INTRODUCTION
Glaucoma is a leading cause of blindness disease and is characterized by elevated intraocular pressure (IOP),optic nerve damage and visual defects[1]. Some types of glaucoma include neovascular glaucoma, secondary glaucoma associated with uveitis, and angle recession, which usually are bad responsive to conventional medical therapies and surgical procedures[2-3]. Uveitis is swelling and irritation of the uvea which is the middle layer of the eye. It accounts for 5%-20%of blindness cases in the United States and Europe[4]. One of the major complications is glaucoma which arises secondary to uveitis or the corticosteroids used to treat uveitis[1,5-6]. Uveitic glaucoma is difficult to manage because it may be difficult to obtain a desirable IOP through medical treatments and surgeries.There are many therapies used to treat of uveitic glaucoma.One of the most common procedures used is trabeculectomy.The major complication of this procedure is bleb fibrosis[7-8].Although the application of anti-fibrotic agents such as mitomycin C, have been used in surgery, the success rate of filtration surgery remains unsatisfactory[9]. Furthermore, as the recurrent inflammatory response of uveitis transpires in these patients, filtration surgery in uveitic glaucoma yields lower success rates than other refractory glaucoma[10].
In recent years, aqueous drainage devices have been widely used to treat uveitic glaucoma. The Ahmed glaucoma valve(AGV) is a shunt device used to restrict flow in uveitic glaucoma[11-12]. It has shown better surgical results with fewer postoperative complications compared with traditional surgical procedures in uveitic glaucoma[12]. The success rates of AGV implantation are higher in some studies compared with trabeculectomy[12-14]. However, success rates are inconsistent among different studies. Moreover, there is little report of success rates of AGV in Chinese uveitic glaucoma. Herein, we present the outcomes of patients with uveitic glaucoma who were treated with AGV implantation.
SUBJECTS AND METHODS
Study Population This was a retrospective and non-comparative study of AGV implantation. We reviewed the records of all uveitic glaucoma patients who underwent AGV implant surgery at the Department of Ophthalmology, the Second Affiliated Hospital of Anhui Medical University from Jun.2009 to Apr. 2012 due to glaucoma that was uncontrolled by medical treatment or with glaucoma surgery. This study contained 67 eyes of 56 patients with uveitic glaucoma.Clinical information including age, gender, race, number of anti-glaucoma medications, previous glaucoma surgeries were collected. As active uveitis may influence the outcome of surgery, the patients in the study were clinically in remission for over 6mo and received oral prednisone 1 mg/kg·d and were tapered for 3wk[1,15]. All the patients underwent a full ophthalmic examination, including visual acuity (VA), IOP,slit-lamp examination of the anterior chamber, gonioscopy,central corneal thickness, measurement of IOP, fundus examination with special attention to optic disc parameters,retinal nerve fiber layer (RNFL), and visual field (VF).The study was approved by the Local Institutional Ethnics Committee of the Second Affiliated Hospital of Anhui Medical University and met the tenets of the Declaration of Helsinki.The participants provided their written consent to participate in this study.
Surgical Technique All AGV implant surgeries were performed under retrobulbar anesthesia by the same surgeon, with the use of a fornix-based conjunctival and Tenon’s capsule flap. The surgery involved a standard technique which was mentioned in the previous studies. Firstly, in order to expose a surgical field, the corneal traction suture was anchored at the peripheral cornea using 8-0 nylon. An AGV single-plate silicone implant (New World Medical Inc., Rancho Cucamonga,CA, USA) was used in all patients. Secondly, a conjunctiva and Tenon’s capsule incision of approximately 10 mm were made circumferentially at 5 mm posterior from the limbus in the supratemporal quadrant, and the sub-Tenon’s space was undermined. The implant was primed by the injection of saline solution through a 25-gauge blunt cannel. The body of the implant was secured onto the sclera at 8 to 10 mm posterior from the limbus with a 10-0 nylon suture. Paracentesis into the anterior chamber was made with a 23-gauge needle at 2 mm posterior to the limbus. A paracentesis was performed temporally for the injection of viscoelastic material. Next, a silicone tube was cut, and a length of approximately 2 mm was inserted into the anterior chamber through this needle track,which was secured to the sclera with three 10-0 nylon sutures.A full thickness donor scleral patch graft, 4 mm×3 mm in size,was attached over the tube near the limbus and secured. The conjunctiva was then closed with 10-0 nylon sutures.
Management After Surgery Follow-up of the patients after surgery included IOP, VF, Ahmed valve area changes and complication, uveitis control, additional glaucoma medications,other complications. When the IOP was above 21 mm Hg, the brinzolamide and carteolol hydrochloride eye drops were used.The tropicamide, tobramycin dexamethasone and pranoprofen eye drops were used in the uveitic glaucoma patients who had eye red, eye pain and VA decreased.
Statistical Analysis Comparisons between continuous outcomes were assessed using a one-way analysis of variance with the Dunnett multiple comparison test. Kaplan-Meier life-table analysis was used to assess cumulative probability of success. Comparisons between categorical factors were examined with the Chi-square or Fisher exact test. P values<0.05 were considered statistically significant.
RESULTS
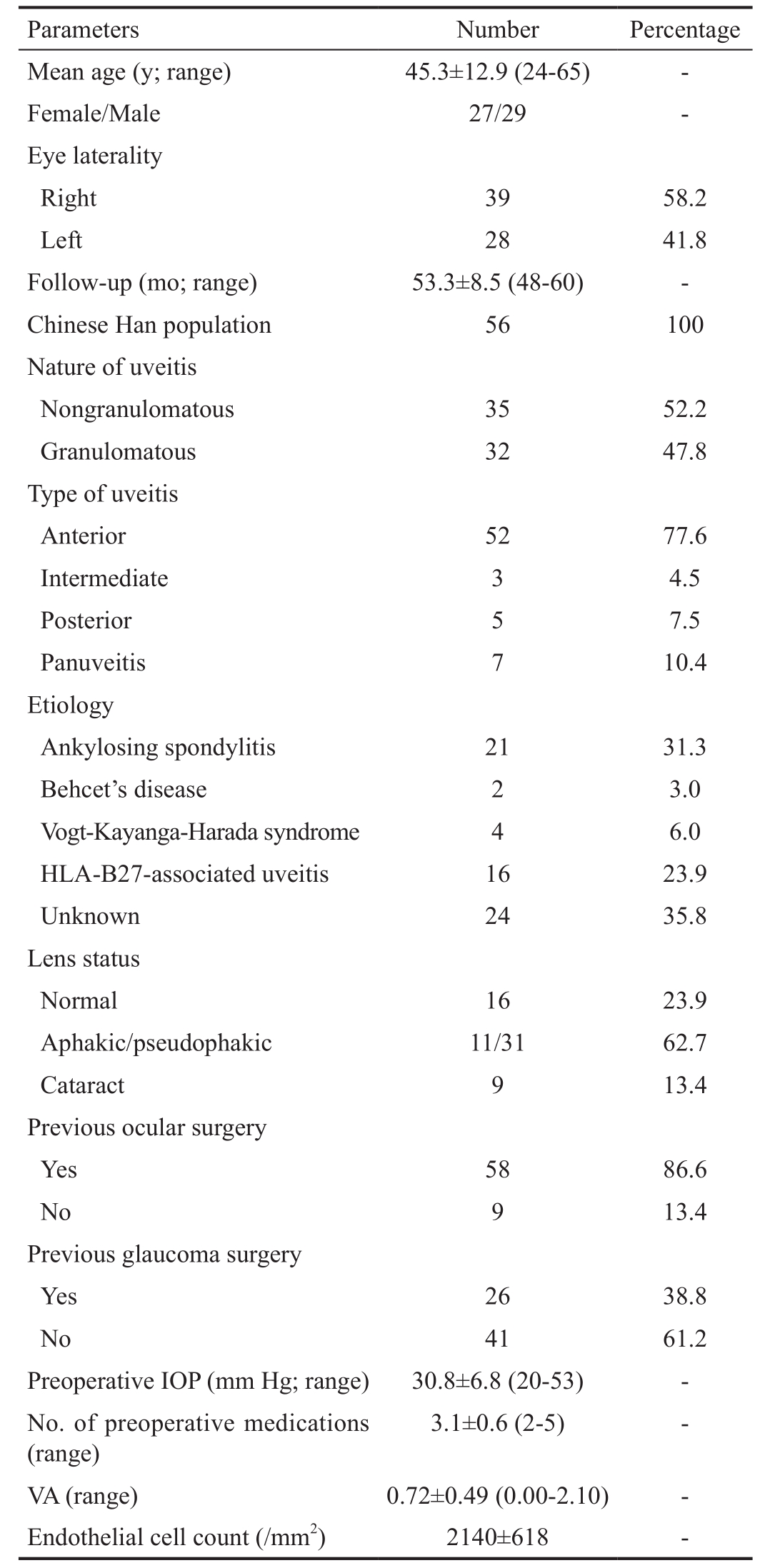
Patient Data Fifty-six patients (67 eyes) underwent AGV implantation for uveitic glaucoma. All the patients underwent surgery before Apr. 2012. The clinical characteristics including age, sex, follow-up period, diagnosis, laterality, previous surgeries, preoperative and last postoperative IOP, VA, number of medications used, and surgical history for each patient are summarized in Table 1. The average age at the time of surgery was 45.3±12.9 (range 24 to 65)y and mean follow-up time was 53.3±8.5 (range 48 to 60)mo. Totally 31 (46.3%) eyes were pseudophakic and 11 (16.4%) eyes were aphakic.
In the present study, anterior uveitis was the common case,which affected 52 (77.6%) eyes. The most of patients were concomitant with other diseases, 21 (31.3%) patients had ankylosing spondylitis and 16 (23.9%) patients were HLA-B27 positive. Surgical histories may influence the success rate of the AGV implantation. Of 58 (86.6%) of the 67 eyes had previous ocular surgeries and 26 (38.8%) had failed trabeculectomies with mitomycin C used in surgeries.
Surgical Success The qualified success rate was 98.5%,95.5%, 89.6%, 83.6%, 76.1%, 70.1%, 65.7% and 61.2% at 1, 3, 6, 12, 24, 36, 48 and 60mo by Kaplan-Meier survival analysis (Figure 1).
Intraocular Pressure Control The mean preoperative and postoperative IOPs are summarized in Table 2. The mean preoperative IOP was 30.8±6.8 mm Hg and postoperative IOPs were 9.9±4.1, 10.1±4.2, 10.9±3.7, 12.9±4.6, 13.8±3.9,13.2±4.6, 12.3±3.5 and 13.1±3.7 mm Hg at 1, 3, 6, 12, 24, 36,48 and 60mo after AGV implantation. There were significant differences between preoperative and postoperative IOP at all follow-up times (P<0.01).
Visual Acuity, Retinal Nerve Fiber Layer and Visual Field The VA was stable in most of the eyes. Before surgery,the mean logMAR VA at baseline was 0.72±0.49 and mean postoperative VA was 0.78±0.69 at 12mo, 0.69±0.56 at 24mo and 0.63±0.54 at 60mo after the AGV implantation. The meanpreoperative and postoperative VA were summarized in Table 2.The VF and RNFL were stable during the following time.
Table 1 Clinical characteristics of study patients
Number of Medications The number medications used was significantly decreased in postoperative glaucoma patients.Table 2 showed the number medications in patients before and after operation. The average number of glaucoma medications decreased from 3.1±0.6 medications at baseline to 0.5±0.3 at 1mo, 0.9±0.4 at 3mo, 0.9±0.2 at 6mo, 1.2±0.5 at 12mo,1.3±0.4 at 24mo, 1.1±0.3 at 36mo and 1.2±0.5 at 60mo.
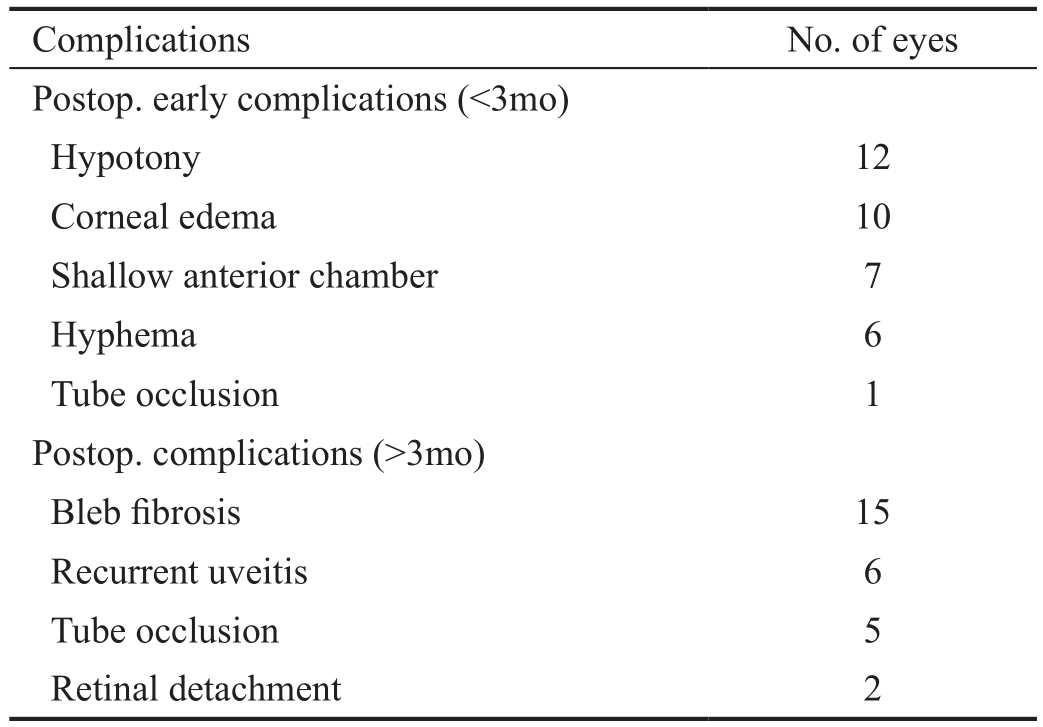
Additional Surgeries and Surgical Complications In the study, 14 of the 67 eyes underwent AGV implantation in combination with other intraocular surgery including phacoemulsification (n=9), pars plana vitrectomy (n=2),anterior vitrectomy (n=3). The major intraoperative complications of AGV implantation in this group was hyphema(3 of 67 eyes, 4.5%) and no other complications occurred during the surgery.
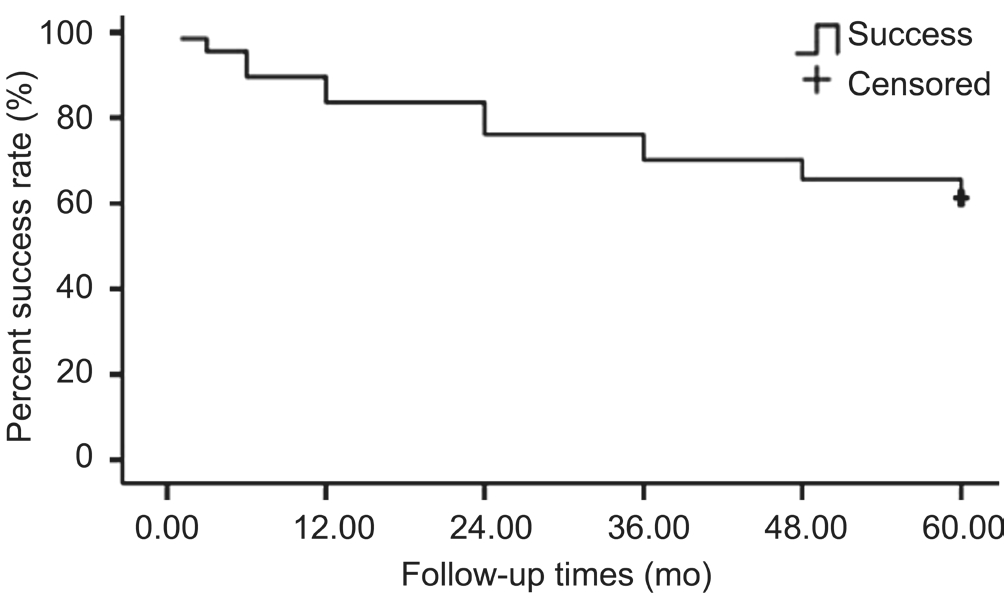
Figure 1 Cumulative probability of success of AGV implantation for uveitic glaucoma Success was defined as an IOP between 5 and 21 mm Hg, reduced by at least 20% from baseline with no additional glaucoma surgery. The curve was generated by means of the Kaplan-Meier life-table analysis.
There were some complications after the AGV implantation.In present study, on one hand, the most common early postoperative complication (<3mo) was transient hypotony which was defined as IOP<5 mm Hg and was observed in 12 eyes. Shallow anterior chambers were found in 7 eyes in the early postoperative period. Totally 6 eyes had moderate hyphema and the AGV tube of one eye was obstructed, 10 eyes had corneal edema. No other corneal complication and would leak were found in the patients. On the other hand, the postoperative complications (>3mo) were found in the study that included tube occlusion, bleb fibrosis, retinal detachment and recurrent uveitis. Totally 5 eyes had tube occlusion at 60mo, the bleb fibrosis was found in 15 eyes at 60mo after surgery, 6 eyes had recurrent uveitis (ankylosing spondylitis in 4 eyes, Vogt-Kayanga-Harada syndrome in 2 eyes) which caused the fail of AGV implantation in uveitic patients. Retinal detachment was found in 2 eyes at 12mo after surgery. The results were shown in Table 3.
DISCUSSION
Uveitis is a common cause of blindness and is characterized by recurrent intraocular inflammation of the eyes. The recurrent uveitis leads many in flamed cells to obstruct the trabeculum,and thus the aqueous humor is unable to flow through the trabeculum. These results led to many types of complications;glaucoma is one of them[1].
Uveitic glaucoma is difficult to manage because of its therapeutic challenges and the lifetime burden of vision loss if the disease is not treated[1,16]. Although glaucoma surgeries have a relatively low success rate in treating uveitic glaucoma,they are thought to be useful methods of controlling IOP.Various studies have reported that glaucoma drainage devicesare more effective methods of reducing IOP in uveitic glaucoma than other conventional treatments[17-19]. As a glaucoma drainage device, the AGV is a shunt device with a restriction flow mechanism that is used in uveitic glaucoma and the study revealed that the complication rate of AGV implants is lower than other kinds of valves[15,19].
Table 2 Changes in IOP, VA, and anti-glaucoma medication before and after AGV implantation
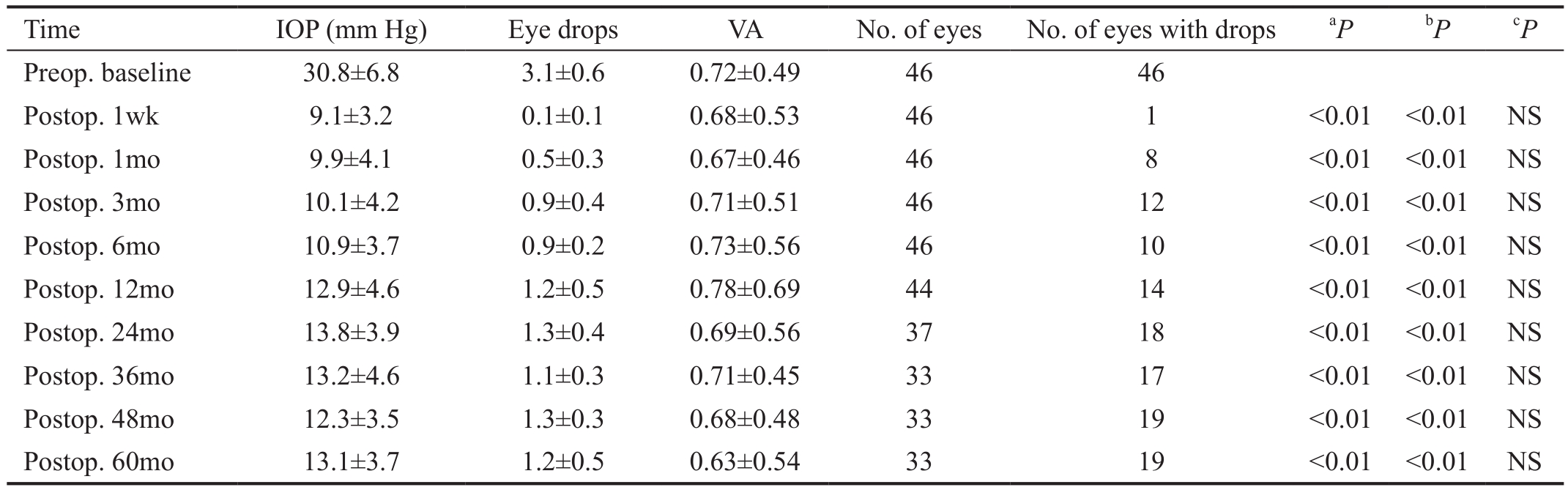
aIOP after operation vs baseline;bEye drops after operation vs baseline;cVA after operation vs baseline. NS: No significant difference.
Table 3 The complications after AGV implantation in the patient with uveitic glaucoma
The success rate of AGV implantation is very important to evaluate the effect of AGV implantation. In past years, the success rates of AGV varied in uveitic glaucoma patients among different populations[12,14,17,19]. The success rates of this study were 83.6% at 12mo after surgery, 70.1% at 36mo after surgery, and 61.2% at 60mo after surgery. The success rates of drainage implantation in uveitic glaucoma were different in these studies. On one hand, the success rates of some studies about uveitic glaucoma were higher than that of this study.Satana et al[17]reported that AGV implantation in the 14 eyes of 10 patients with uveitic glaucoma secondary to Behcet’s disease and success rates (i.e. IOP between 6 and 21 mm Hg)of 90.9% after 18mo and 72.7% after 24mo. The recent study reported that AGV implantation in 24 eyes with uveitic glaucoma had a success rate of 100% at 12mo after surgery[12].On the other hand, a few studies had lower success rate when compared with our study. A retrospective study of 60 eyes of 60 uveitic glaucoma patients who underwent AGV implantation revealed that success rates (IOP range 5 to 21 mm Hg and a 25.0% decrease in IOP from before surgery) of 77.0% after 1y surgery and 50.0% after 4y surgery[20]. The results were different among them because the definitions used to define success varied and the severity of uveitic glaucoma was diverse. Firstly, the definition of success in this study combined both the IOP between 5 and 21 mm Hg and a 20.0% decrease in IOP from that before surgery. This definition is stricter than that of higher success rate studies. Secondly, the conditions of patients in our study were extremely diverse that 86.6%patients had undergone previous ocular surgery and 38.8% had prior glaucoma surgery. These two reasons may explain the differing success rates between the AGV implantation studies.In order to improve the success rate of AGV surgery, we made sure that the patients were not in a period of active uveitis and that they received prednisone treatment before and after surgery[1,21-22]. The postoperative VA was similar to preoperative VA. The VF and RNFL were stable after the surgery. The IOP and number of anti-glaucoma medications were significantly decreased in postoperative patients. These results suggested that AGV implantation was effective in controlling IOP and reducing medication use without VA, VF and RNFL loss.
Like many other studies concerning AGV implantation,this study had many complications. There were several postoperative complications (<3mo) in the present study. In previous studies, the transient hypotony, hyphema, leaking,and corneal complications were common in the early periods after surgery[23-24]. Transient hypotony, hyphema and shallow anterior chambers were usually happened in during operation and the early postoperative period. The results were explained by the lower ocular pressure and pancreatic the 25-gauge blunt cannel during the surgery. The incidences of transient hypotony and shallow anterior chambers may be reduced through injections of viscoelastic materials into the anterior chamber at the end of AGV surgery. The AGV tube was blocked by hyphema in 1 eye, which caused high pressure.Totally 10 eyes had corneal edema with no other corneal complications. This finding was not consistent with the results by others[17,25]. Some studies reported corneal complications as the most common and serious in their studies because some patients had corneal grafts. However, no patient in our study had corneal implantations and this may be an important reason for low corneal complications.
The postoperative complications (>3mo) may have influenced the success rate. Tube occlusion and blebfibrosis were major factors which led to shunt failure of AGV implantation[7]. The bleb fibrosis was resulted in 15 patients having shunt failure after 5y surgery. The postoperative fibrotic capsule that forms around the AGV was the primary resistance to aqueous out flow and was considered as a crucial risk factor for failure of AGV surgery[4,26]. Many studies revealed that antifibrotic agent was a detriment to trabeculectomy survival[12,27-28]. However,recent study showed that the use of mitomycin C was not related the success rate of AGV implantation[20]. Interestingly,mitomycin C-induced tissue damage was reported to induce a reactive fibrosis adjacent to the area around the AGV,which resists aqueous flow through the shunt[29]. Based on the above reasoning, we did not use mitomycin C during the surgeries for the patients with uveitis in the present. As the patients in present study were all Chinese and diagnosed with uveitic glaucoma, they were clinically in remission for over 6mo and received oral prednisone before the operation, the complications of the study were relative low.
The current study had the limitations of a retrospective design,a small size of patients and the relative short duration of followup. Collected data were limited to how corneal endothelial cells changed in study. These may limit the evaluation of the severity of uveitic glaucoma. Another limitation is that the patients who did not follow-up were not included. In conclusion, the present study revealed the outcomes of AGV implantation in Chinese uveitic glaucoma. Our results demonstrated that AGV implantation is effective and safe for patients with uveitic glaucoma. Corneal edema and hypotony were two common early postoperative complications. In addition, bleb fibrosis was another postoperative complication in AGV surgery in Chinese uveitic glaucoma.
ACKNOWLEDGEMENTS
Foundations:Supported by the Key Project of Anhui Provincial Excellent Young Talent Support Program (No.gxyqZD2017033);the Grant of Second Affiliated Hospital of Anhui Medical University (No.2014BKJ047); Spark Program of the Second Affiliated Hospital of Anhui Medical Univeristy (No.2015hhjh02).
Conflicts of Interest:Bao N, None; Jiang ZX, None; Coh P,None; Tao LM, None.
REFERENCES
1 Baneke AJ, Lim KS, Stanford M. The pathogenesis of raised intraocular pressure in uveitis. Curr Eye Res 2016;41(2):137-149.
2 Wiese C, Heiligenhaus A, Heinz C. Changes in inflammatory activity after glaucoma filtration surgery in children with chronic anterior uveitis.Ocul Immunol Inflamm 2016;24(4):397-401.
3 Eksioglu U, Yakin M, Sungur G, Satana B, Demirok G, Balta O,Ornek F. Short- to long-term results of Ahmed glaucoma valve in the management of elevated intraocular pressure in patients with pediatric uveitis. Can J Ophthalmol 2017;52(3):295-301.
4 Amoozgar B, Lin SC, Han Y, Kuo J. A role for antimetabolites in glaucoma tube surgery: current evidence and future directions. Curr Opin Ophthalmol 2016;27(2):164-169.
5 Wang L, Zhou JL, Yang N, Zhang GN, Lu JY, Xiao Y, Qiu HZ. Ectopic variceal bleeding from colonic stoma: two case reports. Medicine(Baltimore) 2015;94(2):e406.
6 Stewart KP, Tawakol JB, Khan T, Capriotti JA. Combination immunotherapy in the treatment of chronic bilateral panuveitis and uveitic glaucoma during acute dengue fever infection in the Caribbean. Int Med Case Rep J 2015;8(9):151-153.
7 Schoenberg ED, Blake DA, Swann FB, Parlin AW, Zurakowski D,Margo CE, Ponnusamy T, John VT, Ayyala RS. Effect of two novel sustained-release drug delivery systems on bleb fibrosis: an in vivo glaucoma drainage device study in a rabbit model. Transl Vis Sci Technol 2015;4(3):4.
8 Medeiros Pinto J, Pinto Ferreira N, Abegao Pinto L. Ahmed valve upstream obstruction caused by fibrous ingrowth: surgical approach. J Glaucoma 2017;26(1):e236-e238.
9 Yazdani S, Mahboobipour H, Pakravan M, Doozandeh A, Ghahari E. Adjunctive mitomycin C or amniotic membrane transplantation for Ahmed glaucoma valve implantation: a randomized clinical trial. J Glaucoma 2016;25(5):415-421.
10 Kalinina Ayuso V, Scheerlinck LM, de Boer JH. The effect of an Ahmed glaucoma valve implant on corneal endothelial cell density in children with glaucoma secondary to uveitis. Am J Ophthalmol 2013;155(3):530-535.
11 Lee N, Ma KT, Bae HW, Hong S, Seong GJ, Hong YJ, Kim CY.Surgical results of trabeculectomy and Ahmed valve implantation following a previous failed trabeculectomy in primary congenital glaucoma patients. Korean J Ophthalmol 2015;29(2):109-114.
12 Bettis DI, Morshedi RG, Chaya C, Goldsmith J, Crandall A, Zabriskie N. Trabeculectomy with mitomycin C or Ahmed valve implantation in eyes with uveitic glaucoma. J Glaucoma 2015;24(8):591-599.
13 Dave P, Senthil S, Choudhari N, Sekhar GC. Outcomes of Ahmed valve implant following a failed initial trabeculotomy and trabeculectomy in refractory primary congenital glaucoma. Middle East Afr J Ophthalmol 2015;22(1):64-68.
14 Yakin M, Eksioglu U, Sungur G, Satana B, Demirok G, Ornek F.Short-term to long-term results of Ahmed glaucoma valve implantation for uveitic glaucoma secondary to Behcet disease. J Glaucoma 2017;26(1):20-26.
15 Sungur G, Yakin M, Eksioglu U, Satana B, Ornek F. Assessment of conditions affecting surgical success of Ahmed glaucoma valve implants in glaucoma secondary to different uveitis etiologies in adults. Eye (Lond)2017;31(10):1435-1442.
16 Sung VC, Barton K. Management of in flammatory glaucomas. Curr Opin Ophthalmol 2004;15(2):136-140.
17 Satana B, Yalvac IS, Sungur G, Eksioglu U, Basarir B, Altan C, Duman S. Ahmed glaucoma valve implantation for uveitic glaucoma secondary to Behcet disease. J Glaucoma 2015;24(8):607-612.
18 Chen A, Yu F, Law SK, Giaconi JA, Coleman AL, Caprioli J. Valved glaucoma drainage devices in pediatric glaucoma: retrospective long-term outcomes. JAMA Ophthalmol 2015;133(9):1030-1035.
19 Parihar JKS, Kaushik J, Jain VK, Trehan HS, Mishra A, Baranwal VK. Combined Ahmed valve and phacoemulsification with intraocular lens implantation under infliximab in refractory uveitic glaucoma. Eur J Ophthalmol 2017;11:0.
20 Costa VP, Azuara-Blanco A, Netland PA, Lesk MR, Arcieri ES. efficacy and safety of adjunctive mitomycin C during Ahmed glaucoma valve implantation: a prospective randomized clinical trial. Ophthalmology 2004;111(6):1071-1076.
21 Riva I, Roberti G, Katsanos A, Oddone F, Quaranta L. A review of the Ahmed glaucoma valve implant and comparison with other surgical operations. Adv Therapy 2017;34(4):834-847.
22 Riva I, Roberti G, Oddone F, Konstas AG, Quaranta L. Ahmed glaucoma valve implant: surgical technique and complications. Clin Ophthalmol 2017;11:357-367.
23 Zhou M, Xu X, Zhang X, Sun X. Clinical outcomes of Ahmed glaucoma valve implantation with or without intravitreal bevacizumab pretreatment for neovascular glaucoma: a systematic review and metaanalysis. J Glaucoma 2016;25(7):551-557.
24 Gdih G, Jiang K. Graft-free Ahmed valve implantation through a 6 mm scleral tunnel. Can J Ophthalmol 2017;52(1):85-91.
25 Papadaki TG, Zacharopoulos IP, Pasquale LR, Christen WB, Netland PA, Foster CS. Long-term results of Ahmed glaucoma valve implantation for uveitic glaucoma. Am J Ophthalmol 2007;144(1):62-69.
26 Amoozgar B, Wei X, Hui Lee J, Bloomer M, Zhao Z, Coh P, He F,Luan L, Xie C, Han Y. A novel flexible micro fluidic meshwork to reduce fibrosis in glaucoma surgery. PLoS One 2017;12(3):e0172556.
27 Quaranta L, Floriani I, Hollander L, Poli D, Katsanos A,Konstas AG. Needle revision with 5-fluorouracil for the treatment of Ahmed glaucoma valve filtering blebs: 5-fluoruracil needling revision can be a useful and safe tool in the management of failing Ahmed glaucoma valve filtering blebs. J Glaucoma 2016;25(4):e367-e371.
28 Quaranta L, Riva I, Floriani IC. Outcomes of using a sutureless bovine pericardial patch graft for Ahmed glaucoma valve implantation. Eur J Ophthalmol 2013;23(5):738-742.
29 Molteno AC, Sayawat N, Herbison P. Otago glaucoma surgery outcome study: long-term results of uveitis with secondary glaucoma drained by Molteno implants. Ophthalmology 2001;108(3):605-613.