INTRODUCTION
Glaucoma is a major public health problem. It is estimated that 64 million people around the world suffer from this disease[1]. Some studies show that its prevalence increases as intraocular pressure (IOP) levels increase[2-3]. Elevated IOP is the only treatable risk factor for glaucoma[4]. Ophthalmologists can lower IOP with medications, laser therapy, or incisional glaucoma surgery. One of the major problems with the medical treatment is the patient’s lack of compliance. The most frequent reasons for this are race, socioeconomic income and level of education[5-6].
Argon laser trabeculoplasty (ALT) was first described by Wise and Witter[7]and has been accepted as a treatment option for primary open angle glaucoma (POAG). The argon laser,wavelength (λ) =488-514 nm, improves the out flow of aqueous humor through the trabecular mesh work. However, histological studies have shown that this laser can lead to coagulative damage of this structure[8]. At present, ALT has been mostly replaced by selective laser trabeculoplasty (SLT) due to its ease of application and the possibility of repeat treatments.SLT uses a 532 nm Q-switched Nd:YAG laser that releases less energy and is selectively absorbed by the pigmented cells of the trabecular meshwork[9]. SLT results in terms of efficacy and safety are comparable to those of ALT[10-12].
In 2006, PASCAL pattern scan laser photocoagulator was introduced with a 532 nm laser used for standard photocoagulation procedures that can apply a uniform pattern of many laser spots at one time[13]. The PASCAL laser allows ophthalmologist to perform macular grid treatments effectively and panretinal photocoagulation more rapidly with less pain than conventional laser due to its short pulse duration and less thermal damage[14-15].
Recently, the patterned laser trabeculoplasty (PLT) has been described as a novel alternative used for the management of POAG. In this modality, PASCAL laser is used to generate a sub-visible treatment on trabecular meshwork. The device uses a sequence of 11.25° patterns that engages the angle and automatically rotates after each application in a 32-step series. Consequently, this avoids a treatment with significant gaps or overlaps[16]. Another advantage of this technology is the reduction of tissue damage since it uses a relatively short pulse duration (5ms). It has been shown that when using subthreshold powers, PLT produces less thermal damage on the trabecular meshwork than ALT[17].
Several studies have shown that PLT is just as effective and safe as ALT and SLT in treating IOP[18-19]. However, in these studies all patients underwent a medication washout period prior to treatment. The aim of this study was to assess the efficacy and safety of PLT as an adjunctive treatment in openangle glaucoma (OAG) or ocular hypertension (OHT) patients who were already using hypotensive drop treatment.
SUBJECTS AND METHODS
Subjects This study was a retrospective review of primary or secondary OAG patients and OHT patients who underwent PLT at Santander Ophthalmologic Foundation from June 2016 to August 2016. All patients provided written informed consent prior to inclusion in the study. The nature and possible consequences of the study were explained fully in accordance with the principles of the Declaration of Helsinki. This study was approved by the Santander Eye Foundation Research Ethics Committee.
Inclusion criteria were POAG, pigmentary glaucoma or OHT patients aged 18 years or older, with uncontrolled IOP(>18 mm Hg), using antiglaucoma medical treatment. Among the exclusion criteria were advanced visual field defects within 10° of fixation (1 point with sensitivity of 0 dB or 2 points with sensitivity less than 15 dB in the same hemifield) and/or mean deviation lower than -12 dB in a 24-2 SITA Standard Humphrey visual field (Heidelberg Engineering, Heidelberg,Germany); previous glaucoma surgery; presence of corneal disease that affected visualization of the trabecular meshwork;treatment with systemic steroids.
Examination The ophthalmological examination included Snellen best corrected visual acuity (BCVA) that was converted to the logarithm of the minimum angle of resolution (logMAR)BCVA for analysis, slit-lamp examination of the anterior segment and indirect gonioscopy with 4-mirror lens. IOP was determined by Goldmann applanation to nometer (GAT).Stereoscopic evaluation of the optic nerve was performed with a Volk (Volk Optical Inc., Mentor, Ohio, USA) lens of 78 D or 90 D.Patients were followed up at 1wk and 1, 3 and 6mo. At each follow-up visit IOP was measured by GAT (IOP measurements were averaged and used in data analysis) by the same observer.Biomicroscopy, BCVA, gonioscopy, funduscopy, and the presence of complications were registered.
Antiglaucoma medical therapy was continued after the laser treatment and was only modified if the IOP deteriorated significantly from its preoperative level or if there was a significant decrease in more than 2 consecutive controls(IOP<12 mm Hg). In the case of post-treatment IOP spikes(increase ≥10 mm Hg compared to the preoperative IOP),additional glaucoma treatment was started and an extra followup assessment visit was performed at one week.
Laser Treatment Procedure Indications for laser procedure were medically uncontrolled IOP and/or intolerance to medical IOP treatment. All the patients were treated using the PASCAL laser (Pascal Streamline 577; Topcon Inc., Tokyo, Japan) in a single 360° session by the same surgeon (Espinoza G). Patients were pre-treated with 1 drop of pilocarpine 2% in the eye to be treated 10min before PLT. Subsequently, 1 drop of topical anesthetic (proparacaine 0.5%) was used in both eyes of the patient.
The pattern parameters were set using a touch screen. PASCAL laser shots were focused onto the trabecular mesh work using a Latina gonioscopy contact lens (Ocular Instruments, Bellevue,WA, USA). Titration of the power to be used (starting with a pre-set power of 550 mW) was carried out by applying 10ms laser pulses until visible light blanching of trabecular mesh work in the inferior quadrant occurred. The exposure time was then reduced to 5ms to decrease the applied energy by half, producing sub-visible treatment spots. After titration the laser was set up to begin with the pattern in the inferior angle(12 o’clock). After each shot the pattern rotated automatically so it could engage with the trabecular meshwork avoiding overlapping shots. As the laser pattern was changing its angle the Latina gonioscopy lens was rotated. The treatment was administered in 32 steps to cover the 360° of trabecular meshwork. The total number of pulses and total amount of energy were recorded. Postoperatively, patients were prescribed prednisolone acetate 1% eye drops 4 times daily for 7d.
Statistical Analysis The mean IOP measured at each follow-up visit was compared with the pre-treatment level.In addition, percentage IOP reduction from baseline was assessed. Statistical analysis was done using the Stata 12.0 software (Stata Corp LLC, Texas, USA) and a P value <0.05 was considered to indicate statistical significance in all tests.The normal distribution of the data was evaluated by the Shapiro-Wilk test. Continuous data were presented in the form of mean±standard deviation. Absolute IOP and percentage IOP reduction from baseline (the IOP reduction rate) as well as the differences in the number of glaucoma medications were analysed statistically using t-test. PLT success was defined as IOP reduction by 20% or more of pretreatment IOP without additional medications, laser or surgery.
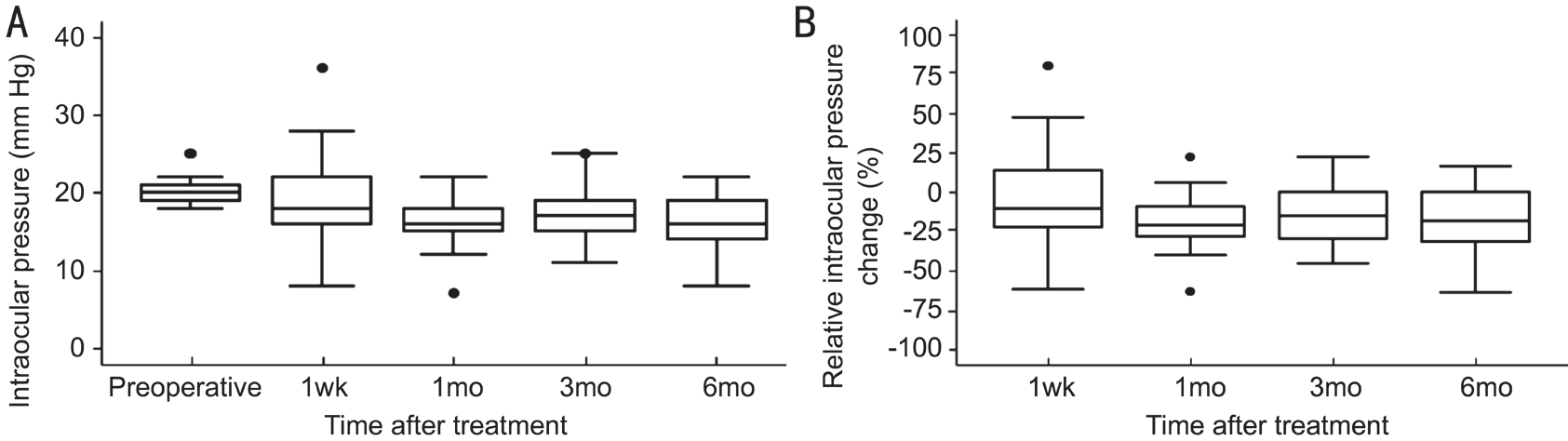
Figure 1 IOP follow-up during the first 6mo A: Average absolute pressure over time; B: Average relative changes in the IOP over time. Boxplots display the median as center line, 25thand 75thpercentiles as a box, and 5thand 95thpercentiles as whiskers.
RESULTS
Baseline Characteristics A total of 41 eyes of 25 patients(61% women and 39% men) were included in this study(53.7% left eyes). The mean age of the patients was 61.0±7.4y(range: 48-75y). The baseline characteristics of the patients are presented in Table 1.
Laser Treatment Outcomes In all cases, the PLT could be performed on the 360° of the trabecular meshwork in a single session. The mean power used for bleaching the trabecular meshwork with 10ms exposure time was 672.0±77.3 mW(range: 550-775 mW). The average of spots applied on the trabecular meshwork was 1044.7±206.3.
Intraocular Pressure Results The pre-treatment mean IOP was 20.2±1.6 mm Hg. As shown in Table 2, the IOP was 19.3±5.2, 16.1±2.7, 17.1±3.7 and 16.3±3.5 mm Hg, at 1wk, 1,3 and 6mo after PLT, respectively. IOP reduction from baseline was statistically significant from the first month, remaining stable at 6mo (P<0.001). Four (9.8%) out of the 41 treated eyes,maintained initial IOP values (first post-operative IOP) at 6mo.Average relative changes in the IOP over time are shown in Table 2 and Figure 1. PLT success rate at 6mo of follow-up was 48.78%.The mean number of glaucoma topical medications used was 2.2±1.2 before PLT and 2.1±1.1 at the final follow-up visit, which did not represent a statistically significant change (P=0.10)(Table 3).
Visual Acuity Outcomes The mean pre-treatment BCVA was 0.10±0.22 logMAR, and the mean post-treatment BCVA at the last follow-up visit was 0.11±0.21 logMAR. There were no statistically significant differences (P=0.37, t-test).
Complications Complications included transient spikes(9.8%) and peripheral anterior synechiae (PAS) (17.1%). There were no serious adverse events. The 4 cases that had an IOP increase were controlled with medical therapy consisting of brimonidine 0.20% and none of them required filtering surgery.Regarding the 7 eyes that developed PAS, none developed PAS greater than 90° of trabecular meshwork or greater than 2 clock hours (Figure 2).
Table 1 Baseline characteristics in patients who underwent patterned laser trabeculoplasty
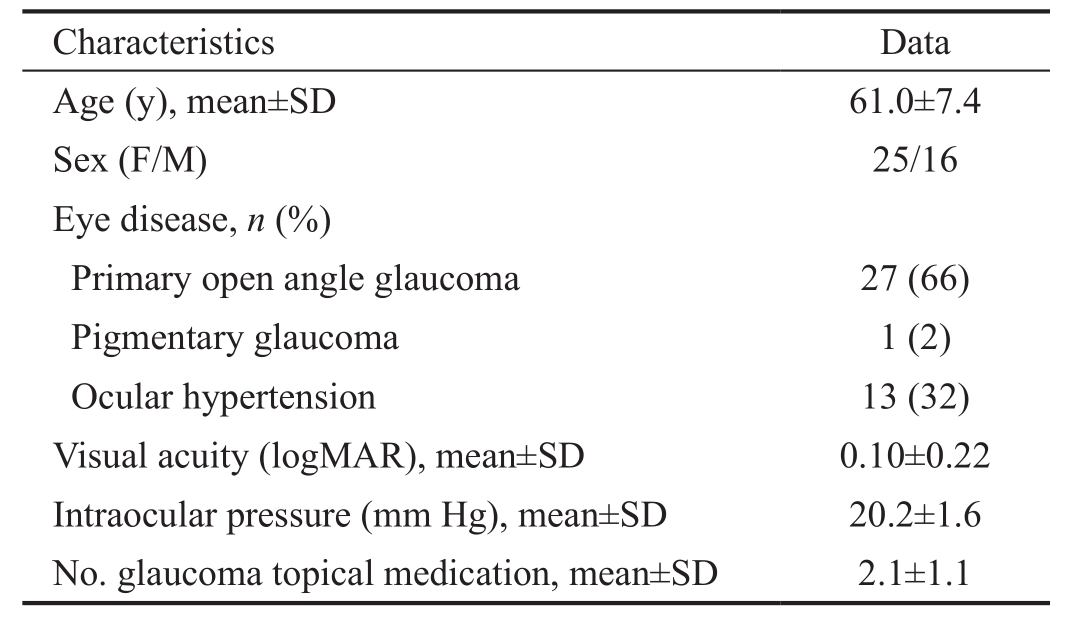
SD: Standard deviation.
Table 2 Intraocular pressure distribution by follow-up visit after patterned laser trabeculoplasty mean±SD (range); n=41
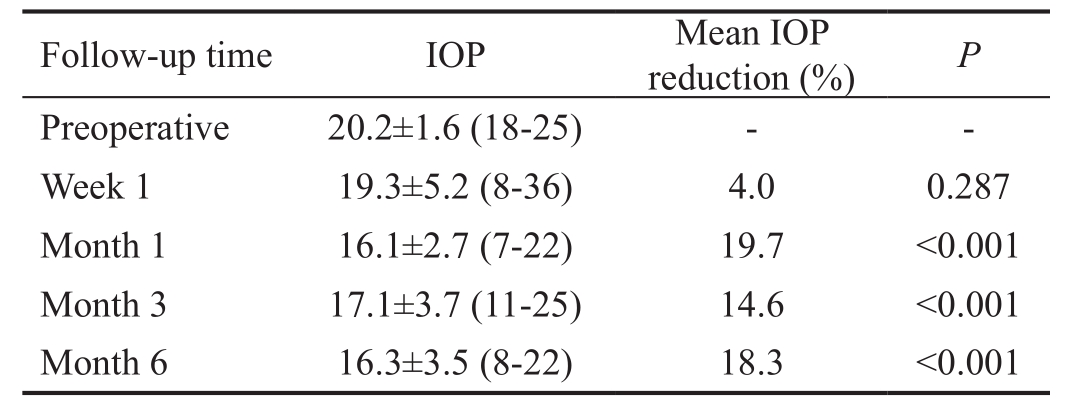
IOP: Intraocular pressure; SD: Standard deviation. P value by the t-test.
Table 3 Success rate and number of glaucoma topical medications in treated eyes during 6mo of follow-up
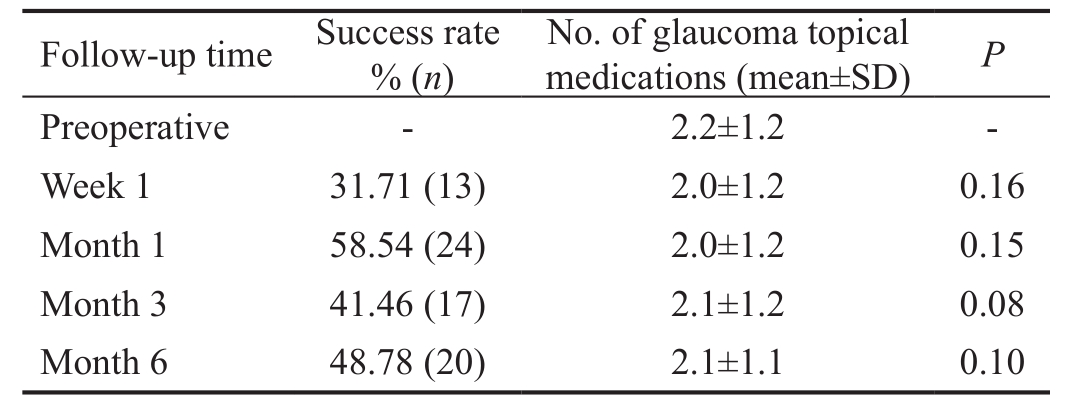
SD: Standard deviation. P value by t-test.
DISCUSSION
This study was aimed to evaluate the effectiveness of PASCAL PLT as an adjuvant treatment in the control of IOP in OHT and OAG patients. Our results show that during a 6-month follow-up period, this procedure proved to be effective with an adequate safety pro file. Similarly to other studies with PLT[19-20],there was no evidence of a statistically significant change in the use of glaucoma topical medications after the procedure.

Figure 2 Gonioscopy image of peripheral anterior synechiae The PAS presented in a 70-year-old female patient 3mo after laser treatment. It has a wide base and inserts to the trabecular meshwork,extending along 2 clock hours (white arrows).
Turati et al[16]in 2010 performed a prospective pilot study in 47 eyes of 25 patients using the PASCAL laser with a wavelength of 532 nm. The PLT results with this PASCAL model showed a mean IOP reduction from 21.9±4.1 mm Hg preoperatively to 15.5±2.7 mm Hg at 6mo after treatment. An IOP reduction >20% was evident in 67% of eyes. However,at 6-month follow-up visit only 30 out of the 47 eyes were evaluated, and 8 eyes were excluded (4 of which IOP returned to its pre-laser values and the other 4 eyes were impossible to evaluate due to viral conjunctivitis). In those patients, no transient IOP spikes or other early complications were found.Nozaki et al[20]conducted a retrospective study in 11 eyes of 9 patients achieving an IOP reduction of 31% (from 20.5±4.7 to 13.4±3.7 mm Hg) at 6mo follow-up. In that study only a transient increase of IOP in one eye (9%) was reported. Barbu et al[19]conducted a prospective, randomized clinical trial in 2014 comparing the effectiveness of PLT and ALT. Fortytwo eyes were evaluated, showing an IOP reduction in the PLT group from 20.2±1.1 to 15.6±0.8 mm Hg at 8wk after the procedure. The ALT group achieved an IOP reduction from a mean preoperative IOP of 18.6 to 15.3 mm Hg at 8wk followup visit. Those results were similar (22.8% IOP reduction in the PLT group and 17.7% in the ALT group), and the comparison between both laser methods was not significant(P=0.26). Mansouri and Shaarawy[18]designed a prospective,randomized clinical trial comparing the efficacy of PLT and SLT. The IOP levels in the PLT group dropped from 17.3±4.0 to 14.0±2.7 mm Hg (19.1%), and from 16.8±3.6 to 13.7±3.1 mm Hg (18.5%) in the SLT group, showing no statistically significant difference between both groups. The>20% IOP decrease in the PLT and SLT groups at 6mo followup was achieved by 37% and 26% of the evaluated eyes,respectively. The authors explained the low IOP reduction rate suggesting that the lower the baseline IOP is, the lower the post-treatment reduction rate might be. Ten eyes in the PLT group had conjunctival hyperaemia and anterior chamber flare within 24h postoperatively.
Similarly to other laser trabeculoplasty studies, we found an IOP reduction in patients with medically uncontrolled glaucoma. Shibata et al[21]carried out a retrospective study in 2012 comparing the results of SLT as an adjuvant treatment in 2 groups: 180° treatment and 360° treatment. During followup both groups showed a significant IOP reduction. At 6mo the IOP reduction had been 5.6 mm Hg in the 360° group and 2.6 mm Hg in the 180° group, which represented a statistically significant difference in favor of the 360° group.
An interesting finding of our work was the presence of PAS in 17% of treated eyes (7 eyes). This can probably be explained by the learning curve that is required for the proper use of the equipment considering that these patients represented our first experiences with this type of technology. As this device uses a pattern of laser spots, it may involve a larger space of the trabecular meshwork, leading to a possible laser application at its posterior area. This mechanism has been described as a risk factor for the development of this complication in ALT patients[22]. It is also important to emphasize that patients who developed PAS presented borderline open angles in the affected areas, which may be a particular condition to perform this type of procedure. Another interesting finding was that the most affected area was the inferior portion of the angle (5/7 eyes) making possible the idea that the titration site could lead to PAS due to more delivered energy. Finally, it is not easy to estimate the appropriate energy for the power titration on the trabecular meshwork, being this a determining effect in the development of PAS, as described by Rouhiainen in eyes treated with ALT, the risk of PAS was higher as long as the laser power increased[23].
In recent years, newer lasers for trabeculoplasty have been described. Micropulse diode laser trabeculoplasty (MDLT)delivers energy in repetitive microsecond pulses followed by an intermittent rest period, thereby reducing the build-up of thermal energy. In a phase II prospective interventional case series, Fea et al[24]evaluated the efficacy of 180° MDLT in 20 eyes of 20 patients during 12mo of follow-up. They found that 66.67% of patients who reached the 12-months follow-up visit(n=15 eyes) achieved an IOP reduction of ≥20%. Only one eye developed IOP spike and flare, and no PAS or change in visual acuity was detected. Titanium-sapphire laser trabeculoplasty(TSLT) is another type of laser trabeculoplasty that uses a 790 nm wavelength laser, emitting near-infrared energy in pulses ranging from 5 to 10ms. This is thought to allow deeper penetration into the yuxtacanalicular trabecular meshwork and the inner wall of Schlemm’s canal. A prospective randomized clinical trial with 37 subjects comparing TSLT versus SLT was published in 2016. After 2y, it demonstrated that TSLT treated eyes had a mean IOP reduction of 35%, while the ALT group achieve a 25% IOP reduction. There was no statistical difference between the two groups. Three patients in the TSLT group and three patients in the SLT group experienced IOP spikes ≥10 mm Hg[25].
SLT and ALT have been standard therapeutic interventions in OAG and OHT. The mechanism through which the laser trabeculoplasty works is not entirely clear. In tissue cultures,SLT has been found to selectively target pigmented trabecular meshwork cells while sparing adjacent cells and tissues from collateral thermal damage. The laser’s brief pulse duration confines heat to the pigmented cells within the irradiated zone. In contrast, ALT destroyed all cells (with and without pigment) in culture models. According to Latina and Park[9],at pulse duration between 10ns and 1µs energy is deposited within the target (pigmented trabecular meshwork cells) more rapidly than it can diffuse away, hence minimising damage to the surrounding non-pigmented trabecular meshwork cells. Therefore with a pulse duration of 3ns, SLT selectively confines the energy to the pigmented cells, whereas in ALT heat gets dissipated from the pigmented cells to the surrounding tissues, damaging the non-pigmented cells within the irradiation zone. Turati et al[16]mentioned that for a pulse duration of 5ms with PLT heat can diffuse to approximately 50 µm.
Recently, Lee et al[17]conducted a study comparing morphologic changes between ALT and PLT in cat’s trabecular meshwork.They demonstrated that performing sub-threshold (250-350 mW)PLT resulted in thinning of the uveal meshwork and denudation of endothelial trabecular cells. Nevertheless, they also reported the late formation of a membranous covering on the trabecular meshwork. They also demonstrated that by applying suprathreshold powers (400-450 mW), thermal damage of the trabecular meshwork could be induced producing an extensive membranous obliteration that could lead to difficulty in later aqueous outflow as seen with ALT. Since trabecular collapse showed by them in ALT and supra-threshold PLT is a consistent finding in the glaucomatous eye, they speculate that supra-threshold PLT may have at least deleterious effects on the IOP behaviour.
Our study is limited by its retrospective design and short-term follow-up. Another possible limitation could be the difference of IOP measurement time of the day before and after laser treatment and the possible improvement of compliance with medical therapy after laser treatment.
In conclusion, we can emphasize that PLT is an effective and safe method for the management of patients with OHT or OAG as an adjunctive therapy. Patients described as having borderline open angles may be carefully selected in order to avoid complications such as PAS. Additional larger studies should be designed to verify the long-term stability of IOP reduction with this laser technology.
ACKNOWLEDGEMENTS
Authors’ contributions:Study concept and design (Espinoza G, Castellanos L, Parra JC); data collection (Espinoza G); analysis and interpretation of data (Espinoza G, Rodriguez-Una I,Camacho PA); drafting of the manuscript (Rodriguez-Una I);critical revision of the manuscript (Espinoza G, Castellanos L,Rodriguez-Una I, Parra JC); supervision (Castellanos L, Parra JC).
Conflicts of Interest:Espinoza G, None; Castellanos L,None; Rodriguez-Una I, None; Camacho PA, None; Parra JC, None.
REFERENCES
1 Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY.Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology 2014;121(11):2081-2090.
2 Gordon MO, Beiser JA, Brandt JD, Heuer DK, Higginbotham EJ,Johnson CA, Keltner JL, Miller JP, Parrish RK 2nd, Wilson MR, Kass MA. The ocular hypertension treatment study: baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol 2002;120(6):714-720; discussion 829-730.
3 Leske MC, Wu SY, Hennis A, Honkanen R, Nemesure B. Risk factors for incident open-angle glaucoma; the Barbados Eye Studies.Ophthalmology 2008;115(1):85-93.
4 Weinreb RN, Aung T, Medeiros FA. The pathophysiology and treatment of glaucoma: a review. JAMA 2014;311(18):1901-1911.
5 Dreer LE, Girkin C, Mansberger SL. Determinants of medication adherence to topical glaucoma therapy J Glaucoma 2012;21(4):234-240.
6 Robin A, Grover DS. Compliance and adherence in glaucoma management. Indian J Ophthalmol 2011;59(Suppl):S93-S96.
7 Wise JB, Witter SL. Argon laser therapy for open-angle glaucoma. A pilot study. Arch Ophthalmol 1979;97(2):319-322.
8 Mchugh D, Marshall J, Ffytche TJ, Hamilton PA, Raven A. Ultrastructural changes of human trabecular meshwork after photocoagulation with a diode laser. Invest Ophthalmol Vis Sci 1992;33(9):2664-2671.
9 Latina MA, Park C. Selective targeting of trabecular meshwork cells: in vitro studies of pulsed and CW laser interactions. Exp Eye Res 1995;60(4):359-371.
10 Bovell AM, Damji KF, Hodge WG, Rock WJ, Buhrmann RR, Pan YI.Long term effects on the lowering of intraocular pressure: selective laser or argon laser trabeculoplasty? Can J Ophthalmol 2011;46(5):408-413.
11 Wong MO, Lee JW, Choy BN, Chan JC, Lai JS. Systematic review and meta-analysis on the efficacy of selective laser trabeculoplasty in openangle glaucoma. Surv Ophthalmol 2015;60(1):36-50.
12 Lowry EA, Greninger DA, Porco TC, Naseri A, Stamper RL,Han Y. A comparison of resident-performed argon and selective laser trabeculoplasty in patients with open-angle glaucoma. J Glaucoma 2016;25(3):e157-e161.
13 Blumenkranz MS, Yellachich D, Andersen DE, Wiltberger MW,Mordaunt D, Marcellino GR, Palanker D. Semiautomated patterned scanning laser for retinal photocoagulation. Retina 2006;26(3):370-376.
14 Muqit MM, Marcellino GR, Gray JC, McLauchlan R, Henson DB, Young LB, Patton N, Charles SJ, Turner GS, Stanga PE. Pain responses of Pascal 20 ms multi-spot and 100 ms single-spot panretinal photocoagulation: Manchester Pascal Study, MAPASS report 2. Br J Ophthalmol 2010;94(11):1493-1498.
15 Nagpal M, Marlecha S, Nagpal K. Comparison of laser photocoagulation for diabetic retinopathy using 532-nm standard laser versus multispot pattern scan laser. Retina 2010;30(3):452-458.
16 Turati M, Gil-Carrasco F, Morales A, Quiroz-Mercado H, Andersen D, Marcellino G, Schuele G, Palanker D. Patterned laser trabeculoplasty.Ophthalmic Surg Lasers Imaging 2010;41(5):538-545.
17 Lee JY, Ha SY, Paik HJ, Kwon KY, Kim YY. Morphologic changes in trabecular meshwork after patterned and argon laser trabeculoplasty in cats. Curr Eye Res 2014;39(9):908-916.
18 Mansouri K, Shaarawy T. Comparing pattern scanning laser trabeculoplasty to selective laser trabeculoplasty: A randomized controlled trial. Acta Ophthalmol 2017;95(5):e361-e365.
19 Barbu CE, Rasche W, Wiedemann P, Dawczynski J, Unterlauft JD.Pattern laser trabeculoplasty and argon laser trabeculoplasty for treatment of glaucoma. Ophthalmologe 2014;111(10):948-953.
20 Nozaki M, Yoshida M, Ogura Y. Outcomes of patterned laser trabecuoplasty versus selective laser trabeculoplasty in open-angle glaucoma. Poster #4529. Presented at ASCRS Meeting 2014; April 25-29,2014; Boston, MA.
21 Shibata M, Sugiyama T, Ishida O, Ueki M, Kojima S, Okuda T,Ikeda T. Clinical results of selective laser trabeculoplasty in open-angle glaucoma in Japanese eyes: comparison of 180 degree with 360 degree SLT. J Glaucoma 2012;21(1):17-21.
22 Traverso CE, Greenidge KC, Spaeth GL. Formation of peripheral anterior synechiae following argon laser trabeculoplasty. A prospective study to determine relationship to position of laser burns. Arch Ophthalmol 1984;102(6):861-863.
23 Rouhiainen HJ, Teräsvirta ME, Tuovinen EJ. Peripheral anterior synechiae formation after trabeculoplasty. Arch Ophthalmol 1988;106(2):189-191.
24 Fea AM, Bosone A, Rolle T, Brogliatti B, Grignolo FM. Micropulse diode laser trabeculoplasty (MDLT): A phase II clinical study with 12 months follow-up. Clin Ophthalmol 2008;2(2):247-252.
25 Kaplowitz K, Wang S, Bilonick R, Oatts JT, Grippo T, Loewen NA.Randomized controlled comparison of Titanium-Sapphire versus standard Q-Switched Nd:YAG laser trabeculoplasty. J Glaucoma 2016;25(7):e663-e667.