INTRODUCTION
Childhood glaucoma encompasses heterogeneous groups of diseases ranging from primary congenital glaucoma(PCG) to different acquired conditions. They may present with solely ocular involvement or as a part of a syndrome with multiple system involvements[1]. However, it seems that they all share a common pathway of pressure associated damage to the eye with possible blindness. The visual outcome of childhood glaucoma is determined by the stage at presentation,the establishment of the diagnosis of glaucoma and its etiology,the time of the intervention and the follow up[2].
In developing countries, there is usually a delay in the discovery of affected children owing to illiteracy among the general population along with limited facilities for appropriate assessment. Thus, the burden of childhood glaucoma in the Middle East and developing countries is so far high. The prevalence of blindness among children in the developing world is estimated to be 0.051% accounting for 3.9% of the total blindness worldwide. This percentage is predicted to continue its rise unless serious measures are taken[3].
A critical step to build up plans for future intervention programs is to understand the distinctive pattern of childhood glaucoma in our region and thereby define our needs. To establish a concrete baseline; there should be a single,consistent classification system agreed upon by different practitioners. Numerous classification schemes have been introduced, although none are broadly followed[4].
Recently, an international association of glaucoma specialists,the Childhood Glaucoma Research Network (CGRN),proposed a simple and logical framework for both diagnosis and classification of childhood glaucoma. Their aim was to populate a classification that comprises every cause of childhood glaucoma not only the most common ones[5].
The main purpose of this study was to analyze childhood glaucoma regarding its demographics, presentations, different causes and surgical modalities used among patients presenting to Mansoura University Ophthalmic Center (one the chief referral centers for eye care in Egypt). Another goal of this study was to apply the CGRN classification retrospectively and evaluate its convenience for further incorporation into ongoing clinical and research work.
SUBJECTS AND METHODS
Study Design and Setting We utilized retrospective, medical record review method in obtaining patient data between July 2014 and September 2017 from the Mansoura Ophthalmic Center, Mansoura University, Egypt, which served pediatric patients from all over the Dakhelia government.
An approval from the Ethical Committee of Mansoura University was obtained (code number R\17.09.21), which was adhered to the Declaration of Helsinki. Information on participating physicians remains confidential. No surgeon-tosurgeon data comparisons were performed.
Selection of Patients Patients eligible for the study were children younger than 16 years old (according to UK-European)diagnosed with glaucoma with available complete medical records. Records with incomplete data were excluded from the study.
Data Collection Clinical rosters were reviewed retrospectively to obtain demographic and clinical data including age, gender,laterality and glaucoma type. Visual acuity (VA), refraction,intraocular pressure (IOP), corneal diameter and cup-disc ratio were obtained both at the time of presentation and at the final visit for patients with multiple visits. Follow up period was the difference between the first and the last visit of given patient.The number and type of both antiglaucomatous drugs (AGD)and glaucoma surgeries were obtained. IOP was measured in young and uncooperative children under inhalation anesthesia with sevoflurane (Sevorane) using Tonopen in the intial phase of anesthesia. In older and cooperative patients,Goldman applanation tonometer was used in measuring the IOP. Cup-disc ratio was examined by direct and indirect ophthal moscope. Corneal diameter was measured horizontally(white to white) by calipers. VA was measured using fixation methods or Cardiff cards in preverbal children and using Snellen’s chart in older verbal patients converted into decimal notation. Only Snellen’s VA results were used in the follow up measures, divided as follows: good VA 0.5 or better, moderate VA from 0.1 to 0.5, and poor VA less than 0.1. Cycloplegic refraction was performed after instillation of cyclopegic agent (cyclopentolate 0.5%) three times, 10min apart within 30min before retinoscopy, confirmation of refraction was done by handheld autorefractometer in younger children(Righton Retinomax K-Plus 2, Tokoyo, Japan) and with autorefractometer (Huvitz-Hannover, Germany) in older children.
Table 1 CGRN definition of glaucoma[5]
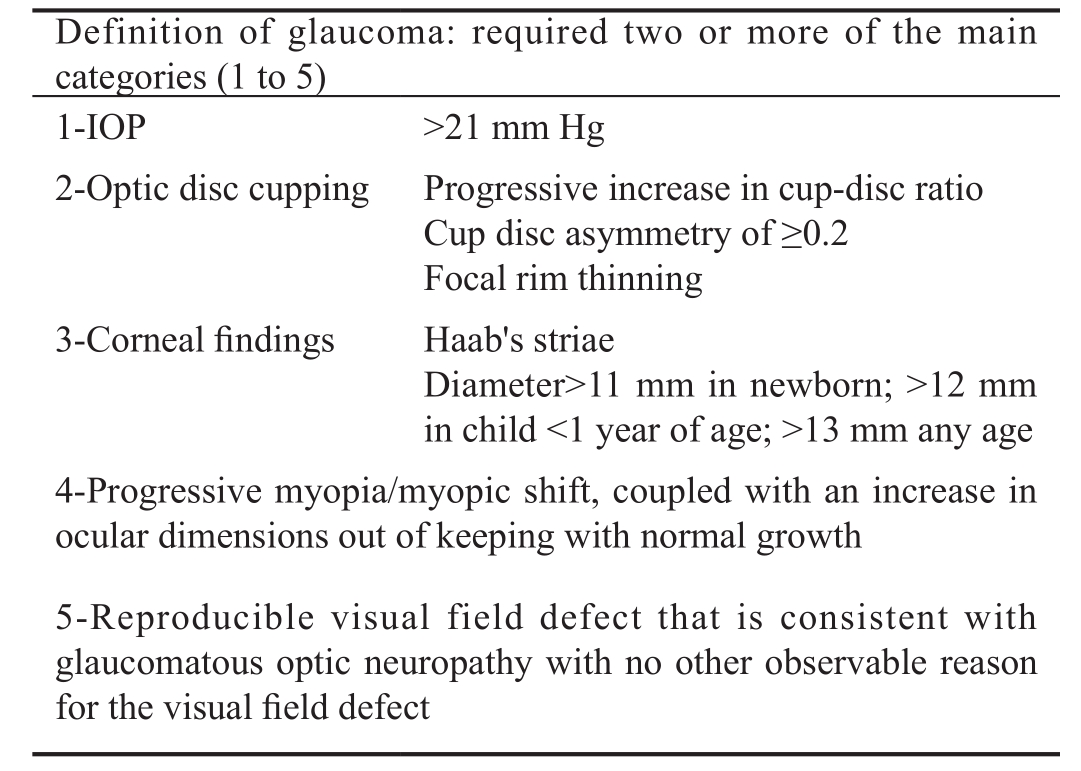
CGRN: Childhood Glaucoma Research Network; IOP: Intraocular pressure.
All the patients diagnosed with glaucoma in our records met the criteria defined by CGRN (Table 1). The patients were then classified into two main groups: primary, defined as idiopathic glaucoma in children younger than 3y and secondary,when glaucoma is due to ocular or systemic disorder either congenital or acquired[5].
Primary childhood glaucoma included PCG and juvenile open angle glaucoma (JOAG). PCG was subclassified according to the age of the onset of the disease into newborn onset(0-1mo), infantile onset (>1-24mo) and late onset (>2y).JOAG represents children with primary glaucoma with no buphthalmos. Secondary childhood glaucoma included,glaucoma associated with non-acquired systemic disease or syndrome, glaucoma associated with non-acquired ocular anomalies, glaucoma associated with acquired conditions, and glaucoma following cataract surgery. No glaucoma suspect was enrolled in this study.
Statistical Analysis Data were analyzed with SPSS software(version 20.00, SPSS, Chicago, IL, USA). Qualitative datawere described using numbers and percentages. Quantitative variables were tested for normality distribution using Shapiro-Wilk test. Parametric data were presented as mean±standard deviation (SD) for and non-parametric data were presented as median (min-max). The six groups’ main variables were compared by one way analysis of variance (ANOVA) test followed by post-hoc tests with Bonferroni’s correction for the pairwise comparison between the groups (P value <0.008 was defined as a statistical significance after Bonferroni’s adjustment). P value ≤0.05 was considered statistically significant in other tests.
Table 2 Demographic data for the studied patients
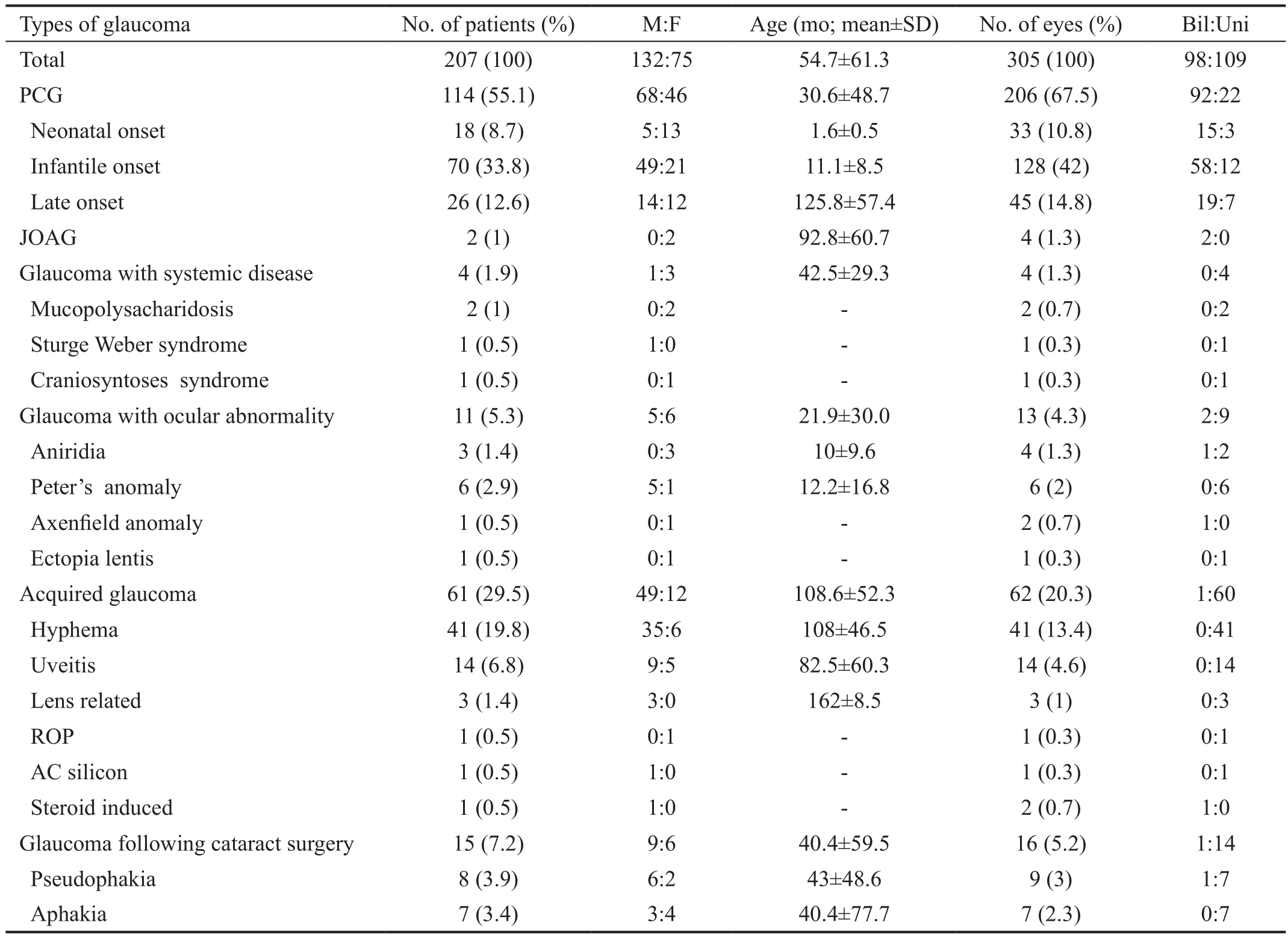
PCG: Primary congenital glaucoma; JOAG: Juvenile open angle glaucoma; M:F: Male to female ratio; SD: Standard deviation; Bil:Uni:Bilateral:unilateral; ROP: Retinopathy of prematurity; AC: Anterior chamber.
RESULTS
Demographic Data A total of 305 eyes of 207 patients’records were included in this survey. These were records with complete medical data reviewed in the specified period. PCG was the most common diagnosis accounted for 55.1% of all the patients, followed by secondary acquired glaucoma which comprised 29.5%. The prevalence of PCG was 2.36 per 10 000 live births (calculated after retrieving the number of births in Dakahelia government corresponding to the period of the study). Males represented 63.8% of the whole studied patients.Although, no significant difference between unilateral (52.7%)and bilateral cases (47.3%) was noted, the majority of patients had unilateral involvement, except patients diagnosed with primary glaucoma. The oldest age was seen in acquired group(mean age 108.6±52.3mo) and the youngest age was seen in glaucoma associated with ocular abnormalities (mean age 21.9±30.0mo) (Table 2, Figure 1).
Baseline Clinical Findings Table 3 gives details about the initial clinical findings among the groups. The median IOP of all the studied eyes was 29 mm Hg (range 19-43 mm Hg).There was a statistically significant difference regarding the IOP with the highest value in glaucoma associated with systemic disease group (P=0.003). There was statistically significant difference in the horizontal corneal diameter;the shortest mean was recorded in the post cataract group(10.4±0.5 mm). Also the difference was significant regarding cup-disc ratio the highest was in the PCG group (0.57±0.12,P<0.0005). Data regarding baseline VA and refraction was not complete and thereby was not statistically compared between groups.
Baseline Clinical Presentation Corneal enlargement comprised 98.0% of the parents’ complaint in neonatal and infantile onset PCG, while corneal haziness was the mostfrequent complaint in late onset PCG (88.0%). Two patients(4 eyes) previously diagnosed in the records as late onset PCG were reclassified to the term JOAG according to CGRN definition, with decreased VA as the chief complaint (97.0%)in this group. Glaucoma in the patients with systemic disease was discovered after referral from the pediatrician for routine ophthalmic examination with no ocular symptoms. Corneal opacification was the chief complaint (54.5%) in patients with glaucoma associated with ocular anomaly. The most common diagnosis in the acquired glaucoma was hyphema(65.6%). The chief complaint was headache and eye pain(78.0%). Glaucoma in all cases in the post cataract group was discovered during routine postoperative follow up. The mean interval between cataract surgery and diagnosis of glaucoma was 2±0.68mo (range 1-3mo).
Table 3 The baseline clinical findings of the studied patients mean±SD (min-max)
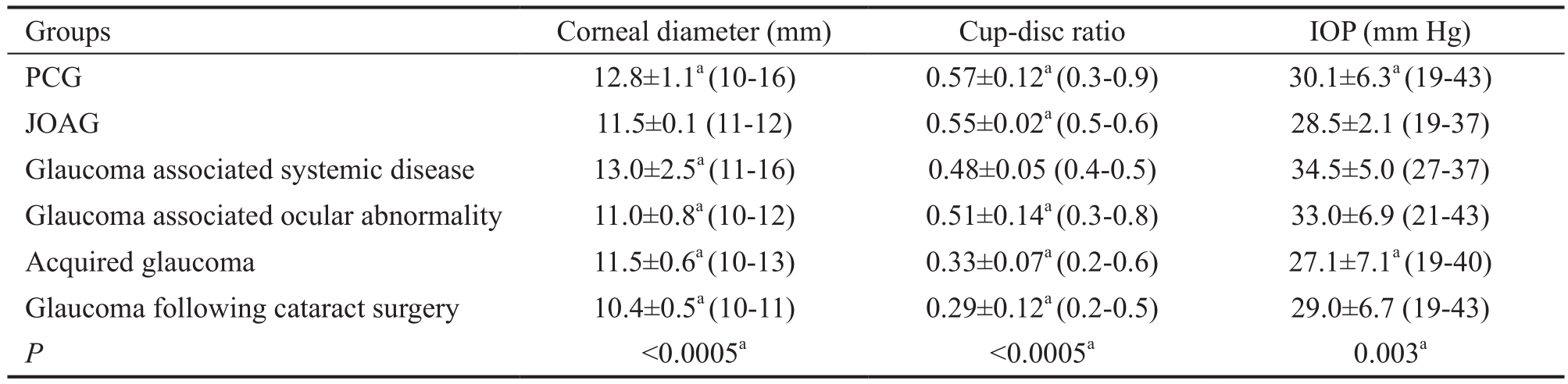
PCG: Primary congenital glaucoma; JOAG: Juvenile open angle glaucoma; IOP: Intraocular pressure.aP<0.008 was significant.
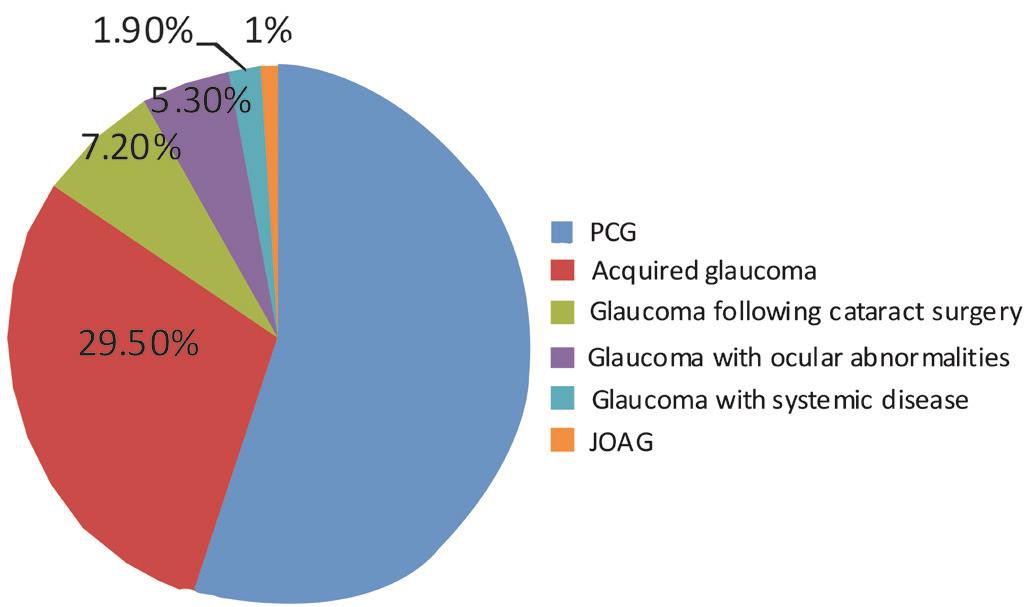
Figure 1 Different types of childhood glaucoma according to their prevalence.
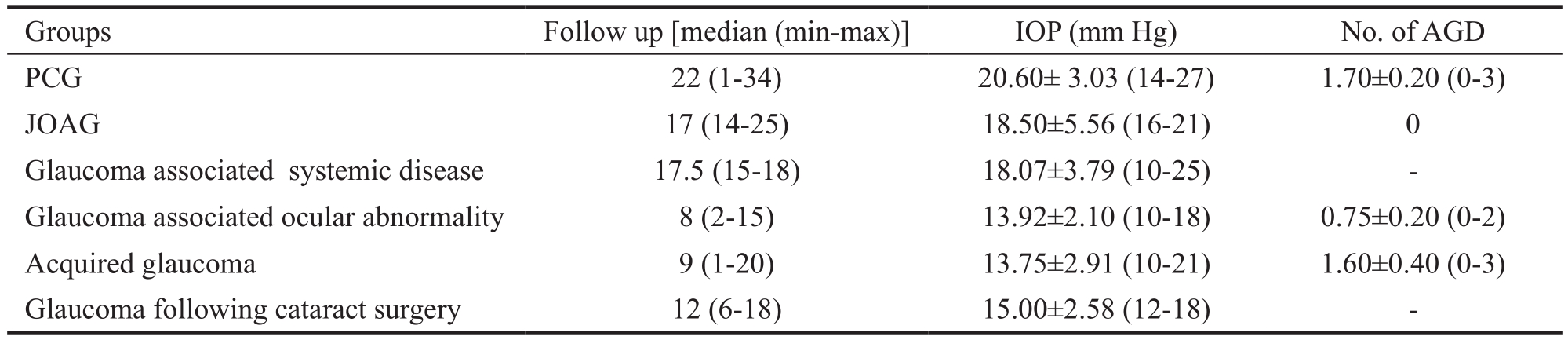
Treatment Figure 2 displays the frequency of different modalities of treatment among the whole studied groups.Primary surgical intervention was reported in 258 eyes (84.6%)of the total included eyes with 46 eyes (15.1%) required resurgery. Combined trabeculotomy-trabeculectomy was the most frequent operation accounts for 34.5% (89 of 258) of all primary surgeries. Trabeculotomy alone was performed in 77 (30.0%) eyes. Ahmed glaucoma valve (AGV) implantation comprised 87.0% of the secondary surgeries. Antiglaucomatous medications were used alone in 47 eyes (15.4%)and as augmentation after surgeries in 109 eyes (35.7%)from the total studied eyes. Topical beta-blockers, carbonic anhydrase inhibi tors (CAIs) and prostaglandin analogs were the most frequent drops prescribed, while systemic CAIs were used in limited number of cases.
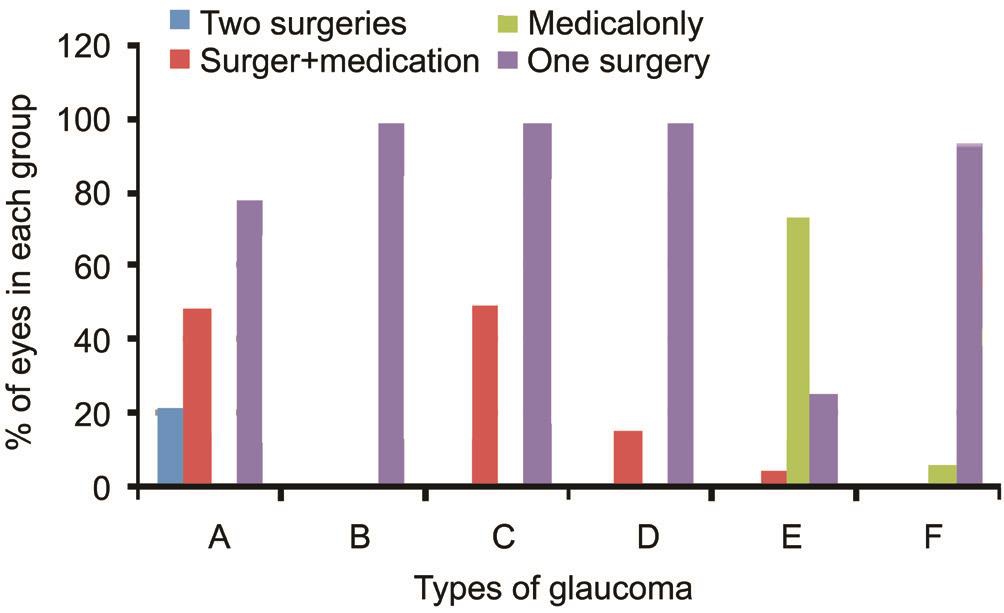
Figure 2 Percentage of different treatment approaches among groups A: PCG; B: JOAG; C: Glaucoma associated with systemic disease; D: Glaucoma associated ocular anomality; E: Acquired glaucoma; F: Glaucoma following cataract surgery.
Follow-up Results
Primary congenital glaucoma Surgical intervention was required in all the cases of this group. Combined trabeculotomytrabeculectomy was the most common operation carried in 82 eyes (40.0%), followed by trabeculotomy alone in 73 (35.4%)eyes. Augmented subscleral trabeculectomy (SST) was done in 37 eyes (18.0%) and primary AGV was implanted in 14 eyes (6.7%). Secondary AGV implantation was performed in 45 (21.8%) eyes. Augmented AGD was reported in 102 eyes(49.5%) either beta-blocker 0.5% alone or combined betablocker and CAIs eye drops with 1.7 mean number of AGD in the final visit.
Juvenile open angle glaucoma Surgical intervention was required in all the cases of this group. Combined trabeculotomytrabeculectomy and trabeculotomy alone were carried equally in this group (2 eyes for each surgery).
Glaucoma associated with systemic disease Augmented SST was performed in all the cases. Combined topical betablocker and CAIs were used in 2 eyes (50.0%).
Glaucoma associated with ocular abnormality Augmented SST was done in 11 eyes (84.6%) and primary AGV in 2 eyes(15.4%). Medical treatment was used postoperative in 2 eyes(15.4%).
Table 4 Clinical data at last visit in each group mean±SD (min-max)
IOP: Intraocular pressure; SD: Standard deviation; AGD: Antiglaucomatous drugs; PCG: Primary congenital glaucoma; JOAG:Juvenile open angle glaucoma.
Table 5 Final visual and refractive outcome among the groups
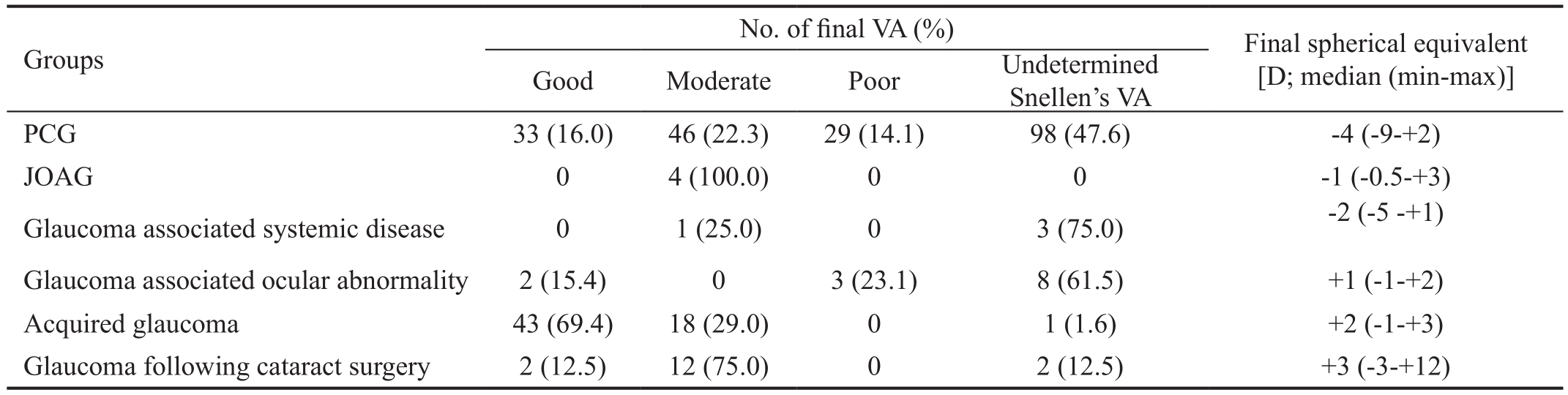
VA: Visual acuity; SD: Standard deviation; PCG: Primary congenital glaucoma; JOAG: Juvenile open angle glaucoma.
Acquired glaucoma Antiglaucoma medications were the most common primary treatment reported in 46 eyes (74.2%)while 3 eyes (4.8%) required postoperative medications.Augmented SST was performed in 7 eyes (11.3%), SST in 5 eyes (8.1%), primary AGV in 4 eyes (6.5%) and secondary valve implantation in one eye (1.6%).
Glaucoma following cataract surgery Almost all eyes 15(93.75%) had surgical treatment except one eye (6.25%) was treated medically with one topical combination beta-blocker and CAIs drops. Combined trabeculotomy-trabeculectomy was performed in 5 eyes (31.25%), trabeculotomy in 2 eyes(12.5%), augmented SST in 2 eyes (12.5%) and primary AGV in 6 eyes (37.5%). Table 4 gives details about final IOP, and number of AGD obtained from the last visit.
As regard the final visual outcome, Table 5 demonstrates the VA obtained from the last visit. Acquired glaucoma group had the highest percent of eyes (69.4%) with good VA, while glaucoma associated with ocular anomaly group had the highest percent of eyes (23.1%) with poor VA. Most of the patients in PCG showed myopic values. Eyes with glaucoma following cataract surgery demonstrated the widest range of refraction. Most of the patients in glaucoma associated with ocular abnormality could not be refracted.
DISCUSSION
Childhood glaucoma is a demanding blinding disease. Clinicbased reports in our region have documented the prevalence of blindness from glaucoma in 2002 to be 12.1%. Unfortunately two thirds (65.5%) of this total number experienced blindness before the age of 10y[6].
In the current study, we analyzed the pattern of childhood glaucoma among patients presented to the Ophthalmic Center, Mansoura University with the rationale of obtaining reliable data using an international consensus newly proposed glaucoma classification system (CGRN)[5].
As an initial step, we implemented the CGRN classification to the obtained medical records. Patients were categorized into six groups with high level of convenience without overlap. At this point of the study, the CGRN system had highlighted one of the drawbacks of our recording system, which was lacking reports for glaucoma suspect patients. These patients are usually managed in the outpatient clinics without admission files.
The term JOAG was somewhat confusing as we usually apply this term on patients diagnosed with primary open angle glaucoma before the age of 40y, especially those with positive family history[7]. After revising the patients’ records,the diagnosis of 2 cases was shifted from ‘late-onset PCG’ to JOAG to follow the CGRN classification.
Scrutinizing our results regarding different types of childhood glaucoma disclosed the predominance of the PCG accounting for 55.1% of the total studied eyes. This was followed by acquired glaucoma representing 29.5% with the traumatic hyphema affiliating the major acquired etiology (66.0%). The latter result was consistent with previous studies, nominating trauma as a major cause of childhood glaucoma[2,6,8]. This draws the attention towards the essence of strictly following children after ocular trauma and the importance of screening for possible glaucoma development in those patients.
PCG was also the most prevalent diagnosis in large numbers of studies[8-11]. Different finding was reported in a populationbased study conducted by Aponte et al[2]over 40y period in a defined population in the United States, where acquired glaucoma was the most prevalent type of childhood glaucoma,comprising more than 63% of cases younger than 20 years old.Over the specified period in our study, the prevalence of PCG was estimated to be 2.36 per 10 000 live births. This was higher than the incidence reported by the British infantile and childhood glaucoma eye study in Britain (0.541 per 10 000)[12], and tremendously higher than the reported incidence in Olmsted,USA, which is considered the lowest incidence compared with all the prior reports (0.146 per 10 000)[2]. We can attribute this difference to the high rate of parental consanguinity encountered in our community[13]. While our incidence is not a nation-wide figure, but it is supported by previous reports assigning PCG being more frequent in communities with more habitual consanguineous marriages, as in Saudi Arabia[14]and India[15].On reviewing the demographic characteristics of the patients in this study, 63.8% of affected patients were male. Male predominance is consistent with previous reports in the literature[8-9]. Genetic basis could provide a clue for this impressive gender bias, yet not proven[16].
Clinical data collected in our study showed that both enlargement and haziness of the cornea were the most frequent finding (98.0% and 88.0% respectively) in PCG motivating parents to seek medical advice. Therefore, it was not unusual that these children were more likely to present earlier than children with secondary glaucoma who were mainly detected through routine follow-up. This raises the importance to have general practitioners familiar with the relevant signs of the disease to ensure that the diagnosis of primary childhood glaucoma will not be missed in the first year of life[8].
As regards the baseline clinical signs, the shortest corneal diameter was reported in the post cataract surgery group(10.4±0.5 mm). It may be related to the fact that eyes of infants with congenital cataract have a smaller corneal diameter compared to controls[17]. Also, pediatric cataract surgery has been assumed to interfere with the normal ocular growth. Moreover,the glaucoma in these eyes is usually discovered early owing to the scheduled follow up visits after the cataract surgery[17].In our study, the median IOP of all the studied eyes was 29 mm Hg higher than that reported by Fung et al[8]in their survey(average<21 mm Hg). This might be related to the late presentation in our community, as most of the cases were discovered late in the course of the disease. Other factors are well known to affect the IOP reading, especially in children, as the anesthetic drug used during measurement[18], the instrument used[19], the axial length[20]and the degree of corneal edema[21].All may contribute to the difference between the IOP results between different studies[17].
Management of childhood glaucoma is usually attained at specialist centers. Combined trabeculotomy-trabeculectomy was the commonest primary surgery in our study, especially in primary glaucomas (34.5%). Trabeculotomy alone was performed in 77 eyes almost all with primary glaucoma.Augmented trabeculectomy was practiced in a small percent of the cases especially in the secondary glaucomas. In contrast,goniotomy was the commonest procedure, performed in 71% of primary cases in the British survey while combined trabeculotomy-trabeculectomy comprised only 16% of primary cases[12]. Owing to the late presentation of our patients,goniotomy was not included in the repertoire of our surgical management. It would be hindered by the corneal edema frequently present in our patients[22]. Trabeculotomy accounts for 86.0% of the total surgeries followed by tube shunt surgeries in the survey published by Fung et al[8]. In their study,combined trabeculotomy-trabeculectomy was not recorded.Trabeculectomy was the surgery of choice in the acquired glaucoma group in our study, this is consistent with the results of the British survey[12].
About 15.0% of the enrolled eyes in our study required more than one surgery. Ahmed valve implantation was performed in 87.0% of the eyes requiring re-surgery. Higher percent of re-surgery was reported in the British survey, where 50% of eyes required a second operation within the first postoperative year[12].
Surgery is considered the foundation management for childhood glaucoma[23], yet medication still plays an important role. More than half of patients in this study (51.4%) received glaucoma medications. The majority of those patients had previous surgeries and need augmentation. Meanwhile,medical treatment was the first-line in acquired glaucoma.Topical combination of carbonic anhydrase inhibi tors and betablockers was the most frequent drops prescribed. Similarly,about 70.0% of the patients required medical treatment,sometimes more than one type in the study by Fung et al[8].This emphasizes the importance of the appropriate use of medications with awareness of their unique adverse effects in this young age group[23].
As regard VA assessment, relevant data for the baseline and final VA was deficient owing to very young age group and the presence of photophobia that was common among the patients in our study. Similarly, the baseline refractive data was irrelevant. Preoperative refraction was hindered by the corneal edema, corneal opacity and in some cases, the presence of hyphema and hypopyon. VA was not included in the criteria for success rates in many studies since the mean age of the patients included is usually too young to obtain dependable results[12,24-25].
In the current study, there was an observable drop in the final IOP means in all the studied groups. However owing to the different points of follow-up in the records, no statistical significant results could be calculated.
Limitations and Recommendations The present study,according to our knowledge, is the first in our region to include this large number of childhood glaucoma patients,studying them from different aspects and applying a new classification system. However, there were some limitations.As most epidemiological studies, our study was limited to the demographics in a particular region at a specified period.Though probably representative of the pediatric population,we recommend extrapolating this work all over our nation.Despite being a referral center, we assume that our results give an image about the childhood glaucoma profile in Egypt since our institution is one of the major referral centers serving patients from different regions.
As a limitation of a retrospective study, some information was missing from our records as the ocular axial length and the corneal thickness. Also, records of glaucoma suspects were not available. We hope this study will trigger the establishment of more reliable recording systems in our community.
Registration of childhood glaucoma adds baseline data about the unique pattern of the disease in our community. PCG is the commonest form of childhood glaucoma. Secondary glaucoma in pediatric patients has distinguished etiologies, with the ocular anomalies and systemic diseases having a higher percentage of childhood glaucoma than in the adults. Applying uniform definitions and classifications among practitioners is important to conduct community-based studies.
ACKNOWLEDGEMENTS
Conflicts of Interest:Mokbel TH, None; El Hefney E, None;Hagras SM, None; ALNagdy A, None; Badawi A, None;Kasem M, None; El Shaer SM, None.
REFERENCES
1 Durnian JM, Cheeseman R, Kumar A, Raja V, Newman W, Chandna A.Childhood sight impairment: a 10-year picture. Eye (Lond) 2010;24(1):112-117.
2 Aponte EP, Diehl N, Mohney BG. Incidence and clinical characteristics of childhood glaucoma: a population-based study. Arch Ophthalmol 2010;128(4):478-482.
3 Magnitude and Causes of Visual Impairment, 2004. World Health Organization, Geneva. November Fact Sheet N_282.
4 Yeung HH, Walton DS. Clinical classification of childhood glaucomas.Arch Ophthalmol 2010;128(6):680-684.
5 Beck A, Chang TC, Freedman S. Definition, classification, differential diagnosis. In: Weinreb RN, Grajewski A, Papadopoulos M, Grigg J, Freedman S,editors. Childhood Glaucoma. Amsterdam: Kugler Publications; 2013:3-10.
6 El-Gilany AH, El Fedawy S, Tharwat M. Causes of blindness and needs of the blind in Mansoura, Egypt. East Mediterr Health J 2002;8(1):6-17.
7 Kwun Y, Lee EJ, Han JC, Kee C. Clinical characteristics of juvenileonset open angle glaucoma. Korean J Ophthalmol 2016;30(2):127-133.
8 Fung DS, Roensch MA, Kooner KS, Cavanagh HD, Whitson JT.Epidemiology and characteristics of childhood glaucoma: results from the dallas glaucoma registry. Clin Ophthalmol 2013;7:1739-1746.
9 Qiao CY, Wang LH, Tang X, Wang T, Yang DY, Wang NL.Epidemiology of hospitalized pediatric glaucoma patients in Beijing Tongren Hospital. Chin Med J (Engl) 2009;122(10):1162-1166.
10 Hoguet A, Grajewski A, Hodapp E, Chang TC. A retrospective survey of childhood glaucoma prevalence according to Childhood Glaucoma Research Network classification. Indian J Ophthalmol 2016;64(2):118-123.
11 Al Obeidan SA, Dewedar A, Osman EA, Mousa A. The profile of glaucoma in a Tertiary Ophthalmic University Center in Riyadh, Saudi Arabia. Saudi J Ophthalmol 2011;25(4):373-379.
12 Papadopoulos M, Cable N, Rahi J, Khaw PT; BIG Eye Study Investigators. The British Infantile and Childhood Glaucoma (BIG) Eye Study. Invest Ophthalmol Vis Sci 2007;48(9):4100-4106.
13 Bayoumi NHL. Surgical management of primary congenital glaucoma in Egypt. J Egypt Ophthalmol Soc 2016;109:85-92.
14 Bejjani BA, Lewis RA, Tomey KF, Anderson KL, Dueker DK, Jabak M, Astle WF, Otterud B, Leppert M, Lupski JR. Mutations in CYP1B1,the gene for cytochrome P4501B1, are the predominant cause of primary congenital glaucoma in Saudi Arabia. Am J Hum Genet 1998;62(2):325-333.
15 Dandona L, Dandona R, Srinivas M, Giridhar P, Vilas K, Prasad MN,John RK, McCarty CA, Rao GN. Blindness in the Indian state of Andhra Pradesh. Invest Ophthalmol Vis Sci 2001;42(5):908-916.
16 Vithana EN, Aung T. Exploring the basis of sex bias in primary congenital glaucoma. J Ophthalmic Vis Res 2009;4(2):73-74.
17 Lambert SR. Changes in ocular growth after pediatric cataract surgery.Dev Ophthalmol 2016;57:29-39.
18 Blumberg D, Congdon N, Jampel H, Gilbert D, Elliott R, Rivers R, Munoz B, Quigley H. The effects of sevoflurane and ketamine on intraocular pressure in children during examination under anesthesia. Am J Ophthalmol 2007;143(3):494-499.
19 Zareei A, Razeghinejad MR, Nowroozzadeh MH, Mehrabi Y, Aghazadeh-Amiri M. Intraocular pressure measurement by three different tonometers in primary congenital glaucoma. J Ophthalmic Vis Res 2015;10(1):43-48.
20 Bruno S, Alain D, Anne G, Jean-François R. Evolution of axial length in congenital glaucoma. Invest Ophthalmol Vis Sci 2012;53(14):6766-6769.
21 Deol M, Taylor DA, Radcliffe NM. Corneal hysteresis and its relevance to glaucoma. Curr Opinion Ophthalmol 2015;26(2):96-102.
22 Mendicino ME, Lynch MG, Drack A, Beck AD, Harbin T, Pollard Z,Vela MA, Lynn MJ. Long-term surgical and visual outcomes in primary congenital glaucoma: 360 degree trabeculotomy versus goniotomy. J AAPOS 2000;4(4):205-210.
23 Papadopoulos M, Edmunds B, Fenerty C , Khaw PT. Childhood glaucoma surgery in the 21stCentury. Eye (Lond) 2014;28(8):931-943.
24 Qayyum A, Baloch RA. Trabeculotomy in primary congenital glaucoma. Pak J Ophthalmol 2014;30(3):125-128.
25 Guo C, Wu Y, Xu L, Li M, Wang Z, Ni N, Guo W. Evaluation of preoperative speed of progression and its association with surgical outcomes in primary congenital glaucoma patients: a retrospective study.BMC Ophthalmol 2017;17(1):170-175.