INTRODUCTION
Residual refractive errors after cataract surgery might have different origins. The principal cause is attributable to intraocular lens (IOL) calculation error due to incorrect corneal power determination, keratometry errors, incorrect axial length determination, small pupil diameter[1-2]. The other reported causes are post-surgical astigmatism and wrong IOL implantation[3]. Low ametropias could be easily resolved by an optical correction, but in high refractive errors or anisometropia as well as in patients refusing glasses or contact lens, other solutions should be adopted. Different techniques such as IOL exchange, piggyback IOL implantation or excimer laser procedures were reported and importance of proper management of this complication was highlighted[4-7].
In this study, we have evaluated the efficacy and safety of photorefractive keratectomy (PRK) for residual ametropia following cataract surgery with IOL implantation, addressing particular attention to the causes of such refractive errors. The Institutional Review Board approval was obtained to perform this study.
SUBJECTS AND METHODS
In this retrospective clinical study, 24 eyes of 24 patientsaffected by residual refractive error after cataract extraction were examined. Fourteen were females, ten were males, and their age ranged from 38 to 79 (52.7±11.49)y. Twenty-two patients had a history of phacoemulsification, and two were subjected to extra-capsular cataract extraction and all patients had IOL implantation. The time interval between PRK and cataract surgery ranged from 1 to 4y. Informed consent was obtained from all individual participants included in the study.Detailed examination of preoperative medical records and the ocular characteristics of all patients before the cataract surgery was done in order to determine the cause of residual refractive errors.
Table 1 Data of patients subjected to laser refractive surgery for residual ametropia following cataract extraction with IOL implantation
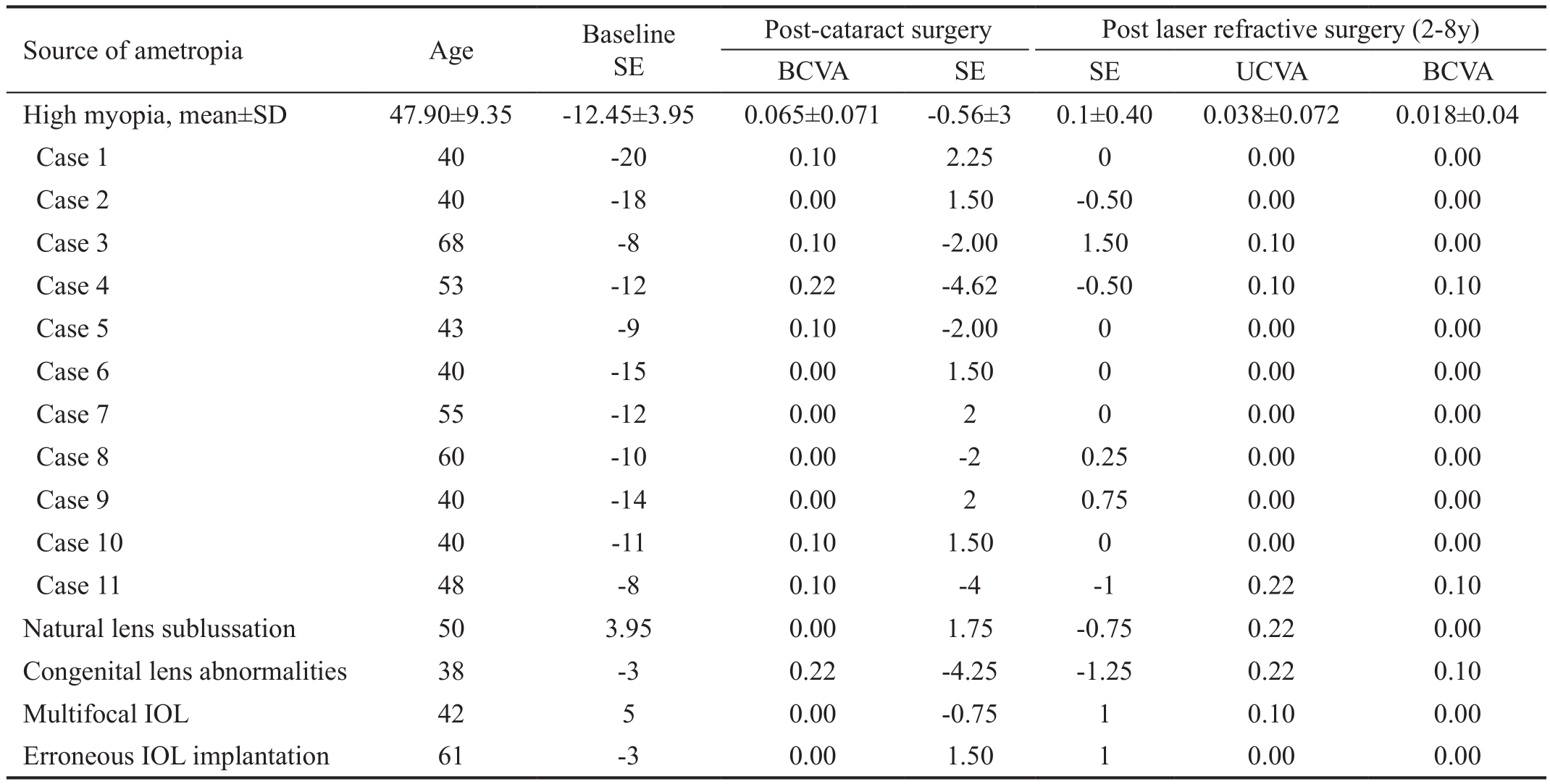
BCVA: Best corrected visual acuity; SE: Spherical equivalent; UCVA: Uncorrected visual acuity; IOL: Intraocular lens; SD: Standard deviation.
All selected participants were submitted to complete ophthalmologic examination, with corneal topography,pachymetry and tear function evaluation. PRK was performed in all eyes with Mel 70 G-Scan excimer laser (Carl Zeiss, Jena,Germany). Anesthetic drops were instilled before the treatment,and epithelium was removed with alcohol delamination (25%for 20s). After the treatment, a soft contact lens was applied and topical therapy was prescribed with antibiotics, steroids and artificial tears (hyaluronate) until epithelium healed.Than the contact lens was removed and therapy changed to steroid drops (fluorometholone 0.2%) for 30d. The mean outcome measures were UCVA, BCVA, refraction and corneal transparency. Follow up ranged from 1 to 8y.
RESULTS
The main origin of postoperative ametropia among our patients was erroneous IOL calculation in abnormal eyes (high myopia,congenital lens abnormalities) and corneal astigmatism both suture induced and preexisting. Eleven eyes presented residual refractive error resulted from inexact IOL calculation in high myopia, and in nine cases from high preoperative or postoperative astigmatism. Postsurgical astigmatism was differentiated in suture induced astigmatism (extracapsular cataract extraction, scleral fixation) or persistence of the high corneal astigmatism already existing before the surgery.Astigmatism induced by suture in extra-capsular extraction and IOL implantation was presented in two eyes. Instead,astigmatism already existing before the surgery occurred in seven eyes. Data were shown in Tables 1, 2. At baseline (before cataract surgery) the mean SE was -12.45±3.95 D ranging from-20 to -8 D in high myopic eyes, and it was 0.86±4.27 D ranging from -4 to +7 D in the astigmatic eyes, with mean cylinder ranging from -8 to +6 D (-2.94±4.86 D).
After cataract surgery and before the laser enhancement the mean SE was -0.56±3 D ranging from -4.62 to +2.25 D in high myopic patients, instead it was -1±1.73 D ranging from-3.25 to +3.75 D in the astigmatic eyes, with a mean cylinder of -3.75±0 ranging from -3 to +5.50 D. After laser refractive surgery the mean SE was 0.1±0.73 D, ranging from -0.50 to+1.50 D in the myopic group, and it was -0.50±0.57 D ranging from -1.25 to +0.50 D in astigmatic patients, with a mean cylinder of -0.25±0.75 D. The visual acuity was expressed in logMAR scale. In myopic patients the mean UCVA and BCVA were 0.038±0.072 and 0.018±0.04 respectively, both ranging from 0.10 to 0.00. In astigmatic patients, the mean UCVA and BCVA were 0.213±0.132 and 0.00±0.0 respectively, UCVA ranging from 0.50 to 0.22 and BCVA was 0.00. All patientspresented normal corneal transparency. No ocular hypertension was detected.
Table 2 Data of patients subjected to laser refractive surgery for residual astigmatic ametropia following cataract extraction with IOL implantation
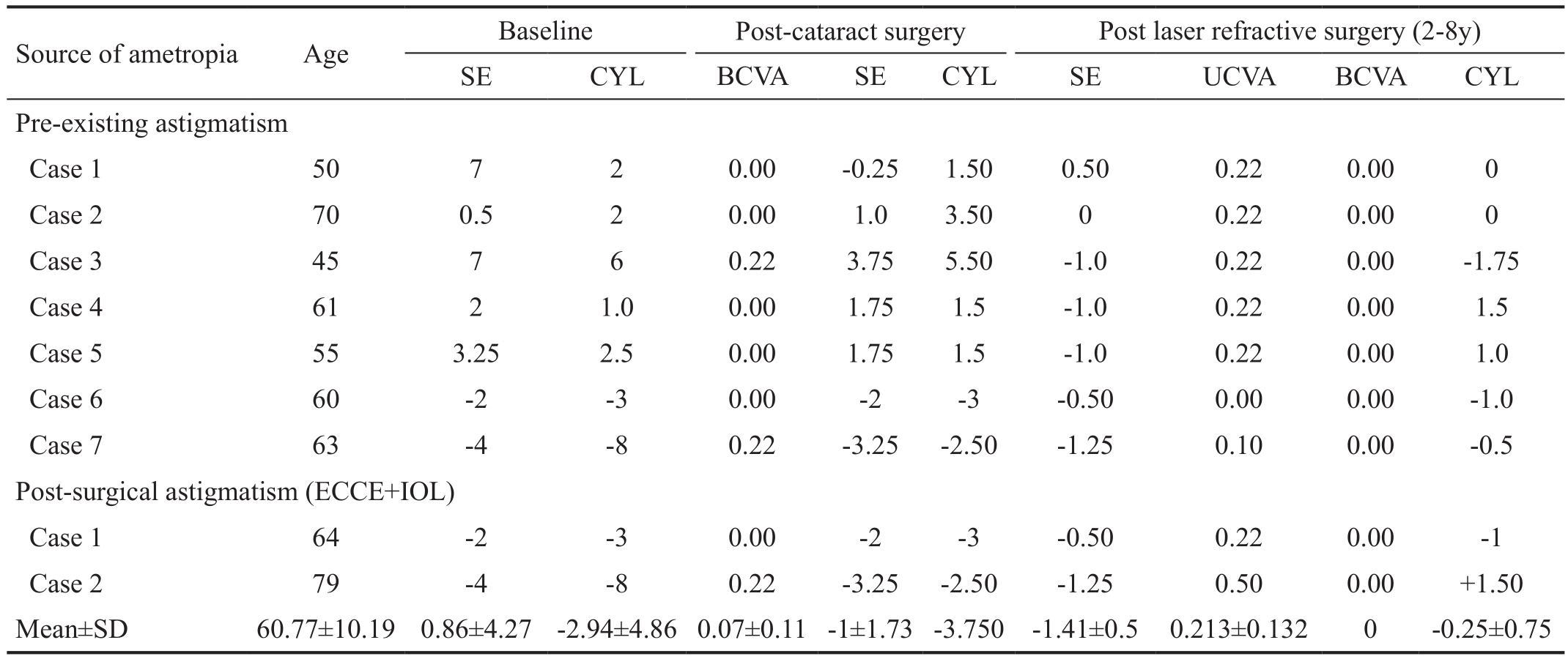
BCVA: Best corrected visual acuity; SE: Spherical equivalent; UCVA: Uncorrected visual acuity; ECCE: Extracapsular cataract extraction;IOL: Intraocular lens; SD: Standard deviation; CYL: Cylinder.
DISCUSSION
Residual refractive errors in patients who undergo cataract surgery with IOL implantation might still occur, nevertheless modern technological approach to calculate the lens power.The most frequently reported cause is due to erroneous power of the implanted IOL and may result from a wrong calculation or inexact lens used[8-9]. In the present study, the principle origin of postoperative ametropia among examined patients was erroneous IOL calculation. Currently two different systems of the lens power calculation are used worldwide, the ultrasound and the optical, that became recently the most used and highly recommended because of its known accuracy and precision.However, it is affected by corneal and lens transparency and in white or total cataract, the ultrasound system is still adopted.Such technique appears less accurate above all in abnormal eyes, especially with high myopia, were the increased axial length and frequent presence of staphyloma, become a source of possible biometric errors[10-11]. IOL calculation might result also difficult in eyes with congenital abnormalities of the lens or in patients with lens subluxation representing the other sources of possible biometric errors. It is more probable to detect a post-cataract refractive error in abnormal eyes, with uncommon antero-posterior length but a minimal residual myopia in patients with premium lens can result in undesirable clinical outcome. As to multifocal IOLs, the perfect emetropia is required to obtain predicted result. Residual low myopia affects the final visual outcome. In fact, even a low residual refractive error can cause high visual discomfort, as succeed in one of our patients. In the examined patients, the IOL calculation was performed using ultrasound biometry, used in our clinic at time. We have considered the not common eyes characteristics so the IOL error was expected and all patients were properly informed as to possible unpredictable results.Corneal astigmatism was the second cause of refractive error in our patients. In one eye, it was related to the corneal suture management and in two eyes it was already present before the cataract surgery. The prevalence and management of residual refractive errors after cataract surgery with IOL implantation have been widely studied.
Sáles et al[12]reviewed available literature regarding different approaches to manage the post-cataract refractive errors such as corneal excimer laser procedures (LASIK or PRK), arcuate keratotomy and intraocular approaches, such as IOL exchange,piggyback IOLs and light-adjustable IOLs. He concluded that laser vision correction yields more effective and predictable outcomes than intraocular surgery, avoiding potential risks of intraocular surgery. Accordingly to the literature the lightadjustable IOL may provide the ideal treatment of ametropia in the pseudophakic eyes by preventing secondary invasive procedures, but its use is limited and it lacks sufficient scientific studies[13-15]. Different authors studied the outcomes of post cataract excimer laser refractive surgery[16]. Fernández-Buenaga et al[17]conduced a retrospective study comprehending patients with an unacceptable final refractive error after phacoemulsification. They compared intraocular approach with IOL exchange and piggyback lens and LASIK. Although all of the three procedures were effective, the LASIK showed the best outcome in terms of efficacy and predictability[17-18].Jin et al[19]compared LASIK to lens-based surgery on 28 eyes for correcting residual refractive error after cataract surgery and stated that both procedures could be considered as safe,effective and predictable procedures. Currently available literature reviewed by Alio et al[20]suggest that laser vision correction gives up more effective and predictable outcomes than intraocular surgery. Theoretically piggyback IOLs and IOL exchange may be superior to surface treatments, but even if standardized and considered as safe, the intraocular procedures present potential risks of severe complications like capsular rupture or endophtalmitis. Consequently, the excimer laser ablation is preferred to avoid dramatic complications as it results in good refractive and clinical outcome as confirmed by the present study. It can be concluded that PRK can be considered as a safe and effective procedure for correction of post cataract residual refractive errors providing the patients with their attempted visual acuity. Moreover, it results stable in the long term, yielding more effective and predictable outcome than intraocular surgery.
ACKNOWLEDGEMENTS
Conflicts of Interest:Roszkowska AM, None; Urso M,None; Signorino GA, None; Spadea L, None; Aragona P,None.
REFERENCES
1 Norrby S. Sources of error in intraocular lens power calculation. J Cataract Refract Surg 2008;34(3):368-376.
2 Preussner PR. Accuracy limits in IOL calculation: current status. Klin Monbl Augenheilkd 2007;224(12):893-899.
3 Jin GJ, Crandall AS, Jones JJ. Intraocular lens exchange due to incorrect lens power. Ophthalmology 2007;114(3):417-424.
4 Falzon K, Stewart OG. Correction of undesirable pseudophakic refractive error with the Sulco flex intraocular lens. J Refract Surg 2012;28(9):614-619.
5 Huerva V. Piggyback multifocal IOLs for a hyperopic-presbyopic surprise after cataract surgery in high myopic patients. Cont Lens Anterior Eye 2014;37(1):57-59.
6 Narang P, Steinert R, Little B, Agarwal A. Intraocular lens scaffold to facilitate intraocular lens exchange. J Cataract Refract Surg 2014;40(9):1403-1407.
7 El Awady HE, Ghanem AA. Secondary piggyback implantation versus IOL exchange for symptomatic pseudophakic residual ametropia. Graefes Arch Clin Exp Ophthalmol 2013;251(7):1861-1866.
8 Abdelghany AA, Alio JL. Surgical options for correction of refractive error following cataract surgery. Eye Vis (Lond) 2014;1(2).
9 Behndig A, Montan P, Stenevi U, Kugelberg M, Zetterström C,Lundström M. Aiming for emmetropia after cataract surgery: Swedish National Cataract Register Study. J Cataract Refract Surg 2012;38(7):1181-1186.
10 Roy A, Das S, Sahu SK, Rath S. Ultrasound biometry vs IOL Master.Ophalmology 2012;119(9):1937-1931.
11 Devgan U. Cataract surgery in myopic eyes requires extra attention.Ocular Surgery News 2010.
12 Sáles CS, Manche EE. Managing residual refractive error after cataract surgery. J Cataract Refract Surg 2015;41(6):1289-1299.
13 Hengerer FH, Hütz WW, Dick HB, Conrad-Hengerer I. Combined correction of sphere and astigmatism using the light-adjustable intraocular lens in eyes with axial myopia. J Cataract Refract Surg 2011;37(2):317-323.
14 Villegas EA, Alcon E, Rubio E, Marín JM, Artal P. Refractive accuracy with light-adjustable intraocular lenses. J Cataract Refract Surg 2014;40(7):1075-1084.
15 Rocha G, Mednick ZD. Light-adjustable intraocular lens in post-LASIK and post-traumatic cataract patient. J Cataract Refract Surg 2012;38(6):1101-1104.
16 Hengerer FH. Current state of the "light-adjustable lens". Klin Monbl Augenheilkd 2012;229(8):784-793.
17 Fernández-Buenaga R, Alió JL, Pérez Ardoy AL, Quesada AL, Pinilla-Cortés L, Barraquer RI. Resolving refractive error after cataract surgery: IOL exchange, piggyback lens, or LASIK. J Refract Surg 2013;29(10):676-683.
18 Alio JL, Abdelghany AA, Fernández-Buenaga R. Management of residual refractive error after cataract surgery. Curr Opin Ophthalmol 2014;25(4):291-297.
19 Jin GJ, Merkley KH, Crandall AS, Jones YJ. Laser in situ keratomileusis versus lens-based surgery for correcting residual refractive error after cataract surgery. J Cataract Refract Surg 2008;34(4):562-569.
20 Alio JL, Abdelghany AA, Fernández-Buenaga R. Management of residual refractive error after cataract surgery. Curr Opin Ophthalmol 2014;25(4):291-297.