INTRODUCTION
Laser in situ keratomileusis (LASIK) has been acknowledged as one of the most widely performed corneal refractive surgery for the correction of myopia, for its high rate of safety and predictability, good visual outcomes and minimal postoperative discomfort[1-3]. Despite generally satisfactory outcomes of LASIK, we need to pay more attention to the high precision and better visual outcomes and to improve some surgical parameters such as ablation centration and the size of optical zone[4-11].
As one of the factors that may impact corneal aberrations induced by laser refractive surgery, ablation centration has been taken great account of particularly in eyes with large angle Kappa[12-16]. The angle Kappa is formally defined as the angular distance in the object space between the pupillary
axis and the line of sight[17]. It could be identified clinically by the nasal displacement of the corneal light reflex f0* 0rom the pupil center, thus, to some extent, it means the misalignment of light passing through the refractive surface of the cornea and the bundle of light formed by the pupil. Therefore, the measurement of angle Kappa is of great significance and paramount consideration in refractive surgery, in order to get the good postoperative optical outcomes. Many studies have concerned decentered ablation in refractive surgery[18]and
angle Kappa adjustment according to topography guidance in excimer laser platform. While how to make an appropriate adjustment when it failed to match the image from topography with the live image during surgery by excimer laser platform is still being unclear. Therefore, this study is performed to compare the effect between angle Kappa adjustment manually based on Oculyzer topography and adjustment automatically guided by Topolyzer Vario topography in ablation of LASIK for myopia, in order to evaluate the clinic value of Oculyzer topography guidance in angle Kappa adjustment during LASIK surgery.
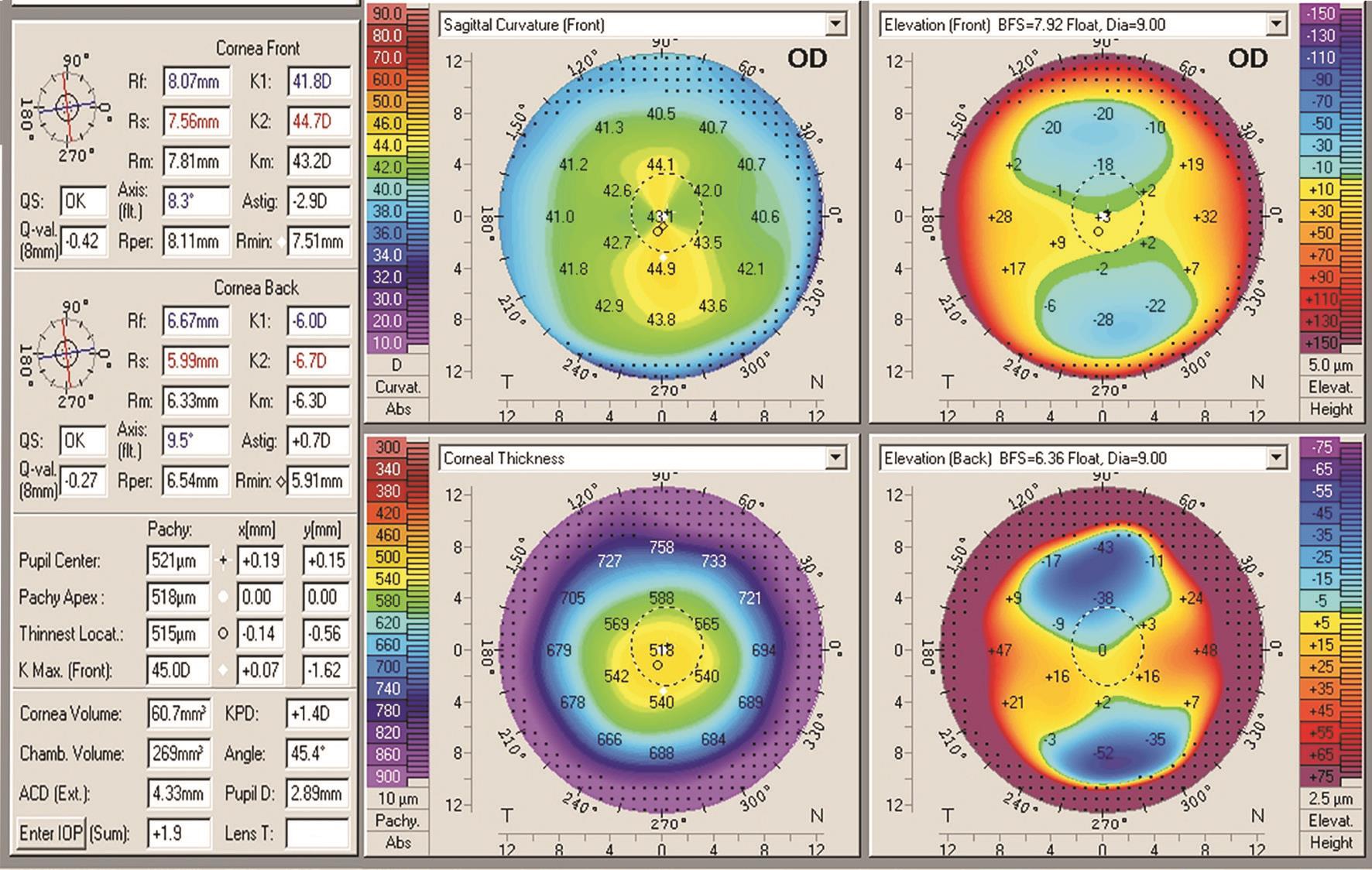
Figure 1 Angle Kappa adjustment guided by Oculyzer topography.
SUBJECTS AND METHODS
This retrospective comparative study comprised 290 eyes of consecutive 145 patients who were performed LASIK from March 2014 to October 2015 in Beijing Tongren Hospital.The study was approved by the Institute’s Ethics and Research Committee and fulfilled the principles of the Declaration of Helsinki. Before surgery each patient was informed about the surgery and signed informed consent.
Preoperative examination included logMAR uncorrected distance visual acuity (UDVA) and corrected distance visual acuity (CDVA), manifest refraction and cycloplegic refraction, slit-lamp examination, handy ultrasonic pachymetry(TOMEYSP-100, Japan), corneal topography (Topolyzer Vario; Oculyzer, WaveLight, Germany), and fundus evaluation.The relative positions of pupil centers with respect to corneal apex were registered by means of topographic Cartesian coordinates (dxocuand dyocuin Oculyzer, dxtopoand dytopoin Topolyzer Vario).
Inclusion criteria were eyes with preoperative CDVA of 20/20 or better, stable refractive diopter more than 2y before surgery,contact lens wear discontinuation for at least 2wk before surgery. Exclusion criteria included keratoconus, glaucoma,cataract, corneal and retinal diseases, infectious diseases,abnormal topography, expected residual bed thickness after LASIK less than 300 μm, expected total pachymetry after LASIK less than 400 μm, and previous refractive surgery.
Surgical Technique LASIK was performed by using the WaveLight EX500 excimer laser (Wavelight GmbH,Germany). Surgeries for all cases were performed by one experienced surgeon (Zhang FJ). All treatments were based on optimized aspheric ablation profiles. The flaps were created with the One Use-Plus microkeratome (Moria SA, France)with the hinge on the nasal position. Photoablation was applied to at least 6.0-mm optical zone, with a transition zone of 9 mm.After folding the corneal flap, the laser beam was focused according to the group of the eye. For the study group, the laser beam was manually centered based on the comparison of corneal topography obtained from Oculyzer (Figure 1) and the live image taken from the WaveLight EX500 platform, and the Cartesian coordinates (dxmanuand dymanu) of the ablation were recorded, whereas for the control group, the laser beam was centered automatically guided by the Topolyzer Vario topography image matched with live image in WaveLight EX500 platform, with the Cartesian coordinates (dxautoand dyauto) of the ablation recorded (Figures 2, 3). Once the laser beam was centered, the active eye tracker system was turned on, and the ablation was performed. After the ablation, the flap was then carefully repositioned over the treatment area by the surgeon and checked for the dislocation of flap, debris and bleeding. The flap remains in position by natural adhesion until healing is completed.
Levofloxacin eye drops 0.5% (Santen, Japan), fluorometholone eye drops 0.1% (Allergan, Ireland), and sodium hyaluronate eye drops 0.1% (URSAPHARM Arzneimittel GmbH, Germany)were used four times a day in two weeks postoperatively. Patients were followed up at 1d, 1wk and 1mo after the surgery.
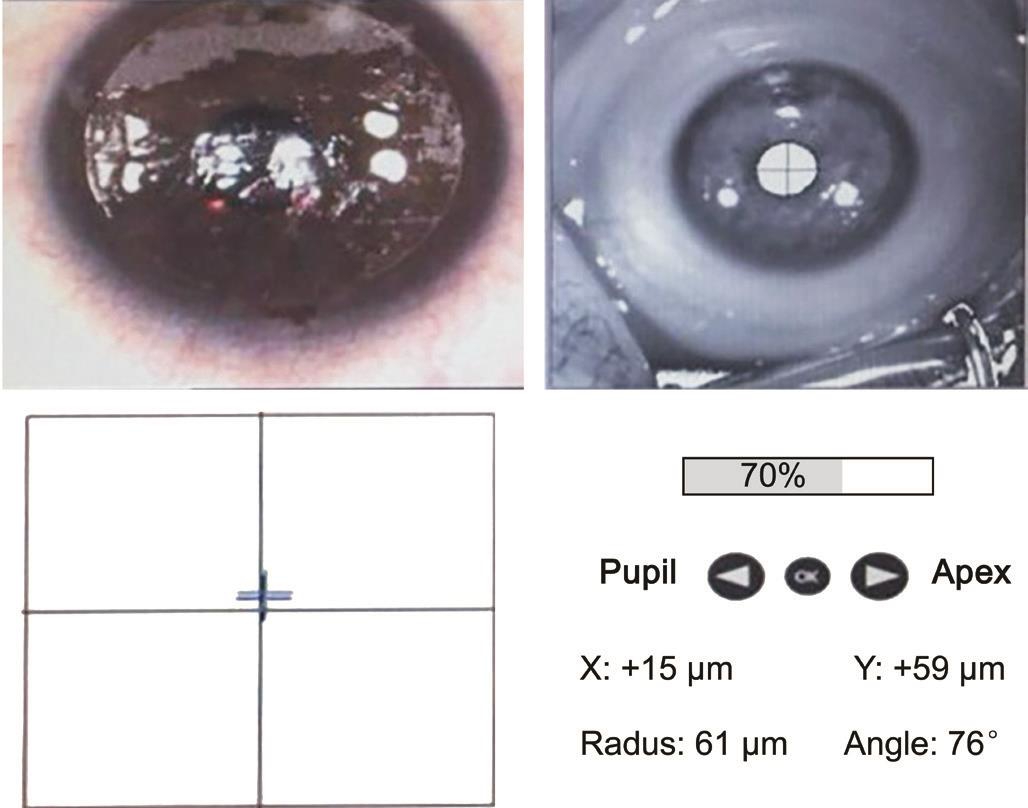
Figure 2 Manually adjustment based on Oculyzer topography in study group dxmanu/dxocuand dymanu/dyocumean the ratio of manually actual values in Figure 2 to Oculyzer topography guided data in Figure 1 in synclastic group.
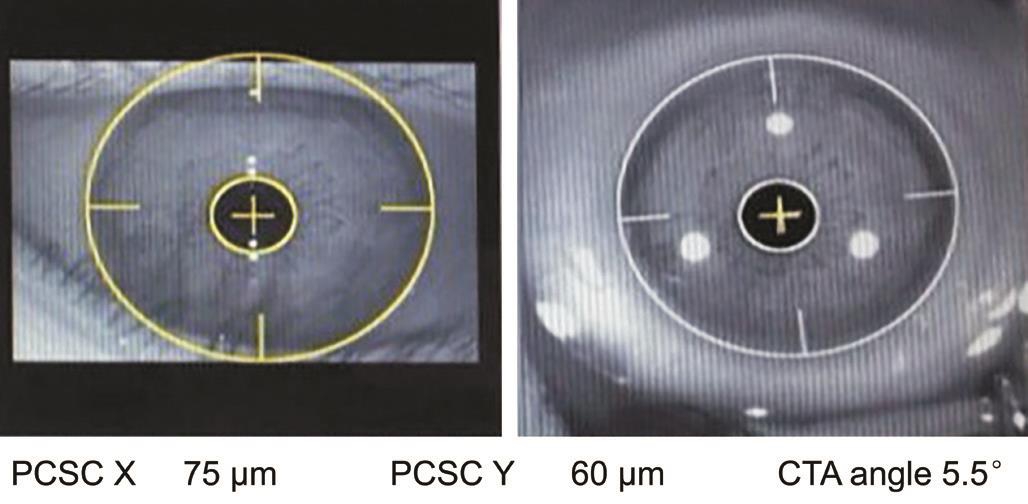
Figure 3 Automatically adjustment guided by Topolyzer Vario topography in control group dxauto/dxocuand dyauto/dyocumean the ratio of automatically actual values in Figure 3 to Oculyzer topography guided data in Figure 1 in synclastic group.
Statistical Analysis Statistical analysis was performed with the SPSS for Windows, version 20.0 (IBM-SPSS, Chicago,Illinois, USA). Visual acuity was converted to logMAR equivalent. The continuous variable were expressed as mean±standard deviation. Independent t-test or Mann-Whitney U test for continuous variables, as appropriate, after testing for normal distributions. The categorical data were expressed as percentage. A P value of less than 0.05 was considered statistically significant. The correlation between different variables was assessed with the correlation coefficients.
Each Cartesian coordinate was analyzed separately in dx and dy. In each direction, we divided data of actual adjustment and Oculyzer topography-guided adjustment into 4 groups:synclastic adjusted (actual adjustment and Oculyzer topography-guided adjustment in the same direction); opposite adjusted (actual adjustment and Oculyzer topography-guided adjustment in the opposite direction); unadjusted (without adjustment actually) and adjusted with no guidance (actual adjustment without Oculyzer topography guidance).
Table 1 Comparison of visual and refractive outcomes between two groups preoperatively mean±SD
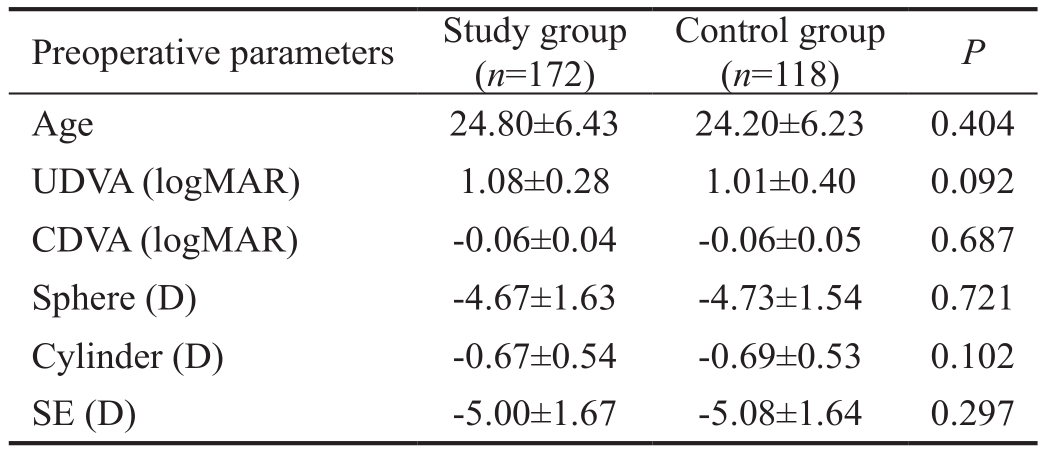
UDVA: Uncorrected distance visual acuity; CDVA: Corrected distance visual acuity; SE: Spherical equivalen.
RESULTS
The study comprised 290 eyes of 145 patients, 172 eyes of 86 patients in the study group and 118 eyes of 59 patients in the control group. Tables 1 and 2 demonstrated that there was no statistically significant difference between two groups in refraction and visual acuity preoperatively and 1d, 1wk, 1mo postoperatively.
Figures 4 and 5 showed the comparison of percentage of eyes in 4 groups between the study and control groups in horizontal and vertical direction. In the overall analysis, 61 eyes (35.5%)were synclastic adjusted and 73 eyes (42.4%) were unadjusted in horizontal direction in the study group, with 64 eyes (54.2%)were synclastic adjusted and 29 eyes (24.6%) were unadjusted in the control group. In vertical direction, 95 eyes (55.2%)were synclastic adjusted and 50 eyes (29.1%) were unadjusted in the study group, with 78 eyes (66.1%) were synclastic adjusted and 20 eyes (16.9%) were unadjusted in the control group. In both two directions, percentage of synclastic adjusted eyes in the study group were less than that in the control group, while the percentage of unadjusted eyes in the study group were more.In unadjusted eyes of the study group, overall 61 eyes (83.6%)were within ±100 μm of Oculyzer topography guidance and 70 eyes (95.9%) were within ±140 μm in horizontal direction, and 46 eyes (92.0%) were within ±100 μm of Oculyzer topography guidance and 49 eyes (98.0%) were within ±140 μm in vertical direction.
The mean ratio of Cartesian coordinate in synclastic adjusted eyes in the study group (dxmanu/dxocuof 0.78±0.48, dymamu/dyocuof 0.61±0.42) were similar with which in the control group (dxauto/dxocuof 0.79±0.66, dyauto/dyocuof 0.66±0.65) in both direction. There was no statistically significant difference between two groups (P=0.951, 0.621).
Figures 6 and 7 showed two scatterplot of actual values versus Oculyzer topography-guided data in synclastic adjusted group.In horizontal direction, the correlation coefficient of actual values (dxmanu) and Oculyzer topography-guided data (dxocu)in the study group (R=0.871, P=0.000) was higher than that in the control group (R=0.709, P=0.000). While in vertical direction, the correlation coefficient of actual values (dymanu)and Oculyzer topography-guided data (dyocu) in the study group (R=0.428, P=0.000) was lower than which in the control group (R=0.549, P=0.000).
Table 2 Comparison of visual and refractive outcomes between two groups postoperatively mean±SD
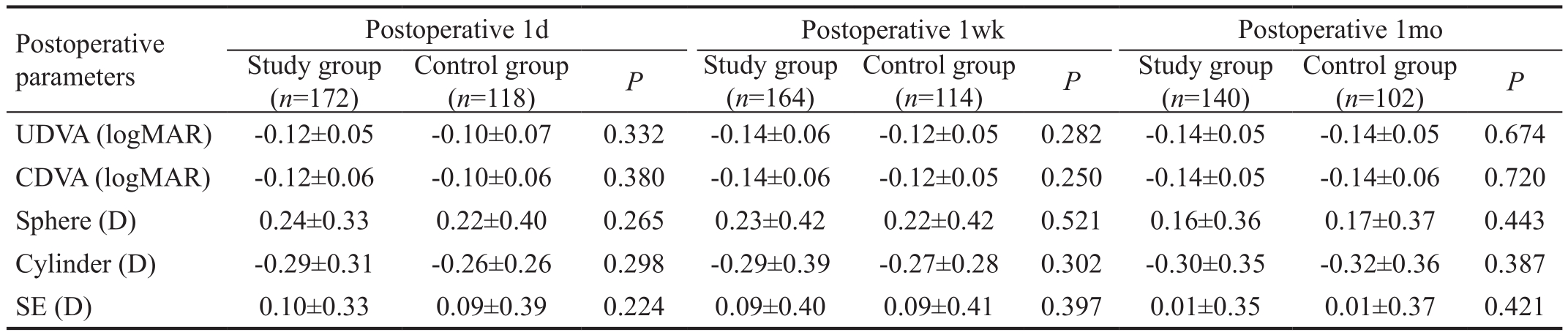
UDVA: Uncorrected distance visual acuity; CDVA: Corrected distance visual acuity; SE: Spherical equivalen.
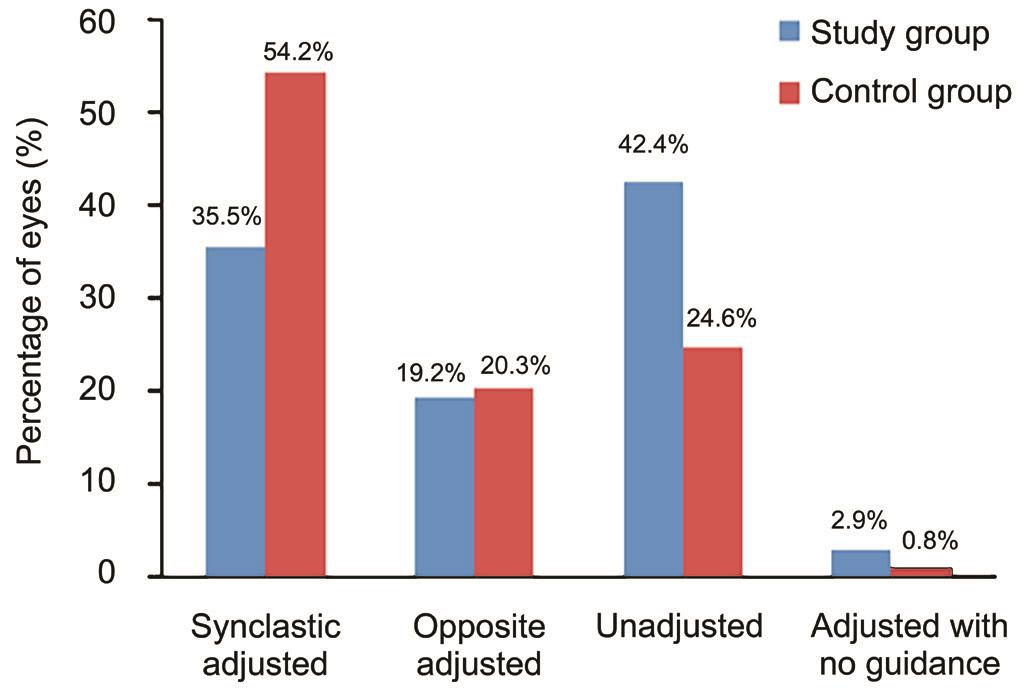
Figure 4 Comparison of percentage of eyes in four groups between the study group and the control group in horizontal direction.
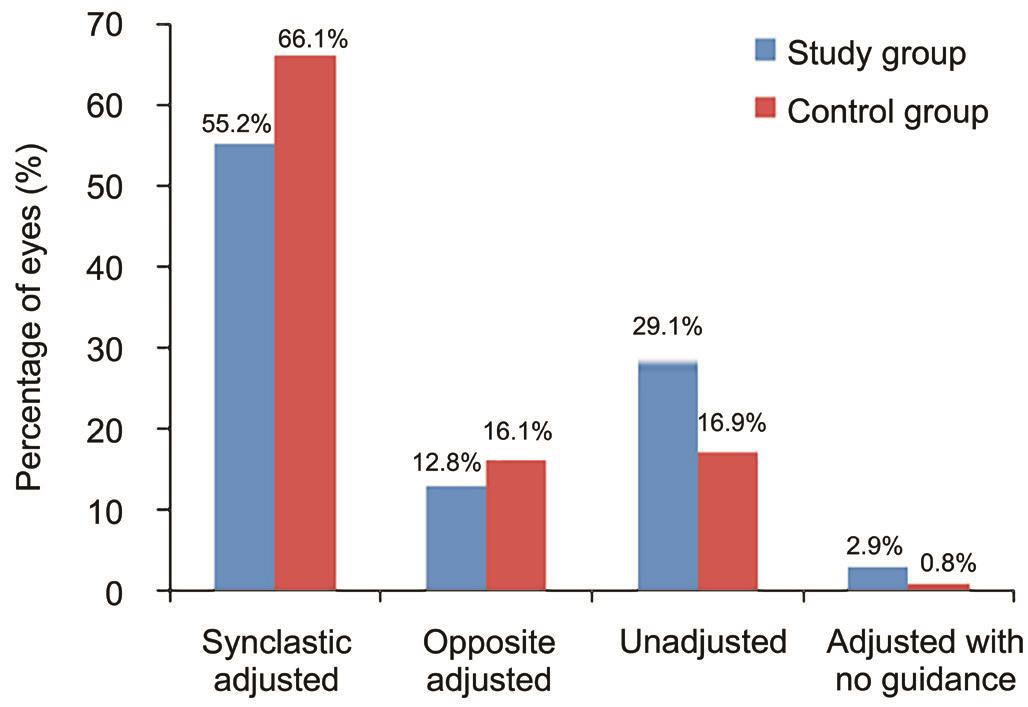
Figure 5 Comparison of percentage of eyes in four groups between the study group and the control group in vertical direction.
DISCUSSION
Research showed that the accuracy of refractive outcomes was highly correlated with the precise alignment of the ablation to the intended location on the cornea[19]. In addition, angle Kappa of eye is one of other vital factors causing misalignment in refractive surgery[20]. Arbelaez et al[6]also indicated the importance of measuring decentration values and adjusting them using the laser ablation algorithm.
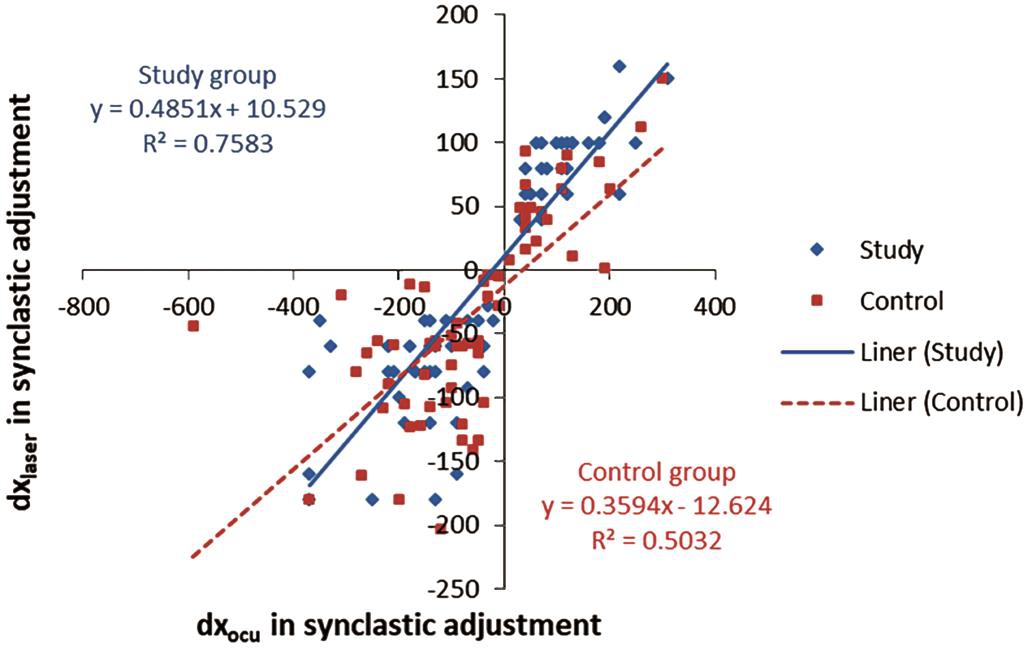
Figure 6 Actual values versus Oculyzer topography-guided data in synclastic adjusted group in horizontal direction.
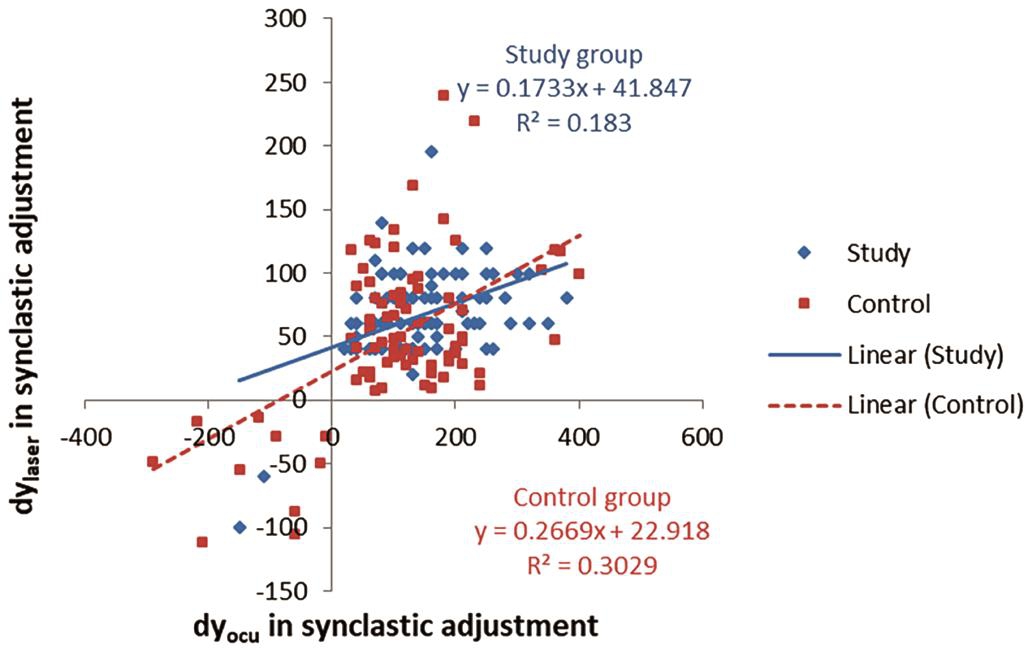
Figure 7 Actual values versus Oculyzer topography-guided data in synclastic adjusted group in vertical direction.
Oculyzer and Topolyzer Vario display X-Y Cartesian coordinates correlation between the corneal vertex and pupil center. When we focus on a target, the cornea vertex as a reproducible point is the highest point, nearing the line of sight and independent of pupil size. If the human optical system were coaxial, the intersection of the optical axis and the cornea is exactly the cornea vertex. The angle between optical and visual axes at the nodal point is termed the angle Alpha, which positively correlating with angle Kappa[6,12].
In this study, we compared the mean ratio of dxactual/dxocuand dyactual/dyocurespectively in synclastic adjusted eyes in the study and control groups, and found that there was no statistically significant difference between them. In addition, correlation analysis between actual values and Oculyzer topographyguided data yielded a substantial correlation in both groups in horizontal and vertical direction. And there was not significant difference between the study and control group in correlation coefficient. Meanwhile, the visual and refractive outcomes were similar between two groups in at 1d, 1wk and 1mo postoperatively.
Not all lasers have specific software and/or hardware to automatically adjust for decentration from angle Kappa, and the image obtained from corneal topography may fail to match with the live image during surgery by excimer laser platform occasionally. To make an appropriate adjustment in ablation,analysis of preoperative topography guidance combined with intra-operative condition is of great importance for surgeon.In our clinic, it is evident that the effect of manually angle Kappa adjustment based on Oculyzer topography guidance is similar to automatically angle Kappa adjustment guided by Topolyzer Vario topography with WaveLight EX500 excimer laser. Therefore, such manually adjustment guided by Oculyzer topography is recommended in the condition of mismatch between Topolyzer Vario topography and the live image during surgery. However, pupil center shift compensation and cyclotorsion compensation are also important for the exact results of ablation in the eye with high myopia and high myopic astigmatism[21-22], therefore, the successful rate of diagnostic image match with live image based on Topolyzer Vario guidance should be improved and be recommended in order to achieve more accurate data, especially the angle of cyclotorsion.
The retrospective design and small sample may be viewed as the limitations of this study. Another limitation is that only myopic patients were incorporated in this study, whose decentration values were low and unobvious compared with hyperopic patients. Till now, topography-guided excimer laser ablation (T-CAT) for hyperopia has been commonly used in our clinic with perfect centration ablation to compensate the large angle Kappa for hyperopic eyes. While, prospective studies including T-CAT for hyperopic patients would be investigated further.
In conclusion, this study demonstrated the high consistency in angle Kappa adjustment guided by Oculyzer topography and Topolyzer Vario topography. The data from Oculyzer topography makes significant sense when the image from Topolyzer Vario topography fails to match with the live image during surgery by WaveLight EX500 excimer Laser.
ACKNOWLEDGEMENTS
Authors’ contributions: Sun MS is responsible for data acquisition, data analysis, drafting manuscript and statistical analysis; Zhang L is responsible for data acquisition; Guo N and Song YZ are responsible for data analysis; Zhang FJ is responsible for the surgical procedure and protocol design, critical revision of manuscript, securing funding and supervision.
Foundation:Supported by 215 High Level Talent Fund of Beijing Health Government (No.2013-2-023).
Conflicts of Interest:Sun MS, None; Zhang L, None; Guo N,None; Song YZ, None; Zhang FJ, None.
REFERENCES
1 Tomita M, Watabe M, Yukawa S, Nakamura N, Nakamura T, Magnago T.Safety, efficacy, and predictability of laser in situ keratomileusis to correct myopia or myopic astigmatism with a 750 Hz scanning-spot laser system.J Cataract Refract Surg 2014;40(2):251-258.
2 Gazieva L, Beer MH, Nielsen K, Hjortdal J. A retrospective comparison of efficacy and safety of 680 consecutive LASIK treatments for high myopia performed with two generations of flying-spot excimer lasers.Acta Ophthalmol 2011;89(8):729-733.
3 Lubatschowski H. Overview of commercially available femtosecond lasers in refractive surgery. J Refract Surg 2008;24(1):S102-S107.
4 Soler V, Benito A, Soler P, Triozon C, Arne JL, Madariaga V, Artal P,Malecaze F. A randomized comparison of pupil-centered versus vertexcentered ablation in LASIK correction of hyperopia. Am J Ophthalmol 2011;152(4):591-599.e2
5 Prakash G, Agarwal A, Ashok Kumar D, Jacob S, Agarwal A.Comparison of laser in situ keratomileusis for myopic astigmatism without iris registration, with iris registration, and with iris registrationassisted dynamic rotational eye tracking. J Cataract Refract Surg 2011;37(3):574-581.
6 Arbelaez MC, Vidal C, Arba-Mosquera S. Clinical outcomes of corneal vertex versus central pupil references with aberration-free ablation strategies and LASIK. Invest Ophthalmol Vis Sci 2008;49(12):5287-5294.
7 Khalifa MA, Alsahn MF, Shaheen MS, Pinero DP. Comparative analysis of the efficacy of astigmatic correction after wavefront-guided and wavefront-optimized LASIK in low and moderate myopic eyes. Int J Ophthalmol 2017;10(2):285-292.
8 Lin HY, Zhang FJ, Chuang YJ, Lin PJ, Yu HC. Highlights for improving cyclotorsional eye-tracking success rate in femtosecond laserassisted LASIK with WaveLight EX500 excimer laser. J Emmetropia 2016;7(2):85-93.
9 Lazaridis A, Droutsas K, Sekundo W. Topographic analysis of the centration of the treatment zone after SMILE for myopia and comparison to FS-LASIK: subjective versus objective alignment. J Refract Surg 2014;30(10):680-686.
10 Arba-Mosquera S, de Ortueta D. LASIK for hyperopia using an aberration-neutral pro file with an asymmetric offset centration. J Refract Surg 2016;32(2):78-83.
11 de Ortueta D, Arba-Mosquera S. Laser in situ keratomileusis for high hyperopia with corneal vertex centration and asymmetric offset. Eur J Ophthalmol 2017;27(2):141-152.
12 Park CY, Oh SY, Chuck RS. Measurement of angle kappa and centration in refractive surgery. Curr Opin Ophthalmol 2012;23(4):269-275.
13 Moshirfar M, Hoggan RN, Muthappan V. Angle Kappa and its importance in refractive surgery. Oman J Ophthalmol 2013;6(3):151-158.
14 Qi H, Jiang JJ, Jiang YM, Wang LQ, Huang YF. Kappa angles in different positions in patients with myopia during LASIK. Int J Ophthalmol 2016;9(4):585-589.
15 Reinstein DZ, Gobbe M, Gobbe L, Archer TJ, Carp GI. Optical zone centration accuracy using corneal fixation-based SMILE compared to eye tracker-based femtosecond laser-assisted LASIK for myopia. J Refract Surg 2015;31(9):586-592.
16 Chang DH, Waring GO IV. The subject-fixated coaxially sighted corneal light reflex: a clinical marker for centration of refractive treatments and devices. Am J Ophthalmol 2014;158(5):863-874.
17 Schwiegerling JT. Eye axes and their relevance to alignment of corneal refractive procedures. J Refract Surg 2013;29(8):515-516.
18 Khakshoor H, McCaughey MV, Vejdani AH, Daneshvar R, Moshirfar M. Use of angle kappa in myopic photorefractive keratectomy. Clin Ophthalmol 2015;9:193-195.
19 Neuhann IM, Lege BA, Bauer M, Hassel JM, Hilger A, Neuhann TF. Static and dynamic rotational eye tracking during LASIK treatment of myopic astigmatism with the Zyoptix laser platform and Advanced Control Eye Tracker. J Refract Surg 2010;26(1):17-27.
20 Okamoto S, Kimura K, Funakura M, Ikeda N, Hiramatsu H, Bains HS.Comparison of myopic LASIK centered on the coaxially sighted corneal light reflex or line of sight. J Refract Surg 2009;25(10 Suppl):S944-S950.
21 Arba Mosquera S, Verma S. Effects of torsional movements in refractive procedures. J Cataract Refract Surg 2015;41(8):1752-1766.
22 Prickett AL, Bui K, Hallak J, Bakhtiyari P, de la Cruz J, Azar DT,Chamon W. Cyclotorsional and non-cyclotorsional components of eye rotation observed from sitting to supine position. Br J Ophthalmol 2015;99(1):49-53.