeutic effect. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Clinical Assessment Data extracted from medical charts included subjective symptoms and signs: patient demographics,medication history, dry eye problems; ocular surface disease index (OSDI), tBUT, and Schirmer test, ocular surface problems; corneal staining (CS) score, and conjunctival injection (CI) score, MGD problems; lid margin telangiectasia(LMT) score, and meibomian gland secretion (MGS) score.
Dry Eye Problems The OSDI is an indicator of the change in symptoms that it is composed of 12 questions related to dry eye syndrome[26]. It is assessed on a scale of 0 to 100, with higher scores representing greater disability. The tBUT was measured the number of seconds that elapse between the last blink and the appearance of the first dry spot in the tear film after exposure of the fluorescein paper (Haag-Streit AG, Köniz,Switzerland) to the lower conjunctival sac in the slit lamp blue filter illumination. The Schirmer test was measured using a filtered paper strip (Eagle Vision, Memphis, TN, USA). It was placed inside the lower eyelid to avoid corneal stimulation and left for five minutes. The filtered paper was removed and the amount of wetting was measured in millimeters after five minutes.
Table 1 Baseline patient Characteristics mean±SD
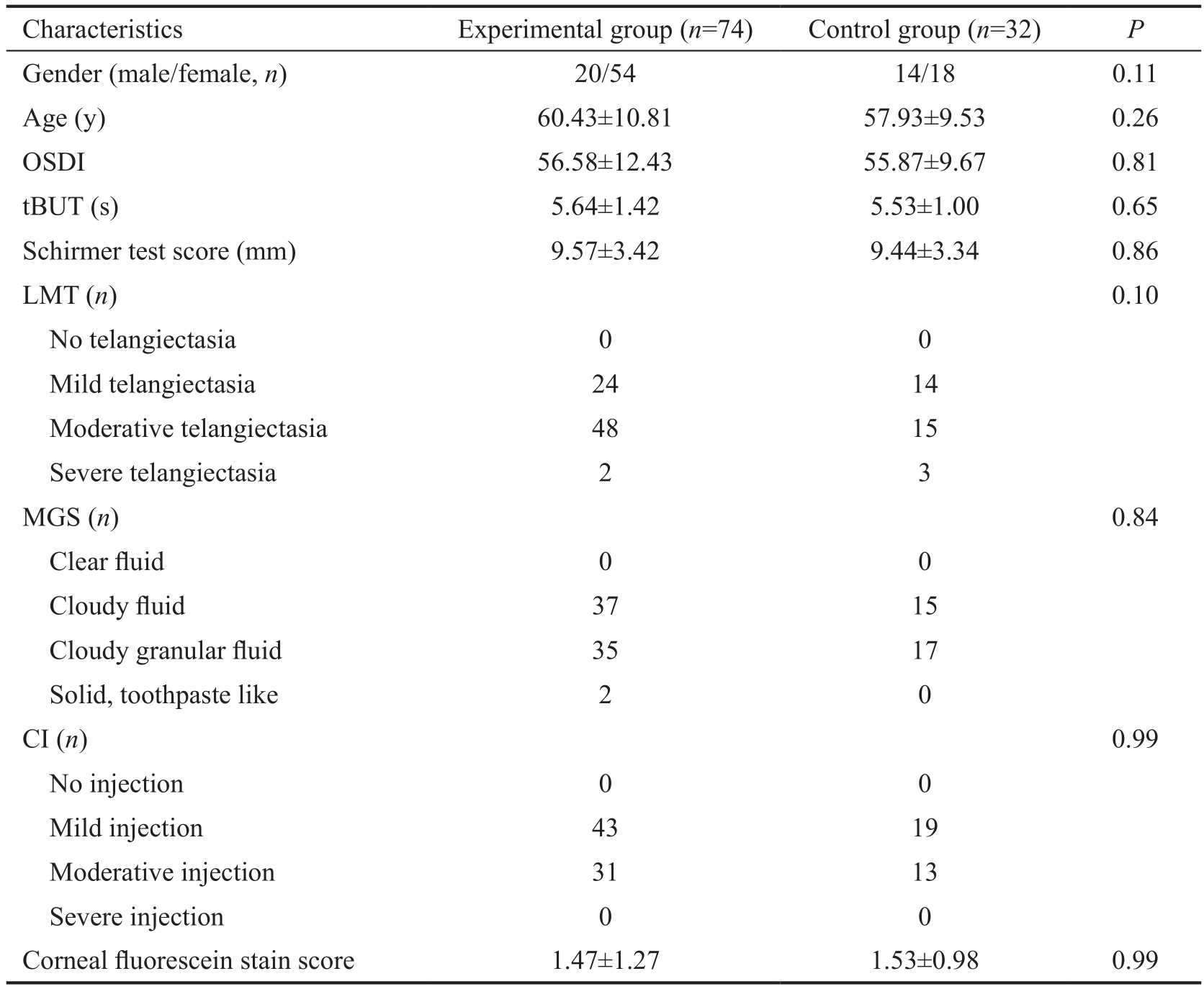
OSDI: Ocular surface disease index; tBUT: Tear film break-up time; LMT: Lid margin telangiectasia; MGS:Meibomian gland secretion; CI: Conjunctival injection. There was no difference between two groups at baseline.
Ocular Surface Problem CS score was performed according to the method described by National Eye Institute[27]. The cornea was divided into 5 regions in the middle and upper,lower, left and right regions. When each area was not stained,0 point was obtained. When there was a slight surface staining,1 point was observed. When there is a slight overlapping speckle, 2 point was observed. When there are multiple stainings or large spots, 3 point was observed and the total score was from 0 to 15. CI score was defined as 0 point for normal, 1 point for mild congestion, 2 points for moderate congestion, and 3 points for severe congestion according to the degree of vasodilatation of the bulbar conjunctiva with reference to Efron et al’s[28]grading scales.
Meibomian Gland Dysfunction Problems There are about 30-40 glands in upper lid margin, and fewer (20-40) in the lower lid margin, and the vascular zone, which can be observed with telangiectasia, is the zone from the mucocutaneous junction near the meibomian gland orifice to the eyelash root.It is easier to observe the talangiectasia in the upper because the vascular zone in the upper eyelid is wider than in the lower eyelid. The LMT was scored based on the degree of telangiectasia at the upper eyelid margin, with 0 points in the absence of capillary dilatation, 1 point in the case of mild capillary dilatation, 2 points in the case of moderate capillary dilatation, and severe capillary dilatation was defined as 3 points[29]. For measurement of MGS, we pressed softly skin and palpable conjunctiva near the center of upper lid margin using a sterilized cotton swab. MGS is defined as 0 point for secretion of clear secretion, 1 point for turbid secretion,2 points for granular secretion, and 3 points for solid form secretion from meibomian orifice[30].
Data Analysis Statistical analysis was performed using SPSS software version 20 for windows (SPSS Inc., Chicago,IL, USA). Repeated measures ANOVA was used for the comparison of effects between the two groups according to time, and Tukey test was used for post-test. Student’s t-test was used to compare the mean changes from baseline between two groups at each time point. P-value less than 0.05 was considered statistically significant.
RESULTS
Data were collected on 106 eyes (53 patients) from five clinical sites. There were no differences between the two groups in the baseline test results including gender, age, OSDI, tBUT,Schirmer test, CS score, CI, LMT, MGS (Table 1).
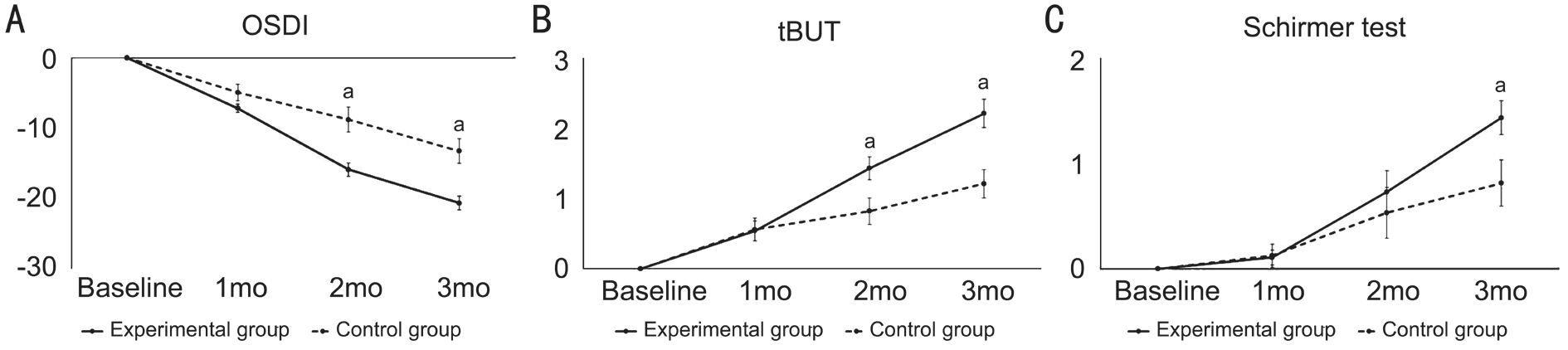
Figure 2 Mean changes in OSDI (A), tBUT (B) and Schirmer test score (C) from baseline to 3mo At 2 and 3mo, the mean changes of OSDI were significantly higher in the experimental group than in the control group (P<0.001, P<0.001); The mean changes of tBUT were significantly higher in the experimental group than in the control group (P=0.031, 0.001). At 3mo, the mean change of Schirmer test was significantly higher in the experimental group than in the control group (P=0.029).aP<0.05 between two groups according to Student’s t-test.
Table 2 The changes of OSDI, tBUT, Shcirmer test, and LMT in two groups for 3mo of treatment mean±SD
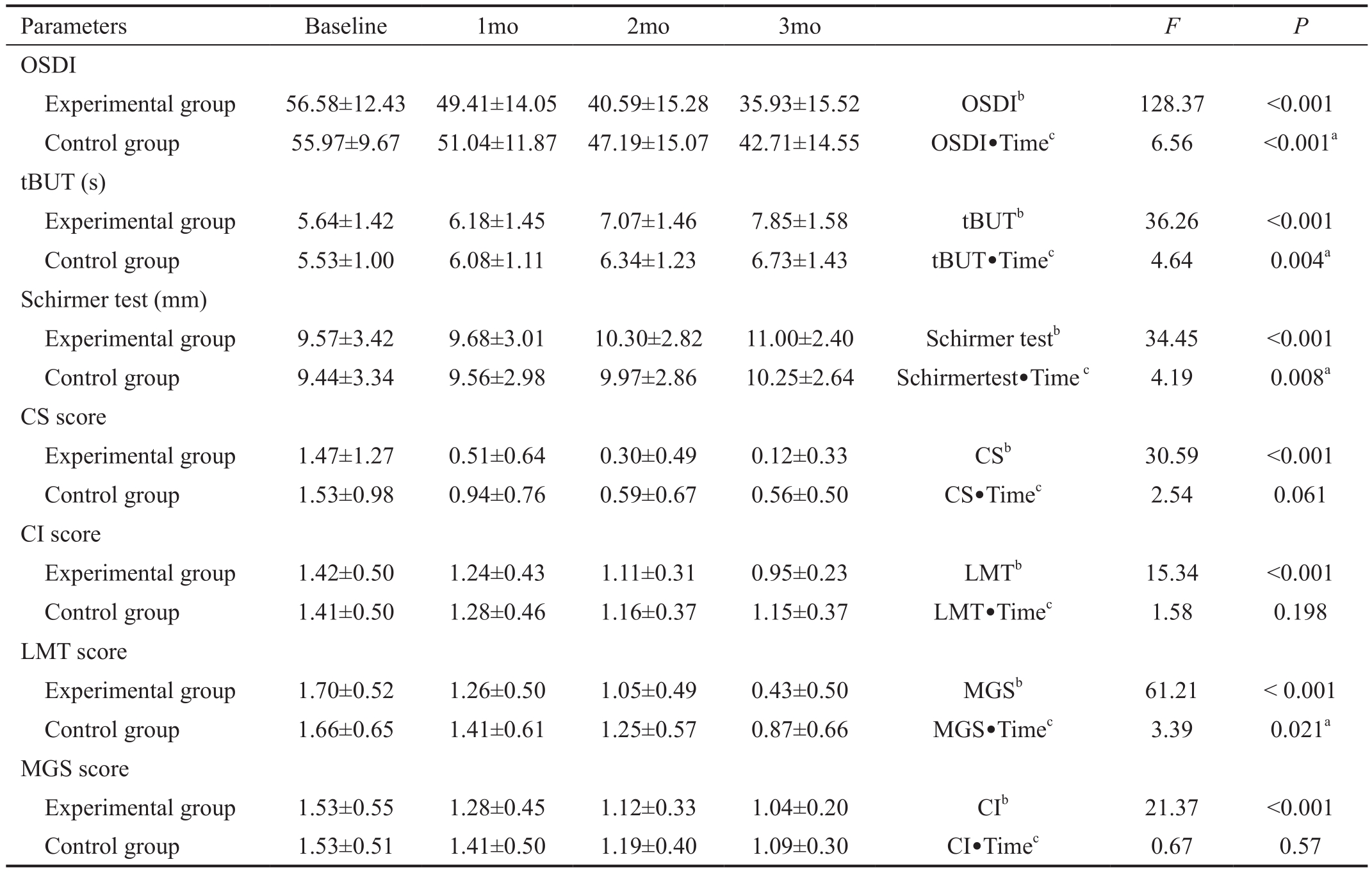
aP<0.05 between experimental group and control group according to repeated measures ANOVA;bVariable values were changed statistically significantly with time;cThe change of the variable was statistically significantly different depending on the group. OSDI: Ocular surface disease index; tBUT: Tear film break-up time; CS: Corneal stain; CI: Conjunctival injection; LMT: Lid margin telangiectasia; MGS: Meibomian gland secretion.
Dry Eye Problem (OSDI, tBUT and Schirmer Test) There was a significant difference in OSDI improvement between two groups by repeated measure ANOVA (F=6.564, P<0.001;Table 2). And mean changes from baseline to 2 and 3mo after instillation were -15.89±0.97, -20.65±0.97 in the experimental group and -8.78±1.76, -13.26±1.76 in the control group, showing a statistically significant improvement in the experimental group compared with the control group (P<0.001, P<0.001; Figure 2A).There was a significant difference in tBUT improvement between two groups by repeated measure ANOVA (F=4.643,P=0.004; Table 2). And mean changes from baseline to 2 and 3mo after instillation were 1.43±0.16, 2.21±0.20 in the experimental group and 0.82±0.19, 1.21±1.16 in the control group, showing a statistically significant improvement between two groups (P=0.031, P=0.001; Figure 2B).
There was a significant difference in Schirmer test improvement between two groups by repeated measure ANOVA (F=4.19, P=0.008; Table 2). And mean changes from baseline to 3mo after instillation were 1.43±1.35 in the experimental group and 0.82±1.22 in the control group,showing a statistically significant improvement between two groups (P=0.029; Figure 2C).
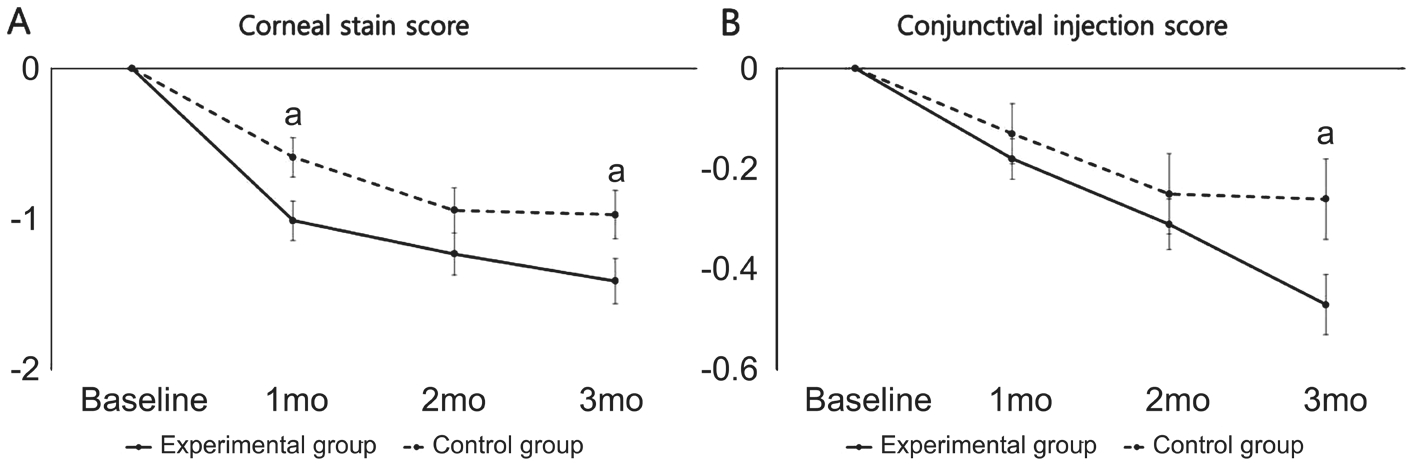
Figure 3 Mean change in CS score (A) and CI score (B) from baseline to 3mo At 1 and 3mo, the mean changes of CS score were significantly higher in the experimental group than in the control group (P=0.048, 0.047). At 3mo, the mean changes of CI score were significantly higher in the experimental group than in the control group (P=0.030).aP<0.05 between two groups according to Student’s t-test.
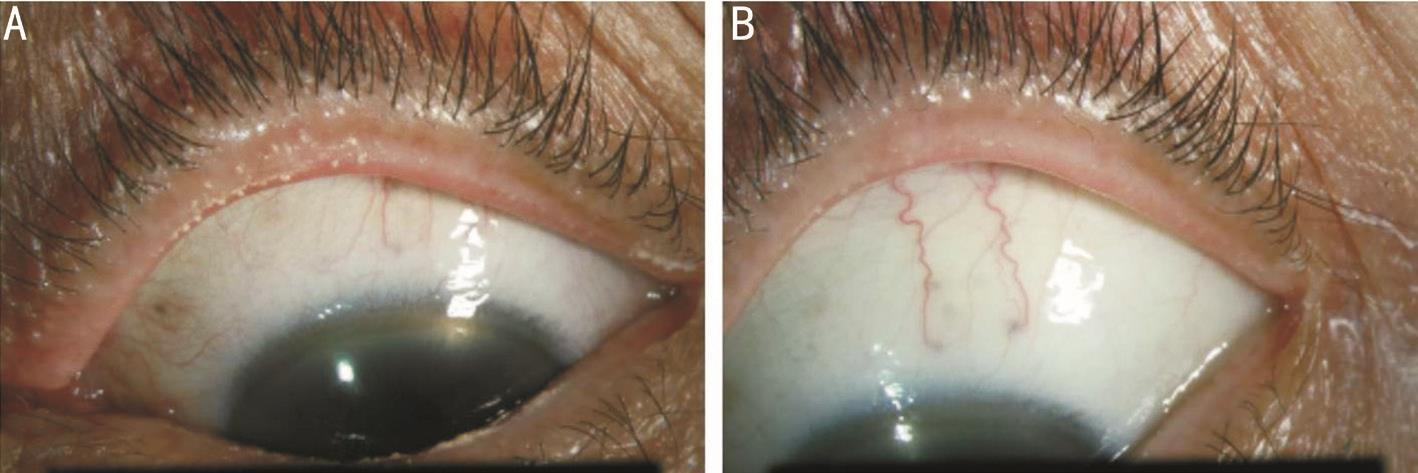
Figure 4 Left eyelid margin and bulbar conjunctiva of a patient with meibomian gland dysfunction A: Before treatment; B: After treatment with 0.05% CsA. Improvement of LMT and hygiene was observed and bulbar CI was also decreased.
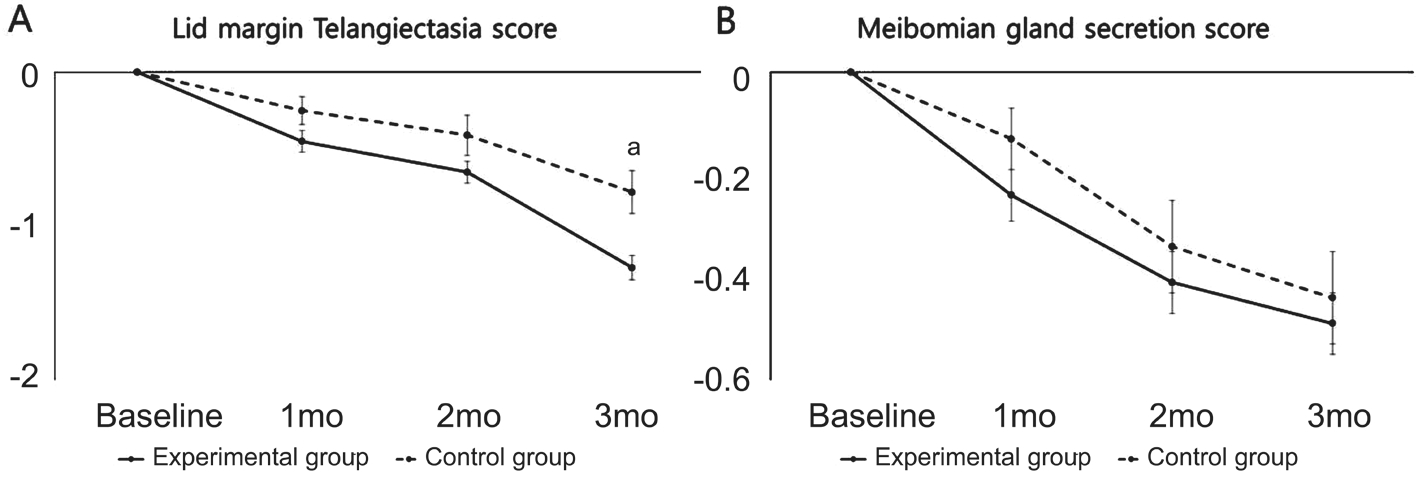
Figure 5 Mean change in LMT score (A) and MGS score (B) from baseline to 3mo At 3mo, the change of LMT score was significantly higher in the experimental group than control group (P=0.002). The MGS score was no significantly different between two groups at all points.aP<0.05 between two groups according to Student’s t-test.
Ocular Surface Problems (Corneal Staining Score and Conjunctival Injection Score) There was no significant difference in CS improvement between two groups (F=2.535,P=0.061; Table 2). However, mean changes from baseline to 1 and 3mo after instillation were -1.01±0.13, -1.41±0.15 in the experimental group and -0.59±0.13, -0.97±0.16 in the control group, showing a statistically significant improvement between two groups (P=0.048, 0.047; Figure 3A).
There was no significant difference in CI score improvement between two groups (F=1.027, P=0.384; Table 2). Mean changes from baseline at 3mo after instillation were -0.47±0.06 in the experimental group and -0.25±0.08 in the control group,showing a statistically significant improvement between two groups (P=0.030; Figure 3B).
MGD Problems (Lid Margin Telangiectasia Score And Meibomian Gland Secretion Score) There was a significant difference in improvement of LMT score between two groups by repeated measure ANOVA (F=3.391, P=0.021; Table 2,Figure 4). Mean changes from baseline to 3mo after instillation were -1.27±0.08 in the experimental group and -0.78±0.14 in the control group, showing a statistically significant improvement between two groups (P=0.002; Figure 5A).
There was no significant difference in improvement of MGS score between two groups (F=0.671, P=0.571; Table 2). And there was also no significant difference in mean changes of MGS score between the two groups at all points by Student’s t-test (P>0.05; Figure 5B).
DISCUSSION
In this study, CsA is effective to treat symptoms and signs in MGD. Patients were treated with eyelid warming massage for 10min and artificial tear solution, which are widely used as treatments for MGD, and patients were classified according to whether CsA was added or not. CsA-added group(experimental group) was statistically significant better in the improvement of OSDI, tBUT, Schirmer test and LMT over time for 3mo compared with the control group respectively.Especially at 3mo of treatment, the CsA-added group was more effective than the control group in terms of OSDI, tBUT,Schirmer test, CS, LMT, CI.
MGD is blockage or some other abnormality of the meibomian glands. MGD can lead to inflammation of the meibomian glands and excess oil in the tear film. In MGD, concentrations of inflammatory cytokines such as epidermal growth factor(EGF), interleukin-1 (IL-1), interleukin-6 (IL-6), interleukin-8(IL-8), tumor necrosis factor-α (TNF-α) are increased[10-11,31].And these increased inflammatory cytokines have been reported to be associated with CS[10-11], conjunctival staining and injection[9-10,12], tear film instability[13]as well as ocular discomfort[10-11]in dry eye syndrome. Increased inflammation in MGD affects not only ocular surface but also eyelid margin including meibomian gland, causing angiogenesis and capillary dilatation around the margin of the eyelid and meibum stasis[8-9,29]. Therefore, TFOS workshop on MGD recommends anti-inflammatory treatment for stage 3 MGD or worse that meibomian orifice plugging and vascularity are found[8]. In this study, we investigated MGD patients with lid margin plugging or increased vascularity, well known for lid margin inflammation.
CsA is a widely used anti-inflammatory agent for the management of dry eye disease. It is known as it regulates immune function in conjunctival and lacrimal cells of dry eye syndrome resulting to reduce inflammation and to increase tear production. Due to this property, topical CsA has been successfully used in dry eye and other ocular inflammatory disease. Inflammation is not the core mechanism of MGD, but it induces atrophy of secretory acini and evaporative dry eye syndrome. It also induces increased viscosity of meibum through changes of meibum quality and quantity. Threfore, the reduction of inflammation due to the use of CsA seems to improve symptoms of MGD and dry eye syndrome.
This study suggests that topical CsA may decrease the inflammation of the ocular surface and meibomian gland. CS and CI are known to be related to ocular surface inflammation.And LMT or meibum stasis is one of the many indicator that represent inflammation of meibomian gland. In this study,CsA treatment for 3mo provided statistically significant improvement in CS, CI, and LMT as compared with group without topical CsA. Increased cytokines are associated with CS, CI, and LMT. CS has been associated with increased inflammatory cytokines and has improved through antiinflammatory therapy. CI and LMT are reported to be associated with an increase of interleukin-17 (IL-17). IL-17 is increased to T-cell mediated in dry eye syndrome and MGD[32-33], and IL-17 can induce CI and LMT by stimulating secretion of VEGF and other angiogenic chemokine[12]. CsA lowers cytokines through T-cell immune regulation and may improve inflammatory markers[34]. Based on the results of this study, we suggest that the anti-in flammatory property of CsA can decrease tear cytokine levels significantly, resulting in reduction of CS and CI indicating ocular surface inflammation and eyelid telangiectasia indicating eyelid margin inflammation.
We found that OSDI, CS and Schirmer test were improved better in experimental group. MGD is a major cause of evaporative dry eye syndrome, and most symptoms in MGD patients are consistent with dry eye symptoms. It is well known that CsA increases tear volume through inflammation control of lacrimal gland and improve tear film stability by increasing mucin through increasing number and density of conjunctival goblet cells[19,35]. Increased tear volume and improved tear film stability seem to have improved the symptoms of dry eye syndrome in MGD patients.
However, there was no additional effect of CsA on MGS,in contrast to previous studies of CsA in MGD showing significantly improved MGS. The difference in whether or not undergoing lid hygiene may account for this difference.Obstruction of meibomian gland causes meibum stasis,resulting to inflammation and bacterial overgrowth. This changes normal meibum to abnormal, which has a melting point above the ocular surface temperature. According to TFOS, warm massage is recommended from the initial treatment of MGD[8]. And Guillon et al[36]reported the improvement of MGS with only eyelid hygiene as like eyelid warm massage and Blephaclean wipes. In our study, all patients underwent lid warm massage for 10min essentially.The MGS was improved in both groups. And there was no statistical significance between the two groups, although the experimental group showed better improvement than the control group. It is important to stop the vicious cycle between meibum stasis and inflammation through treatment with CsA,but it is expected to take longer, and lid hygeine, such as warm massage, is effective in improving early meibum stasis.Meibomian gland occlusion resulted from meibum stasis are improved by lid hygiene, such as eyelid warm massage, thus the benefits of using additional CsA are limited in this study.
We found that improvement of subjective and objective symptoms including reduction of inflammation were con firmed by steady treatment for about 3mo. In this study, topical CsA instillation for 3mo was more effective to treat MGD according to repeated measures analysis of variance. And there was a significant difference at 3 mo, but no difference at 1 and 2mo according Student’s t-test between two groups. Our results are consistent with other reports. Perry et al[37]and Fakhraie et al[38]reported that symptoms of dry eye was improved at 3-6mo after CsA instillation. And Rubin et al[25]showed that CsA shows less improvement at 1mo but better at 3mo after treatment against dexamethasone in posterior blepharitis,suggesting that CsA has a slow but better effect. Short-term treatment due to ocular discomfort at initial treatment makes the benefits limited, therefore long-term treatment for at least 3mo is considered necessary. This point means some big advantages of CsA induced anti-inflammatory reaction of ocular surface and eyelid compared with long-term therapy of topical steroid eye drops. Long-term usage of topical steroid eye drops has the possible complications, such as cataract,glaucoma and infection, while long-term usage of topical CsA has rare of these[39].
In conclusion, CsA not only alleviates symptoms and signs of dry eye associated with MGD, but also is effective in controlling inflammation of eyelid or dysfunction of meibomian gland.Therefore additional use of topical CsA in cases that do not respond to conservative treatments in MGD, such as artificial tear and eyelid hygiene, helps to reduce inflammation of ocular surface and eyelid margin, resulting to improve symptoms and signs. However, additional effects of CsA on MGS have not been identified in this study, so further studies are needed to further investigate the effect of CsA on meibomian glands,such as structure of meibomian gland, charicteristics of meibum.
ACKNOWLEDGEMENTS
Foundation:Supported by a grant from University Research Park Project of Busan National University funded by Busan Institute of S&T Evaluation and Planning (No.201726550002).
Conflicts of Interest:Kim HY, None; Lee JE, None; Oh HN,None; Song JW, None; Han SY, None; Lee JS, None.
REFERENCES
1 Geerling G, Baudouin C, Aragona P, Rolando M, Boboridis KG,Benítez-del-Castillo JM, Akova YA, Merayo-Lloves J, Labetoulle M,Steinhoff M, Messmer EM. Emerging strategies for the diagnosis and treatment of meibomian gland dysfunction: proceedings of the OCEAN group meeting. Ocul Surf 2017;15(2):179-192.
2 Baudouin C, Messmer EM, Aragona P, Geerling G, Akova YA,Benítez-del-Castillo J, Boboridis KG, Merayo-Lloves J, Rolando M,Labetoulle M. Revisiting the vicious circle of dry eye disease: a focus on the pathophysiology of meibomian gland dysfunction. Br J Ophthalmol 2016;100(3):300-306.
3 Borchman D, Foulks GN, Yappert MC, Bell J, Wells E, Neravetla S,Greenstone V. Human meibum lipid conformation and thermodynamic changes with meibomian-gland dysfunction. Invest Ophthalmol Vis Sci 2011;52(6):3805-3817.
4 Thode AR, Latkany RA. Current and emerging therapeutic strategies for the treatment of meibomian gland dysfunction (MGD). Drugs 2015;75(11):1177-1185.
5 Lee H, Chung B, Kim KS, Seo KY, Choi BJ. Kim TI. Effects of topical loteprednol etabonate on tear cytokines and clinical outcomes in moderate and severe meibomian gland dysfunction: randomized clinical trial. Am J Ophthalmol 2014;158(6):1172-1183.
6 Liu Y, Kam WR, Ding J, Sullivan DA. Can tetracycline antibiotics duplicate the ability of azithromycin to stimulate human meibomian gland epithelial cell differentiation? Cornea 2015;34(3):342-346.
7 Mizoguchi S, Iwanishi H, Arita R, Shirai K, Sumioka T, Kokado M,Jester JV, Saika S. Ocular surface inflammation impairs structure and function of meibomian gland. Exp Eye Res 2017;163:78-84.
8 Nichols KK, Foulks GN, Bron AJ, Glasgow BJ, Dogru M, Tsubota K,Lemp MA, Sullivan DA. The international workshop on meibomian gland dysfunction: executive summary. Invest Ophthalmol Vis Sci 2011;52(4):1922-1929.
9 Prabhasawat P, Tesavibul N, Mahawong W. A randomized doublemasked study of 0.05% cyclosporine ophthalmic emulsion in the treatment of meibomian gland dysfunction. Cornea 2012;31(12):1386-1393.
10 Lam H, Bleiden L, De Paiva CS, Farley W, Stern ME, P flugfelder SC.Tear cytokine pro files in dysfunctional tear syndrome. Am J Ophthalmol 2009;147(2):198-205.
11 Enríquez-de-Salamanca A, Castellanos E, Stern ME, Fernández I,Carreño E, García-Vázquez C, Herreras JM, Calonge M. Tear cytokine and chemokine analysis and clinical correlations in evaporative-type dry eye disease. Mol Vis 2010;16:862-873.
12 Kim JT, Lee SH, Chun YS, Kim JC. Tear cytokines and chemokines in patients with Demodex blepharitis. Cytokine 2011;53(1):94-99.
13 Lee SY, Han SJ, Nam SM, Yoon SC, Ahn JM, Kim TI, Kim EK,Seo KY. Analysis of tear cytokines and clinical correlations in Sjögren syndrome dry eye patients and non-Sjögren syndrome dry eye patients.Am J Ophthalmol 2013;156(2):247-253.
14 Arman A, Demirseren DD, Takmaz T. Treatment of ocular rosacea:comparative study of topical cyclosporine and oral doxycycline. Int J Ophthalmol 2015;8(3):544-549.
15 Muftuoglu IK, Akova YA, Gungor SG. Effect of 0.05% topical cyclosporine for the treatment of symptomatic subepithelial infiltrates due to adenoviral keratoconjunctivitis. Int J Ophthalmol 2016;9(4):634-635.
16 Chen JJ, Applebaum DS, Sun GS, Pflugfelder SC. Atopic keratoconjunctivitis: a review. J Am Acad Dermatol 2014;70(3):569-575.
17 Pucci N, Caputo R, Grande L, de Libero C, Mori F, Barni S, di Simone L, Calvani A, Rusconi F, Novembre E. Tacrolimus vs. cyclosporine eyedrops in severe cyclosporine-resistant vernal keratoconjunctivitis: A randomized, comparative, double-blind, crossover study. Pediatr Allergy Immunol 2015;26(3):256-261.
18 Kiang E, Tesavibul N, Yee R, Kellaway J, Przepiorka D. The use of topical cyclosporin A in ocular graft-versus-host-disease. Bone Marrow Transplant 1998;22(2):147-151.
19 Zhou XQ, Wei RL. Topical cyclosporine A in the treatment of dry eye:a systematic review and meta-analysis. Cornea 2014;33(7):760-767.
20 Qiao J, Yan X. Emerging treatment options for meibomian gland dysfunction. Clin Ophthalmol 2013;7:1797-1803.
21 Schein OD, Muñoz B, Tielsch JM, Bandeen-Roche K, West S.Prevalence of dry eye among the elderly. Am J Ophthalmol 1997;124(6):723-728.
22 Lin PY, Tsai SY, Cheng CY, Liu JH, Chou P, Hsu WM. Prevalence of dry eye among an elderly Chinese population in Taiwan: the Shihpai Eye Study. Ophthalmology 2003;110(6):1096-1101.
23 Jie Y, Xu L, Wu YY, Jonas JB. Prevalence of dry eye among adult Chinese in the Beijing Eye Study. Eye(Lond) 2009;23(3):688-693.
24 Perry HD, Doshi-Carnevale S, Donnenfeld ED, Solomon R, Biser SA, Bloom AH. efficacy of commercially available topical cyclosporine A 0.05% in the treatment of meibomian gland dysfunction. Cornea 2006;25(2):171-175.
25 Rubin M, Rao SN. Efficacy of topical cyclosporin 0.05% in the treatment of posterior blepharitis. J Ocul Pharmacol Ther 2006;22(1):47-53.
26 Schiffman RM, Christianson MD, Jacobsen G, Hirsch JD, Reis BL. Reliability and validity of the ocular surface disease index. Arch Ophthalmol 2000;118(5):615-621.
27 Lemp MA. Report of the National Eye Institute/Industry workshop on clinical trials in dry eyes. CLAO J 1995;21(4):221-232.
28 Efron N, Morgan PB, Katsara SS. Validation of grading scales for contact lens complications. Ophthalmic Physiol Opt 2001;21(1):17-29.
29 Foulks GN, Bron AJ. Meibomian gland dysfunction: a clinical scheme for description, diagnosis, classification, and grading. Ocul Surf 2003;1(3):107-126.
30 Arita R, Suehiro J, Haraguchi T, Maeda S, Maeda K, Tokoro H, Amano S. Topical diquafosol for patients with obstructive meibomian gland dysfunction. Br J Ophthalmol 2013;97(6)725-729.
31 Massingale ML, Li X, Vallabhajosyula M, Chen D, Wei Y, Asbell PA. Analysis of inflammatory cytokines in the tears of dry eye patients.Cornea 2009;28(9):1023-1027.
32 Chen Y, Chauhan SK, Lee HS, Saban DR, Dana R. Chronic dry eye disease is principally mediated by effector memory Th17 cells. Mucosal Immunol 2014;7(1):38-45.
33 Kang MH, Kim MK, Lee HJ, Lee HI, Wee WR, Lee JH. Interleukin-17 in various ocular surface inflammatory diseases. J Korean Med Sci 2011;26(7):938-944.
34 Hessen M, Akpek EK. Dry eye: an inflammatory ocular disease. J Ophthalmic Vis Res 2014;9(2):240-250.
35 Wan KH, Chen LJ, Young AL. efficacy and safety of topical 0.05%cyclosporine eye drops in the treatment of dry eye syndrome: a systematic review and meta-analysis. Ocular Surf 2015;13(3):213-225.
36 Guillon M, Maissa C, Wong S. Eyelid margin modification associated with eyelid hygiene in anterior blepharitis and meibomian gland dysfunction. Eye Contact Lens 2012;38(5):319-325.
37 Perry HD, Solomon R, Donnenfeld ED, Perry AR, Wittpenn JR,Greenman HE, Savage HE. Evaluation of topical cyclosporine for the treatment of dry eye disease. Arch Ophthalmol 2008;126(8):1046-1050.
38 Fakhraie G, Lopes JF, Spaeth GL, Almodin J, Ichhpujani P, Moster MR. Effects of postoperative cyclosporine ophthalmic emulsion 0.05%(Restasis) following glaucoma surgery. Clin Exp Ophthalmol 2009;37(9):842-848.
39 Foulks GN, Forstot SL, Donshik PC, Forstot JZ, Goldstein MH,Lemp MA, Nelson JD, Nichols KK, P flugfelder SC, Tanzer JM. Asbell P, Hammitt K, Jacobs DS. Clinical guidelines for management of dry eye associated with Sjögren disease. Ocul Surf 2015;13(2):118-132.