Change in foveal position based on age and axial length in high myopic eyes
Qian Zhang1, Kaddie Kwok Chen2,3, Wei-Feng Liu2, Guo-Fu Huang2
1Department of Ophthalmology, the Second Affiliated Hospital of Nanchang University, Nanchang 330000, Jiangxi Province,China
2Department of Ophthalmology, the Third Affiliated Hospital of Nanchang University, Nanchang 330000, Jiangxi Province,China
3Department of Ophthalmology, University of California San Francisco, San Francisco, CA 94143, USA
Abstract· AlM: To evaluate the influence of age and axial length (AL)on the position of the fovea in patients with high myopia (HM).· METHODS: ln this prospective study, 96 patients (186 eyes)with HM were consecutively recruited from the Third Affiliated Hospital of Nanchang University. DRl-OCT Atlantis, fundus imaging, and lOL Master were used in this study. Three indices were measured: the distance between the fovea and the optic nerve head (ONH) center (DFO),the vertical distance between the fovea and the horizontal line pass of the ONH center (VDFO), and the horizontal distance between the fovea and the vertical line pass of the ONH center (HDFO). These measurements were used to analyze the effects of different age groups (A1, A2, A3 groups) and AL (AL1, AL2, AL3, AL4 groups) on these indices.· RESULTS: The results showed that there was no statistical significance in DFO among the age and AL groups(F=0.46, 0.37; P=0.62, 0.76, respectively). ln HDFO, there was also no statistical significance among the age and AL groups (F=0.10, 0.48; P=0.90, 0.69, respectively). ln VDFO, however, the difference in the age and AL groups was statistically significant (F=3.21, 3.12; P=0.04, 0.02,respectively). Thus, VDFO were correlated with age and AL (r=0.21, 0.23, all P<0.01), while HDFO and DFO were not correlated with age and AL (r=0.30, P>0.05).· CONCLUSlON: ln high myopia, the foveal position changes mainly in the vertical direction along with factors of age and AL.
KEYWORDS: high myopia; foveal position; age; axial length
INTRODUCTION
Recent research shows that the occurrence of myopia is on a rising trend[1-3]. With the increasing prevalence of myopia, high myopia (HM) is becoming more commonly widespread as well[4-6]. The elongation of the eye axis in high myopia typically results in peripapillary atrophy, disc tilt,sub-foveal choroidal thinning, scleral thinning, and deformed eye structure[7-10]. Koh et al[11] showed that disc tilt, posterior staphyloma, and chorioretinal atrophy were associated with reduced visual acuity and that myopic-related changes of the optic disc and macula are commonly found in HM eyes,even at young ages. Accumulating evidence shows that age is another risk factor for myopic maculopathy, in which some of these changes are associated with reduced central visual function[12-15]. However, changes in the location of the fovea should not be overlooked, as it has not been reported yet whether the shift in the posterior pole affects the location of the fovea.
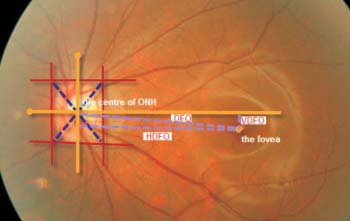
In this study, we analyze the effect of different ages and axial lengths (AL) on the foveal position by evaluating the position of the fovea relative to the center of the optic nerve head(ONH). With the ONH as the reference point, three indices were measured: the distance between the fovea and the ONH center (DFO), the vertical distance between the fovea and the horizontal line pass of the ONH center (VDFO), and the horizontal distance between the fovea and the vertical line pass of the ONH center (HDFO). These measurements, conducted by Topcon Atlantis DRI-OCT, were used to investigate the relationship between age and AL.
SUBJECTS AND METHODS
Subjects Patients with HM were consecutively recruited from the Third Affiliated Hospital of Nanchang University between May 2016 and February 2017. HM was defined as a lens correction of more than 6.0 diopters or an AL greater than 26 mm. In this study, subjects with an AL less than 26 mm were additionally included if they had a largecorneal curvature, as it results in a correction of more than 6.0 diopters. Exclusion criteria comprised of other ocular diseases that affected the position of the fovea. A total of 96 cases (186 eyes) were selected for this study: 62 females (123 eyes), 34 males (63 eyes), right eyes (94 eyes), and left eyes (92 eyes).The age range was from 7 to 81 (41.53±18.14) years old,and AL from 24.75 to 36.10 (28.76±2.61) mm. Participants obtained oral informed consent and not received any stipend.The study protocol was approved by the Institutional Review Board of the Third Affiliated Hospital of Nanchang University and complied with the tenets of the Declaration of Helsinki.
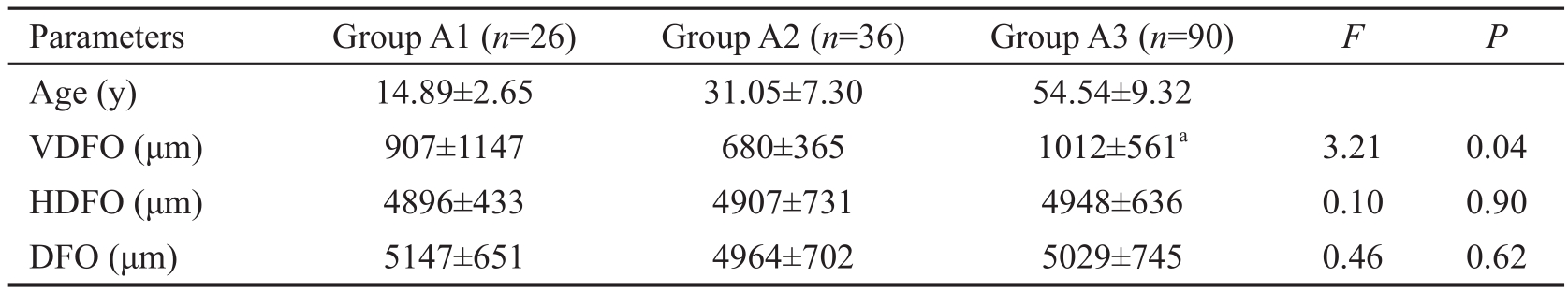
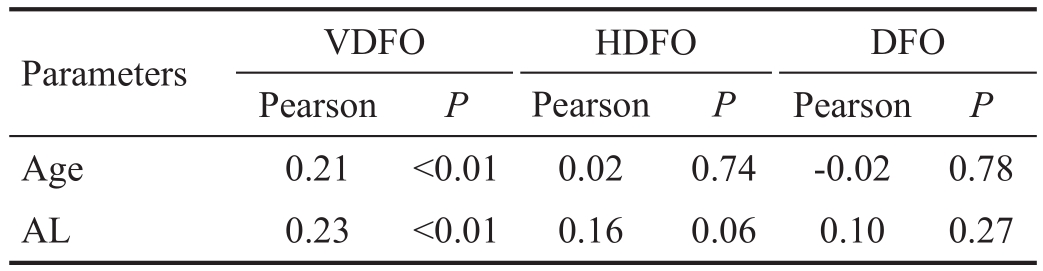
Table 1 Comparison of the foveal position in different age groups
aStatistical significance compared with group A2.
Parameters Group A1 (n=26) Group A2 (n=36) Group A3 (n=90) F P Age (y) 14.89±2.65 31.05±7.30 54.54±9.32 VDFO (μm) 907±1147 680±365 1012±561a 3.21 0.04 HDFO (μm) 4896±433 4907±731 4948±636 0.10 0.90 DFO (μm) 5147±651 4964±702 5029±745 0.46 0.62
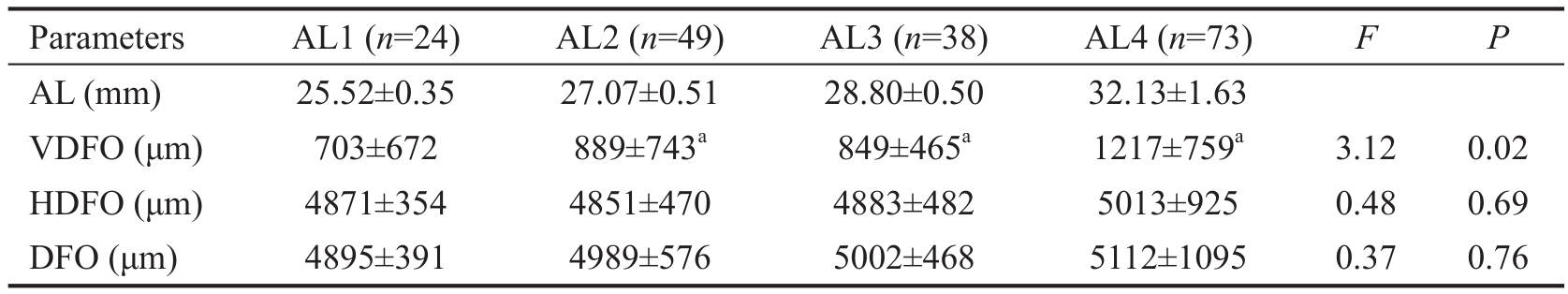
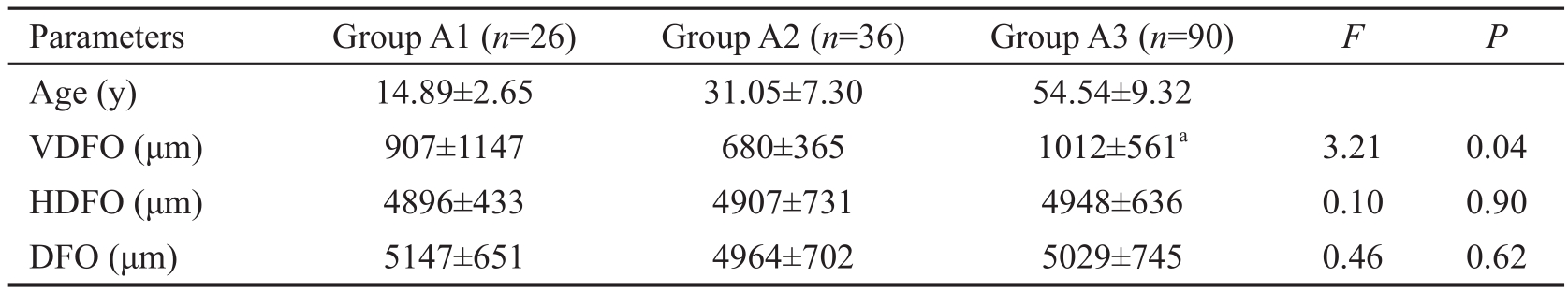
Table 2 Comparison of AL to the horizontal and vertical changes in the foveal position
aStatistical significance with AL1.
Parameters AL1 (n=24) AL2 (n=49) AL3 (n=38) AL4 (n=73) F P AL (mm) 25.52±0.35 27.07±0.51 28.80±0.50 32.13±1.63 VDFO (μm) 703±672 889±743a 849±465a 1217±759a 3.12 0.02 HDFO (μm) 4871±354 4851±470 4883±482 5013±925 0.48 0.69 DFO (μm) 4895±391 4989±576 5002±468 5112±1095 0.37 0.76
Position of the Fovea Topcon DRI-OCT Atlantis was utilized, using the 12 mm×9 mm scan mode to capture OCT images. We used three indices to accurately determine the position of the fovea. As seen in Figure 1, the position of the fovea and the ONH was determined using HDFO (long violet line), VDFO (short violet line), and the calculation of DFO(DFO2=HDFO2-VDFO2).
Refractive Error Patients (<18 years of age) were examined retinoscopically following an instillation of three drops of tropicamide 0.5%, which were instilled at 5-min intervals.After the instillation of the third drop (>30min), subjective refraction was performed. Patients >18 years of age were examined directly using subjective refraction.
Axial Length Measurement IOL Master (Carl Zeiss Meditec, USA) was used to measure the AL for 5 times. The average was taken, and if there was a deviation within the 5 measurements, the datum was not used in the study.
Grouping Method Age groups (A1, A2, and A3) were divided by age range: ≤18y, >18 to ≤40y, and >40y, respectively. AL groups (AL1, AL2, AL3, AL4) were determined by length:≤26 mm, 26.01 mm to ≤28 mm, 28.01 mm to ≤30 mm, and>30 mm, respectively.
Statistical Analysis Descriptive analyses of the data were undertaken by using SPSS 16.0 software (SPSS, Inc., Chicago,IL, USA). A one-way analysis of variance (ANOVA) and a correlation analysis of the statistical methods were used. A P value of less than 5% was considered statistically significant.
RESULTS
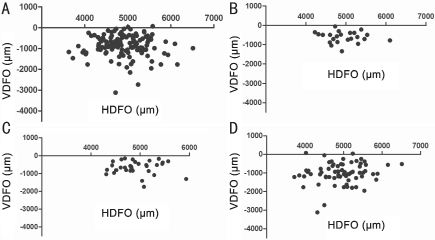
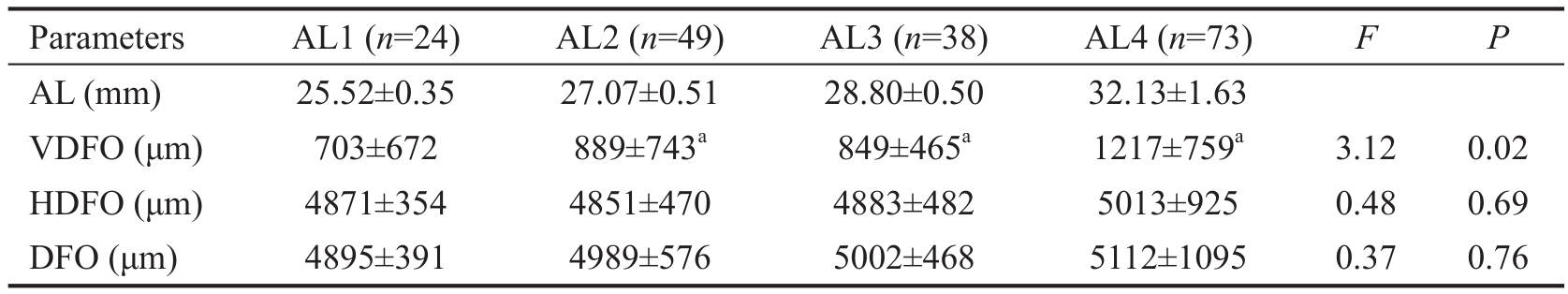
Effect of Age on the Foveal Position In the HDFO and DFO comparison, groups A1, A2, and A3 were not statistically significant. However, there was a statistically significant difference within the VDFO comparison. Compared to groups A1 and A2, the VDFO of group A3 was significantly larger(Table 1). The location of the fovea in different age groups is shown in Figure 2.
Effect of Axial Length on the Foveal Position The VDFO of AL2, AL3, and AL4 was significantly larger compared to AL1, as the difference between the groups was statistically significant. Yet, there was no statistical significance within groups AL2, AL3, and AL4. For HDFO and DFO, there was no statistical significance within the four groups (AL1, AL2,AL3, AL4) (Table 2). The location of the fovea with different ALs is presented in Figure 3.
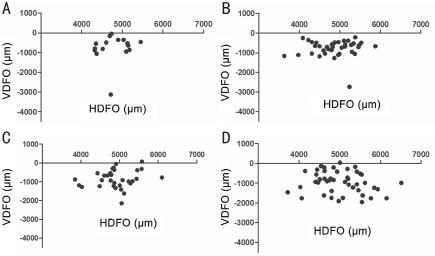
Analysis of the Relationship among VDFO, HDFO, DFO,Age, and AL VDFO is associated with age and AL, while HDFO and DFO are not correlated with age and AL (Table 3).
Table 3 The correlation among VDFO, HDFO, DFO, age, and AL
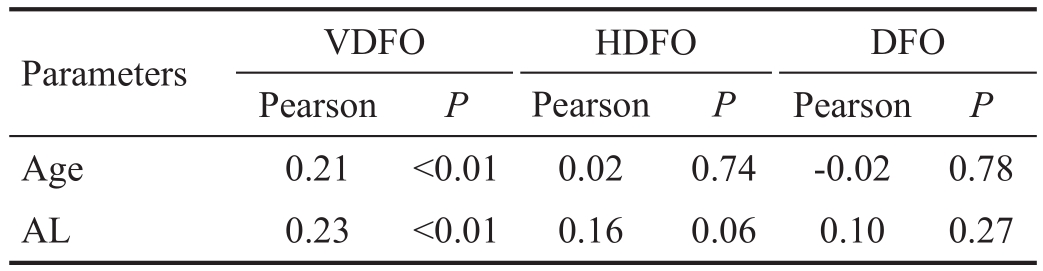
Parameters VDFO HDFO DFO Pearson P Pearson P Pearson P Age 0.21 <0.01 0.02 0.74 -0.02 0.78 AL 0.23 <0.01 0.16 0.06 0.10 0.27
DISCUSSION
HM, along with the elongation of the eye axis and the formation of posterior scleral staphyloma, leads to the irregular expansion of the posterior pole. In the posterior scleral staphyloma of a HM eye, the tilting of the optic disc often leads to morphological changes in the macula. However, it has been rarely reported whether this affects the position of the fovea. To better determine the positional changes of the fovea,this study used DRI-OCT (with the ONH as a reference point)to accurately locate the position of the fovea with VDFO,HDFO, and DFO. We also categorized different ages and AL to undergo group analysis.
In a normal eye, the marginal distance from the fovea to the temporal side of the ONH (DFO) is always consistent[16]. In a group with a refractive power of 0.9±1.7 diopter of spherical power (DS), the average DFO was 4.78 mm (4.69-4.86 mm);in a group of -9±1.7 DS, the average DFO was 4.62 mm (4.22-5.04 mm)[17]. Yet, the average DFO in a high myopic eye is 4.95±0.40 mm (4.34-6.16 mm), which is about 44.3% greater than 5 mm[16-17]. In this study, the distance analyzed (dMO)was calculated from the fovea to the center of the ONH, not the temporal side of the ONH. The average DFO in an HM eye was 5032±716 μm and ranged from 1800 to 7747 μm,with 25% of the eyes under 4651 μm, 50% under 5000 μm,and 75% under 5385 μm. There were 4 eyes (2.9%) under 4000 μm,65 eyes (46.7%) between 4000-5000 μm, 61 eyes (43.9%)between 5000-6000 μm, and 9 eyes (6.5%) above 6000 μm.
Analysis of the age groups indicated that from the differences in DFO, HDFO, and VDFO, positional changes in the fovea were not obvious in ages under 40y. But after the age of 40, vertical changes were evident. Figure 2B and 2C show horizontal distribution (with 500 μm as the center of the distribution) and vertical changes under 1000 μm in ages below 40y. Figure 2D shows that the location of the fovea shifted to be around 1000 μm away from the vertical distance, increasing the range of the horizontal distribution. In addition, there was no large horizontal change following the elongation of the eye axis. After an AL greater than 26 mm,the fovea started changing towards the vertical direction. As demonstrated in Figure 3, HM eyes with an AL within 26 mm had a VDFO of 0 to 1000 μm and a HDFO of around 5000 μm(Figure 3A). Following the lengthening of the eye axis, the fovea was first distributed in the horizontal direction (Figure 3B),and then distributed in the vertical direction (Figure 3C). When the AL was greater than 30 mm, the distribution of VDFO was between 0 to 2000 μm and the distribution of HDFO was between 4000 to 6000 μm. Correlation analyses demonstrate that VDFO is associated with age and AL, while HDFO and DFO are not correlated with age and AL.
An additional study by one of the authors further compared the HDFO and VDFO of HM and pathological myopia.Analysis of the data showed that the HDFO and VDFO of HM were 5046±719 μm and 966±603 μm, respectively.There was no statistical significance between the horizontal distances (HDFO), despite a statistically significant difference in the vertical distances (VDFO). This highly suggests that the position of the fovea shifts in the vertical direction in the progression of high myopia to pathological myopia. Some researchers have used the same DFO parameters, and found that DFO, AL, and optic disc tilt are related[18-20]. Other researchers have also used the distance between the fovea to the ONH or the side distance of the myopic arc to analyze the morphological changes in the retina of HM eyes[21-22]. Although other studies use different measurement techniques, these data demonstrate that the distance from the optic disc to the position of the fovea is elongated compared to normal eyes, simple high myopia, and pathological myopia in HM.
The current study does have some limitations, such as a small number of subjects. We had also excluded some subjects with ocular diseases that affected the position of the fovea. Thus,the sample population may not have been truly representative of the general HM population. Another investigation with more subjects may be needed in the future. In addition, some confounding factors, such as other factors affecting the foveal position, may not have been controlled and therefore we cannot completely exclude the uncontrolled confounders. However,with the increasing prevalence of high myopia, we hope that our measurements and findings will enhance the understanding of HM and advance research on this disease. In summary, the position of the fovea shifted mainly in the vertical direction as a result of age and the elongation of the eye axis in HM eyes.Our results clearly show that VDFO is associated with age and AL, while HDFO and DFO are not correlated with age and AL.The foveal position changed mainly in the vertical direction along with factors of age and AL in high myopic eyes.
ACKNOWLEDGEMENTS
We would like to acknowledge Peng Huang (Department of Epidemiology, School of Public Health, Nanchang University,Jiangxi Province, China) for conducting the statistical analyses.
Foundations: Supported by the Research and Development Project of Science and Technology of the Jiangxi Province(No.20171BBG70100); the Ophthalmic Innovation Project of Nanchang City (No.2016114).
Conflicts of Interest: Zhang Q, None; Chen KK, None; Liu WF, None; Huang GF, None.
REFERENCES
1 Xu XQ, Li SP, Xu YJ, Wei J. Prevalence of myopia among primary school students in mainland China: a Meta-analysis. Guoji Yanke Zazhi(Int Eye Sci) 2016;16(7):1221-1227.
2 Pan CW, Ramamurthy D, Saw SM. Worldwide prevalence and risk factors for myopia. Ophthalmic Physiol Opt 2012;32(1):3-16.
3 Pan CW, Dirani M, Cheng CY, Wong TY, Saw SM. The age-specific prevalence of myopia in Asia: a meta-analysis. Optom Vis Sci 2015;92(3): 258-266.4 He M, Huang W, Li Y, Zheng Y, Yin Q, Foster PJ. Refractive error and biometry in older Chinese adults: theLiwan eye study. Invest Ophthalmol Vis Sci 2009;50(11):5130-5136.
5 Liang YB, Wong TY, Sun LP, Tao QS, Wang JJ, Yang XH, Xiong Y, Wang NL, Friedman DS. Refractive errors in a rural Chinese adult population the Handan eye study. Ophthalmology 2009;116(11):2119-2127.
6 Fan DS, Lam DS, Lam RF, Lau JT, Chong KS, Cheung EY, Lai RY,Chew SJ. Prevalence, incidence, and progression of myopia of school children in Hong Kong. Invest Ophthalmol Vis Sci 2004;45(4):1071-1075.
7 Sainz-Gómez C, Fernández-Robredo P, Salinas-Alamán A, Montañés JM, Escudero Berasategui JM, Guillén-Grima F, Ruiz-Moreno JM,García-Layana A. Prevalence and causes of bilateral blindness and visual impairment among institutionalized elderly people in Pamplona, Spain.Eur J Ophthalmol 2010;20(2):442-450.
8 Cheng CY, Hsu WM, Liu JH, Tsai SY, Chou P. Refractive errors in an elderly Chinese population in Taiwan: the Shihpai Eye Study. Invest Ophthalmol Vis Sci 2003;44(11):4630.
9 Buch H, Vinding T, La Cour M, Appleyard M, Jensen GB, Nielsen NV.Prevalence and causes of visual impairment and blindness among 9980 Scandinavian adults: the Copenhagen City Eye Study. Ophthalmology 2004;111(1):53-61.
10 Verkicharla PK, Ohno-Matsui K, Saw SM. Current and predicted demographics of high myopia and an update of its associated pathological changes. Ophthalmic Physiol Opt 2015;35(5):465-475.
11 Koh V, Tan C, Tan PT, Tan M, Balla V, Nah G, Cheng CY, Ohno-Matsui K, Tan MM, Yang A, Zhao P, Wong TY, Saw SM. Myopic maculopathy and optic disc changes in highly myopic young Asian eyes and impact on visual acuity. Am J Ophthalmol 2016;164:69-79.
12 Samarawickrama C, Mitchell P, Tong L, Gazzard G, Lim L, Wong TY, Saw SM. Myopia-related optic disc and retinal changes in adolescent children from singapore. Ophthalmology 2011;118(10):2050-2057.
13 Chang L, Pan CW, Ohno-Matsui K, Lin X, Cheung GC, Gazzard G,Koh V, Hamzah H, Tai ES, Lim SC, Mitchell P, Young TL, Aung T, Wong TY, Saw SM. Myopia-related fundus changes in Singapore adults with high myopia. Am J Ophthalmol 2013;155(6):991-999.e1.
14 Asakuma T, Yasuda M, Ninomiya T, Noda Y, Arakawa S, Hashimoto S, Ohno-Matsui K, Kiyohara Y, Ishibashi T. Prevalence and risk factors for myopic retinopathy in a Japanese population: the Hisayama Study.Ophthalmology 2012;119(9):1760-1765.
15 Asai T, Ikuno Y, Akiba M, Kikawa T, Usui S, Nishida K. Analysis of peripapillary geometric characters in high myopia using swept-source optical coherence tomography. Invest Ophthalmol Vis Sci 2016;57(1): 137-144.
16 Mok KH, Lee VW. Disc-to-macula distance to disc-diameter ratio for optic disc size estimation. J Glaucoma 2002;11(5):392-395.
17 Saka N, Ohno-Matsui K, Shimada N, Sueyoshi SI, Nagaoka N,Hayashi W, Hayashi K, Moriyama M, Kojima A, Yasuzumi K, Yoshida T,Tokoro T, Mochizuki M. Long-term changes in axial length in adult eyes with pathologic myopia. Am J Ophthalmol 2010;150(4):562-568.e1.
18 Witmer MT, Margo CE, Drucker M. Tilted optic disks. Surv Ophthalmol 2010;55(5):403-428.
19 Fledelius HC, Goldschmidt E. Optic disc appearance and retinal temporal vessel arcade geometry in high myopia, as based on follow-up data over 38y. Acta Ophthalmol 2010;88(5):514-520.
20 Nonaka A, Hangai M, Akagi T, Mori S, Nukada M, Nakano N,Yoshimura N. Biometric features of peripapillary atrophy beta in eyes with high myopia. Invest Ophthalmol Vis Sci 2011;52(9):6706-6713.
21 Nakazawa M, Kurotaki J, Ruike H. Longterm fi ndings in peripapillary crescent formation in eyes with mild or moderate myopia. Acta Ophthalmol 2008;86(6):626-629.
22 Chui TY, Zhong Z, Burns SA. The relationship between peripapillary crescent and axial length: Implications for differential eye growth. Vision Res 2011;51(19):2132-2138.
Correspondence to:Wei-Feng Liu and Guo-Fu Huang.The Third Affiliated Hospital of Nanchang University, 128 Xiangshan Northern Road, Nanchang 330000, Jiangxi Province, China. 18970040725@163.com; hgf2222@sina.com
Received:2017-12-30
Accepted:2018-04-03
DOl:10.18240/ijo.2018.05.21
Citation: Zhang Q, Chen KK, Liu WF, Huang GF. Change in foveal position based on age and axial length in high myopic eyes. Int J Ophthalmol 2018;11(5):844-847