INTRODUCTION
Descemet-stripping automated endothelial keratoplasty(DSAEK) has become the primary surgical treatment for endothelial dysfunction. And increasingly articles have focused on combining DSAEK with other surgeries. Intraocular lens(IOL) surgery is the most commonly combined procedure with DSAEK. As the cornea and crystalline lens are both classified as belonging to the anterior segment, the surgeries can be performed through the same incision, which reduces iatrogenic astigmatism. For eyes with intact posterior capsules, a typical surgical method used is “in-the-bag” IOL implantation[1-3]. A suture-fixated IOL is an effective method, which is often used in eyes without capsular support[4-5], but it has its disadvantages,including being a challenging technique, having a long surgery duration, and requiring excessive manipulation. Possible complications of the suture- fixated IOL include suture break,cystoid macular edema and exposure of the haptic suture[6-8].
Many studies have reported favorable outcomes of the irisclaw IOL since it was first implanted in 1986. The iris-claw IOL can be implanted to correct myopia in phakic patients and it has been used for aphakia[9-10]. The artisan aphakia IOL(Ophthec BV, Groningen, the Netherlands), one of the latest versions of the iris- fixated IOL, is a single-piece IOL. There is one haptic on both sides of the optic. The haptics have fine fissures to capture a fold of midperipheral iris stroma. The manipulation is simpler, the surgical time is shorter, the impact is lessened on the corneal endothelial cells and long-term observation shows a good outcome[11-12].
Because of perforating ocular trauma and cataract surgery failure, many patients in China have endothelial dysfunction and lenses that have no capsular support. DSAEK and artisan aphakia IOL implantation was performed for these patients in the Peking University Third Hospital. This study evaluates complications and outcomes of DSAEK combined with artisan aphakia IOL implantation and resolving of the related complications.
SUBJECTS AND METHODS
We retrospectively reviewed 29 consecutive eyes with bullous keratopathy (BK) and absence of posterior capsule support.Surgeries that combined DSAEK with IOL were performed at Peking University Eye Center from June 2008 to December 2011. Abnormal anterior segment structure and a complicated intraocular surgical history were the common characteristics among the 29 eyes. All DSAEK procedures were performed by Professor Hong. The lens surgeries were performed by Professor Hao.
All procedures performed in studies involving human participants were in accordance with the ethical standards of Peking University Third Hospital’s Institutional Review Board and with the Helsinki Declaration and its later amendments or comparable ethical standars. Informed consent was obtained from all individual participants included in the study.
Surgical Technique The surgery was performed under retrobulbar anesthesia. The host corneal epithelium was marked with a 7.5-8.5 mm trephine stained with gentian violet dye. A 5.5-mm superotemporal corneoscleral tunnel incision was made. Two vertical paracentral paracenteses (at the 10 and 2 o’clock positions) were performed. The edematous corneal epithelium and subepithelium fibrous membrane were removed. The anterior chamber (AC) was filled with viscoelastic (Healon GV, Alcon Surgical, Inc., Ft. Worth,Texas, America). AC-IOL was extracted. The synechia was separated. The fibrous membrane was removed when it was found over the iris and angle of the AC. Anterior vitrectomy was performed. AC was filled again with viscoelastic to support the AC and tamponade the vitreous. Artisan aphakia IOL was inserted into the AC upside-down. With the aid of lens fixation forceps, the IOL was slipped through the pupil area and placed behind the iris plane. The body of the lens was clamped by the forceps to maintain position and centered over the pupil. Through paracentesis, a modified blunt enclavation needle was introduced. By applying gentle pressure over the slotted center of the lens haptic, the iris was entrapped. The iris was folded to ensure lasting lens stability and to prevent it from moving into the vitreous. IOL was then fixated behind the iris plane. The viscoelastic was irrigated out of the AC by balanced salt solution. Then DSAEK was performed. The basic procedures were similar as to what was reported by Terry et al[13]. All the grafts were inserted by Busin glide(Moria USA, Doylestown, Pennsylvania, USA).
Main Outcome Measures Best corrected visual acuity(BCVA) and intraocular pressure (IOP) were noted and compared with that the preoperative data. A slit lamp (Suzhou 66 Vision Tech Co., Ltd, China) and anterior segment optical coherence tomography (Carl Zeiss Meditec, Inc., Dublin California, USA) were utilized to observe the grafts and IOL.The refraction and astigmatism were observed with a Pentacam(Pentacam 70700: Oculus, Wetzlar, Germany). The endothelial cell density (ECD) was counted by laser confocal scanning microscopy (HRT III Heidelberg Engineering, Heidelberg,Germany).
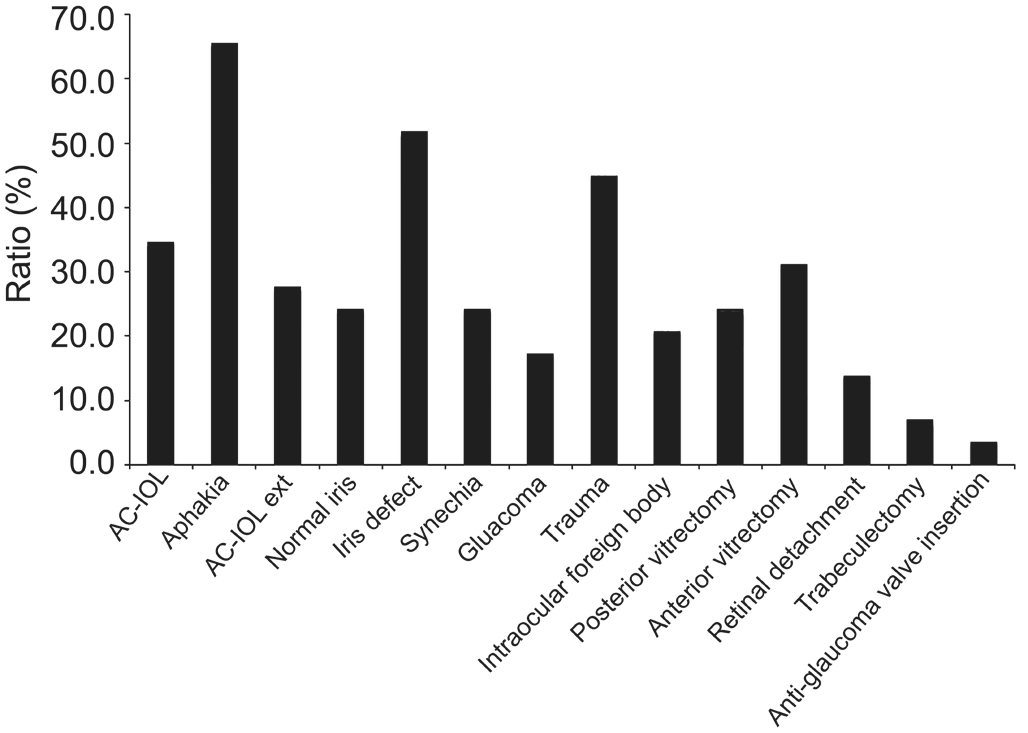
Figure 1 The rate of preoperative ocular situations and past history Ten eyes (34.5%) had AC-IOL. Nineteen eyes (65.5%) were aphakic, including 8 eyes (27.6%), which had AC-IOL extraction.Only 7 eyes (24.1%) had normal irises. The irises of the other 22 eyes (75.9%) were abnormal (51.7% had an iris defect and 24.1%had synechia). Five eyes (17.2%) had glaucoma. Two eyes had trabeculectomy and anti-glaucoma valve insertion. Thirteen eyes(44.8%) had ocular trauma and 6 eyes (20.7%) had an intraocular foreign body. Seven eyes (24.1%) had posterior vitrectomy. Two eyes had retinal detachment and had surgical treatment.
RESULTS
Availability of Data and Materials The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Patient Demographics Twenty-nine eyes of 29 patients underwent DSAEK combined with artisan aphakia IOL implantation. The average age at the time of surgery was 60y(range, 15-88). Of the 29 patients, 26 were male and 3 were female. The ratio of left eye to right eye was 13:16. Common characteristics were abnormal eye structure and complicated ocular surgery history. Thirteen cases had prior ocular trauma,10 cases had AC-IOL, and 16 cases had prior vitrectomy. The iris was abnormal in 22 cases. Preoperative ocular trauma and surgical history is shown in Figure 1.
Visual Acuity Preoperative mean BCVA in this study was 20/286 (range from 20/6060 to 20/120). For all 29 eyes, BCVA improved significantly. During the 6mo period, visual acuity was obtained for all eyes. The mean BCVA improved to 20/42(range from 20/1000 to 20/20). BCVA was 20/20 in 5 cases and varied from 20/20 to 20/32 in 14 cases. The BCVA of 4 eyes was lower than 20/200.
Endothelial Cell Density The mean preoperative donor ECD was 3010±302 cells/mm2(range from 2876 to 3520 cells/mm2).At the 6mo postoperative interval, the mean ECD had diminished to 1965.3±282 cells/mm2(range from 1279 to 2537 cells/mm2). The donor endothelial cell loss was 34.7%compared with 3010/mm2preoperative ECD.
Difficult Intraoperative Graft Attachment A significant complication of DSAEK was difficulty in attaching the intraoperative graft. Even with the aid of cohesive viscoelastic,the air bubble in 3 cases did not stay in the AC and migrated into the vitreous cavity during surgery. The graft could not attach to the posterior cornea lamellar. After the air bubble in the posterior chamber was ejected, a large amount of viscoelastic had to be injected into the AC to directly support the graft. In these 3 cases, only viscoelastic was used to fully support the graft during the surgery.
Graft Dislocation The rate of graft dislocation in this study was 17.2% (5/29 eyes). Four grafts and 1 graft dislocation were detected on the 1stand the 7thpostoperative day. All the graft dislocation cases had air reinjected into the AC, but only two of the grafts were successfully reattached by air re-injection alone. One graft inverted, causing trauma to the donor tissue,and the graft was ultimately exchanged.
Intraocular Lens Dislocation IOL dislocation occurred in 2 eyes (6.9%). The haptic at 6 o’clock detached from the iris on the sixth postoperative day, and the haptic at 9 o’clock detached from the iris on the 34thpostoperative day. Repositioning of the IOL was performed. The forceps clawed the body of the IOL.And amount of iris tissue was entrapped into the slot of the dislocated haptic. Each IOL was well positioned behind the iris.
High Intraocular Pressure Nine eyes had high IOP in the early postoperative period. In 4 eyes this was due to use of viscoelastic.After puncturing and releasing some of the viscoelastic, the IOP returned to normal. Five eyes had preoperative glaucoma. The IOP of 4 of these eyes (4/5) were treated and returned to normal.One eye had transscleral cyclophotocoagulation treatment.
DISCUSSION
According to the DSAEK widely performed, other intraocular procedures, such as phacoemucification or IOL exchange, were combined with DSAEK. In previous reports, a suture- fixated IOL was commonly applied for eyes without adequate capsular support.
In this study, we retrospectively analyzed the complications and outcomes of DSAEK combined with artisan aphakia IOL implantation and resolving the related complications that occured.Artisan aphakia IOL implantation was used to correct aphakia in eyes without adequate capsular support. Dighiero et al[14]reported artisan aphakia IOL combined with penetrating keratoplasty, but previously, only two reports referred to this combination surgery. Karimian et al[15]reported a combination of surgical techniques during DSAEK and IOL exchange with a posterior chamber iris-claw IOL enclavated. Lapenna et al[16]reported a case wherein IOL exchange was performed because the artisan IOL broke after DSAEK.
Abnormal Structure of Eyes In this study, the common characteristics among patients was the abnormal structure of the eyes. The situation of the iris was superiorly important for this combination surgery. This was crucial for fixation of the artisan IOL and/or for AC stabilization. If the eye had only had BK, the iris was usually intact and maintained normal tension.If the patient experienced ocular trauma, unfavorable cataract surgery, or other intraocular surgery, the intact iris and tension was destroyed. The artisan-fixated IOL was unstable if there was not enough iris, if the iris was atrophic, or if there was iris synechiae. In these cases, the DSAEK complication rate was increased, especially graft dislocation[17].
Visual Acuity The mean BCVA was 20/42 postoperatively,ranging from 20/1000 to 20/20. In previous reports, the mean BCVA of simple DSAEK was 20/34, and the mean BCVA of DSAEK combined with AC-IOL exchange was 20/40[18-20].The cornea of the eyes was transparent except one cornea had a line keratoleukoma over the pupil. According to our analysis,the reason the BCVA could not reach 20/20 was due to the iris being abnormal in more than half eyes, which made the shape of pupil irregular. This might affect the imaging quality even if a pinhole is applied. Another reason BCVA could not reach 20/20 was the function of the retina and optic nerve.In this study, the preoperative existence of cases of retinal detachment, glaucoma, intraocular trauma, damage to the retina or optic nerve and high corneal astigmatism could have impacted the BCVA negatively.
Endothelial Cell Density For DSAEK surgery, particular attention is paid to ECD, especially the loss of the ECD. The ECD loss rate is stated in many reports (13.1%-47%)[21-23]. In this study, which discusses combination surgeries, the 6mo postsurgical ECD loss rate was 34.7%. Graft manipulation during insertion is the primary cause of endothelial cell loss[24].Graft insertion from simple DSAEK was the last procedure done on all eyes. Before insertion of the graft, the eye was in its optimum state prior to treatment. High postoperative IOP or treatment of complications, such as graft dislocation or IOL dislocation increased the endothelial cell loss.
Graft Dislocation For DSAEK, more attention is focused on the graft dislocation. The rate of graft dislocation in this study was 17.2% (5/29 eyes), which is higher than previous reports.The iris was abnormal in all eyes, and the area of iris defect was more than 1/3. The air bubble can move within the eye.Once the IOP of the posterior chamber is lower than the AC,the air bubble will move to the posterior chamber and the graft will dislocate.
The air bubbles went into the vitreous cavity from the defected area of iris in other eyes. Without the support from the air bubbles, the graft could not reattach well. The air bubbles were ejected from the vitreous cavity and a small amount of Healon was injected between the graft and IOL. Due to its cohesive character, the Healon ball remained in the AC. The needle of the air syringe was inserted in the Healon and produced an air bubble, which was used to successfully reattach one graft.In the other eyes, the air bubble went into the vitreous cavity.Ultimately, a significant amount of Healon was injected behind the graft until the interface gap disappeared. Three days after a successful repositioning surgery, the IOP was high. This was treated by gradually ejecting the Healon, and the IOP returned to normal.
Except for one eye, all grafts reattached well. During repositioning, special procedures were applied to aid the graft attachment. The common method of graft repositioning is reinjection of air, which is usually valid for most cases. For abnormally structured eyes, however, especially for eyes without an intact iris-lens diaphragm, the air cannot stabilize in the AC. In a former published report, a method that used viscoelastic as an aid in reattaching the dislocated graft in abnormally structured eyes[25]. In this study, only 2 grafts successfully reattached just through air reinjection. The air bubbles moved into the vitreous cavity from the area of the iris defect. As stated in our previous work, a small amount of Healon was injected between the graft and IOL[25]. The needle of the air syringe was inserted in the Healon and produced an air bubble to support the graft. The air bubble can be absorbed by the Healon. One graft was reattached in this manner. In the other eye, because the area of iris defect was larger, the air bubble still moved into the vitreous cavity. A significant amount of Healon was then injected behind the graft until the interface gap disappeared. The most likely complication from this procedure is high IOP due to viscoelastic[26-27]. An AC puncture was performed to lower the IOP and release the viscoelastic, which returned the IOP back to normal.
Intraocular Lens Dislocation Dislocation is the most common complication of the iris claw IOL implant[28-29]. Lapenna et al[16]reported 1 case of DSAEK with artisan IOL implantation. The IOL dislocated and was extracted because the iris claw had broken. The IOL implantation is affixed with an iris claw. The condition of the iris is crucial. In our study, artisan aphakia IOLs dislocated in 2 cases. The patient’s iris was not in prime condition due to long-term AC-IOL stimulation leading to iris adhesion and atrophy. Prior to the IOL dislocating, the patient had a graft dislocation and an air bubble was used to reposition the graft. When the air bubble was injected into the AC, the iris and IOL may have been pressed, resulting in one of the claws releasing from the iris. Because the air bubble and corneal edema impeded observation, the dislocation was not discovered until the 6thpostoperative day. Rauen et al[30]have reported on an air bubble leading to posterior IOL dislocation at the point of graft repositioning. In the second dislocation,one temporal claw of the IOL released on the 34thpostoperative day possibly due to postoperative trauma, iris atrophy, or iridocoloboma. The postoperative puncture and release of the viscoelastic could also have contributed to the IOL dislocation.Ultimately, both IOLs were successfully repositioned. If the claw of the dislocated artisan aphakia IOL remains intact, the IOL can be repositioned by simply entrapping the iris through the slotted center of the lens haptic[31-32].
High Intraocular Pressure It is also critical to monitor the patient’s IOP. In this study, 9 eyes had high postoperative IOP. This rate is higher than the previous reports of DSAEK or artisan IOL implantation[23,33]. The higher rate of IOP was caused by two reasons: first was the high rate of preoperative glaucoma and AC-IOL (5/29)[34]; the second was the application of viscoelastic, used either during the DSAEK procedure or to treat the graft dislocation. The AC-IOL injured the endothelium and the angle of the chamber, leading to angle adherence and the fibrosis membrane formation covering the angle(according to ultrasound biomicroscopy and the intraoperative appearance), which caused secondary glaucoma. Inflammatory mediators may have compressed the functional residual angle due to surgical stimulation, breaking the balance and heightening the IOP. The amount of viscoelastic used in eyes that had difficulty in graft attachment excessively exceeded what was used for the patients in the 2009 report, which may be a contributor to the high IOP level. The viscoelastic was punctured and released several times, and the IOP returned to normal. We can conclude that the amount of viscoelastic used critically impacts the IOP.
In conclusion, DSAEK combined with iris claw IOL implantation is an alternative procedure for patients with endothelial keratopathy who have severely damaged eyes and no posterior capsular support. It should be performed cautiously on eyes with severely defected irises.
ACKNOWLEDGEMENTS
The authors would like to acknowledge Tina-Marie Gauthier,Medical Editor and Writer, Eye Cite Editing for editing the grammar of the paper.
Foundations:Supported by the National Natural Science Foundation of China (No.30871315; No.31140025; No.31271045).
Conflicts of Interest:Peng RM, None; Guo YX, None; Qiu Y, None; Hao YS, None; Hong J, None.
REFERENCES
1 Clemmensen K, Ivarsen A, Hjortdal J. Changes in corneal power after descemet stripping automated endothelial keratoplasty. J Refract Surg 2015;31(12):807-812.
2 Kobayashi A, Yokogawa H, Mori N, Sugiyama K. Case series and techniques of descemet’s stripping automated endothelial keratoplasty for severe bullous keratopathy after birth injury. BMC Ophthalmol 2015;15:92.
3 Sykakis E, Lam FC, Georgoudis P, Hamada S, Lake D. Patients with fuchs endothelial dystrophy and cataract undergoing descemet stripping automated endothelial keratoplasty and phacoemulsification with intraocular lens implant: staged versus combined procedure outcomes. J Ophthalmol 2015;2015:172075.
4 Shah AK, Terry MA, Shamie N, Chen ES, Phillips PM, Hoar KL,Friend DJ, Davis-Boozer D. Complications and clinical outcomes of descemet stripping automated endothelial keratoplasty with intraocular lens exchange. Am J Ophthalmol 2010;149(3):390-397.
5 Kristianslund O, Råen M, Østern AE, Drolsum L. Glaucoma and intraocular pressure in patients operated for late in-the-bag intraocular lens dislocation: a randomized clinical trial. Am J Ophthalmol 2017;176:219-227.
6 Hirashima DE, Soriano ES, Meirelles RL, Alberti GN, Nosé W.Outcomes of iris-claw anterior chamber versus iris-fixated foldable intraocular lens in subluxated lens secondary to Marfan syndrome.Ophthalmology 2010;117(8):1479-1485.
7 Yazu H, Yamaguchi T, Dogru M, Ishii N, Satake Y, Shimazaki J. Descemetstripping automated endothelial keratoplasty in eyes with transscleralsutured intraocular lenses. J Cataract Refract Surg 2016;42(6):846-854.
8 Kristianslund O, Råen M, Østern AE, Drolsum L. Late in-the-bag intraocular lens dislocation: a randomized clinical trial comparing lens repositioning and lens exchange. Ophthalmology 2017;124(2):151-159.
9 Shajari M, Scheffel M, Koss MJ, Kohnen T. Dependency of endothelial cell loss on anterior chamber depth within first 4 years after implantation of iris-supported phakic intraocular lenses to treat high myopia. J Cataract Refract Surg 2016;42(11):1562-1569.
10 Güell JL, Verdaguer P, Mateu-Figueras G, Elies D, Gris O, Amich JM,Manero F, Morral M. Unilateral iris-claw intraocular lens implantation for aphakia: a paired-eye comparison. Cornea 2 016;35(10):1326-1332.
11 Park YM, Choi BJ, Lee JS. Effect of incision types for artisan aphakic intraocular lens implantation on ocular higher order aberrations. Int J Ophthalmol 2016;9(12):1785-1789.
12 Aerts AA, Jonker SM, Wielders LH, Berendschot TT, Doors M, De Brabander J, Nuijts RM. Phakic intraocular lens: two-year results and comparison of endothelial cell loss with iris- fixated intraocular lenses. J Cataract Refract Surg 2015;41(10):2258-2265.
13 Terry MA, Shamie N, Chen ES, Hoar KL, Friend DJ. Endothelial keratoplasty a simplified technique to minimize graft dislocation,iatrogenic graft failure, and pupillary block. Ophthalmology 2008;115(7):1179-1186.
14 Dighiero P, Guigou S, Mercie M, Briat B, Ellies P, Gicquel JJ.Penetrating keratoplasty combined with posterior Artisan iris-fixated intraocular lens implantation. Acta Ophthalmol Scand 2006;84(2):197-200.
15 Karimian F, Sadoughi MM. Air-assisted descemet-stripping automated endothelial keratoplasty with posterior chamber iris-fixation of aphakic iris-claw intraocular lens. J Cataract Refract Surg 2011;37(2):224-228.
16 Lapenna L, Kadyan A, Busin M. Intraocular lens exchange 1 week after descemet stripping automated endothelial keratoplasty. Cornea 2010;29(2):207-209.
17 Goshe JM, Terry MA, Li JY, Straiko MD, Davis-Boozer D. Graft dislocation and hypotony after descemet’s stripping automated endothelial keratoplasty in patients with previous glaucoma surgery. Ophthalmology 2012;119(6):1130-1133.
18 Tannan A, Vo RC, Chen JL, Yu F, Deng SX, Aldave AJ. Comparison of ACIOL retention with IOL exchange in patients undergoing descemet stripping automated endothelial keratoplasty. Cornea 2015;34(9):1030-1034.
19 Shpitzer SA, Rosenblatt A, Bahar I. Outcomes of descemet stripping automated endothelial keratoplasty in patients with an anterior chamber versus posterior chamber intraocular lens. Cornea 2014;33(7):686-690.
20 Ang M, Li L, Chua D, Wong C, Htoon HM, Mehta JS, Tan D.Descemet’s stripping automated endothelial keratoplasty with anterior chamber intraocular lenses: complications and 3-year outcomes. Br J Ophthalmol 2014;98(8):1028-1032.
21 Gupta PK, Bordelon A, Vroman DT, Afshari NA, Kim T. Early outcomes of descemet stripping automated endothelial keratoplasty in pseudophakic eyes with anterior chamber intraocular lenses Am J Ophthalmol 2011;151(1):24-28.
22 Khor WB, Mehta JS, Tan DT. Descemet stripping automated endothelial keratoplasty with a graft insertion device: surgical technique and early clinical results. Am J Ophthalmol 2011;151(2):223-232.
23 Shah AK, Terry MA, Shamie N, Chen ES, Phillips PM, Hoar KL,Friend DJ, Davis-Boozer D. Complications and clinical outcomes of descemet stripping automated endothelial keratoplasty with intraocular lens exchange. Am J Ophthalmol 2010;149(3):390-397.
24 Elbaz U, Yeung SN, Lichtinger A, Zauberman NA, Goldich Y, Ziai S,Chan CC, Rootman DS, Slomovic AR. EndoGlide versus EndoSerter for the insertion of donor graft in descemet stripping automated endothelial keratoplasty. Am J Ophthalmol 2014;158(2):257-262.
25 Peng RM, Hao YS, Chen HJ, Sun YX, Hong J. Endothelial keratoplasty:the use of viscoelastic as an aid in reattaching the dislocated graft in abnormally structured eyes. Ophthalmology 2009;116(10):1897-1900.
26 Bruynseels A, Sii F, Masood I, Shah P. Severe intraocular pressure elevation after intracameral healon 5 viscoelastic support for post-operative hypotony after XEN Gel stent insertion. J Glaucoma 2018.
27 Holzer MP, Tetz MR, Auffarth GU, Welt R, Völcker HE. Effect of Healon5 and 4 other viscoelastic substances on intraocular pressure and endothelium after cataract surgery. J Cataract Refract Surg 2001;27(2):213-218.
28 Gonnermann J, Torun N, Klamann MK, Maier AK, von Sonnleithner C, Rieck PW, Bertelmann E. Posterior iris-claw aphakic intraocular lens implantation in children. Am J Ophthalmol 2013;156(2):382-386.
29 Gonnermann J, Klamann MK, Maier AK, Rjasanow J, Joussen AM,Bertelmann E, Rieck PW, Torun N. Visual outcome and complications after posterior iris-claw aphakic intraocular lens implantation. J Cataract Refract Surg 2012;38(12):2139-2143.
30 Rauen M, Russell SR, Tauber S, Goins KM. Surgical management of a posterior dislocated intraocular lens after descemet stripping automated endothelial keratoplasty. Cornea 2010;29(3):350-353.
31 Fouda SM, Al Aswad MA, Ibrahim BM, Bori A, Mattout HK.Retropupillary iris-claw intraocular lens for the surgical correction of aphakia in cases with microspherophakia. Indian J Ophthalmol 2016;64(12):884-887.
32 Forlini M, Soliman W, Bratu A, Rossini P, Cavallini GM, Forlini C. Long-term follow-up of retropupillary iris-claw intraocular lens implantation: a retrospective analysis. BMC Ophthalmol 2015;15:143.
33 Terry MA, Shamie N, Chen ES, Phillips PM, Shah AK, Hoar KL,Friend DJ. Endothelial keratoplasty for Fuchs’ dystrophy with cataract:complications and clinical results with the new triple procedure Ophthalmology 2009;116(4):631-639.
34 Quek DT, Wong T, Tan D, Mehta JS. Corneal graft survival and intraocular pressure control after descemet stripping automated endothelial keratoplasty in eyes with pre-existing glaucoma. Am J Ophthalmol 2011;152(1):48-54.