INTRODUCTION
Laser in situ keratomileusis (LASIK) has been widely accepted as an effective method for the correction of myopia. Armed the femtosecond laser technology and the wavefront technology, both the operation safety and the postoperative visual performance of LASIK have been greatly improved. However, LASIK, as a type of cornea refractive surgery, may not be suitable for high myopia or thin cornea because of the risk for keratectasia. The visian implantable collamer lens (ICL; STAAR Surgical, Nidau, Switzerland), a posterior chamber phakic intraocular lens (pIOL), is developed to rectify these disadvantages[1-5].
Previous studies have shown that ICL implantation is a better approach than laser refractive surgery in terms of fewer higher order aberration (HOA) induction[6-7]. Besides ocular aberrations, many other factors such as cornea clarity[8], cornea density[9]and compromised ocular surface integrity[10]have been proposed to evaluate the optical quality after refractive surgery.
Recently, a newer optical quality evaluation technology,the Optical Quality Analysis System (OQAS; Visiometrics,Terrassa, Spain), has been employed to evaluate the visual performance after cataract or refractive surgeries[11-13]. The system is based on the double-pass technique[14]. It allows the detection of possible asymmetries in the retina images and the objective measurement of ocular scatter[15].
The purpose of our study was to employ two types of technology:the OQAS and wavefront system to evaluate the changes of the optical quality after ICL implantation or wavefront-guided LASIK and explore the relationship between the intraocular scatter and HOA.
SUBJECTS AND METHODS
Participants Forty eyes of twenty subjects (11 females, 9 males)with myopia that received wavefront-guided LASIK (WGLASIK) and forty eyes of twenty-two subjects (10 females,12 males) with myopia that underwent ICL implantation(V4c model, Staar Surgical Company, Monrovia, California,USA) were enrolled in this prospective study. Four eyes of four patients in ICL group were excluded due to unreliable preoperative wavefront data or optical quality images (poor visual acuity or fixation). Informed consent was obtained from all subjects in accordance with institutional guidelines. The study followed the tenets of the Declaration of Helsinki and was approved by the Guangxi Institutional Review Board/Ethics Committee.
Methods Before and three months after surgery, the OQAS(Visiometrics, Terrassa, Spain) was applied to access the optical quality parameters, namely the objective scattering index (OSI), the values of modulation transfer function (MTF)cutoff frequency, the Strehl ratio, and the Optical Quality Analysis System values (OVs).
The meanings and calculations of the parameters have been explained in several studies[13,16]. The OSI is an objective evaluation of intraocular scattered light. The index is calculated by evaluating the amount of light outside the double-pass retinal intensity point spread function (PSF) image in relation to the amount of light in the center. The MTF cutoff value is the frequency at which the MTF reaches a value of 0.01.It refers to the frequency up to which the eye can focus an object on the retina with a significant 1% contrast. The three OVs are normalized values of three spatial frequencies, which correspond to MTF values that describe the optical quality of the eye for three contrast conditions, commonly used in ophthalmic practice: 100% (OV 100%), 20% (OV 20%), and 9% (OV 9%).
The Strehl ratio is the ratio of the central maximum of the illuminance of the PSF in the aberrated eye to the central maximum that would be found in a corresponding aberrationfree system.
The HOAs data were also obtained with the iDesign WaveScan System (Abbott Medical Optics Inc., California, USA).Wavefront aberrations data, namely the total HOA, the coma,the trefoil, the spherical, the 2ndastigmatism and the tetrafoil were recorded at the central 4 mm area if pupil’s diameter smaller than 6 mm or central 6 mm area if pupil’s diameter larger than 6 mm. Zernike polynomial expansions up to fourth radial order are calculated to for a 4 mm and 6 mm pupil. Root mean square (RMS) values of the HOAs were analyzed. All RMS were expressed in micrometers.
Implantable Collamer Lens Calculation and Surgical Procedure ICL power calculations were performed with the STAAR surgical official online calculator. The size of the ICL was also chosen based on the horizontal corneal diameter and anterior chamber depth measured with scanning-slit topography (Orbscan IIz; Bausch & Lomb, Rochester, New York, USA). Emmetropia was selected as the target refraction to minimize preoperative refractive errors.
On the day of surgery, the patients were given dilating and cycloplegic agents. After topical anesthesia, a 3.0-mm clear corneal incision was made. The anterior chamber was filled with 1% sodium hyaluronate, and a model V4c ICL was injected through the incision into the anterior chamber. Distal and proximal foot plates were tucked under the iris with a spatula. The ICL was centered, and the remaining viscoelastic material was irrigated out of the anterior chamber with a balanced salt solution (BSS).
Wavefront-guided Laser In Situ Keratomileusis The wavefront-guided LASIK procedure was performed with the STAR S4 IR excimer laser system with iris registration (Abbott Medical Optics Inc., California, USA). Wavefront data was obtained with the iDesign Wavescan system (Abbott Medical Optics Inc., California, USA) one day before the operation.LASIK flaps were created using the IntraLase femtosecond laser system (Abbott Medical Optics, Inc., California, USA)with a superior hinge of 110-µm thicknesses.
Statistical Analysis All analyses were performed using SPSS statistical package (Version 22.0; IBM SPSS Inc., Chicago,Illinois, USA). Wilcoxon signed-ranks test was applied to compare the data before and after operations due to the nonnormal distribution of the data. A P-value less than 0.05 was considered statistically significant.
Table 1 Preoperative demographics of study subjects mean±SD
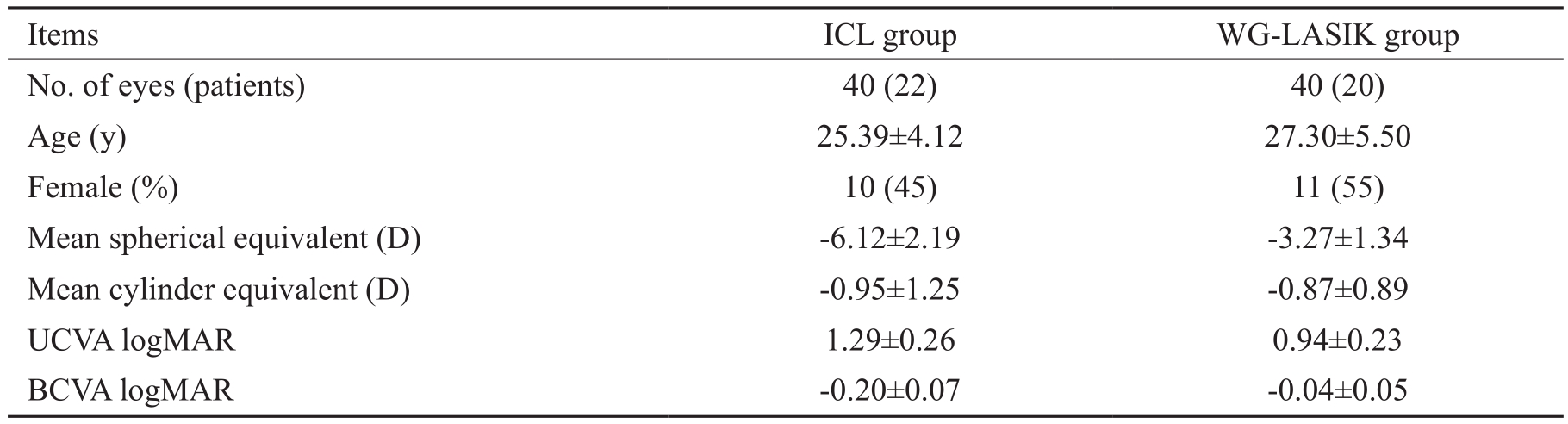
ICL: Implantable collamer lens; WG-LASIK: Wavefront-guided laser in situ keratomileusis; D: Diopters; UCVA:Uncorrected visual acuity; BCVA: Best-corrected visual acuity; logMAR: Logarithm of the minimal angle of resolution.
Table 2 Pre- and postoperative optical quality parameters in both groups
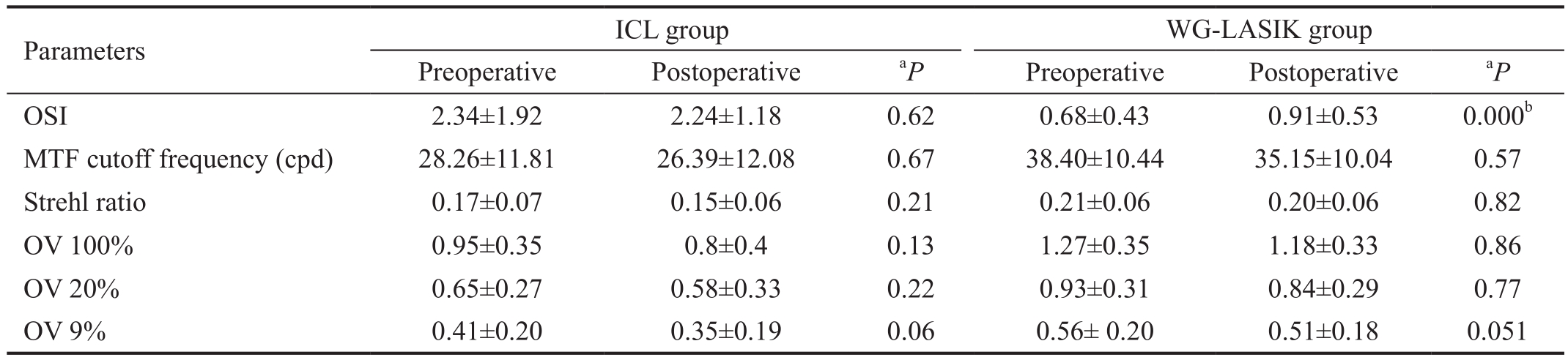
aPre-post comparison by Wilcoxon signed ranks test;bStatistical significance. ICL: Implantable collamer lens; WG-LASIK: Wavefront-guided laser in situ keratomileusis; OSI: Objective scattering index; MTF: Modulation transfer function; OV: Optical Quality Analysis System values.
RESULTS
All surgical procedures were uneventful and no postoperative complications were observed during the three months follow up. Detailed demographic information of the study subjects was shown in Table 1. There were no significant differences between two groups in age or gender.
The preoperative logMAR UCVA in the ICL group and the WG-LASIK group were 1.29±0.26 and 0.94±0.23,respectively. After the operations, logMAR UCVA improved significantly to -0.04±0.05 in the ICL group and -0.08±0.06 in the WG-LASIK group (Wilcoxon signed ranks test,P<0.001).
The preoperative refractive error (mean spherical equivalent) in the ICL group and WG-LASIK group were -6.12±2.19 D and-3.27±1.34 D, respectively. Significant reduction in spherical equivalent was found postoperatively, with the refractive error was 0.22±0.48 D in the ICL group and -0.12±0.36 D in the WG-LASIK group (Wilcoxon signed ranks test, P<0.001).
Because of the relatively high myopia in the ICL group and low-moderate myopia in the LASIK group, the analysis of optical quality changes was applied to the data of each group.No direct between-groups comparison was used in this study.There were no statistical differences of the OSI, the MTF cutoff frequency, and the OVs before and after ICL implantation.In the WG-LASIK group, the OSI increased from 0.68±0.43 preoperatively to 0.91±0.53 postoperatively (Wilcoxon signed ranks test, P=0.000). The results are summarized in Table 2 and Figure 1.
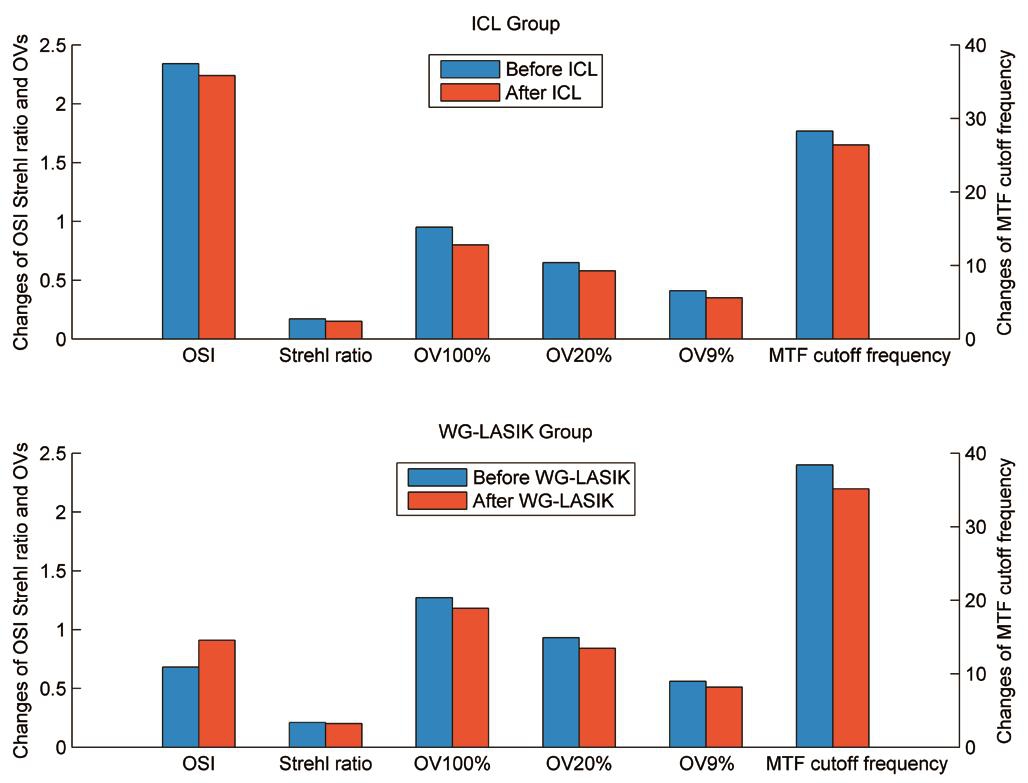
Figure 1 Pre- and postoperative optical quality parameters in both groups.
None of HOAs parameters in the ICL group statistically changed after the operation at either 4 mm-pupil or 6 mmpupil, except some higher order components such as trefoil,tetrafoil and 2ndastigmatism increased at 6 mm-pupil. The total ocular HOAs, coma, spherical and 2ndastigmatism increased significantly at 4 mm-pupil in the WG-LASIK group, with the corresponding values of 0.16±0.07 μm, 0.08±0.05 μm,-0.04±0.04 μm, 0.03±0.01 μm, postoperatively (Wilcoxon signed ranks test, all P values <0.05). No changes of total HOAs in the WG-LASIK group at 6 mm-pupil were observed. Table 3 and Figure 2 showed the HOA data in both groups.
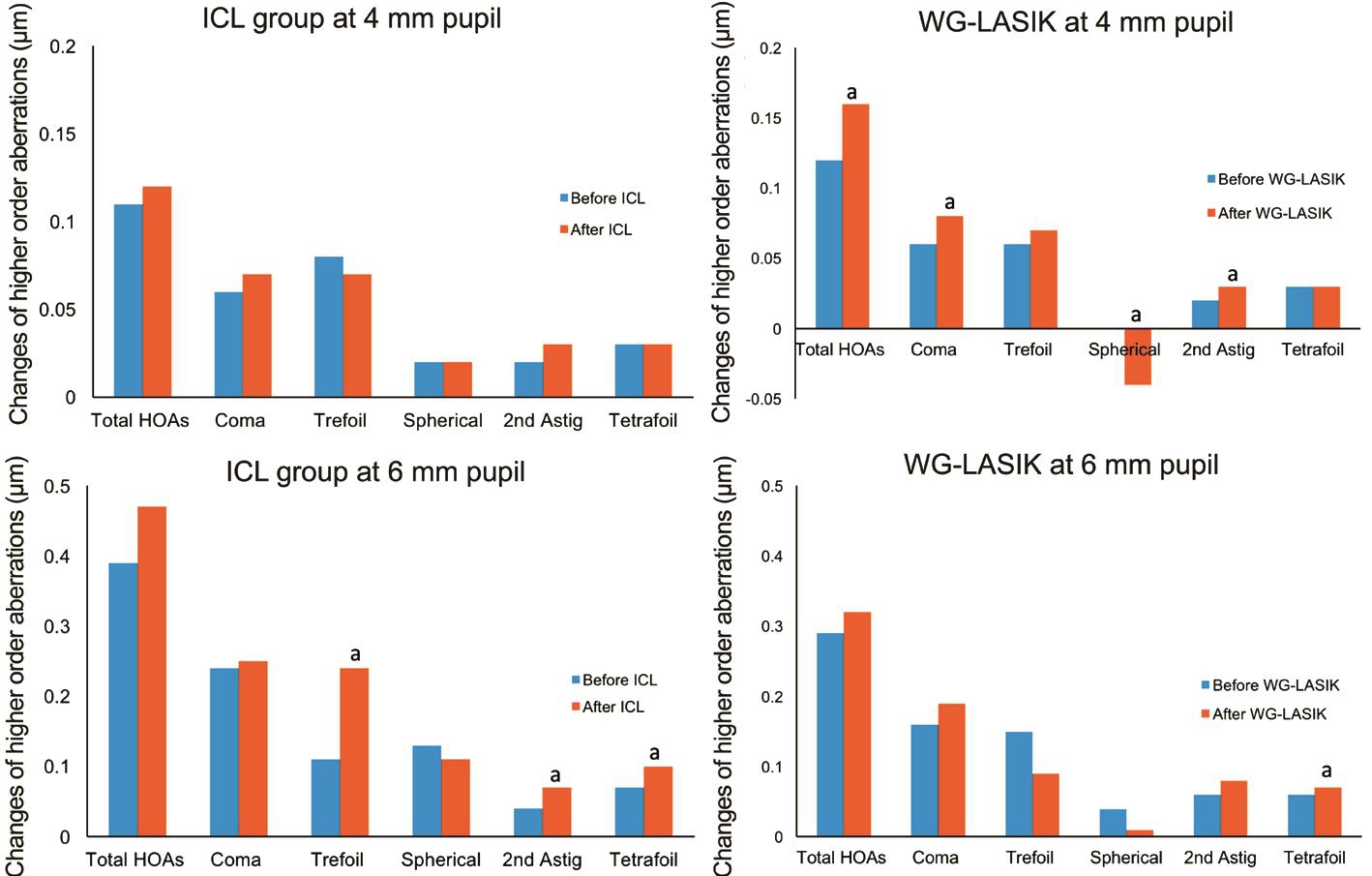
Figure 2 Pre- and postoperative higher order aberrations in both groupsaStatistically significant difference after ICL or WG-LASIK operation.
Table 3 Pre- and postoperative higher order aberrations in both groups mean±SD, μm
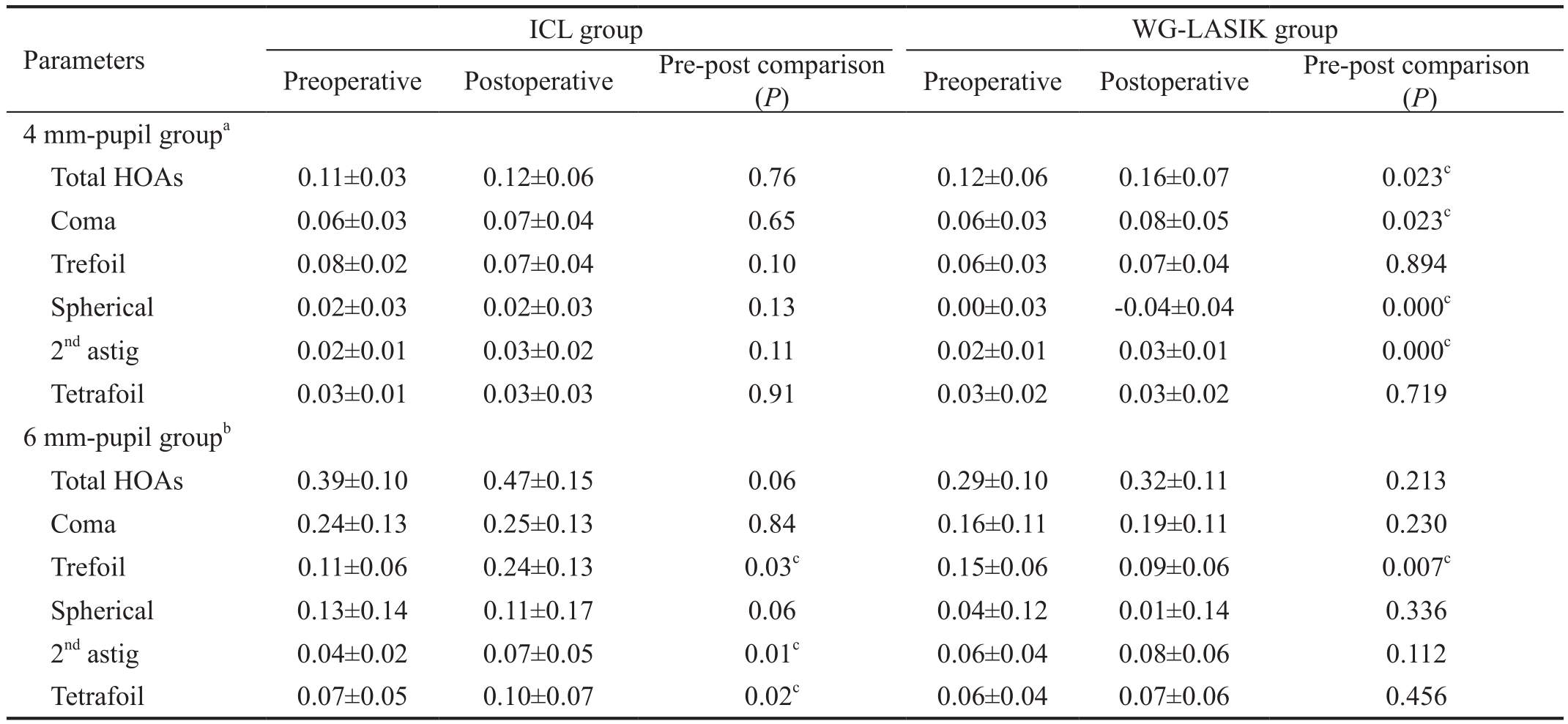
an=19 of 4 mm-pupil in ICL group, n=16 of 4 mm-pupil in WG-LASIK group;bn=21 of 6 mm-pupil in ICL group, n=24 of 6 mm-pupil in WGLASIK group;cStatistical significance. ICL: Implantable collamer lens; WG-LASIK: Wavefront-guided laser in situ keratomileusis; HOAs:Higher-order aberrations.
DISCUSSION
With the ability of quantitatively accessing retina image quality and intraocular scattering, OQAS is an advanced tool in evaluating the optical quality changes after refractive surgeries[13,17].
Our study demonstrated that ICL implantation nearly had no disturbance to the optical quality, as there was no statistically significant change of the OSI after the operation. In contrast,the OSI of LASIK group slightly increased postoperatively.This is probably due to their entirely different approaches of correcting myopia. ICL surgery implants or “adds” a mini optical lens hence leaves the optical eye system intact. LASIK surgery removes or “minuses” a small amount of corneal tissue and the cornea curve flattens consequently. The cornea tissue damage, flap-stroma interface healing process after LASIK may cause the potential loss of corneal transparency[9].The increased intraocular scattering and increased cornea densitometry after cornea refractive surgeries were also observed in several studies[9,17-18].
In LASIK, the wavefront guided-ablation method has been reported to be effective for reducing the induction of HOAs than conventional LASIK[19-20]. The femtosecond laser technology used in the flap creation was also proved to be better than a mechanical microkeratome in terms of induction of HOAs[21].Our study results indicated that ICL implantation induced fewer HOA than wavefront guide and femtosecond-assisted LASIK, which is in accordance with previous studies[6-7,22].Different anatomical targets to correct refractive errors may be responsible for these results[22]. The ICL implantation does not involve surgical tissue abstraction and leaves the central cornea untouched while LASIK requires cornea ablation and creates a flattened cornea shape. The change of the corneal contour resulted in an increase in HOAs, especially the spherical aberration shifting from positive value preoperatively to negative value postoperatively, as shown in our LASIK group.Besides the OSI, the OQAS provides other parameters such as the MTF cutoff value, the Strehl ratio, and the three OVs to access the optical quality. In our study, none of them has showed significant changes in both ICL and LASIK groups.The high sensitivity of OSI was observed when evaluating the effect of aging[5]on optical quality or grading posterior capsule opacification[11]. The OSI parameter also proved to be more sensitive than HOAs in evaluating the corneal optical quality.Kamiya et al[23-24]suggested that light scattering, represented by OSI, played a more vital role in visual performance than corneal aberrations in eyes with GCD and DSAEK.
We noticed that in the ICL group, some higher order components such as trefoil, tetrafoil and 2ndastigmatism increased at 6 mm pupil, it is probably due to the relatively small optical zone of the V4c model (5.8 mm for less than-10.00 D), a newer generation (Model V5) with larger optical zone will be soon launched on market to overcome the drawback[25].
The limits of the study were that the ICL group consisted of patients with high myopia while LASIK group mainly included patients with low-moderate myopia. In consideration of the complexity of ICL implantation as well as the relative high costs, ICL is taken as a complementary treatment in our clinic when patients are not illegible for LASIK. It led to higher myopia in our ICL group. Hence, we adopted a matched pair design to analyze the pre- and postoperative optical quality changes within each group. A direct comparison of ICL group and WG-LASIK group was avoided.
In conclusion, ICL implantation induces less optical quality disturbance that LASIK operation. The optical scattering index, obtained with the OQAS, is a more sensitive parameter to evaluate the optical quality than the HOAs. Further studies of a greater number of subjects with equivalent myopia degrees are required to con firm these preliminary findings.
ACKNOWLEDGEMENTS
Foundations:Supported by the Research Grant of Guangxi Natural Science Foundation (No.2015GXNSFCB139012;No.2017GXNSFBA198320); the Research Grant of Guangxi Technology and Science Agency (No.Z2015316).
Conflicts of Interest:Liu HT, None; Zhou Z, None; Luo WQ, None; He WJ, None; Agbedia O, None; Wang JX,None; Huang JZ, None; Gao X, None; Kong M, None; Li M,None; Li L, None.
REFERENCES
1 Sanders DR, Brown DC, Martin RG, Shepherd J, Deitz MR, DeLuca M. Implantable contact lens for moderate to high myopia: phase 1 FDA clinical study with 6 month follow-up. J Cataract Refract Surg 1998;24(5):607-611.
2 Uusitalo RJ, Aine E, Sen NH, Laatikainen L. Implantable contact lens for high myopia. J Cataract Refract Surg 2002;28(1):29-36.
3 Sanders DR, Vukich JA, Doney K, Gaston M; Implantable Contact Lens in Treatment of Myopia Study Group. U.S. Food and Drug Administration clinical trial of the implantable contact lens for moderate to high myopia.Ophthalmology 2003;110(2):255-266.
4 Sanders D, Vukich JA. Comparison of implantable collamer lens (ICL)and laser-assisted in situ keratomileusis (LASIK) for low myopia. Cornea 2006;25(10):1139-1146.
5 Martinez-Roda JA, Vilaseca M, Ondategui JC, Aguirre M, Pujol J.Effects of aging on optical quality and visual function. Clin Exp Optom 2016;99(6):518-525.
6 Kamiya K, Igarashi A, Shimizu K, Matsumura K, Komatsu M. Visual performance after posterior chamber phakic intraocular lens implantation and wavefront-guided laser in situ keratomileusis for low to moderate myopia. Am J Ophthalmol 2012;153(6):1178-1186 .
7 Igarashi A, Kamiya K, Shimizu K, Komatsu M. Visual performance after implantable collamer lens implantation and wavefront-guided laser in situ keratomileusis for high myopia. Am J Ophthalmol 2009;148(1):164-170.
8 van de Pol C, Soya K, Hwang DG. Objective assessment of transient corneal haze and its relation to visual performance after photorefractive keratectomy. Am J Ophthalmol 2001;132(2):204-210.
9 Poyales F, Garzón N, Mendicute J, Illarramendi I, Caro P, Jáñez O, Argüeso F, López A. Corneal densitometry after photorefractive keratectomy, laser-assisted in situ keratomileusis, and small-incision lenticule extraction. Eye (Lond) 2017;31(12):1647-1654.
10 Montés-Micó R, Cerviño A, Ferrer-Blasco T, García-Lázaro S,Madrid-Costa D. The tear film and the optical quality of the eye. Ocul Surf 2010;8(4):185-192.
11 Zhang H, Wang J. Visual quality assessment of posterior capsule opacification using Optical Quality Analysis System (OQAS). J Ophthalmol 2017;2017:9852195.
12 Chen Y, Wang X, Zhou CD, Wu Q. Evaluation of visual quality of spherical and aspherical intraocular lenses by Optical Quality Analysis System. Int J Ophthalmol 2017;10(6):914-918.
13 Kamiya K, Shimizu K, Saito A, Igarashi A, Kobashi H. Comparison of optical quality and intraocular scattering after posterior chamber phakic intraocular lens with and without a central hole (Hole ICL and Conventional ICL) implantation using the double-pass instrument. PLoS One 2013;8(6):e66846.
14 Güell JL, Pujol J, Arjona M, Diaz-Douton F, Artal P. Optical Quality Analysis System; Instrument for objective clinical evaluation of ocular optical quality. J Cataract Refract Surg 2004;30(7):1598-1599.
15 Artal P, Marcos S, Navarro R, Williams DR. Odd aberrations and double-pass measurements of retinal image quality. J Opt Soc Am A Opt Image Sci Vis 1995;12(2):195-201.
16 Shimizu K, Kamiya K, Igarashi A, Shiratani T. Intraindividual comparison of visual performance after posterior chamber phakic intraocular lens with and without a central hole implantation for moderate to high myopia. Am J Ophthalmol 2012;154(3):486-494
17 Miao H, Tian M, Xu Y, Chen Y, Zhou X. Visual outcomes and optical quality after femtosecond laser small incision lenticule extraction: an 18-month prospective study. J Refract Surg 2015;31(11):726-731.
18 Lee K, Ahn JM, Kim EK, Kim TI. Comparison of optical quality parameters and ocular aberrations after wavefront-guided laser in-situ keratomileusis versus wavefront-guided laser epithelial keratomileusis for myopia. Graefes Arch Clin Exp Ophthalmol 2013;251(9):2163-2169.
19 Kim TI, Yang SJ, Tchah H. Bilateral comparison of wavefront-guided versus conventional laser in situ keratomileusis with Bausch and Lomb Zyoptix. J Refract Surg 2004;20(5):432-438.
20 He R, Qu M, Yu S. Comparison of NIDEK CATz wavefront-guided LASIK to traditional LASIK with the NIDEK CXII excimer laser in myopia. J Refract Surg 2005;21(5):S646-S649.
21 Buzzonetti L, Petrocelli G, Valente P, Tamburrelli C, Mosca L, Laborante A, Balestrazzi E. Comparison of corneal aberration changes after laser in situ keratomileusis performed with mechanical microkeratome and IntraLase femtosecond laser: 1-year follow-up. Cornea 2008;27(2):174-179.
22 Shin JY, Ahn H, Seo KY, Kim EK, Kim TI. Comparison of higher order aberrations after implantable collamer lens implantation and wavefrontguided LASEK in high myopia. J Refract Surg 2012;28(2):106-111.
23 Kamiya K, Kobashi H, Igarashi A, Shoji N, Shimizu K. Effect of light scattering and higher-order aberrations on visual performance in eyes with granular corneal dystrophy. Sci Rep 2016;6:24677.
24 Kamiya K, Asato H, Shimizu K, Kobashi H, Igarashi A. Effect of Intraocular forward scattering and corneal higher-order aberrations on visual acuity after descemet’s stripping automated endothelial keratoplasty. PLoS One 2015;10(6):e0131110.
25 Domínguez-Vicent A, Ferrer-Blasco T, Pérez-Vives C, Esteve-Taboada JJ, Montés-Micó R. Optical quality comparison between 2 collagen copolymer posterior chamber phakic intraocular lens designs. J Cataract Refract Surg 2015;41(6):1268-1278.