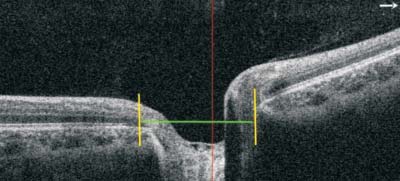
Figure 1 OCT image of ONH Yellow lines represent the RPE edge and green line means the optic disc diameter.
Abstract· Myopia, a worldwide condition, is a multifactorial disease resulting in many ocular complications. Early onset of myopia has a great tendency to develop high myopia and pathological myopia later in life. The pathophysiology and progression of myopia is still unclear. Owing to its involving in visual function, optic disc and peripapillary change in high myopia can’t be neglected, and it may help in better understanding of the pathophysiology or mechanism of myopia progression. Recently, advanced imaging techniques have been developed, such as optical coherence tomography (OCT), allowing for better detecting of optic disc and peripapillary change. OCT is a highresolution and noninvasive measurement for detection of ocular structure. Herein, we provide an updated review of optic disc and peripapillary change in OCT image, including its characteristics and clinical significance. We also propose some problems needed further investigation.
KEYWORDS: high myopia; optical coherence tomography;optic disc; peripapillary
Myopia is an increasingly important public health problem across the world, especially in East Asia. In Singapore, the occurrence of myopia is 20% to 30% among children and up to 84% in high school students[1]. Early inception of myopia is one of the most important forecasters of having high myopia in their later life. A review assessed that by 2050 half of the global residents would be myopic, one fi fth of which could be highly myopic (>-5 D)[2].
Myopia is multifactorial, possibly containing major environmental factors and a number of genes of small effect. It has been constantly reported that years of schooling is associated with myopia, while increased amounts of outside time protect against myopia developing. Thus, taking more out-of-doors activities can minimize myopia risk that associated with near work or with having myopic parents, which may be related to the dopamine levels in retina[3-4]. Evidence also suggests children with eyelid ptosis or corneal opacities can cause myopia[5]. Generally, refractive error is calculated as spherical equivalent (SE; spherical refraction plus half of the negative cylinder) in diopters, and myopia is commonly described as an SE of -0.5 D or greater, whereas high myopia is definitude as refraction of -6 D or greater (some studies described it as -5 D or greater[1-2,6]). High myopia has a vast trend to acquire pathological myopia. Pathological myopia was initially described as high myopia along with typical degenerative changes in neurosensory retina, retinal pigment epithelium (RPE),choroid, sclera, and notably, visual impairment[6]. High myopia or pathological myopia also have an elevated rate of ocular complications comprising pre-senile cataracts, glaucoma,retinal detachment, myopic choroidal neovascularization(CNV), staphyloma, macular atrophy, even blindness[7].
Ophthalmology is one of the most technology-based medical subjects with numerous recent advances due to developments in imaging technology. Evolves in the imaging technology of optic disc and peripapillary change have allowed for better understanding of the myopic pathophysiology, recording of myopia progression, and evaluating therapeutic response. In addition to traditional imaging techniques including fundus photography, B-scan ultrasound, and fundus fluorescein angiography (FFA), up-to-date imaging techniques such as optical coherence tomography (OCT), confocal scanning laser ophthalmoscope (HRT), have made a golden age heralded in the diagnosis of myopia. Since 1990s, OCT has emmitted its third-generation equipment, and the latest emerging swept source OCT (SS-OCT) and OCT angiography (OCTA) have gained clinical popularity. SS-OCT shows less signal decay and a higher speed compared with the current spectral-domain OCT (SD-OCT), while OCTA is a noninvasive, high-resolution measurement for reveal of vasculature change. Currently, OCT is extensively applied in clinical or scientific ophthalmology to attain high-resolution cross-sections retina images and has become essential in the diagnosis and management of high myopia related complications. However, optic disc and peripapillary change in high myopia has been less reviewed,herein we aim to provide an updated review of optic disc and peripapillary change in OCT image.
The morphology of the optic disc is depicted by the range and contour of the papillary. The optic nerve head (ONH) was outlined as the area within the peripapillary scleral ring. The border of the ONH is usually defined by revealing the top and inner rims of RPE. The line is then joined and considered as the disc diameter (Figure 1).
After amplification modification, the disc area and rim area in highly myopic eyes was drastically larger than normal, mainly owing to the broadening of the scleral canal and the following expansion of the lamina cribrosa[8]. Jonas[9] deduced that optic disc size depends on refractive error merely when it was beyond -8 D. Whether the papillary size enlarged with myopia need further investigation. It’s vital that manual drawing of the optic disc boundary was performed as the temporal disc margin mechanically determined by Stratus OCT was farther absent from the disc, resulting in a greater optic disc area.
Besides the variation in optic disc area, slanted optic disc is uncovered in myopia. In myopic eyes, sloped insertion of the optic nerve classically arises and this may put underlying mechanical pressure on the ONH. Oblique index (OI),termed as the shortest/longest axis of the ONH, formerly was the benchmark to detect this ‘inclination’ in myopic eyes.Nevertheless, current studies[10] proposed that OI could be substituted by the peripapillary tilting index (PTI) on OCT vision because of its’ two-dimensional quality. The PTI is defined as the difference between the RPE altitude of one sector and the average RPE altitude, which is averaged from the height of RPE of all sectors (standard RPE plane) (Figure 2). If the RPE position was below the standard plane, it was defined as a negative value and if upwards, it was a positive value.
PTI is defined as the difference between the RPE altitude of one sector and the average RPE altitude. The average RPE altitude, or standard RPE plane (white line in Figure 2),is calculated from RPE altitudes of all sectors. If the RPE position was below the standard plane, it was defined as a negative value and if upwards, it was a positive value.
The revolving over the vertical axis (temporal disc border rearward and nasal frontward) leads to a vertically oval shape of the papillary and a relatively reducing of the horizontal disc width. Conversely, the spin over the horizontal axis(inferior disc margin rearward and superior frontward) causes a horizontally oval shape with a fairly reduction of the vertical disc width. The measurement of papillary titling over the vertical or horizontal axis is quantified as the angle among Bruch’s membrane line and the OCT scanning line horizontally or vertically through the optic disc (Figure 3).
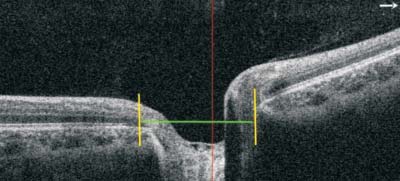
Figure 1 OCT image of ONH Yellow lines represent the RPE edge and green line means the optic disc diameter.
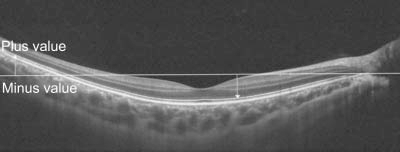
Figure 2 OCT B-scan image illustrating the PTI.

Figure 3 OCT image of ONH Yellow line represents the Bruch’s membrane line.
The incidence of optic titling is about 77% of myopic eyes and was evidently greater in the elderly. Optic disc slanting has considerable association with the degree of myopia, axial length, retinal nerve fiber layer (RNFL) thickness and parapapillary beta/gamma zone[10-15]. Larger slope was also testified to have correlation with enlarged corneal astigmatism[16] and worse staphyloma[10].Current studies have revealed that through horizontal eye actions, the optic nerve dragged the papillary posteriorly[17-18].As the optic nerve initiates in the nasal superior section of the orbit, the optic nerve dragging is academically tougher on the temporal or inferior part of the ONH. These alterations could elucidate the disc rotation.
Studies demonstrated that without amplification modification OCT quantities of universal RNFL and non-temporal RNFLs become drastically thinner while temporal RNFL is considerably thicker in myopic eyes than regular[19-20]. It was hazarded that as the axial distance enlarged, the retina is hauled to the temporal sphere, and the chunkiness of the temporal peripapillary RNFL added while that of the nontemporal peripapillary RNFL declined. RNFL thickness was notably less in high or moderate myopia when compared that with low myopia, while the discrepancy among moderate and high myopia didn’t have arithmetical meaning[21-22]. RNFL thinning could be found in glaucoma either, which need careful investigations to avoid misdiagnosis.
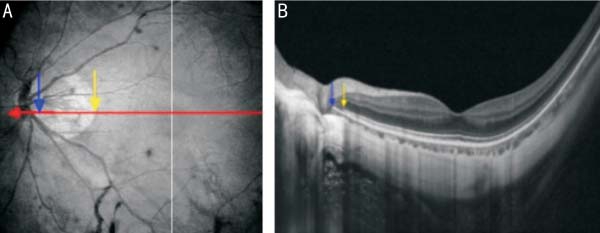
Figure 4 NIR images of fundi (A) and horizontal cross-sectional images obtained by OCT (B) The red line indicates the direction of OCT scanning. Yellow arrows indicate the temporal margins of PPA-β and blue arrows indicate the nasal margins of PPA-β.
In contrast, after amplification modi fication OCT measurements revealed that the global and temporal RNFLs were notably thicker and nasal RNFL was notably thinner in highly myopic eyes, while superior or inferior quantities did not considerably differ in two groups[8,23]. To conclude, with or without amplification modification, temporal RNFL is thicker and nasal is thinner in high myopia than that of normal eyes. The relocation of the RNFL in high myopia eye triggers temporal retinal pulling, which causes the temporal thickening and enlarged posterior staphyloma. Whether the global RNFL is thicker or thinner in high myopia than normal remains controversial. Eyes with a huger optic disc region is likely to develop a thicker RNFL, which could be due to the extra retinal nerve fiber axons it maintained or the overestimation connected to scanning circle space[20].
Liu et al[16] stated that astigmatism also has correlation with the RNFL thickness. High myopic eyes with greater corneal astigmatism could have a thinner temporal RNFL thickness and a more temporally positioned RNFL peak. The peripapillary RNFL thickness were also correlated with the extent of optic disc tilt, exclusively in the temporal region[14]. As the optic disc turns into tilted, the temporal peripapillary region would be stretched and atrophied. Such changes can cause alterations in reflectivity or back dot discovered by the OCT and then variations in RNFL thickness quantifications. In pathologic myopia, eyes with a peripapillary retinal detachment (PRD)had a considerably greater mean RFNL thickness than those without due to the RNFL external outline misidenti fi cation[24].The axial length-produced exaggeration effect, the extent of corneal astigmatism, or the papillary tilt grade ought to be modi fi ed by ophthalmologists as well as the current OCT database.
Peripapillary atrophy (PPA) is a clinical discovering related to choroid-retinal thinning and interruption of RPE in peripapillary area (Figure 4). It can happen in both benign and pathologic states, involving aging or high myopia, but they may be triggered by different mechanisms[14]. PPA was sorted into three groups: existence of Bruch’s membrane with random RPE (α zone); existence of Bruch´s membrane lacking RPE(β zone); absence of Bruch’s membrane (γ zone)[25]. α zone can lead to a relative scotoma while β zone may result in a complete scotoma, which is in line with the OCT findings of photoreceptor and RPE deficiency[26].
The incidence and area of PPA-β were notably greater in eyes having visual field deficiency than those haven’t, which indicate the relationship between PPA and visual impairment.In myopic eyes, histologic findings showed Bruch’s membrane and choroid-capillary absent in the region of PPA. In OCT study, sloped spreading of the neural canal was detected,resulting in its mismatch with scleral canal opening[27],which may have connection with the histologic results. The prevalence of PPA is high in myopic eyes (>90%), though it can be seen by fundus photography, OCT can discover the exact status of inner retina and do help in understanding of its mechanism.
With the progression of myopia, peripapillary intra-choroidal cavitation (PICC) and peripapillary detachment (PD) occur.PICC previously defined as ‘PD’ of pathologic myopia[28],was depicted by an intra-choroidal hypo-reflective space with regular retina and RPE by OCT[29] (Figure 5). On fundus photography, PICC revealed a yellow-orange lesion. On OCT images, PICCs were described as trilateral thickening of choroid and the Bruch’s membrane to sclera distance over 200 μm. The prevalence of PICC was 17%±4.0% in highly myopic eyes, while no PICC has been detected in emmetropic eyes[29-30]. Only 50% of PICCs discovered on OCT pictures revealed a yellow-orange lesion on fundus photography. OCT can clearly detect the sharp of PICC and help in distinguish it from myopic optic pits or conus pits.
Incidence of PICC was drastically related with a higher level of papillary tilting and the existence of posterior staphyloma. It was estimated that about 52.5% PICC eyes have a peripapillary staphyloma, which indicates the close relationship between them. PICC frequently occurred in the inferior border of papillary, but recently temporally PICCs was found. The temporal intra-choroidal cavitertions (ICCs) are more massive and can even spread over the central fovea, while the inferior ICC appears to be limited to the myopic conus region[29-31]. The pathophysiology of PICC is still blurred. During the progression of PICC, extension of the peripapillary sclera, defect in the retina,and transmission between intra-choroidal cavity and vitreous may be important fractions.
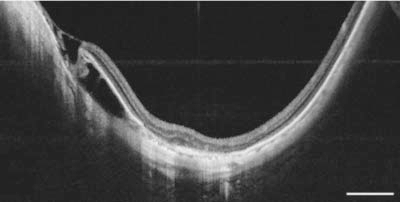
Figure 5 Horizontal OC T scans detect an ICC in the temporal of the optic disc, with the herniated retina A hypo-reflective space indicates the existence of fluid inside the ICC. This figure was adapted from reference No.30 and we have got reprint permission from its publisher.
Posterior retinoschisis in high myopia is not rare. There could be a gradual development from myopic retinoschisis to retinal detachm[32]. It may result from posterior staphyloma, tractions from the vitreous, or retinal atrophy, which normally cannot be clearly discovered by fundoscopic examination. SD OCT can clearly acquire the morphological alterations of retinoschisis(Figure 6). The schisis could be seen in each layers of the retina and inner schisis resolved earlier than the outer schisis, which may due to different tractions[33]. Vitrectomy plus internal limiting membrane (ILM) peeling is effective in treating the schisis, but ophthalmologist need cautious evaluation before ILM peeling.
Peripapillary detachment of pathologic myopia (PDPM) was described as a yellow-orange lesion near the inferior margin of myopic conus in fundus photography and a hypo-re flective region located between RPE and neurosensory retina in OCT manifestation[28]. Not all PDPM could be detected by the ophthalmoscopy, especially when PDPM was covered by the conus. In addition, the lesion of PDPM might be confused by other ocular diseases like tumor or CNV on fundus photography. Thus, PDPM might be more often detected in high myopic eyes by OCT than by fundus check alone. B-scan can also be applicated in detecting PD, but OCT can clearly show the morphology of retina layers and discover other complications of high myopia. The OCT scans found in PD eyes 52.38% having PICC[29], which promotes us to further explore the correlation between PICC and PD.
Optic nerve is surrounded by the retrobulbar subarachnoid space (SAS), a place with cerebrospinal fluid flows. SAS is a hypo-reflective triangle region, with its apex toward the optic nerve on SS-OCT (Figure 7). SAS size was described as the maximum distance from dura mater to optic nerve and it was obviously enlarged in highly myopic eyes[34]. When the axial length of high myopic eyes was more than 28 mm, the incidence of SS-OCT detected SAS could be 93.2%, while no SAS couldn’t be seen in emmetropic eyes[35]. Visibility and breadth of SAS were influenced by choroid thickness, axial length, myopia degree and PPA or optic disc area.

Figure 6 OCT image of a retinoschisis.
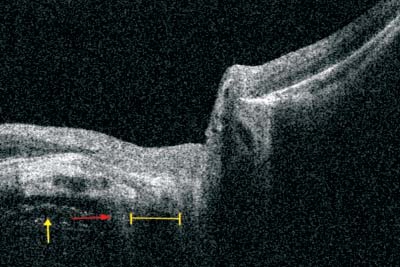
Figure 7 OCT image of SAS The width was described as the maximum distance from the dura mater (red arrow) to the optic nerve(yellow line). Yellow arrow shows the orbital fat.
SAS pressure was found to be related to many ocular sickness,involving papilledema, glaucoma or optic pit. Enlarged SAS causes optic nerve increased tendency of exposing to the cerebrospinal fluid stress, and increases peripapillary sclera burden. SAS can be detected temporal to or on both side of the optic nerve in eyes with huge temporal conus or annular atrophy respectively. The histologic findings of peripapillary conus in high myopic eyes showed an elongation and thinning of the peripapillary scleral flange (sclera between optic nerve edge and dura matter), which was consistent with the expansion of SAS into the retro-papillary section[36].Investigations are needed to further explore the biomechanics of the optic nerve dura mater, which may play a vital role in optic disc tilting and peripapillary degenerative damage[15].
Myopic CNV is one of the most crucial causes of irreparable visual deficit in myopic patients (Figure 8). Its prevalence is around 10%±5%, fortunately its post-treatment outcome is usually better than other kinds of CNV[37]. Morphological vasculature alteration used to be examined by Doppler ultrasound or FFA. Doppler ultrasound provides low-resolution pictures and FFA is an invasive assessment. Lately, a noninvasive, highresolution and three-dimensional (3D) illustration technique to discover retinal vessels by OCTA has been created (Figure 9).It provides morphological material of retinal vessels and can quantify the vascular density[38]. A peripapillary CNV is located at the margin of the papillary, appearing as a hyper-re flective tissue with vague borders over the RPE and slight retinal exudation on SD-OCT[39].

Figure 8 NIR (A) and OCT (B) image of a peripapillary CNV temporal to the optic disc.
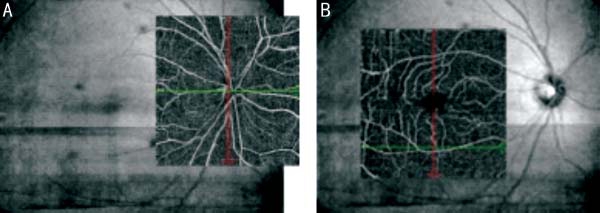
Figure 9 OCTA image of optic disc angiography (A) and macular angiography (B), providing morphological material of retinal vessels and quantify the vascular density.
Choroid-retinal atrophy could allow fresh vessels penetrate into the neural retina across the Bruch membrane defect,which were thought to be a risk factor of CNV occurrence[37].Moreover, a peripapillary CNV eye had a considerably larger myopic conus, decreased blood flow and reduced retinal vessel diameter or density, which were thought to promote the myopic degenerative changes[39]. To avoid the vicious cycle, myopic CNV requires early detection and careful follow-up. Recently anti-angiogenesis therapy like anti-vascular endothelial growth factor treatment has been broadly used to control CNV and OCT can be used as follow-up assessment method.
Para-vascular inner retinal defects (PIRD) are dark spindle shaped retinal defects alongside the main retinal vessels on fundus photography and fi ssure-like places or retinoschisis-like alters on OCT. The prevalence of PIRD is almost 40% in high myopic eyes.PIRD have association with myopia degree, axial length, and staphyloma severity[40]. It can occur in high myopic eyes or eyes with epiretinal membrane. It was considered that the eyeball anteroposterior elongation leads to coaxial deviation and defects of major retinal vessels, while the epiretinal membrane can induce traction force causing retinal vessels to diverge tangentially[41]. SS-OCT images reveal that major vessels are strayed into the vitreous cavity and PIRDs are associated with broad retinal thinning[40]. Extra studies are needed to validate whether PIRDs may develop into fullthickness retinal defects or retinal detachment.
The choroid supplies blood to the outer retina including the prelaminar part of the optic nerve. Choroid thinning would result in declined blood flow in choroid capillaries, making it more vulnerable to hypoxia or intraocular pressure (IOP)elevation, which push us to find some ways to alleviate the choroid thinning. Quantitative measurement of peripapillary choroidal thickness (PPCT) may help explicate the mechanisms the peripapillary choroid works. OCT offers an easy and noninvasive approach to measure PPCT. The PPCT was measured as the vertical distance between the Bruch’s membrane and the choroid-scleral interface[42] (Figure 10).
The mean PPCT was notably smaller in high myopic eyes,especially in inferotemporal region. Axial length, IOP,staphyloma and retinal atrophy extensively affect PPCT[42]and should be taken into concern during clinical explanation of PPCT measurement. Data of normal PPCT in high myopic eyes may help in the learning of pathophysiological changes of peripapillary choroid-retinal conditions.
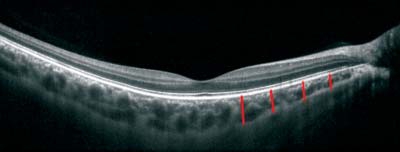
Figure 10 OCT image of PPCT The PPCT was measured as the vertical distance between Bruch’s membrane and the choroid-scleral interface (red lines).
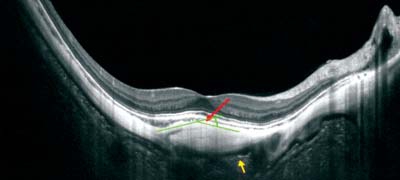
Figure 11 OCT image of scleral deformation, showing moderate temporal scleral bending (red arrow), highly reflective tissue behind scleral bending (yellow arrow); two lines were drawn along the scleral bending (green lines). The angle between the green lines was measured with a green arch.
SS-OCT allows clear detection of peripapillary scleral changes which are not apparent on fundus photography. The quantitative measurement of the scleral structures by OCT can help in revealing their clinical relevance. The scleral bending angel was calculated by drawing 2 lines along the scleral bending, and then measured the angle between them (Figure 11).The prevalence of scleral was 13.3%, more frequently in eyes having visual field defects than those have n’t. Scleral bending displayed a wide variety of angles, which was linked to thinner RNFL and worse visual field defect[43-44]. Considering the relationship between scleral protrusion and visual field defects,those highly myopic patients with harsh scleral bending on OCT need careful follow-up.
Furthermore, a highly re flective matter was observed beneath the scleral bending in almost half of the eyes[44]. This structure possessed a similar reflectivity strength with the sclera, but was detached from the covering sclera, which was presumed to be the reason of scleral bending. Further OCT inspections and histologic researches are required to discover what this structure is and whether it is blamable for the scleral bending.
In myopic eyes, various papillary and peripapillary changes can develop. OCT is a non-invasive technique to acquire high-resolution cross-sectional fundus images. OCT should be considered when high myopia patients have a decreasing vision but with no obvious fundoscopic findings. To date,retinal changes in high myopia is still unclear, which promote us to investigate the retinal changes even in both early and late stages. In addition, RNFL thinning, optic disc deformation,or direct scleral compression in the peripapillary region can also be detected as characteristics in other diseases such as glaucoma. Therefore, a normative OCT database is needed for high myopic so as to distinguish the physiological changes of high myopia from other diseases. Moreover, there is a need to improve the resolution, scan depth and speed, and the accuracy of OCT automatic segmentation within the optic disc margin in high myopia.
Foundation: Supported by the National Key Project of Research and Development Plan (No.2017YFA0104101).
Conflicts of Interest: Pan T, None; Su Y, None; Yuan ST,None; Lu HC, None; Hu ZZ, None; Liu QH, None.
REFERENCES
1 Chua SY, Sabanayagam C, Cheung YB, Chia A, Valenzuela RK, Tan D,Wong TY, Cheng CY, Saw SM. Age of onset of myopia predicts risk of high myopia in later childhood in myopic Singapore children. Ophthalmic Physiol Opt 2016;36(4):388-394.
2 Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, Wong TY, Naduvilath TJ, Resnikoff S. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050.Ophthalmology 2016;123(5):1036-1042.
3 Ashby R. Animal studies and the mechanism of myopia-protection by light? Optom Vis Sci 2016;93(9):1052-1054.
4 Jones-Jordan LA, Sinnott LT, Cotter SA, Kleinstein RN, Manny RE,Mutti DO, Twelker JD, Zadnik K. Time outdoors, visual activity, and myopia progression in juvenile-onset myopes. Invest Ophthalmol Vis Sci 2012;53(11):7169-7175.
5 Hoyt CS, Stone RD, Fromer C, Billson FA. Monocular axial myopia associated with neonatal eyelid closure in human infants. Am J Ophthalmol 1981;91(2):197-200.
6 Morgan IG, Ohno-Matsui K, Saw SM. Myopia. Lancet 2012;379(9827):1739-1748.
7 Saw SM, Gazzard G, Shih-Yen EC, Chua WH. Myopia and associated pathological complications. Ophthalmic Physiol Opt 2005;25(5):381-391.
8 Hsu SY, Chang MS, Ko ML, Harnod T. Retinal nerve fibre layer thickness and optic nerve head size measured in high myopes by optical coherence tomography. Clin Exp Optom 2013;96(4):373-378.
9 Jonas JB. Optic disk size correlated with refractive error. Am J Ophthalmol 2005;139(2):346-348.
10 Asai T, Ikuno Y, Akiba M, Kikawa T, Usui S, Nishida K. Analysis of peripapillary geometric characters in high myopia using swept-source optical coherence tomography. Invest Ophthalmol Vis Sci 2016;57(1):137-144.
11 Dai Y, Jonas JB, Ling Z, Sun X. Ophthalmoscopic-perspectively distorted optic disc diameters and real disc diameters. Invest Ophthalmol Vis Sci 2015;56(12):7076-7083.
12 Fan YY, Jonas JB, Wang YX, Chen CX, Wei WB. Horizontal and vertical optic disc rotation: The Beijing Eye Study. PLoS One 2017;12(5):e175749.
13 Hosseini H, Nassiri N, Azarbod P, Giaconi J, Chou T, Caprioli J,Nouri-Mahdavi K. Measurement of the optic disc vertical tilt angle with spectral-domain optical coherence tomography and influencing factors.Am J Ophthalmol 2013;156(4):737-744.
14 Hwang YH, Yoo C, Kim YY. Myopic optic disc tilt and the characteristics of peripapillary retinal nerve fiber layer thickness measured by spectraldomain optical coherence tomography. J Glaucoma 2012;21(4):260-265.
15 Jonas JB, Wang YX, Zhang Q, Fan YY, Xu L, Wei WB, Jonas RA.Parapapillary gamma zone and axial elongation-associated optic disc rotation: the Beijing eye study. Invest Ophthalmol Vis Sci 2016;57(2):396-402.
16 Liu L, Zou J, Huang H, Yang JG, Chen SR. The in fl uence of corneal astigmatism on retinal nerve fiber layer thickness and optic nerve head parameter measurements by spectral-domain optical coherence tomography. Diagn Pathol 2012;7:55.
17 Demer JL. Optic Nerve sheath as a novel mechanical load on the globe in ocular duction. Invest Ophthalmol Vis Sci 2016;57(4):1826-1838.
18 Wang X, Beotra MR, Tun TA, Baskaran M, Perera S, Aung T, Strouthidis NG, Milea D, Girard MJ. In vivo 3-dimensional strain mapping confirms large optic nerve head deformations following horizontal eye movements.Invest Ophthalmol Vis Sci 2016;57(13):5825-5833.
19 Malakar M, Askari SN, Ashraf H, Waris A, Ahuja A, Asghar A. Optical coherence tomography assisted retinal nerve fi bre layer thickness pro fi le in high myopia. J Clin Diagn Res 2015;9(2):NC01-NC03.
20 Seo S, Lee CE, Jeong JH, Park KH, Kim DM, Jeoung JW. Ganglion cell-inner plexiform layer and retinal nerve fi ber layer thickness according to myopia and optic disc area: a quantitative and three-dimensional analysis. BMC Ophthalmol 2017;17(1):22.
21 Mohammad Salih PA. Evaluation of peripapillary retinal nerve fiber layer thickness in myopic eyes by spectral-domain optical coherence tomography. J Glaucoma 2012;21(1):41-44.
22 Oner V, Aykut V, Tas M, Alakus MF, Iscan Y. Effect of refractive status on peripapillary retinal nerve fibrelayer thickness: a study by RTVue spectral domain optical coherence tomography. Br J Ophthalmol 2013;97(1):75-79.
23 Kang SH, Hong SW, Im SK, Lee SH, Ahn MD. Effect of myopia on the thickness of the retinal nerve fiber layer measured by Cirrus HD optical coherence tomography. Invest Ophthalmol Vis Sci 2010;51(8):4075-4083.
24 Kamal Salah R, Morillo-Sánchez MJ, García-Ben A, Rius-Diaz F, Cilveti-Puche Á, Figueroa-Ortiz L, García-Campos JM. The effect of peripapillary detachment on retinal nerve fiber layer measurement by spectral domain optical coherence tomography in high myopia.Ophthalmologica 2015;233(3-4):209-215.
25 Dai Y, Jonas JB, Huang H, Wang M, Sun X. Microstructure of parapapillary atrophy: beta zone and gamma zone. Invest Ophthalmol Vis Sci 2013;54(3):2013-2018.
26 Ren sch F, Jonas JB. Direct microperimetry of alpha zone and beta zone parapapillary atrophy. Br J Ophthalmol 2008;92(12):1617-1619.
27 Str outhidis NG, Yang H, Reynaud JF, Grimm JL, Gardiner SK, Fortune B, Burgoyne CF. Comparison of clinical and spectral domain optical coherence tomography optic disc margin anatomy. Invest Ophthalmol Vis Sci 2009;50(10):4709-4718.
28 Fre und KB, Ciardella AP, Yannuzzi LA, Pece A, Goldbaum M,Kokame GT, Orlock D. Peripapillary detachment in pathologic myopia.Arch Ophthalmol 2003;121(2):197-204.
29 Ohno-Matsui K, Shimada N, Akiba M, Moriyama M, Ishibashi T,Tokoro T. Characteristics of intrachoroidal cavitation located temporal to optic disc in highly myopic eyes. Eye (Lond) 2013;27(5):630-638.
30 You QS, Peng XY, Chen CX, Xu L, Jonas JB. Peripapillary intrachoroidal cavitations. The Beijing eye study. PLoS One 2013;8(10):e78743.
31 Shi nohara K, Moriyama M, Shimada N, Yoshida T, Ohno-Matsui K. Characteristics of peripapillary staphylomas associated with high myopia determined by swept-source optical coherence tomography. Am J Ophthalmol 2016;169:138-144.
32 Shi mada N, Ohno-Matsui K, Yoshida T, Sugamoto Y, Tokoro T, Mochizuki M. Progression from macular retinoschisis to retinal detachment in highly myopic eyes is associated with outer lamellar hole formation. Br J Ophthalmol 2008;92(6):762-764.
33 Wan g S, Peng Q, Zhao P. SD-OCT use in myopic retinoschisis preand post-vitrectomy. Optom Vis Sci 2012;89(5):678-683.
34 Fan H, Ma H, Gao R, Ng DS, Cheung CY, Li S, Wu D, Tang S.Associated factors for visibility and width of retrobulbar subarachnoid space on swept-source optical coherence tomography in high myopia. Sci Rep 2016;6:36723.
35 Ohn o-Matsui K, Akiba M, Moriyama M, Ishibashi T, Tokoro T, Spaide RF. Imaging retrobulbar subarachnoid space around optic nerve by sweptsource optical coherence tomography in eyes with pathologic myopia.Invest Ophthalmol Vis Sci 2011;52(13):9644-9650.
36 Jon as JB, Jonas SB, Jonas RA, Holbach L, Panda-Jonas S. Histology of the parapapillary region in high myopia. Am J Ophthalmol 2011;152(6):1021-1029.
37 Bro wning DJ, Fraser CM. Ocular conditions associated with peripapillary subretinal neovascularization, their relative frequencies, and associated outcomes. Ophthalmology 2005;112(6):1054-1061.
38 Li J, Yang YQ, Yang DY, Liu XX, Sun YX, Wei SF, Wang NL.Reproducibility of perfusion parameters of optic disc and macula in rhesus monkeys by optical coherence tomography angiography. Chin Med J (Engl) 2016;129(9):1087-1090.
39 Nag aoka N, Shimada N, Hayashi W, Hayashi K, Moriyama M, Yoshida T, Tokoro T, Ohno-Matsui K. Characteristics of periconus choroidal neovascularization in pathologic myopia. Am J Ophthalmol 2011;152(3):420-427.40 Shi mada N, Ohno-Matsui K, Nishimuta A, Moriyama M, Yoshida T,Tokoro T, Mochizuki M. Detection of paravascular lamellar holes and other paravascular abnormalities by optical coherence tomography in eyes with high myopia. Ophthalmology 2008;115(4):708-717.
41 Mur aoka Y, Tsujikawa A, Hata M, Yamashiro K, Ellabban AA,Takahashi A, Nakanishi H, Ooto S, TanabeT, Yoshimura N. Paravascular inner retinal defect associated with high myopia or epiretinal membrane.JAMA Ophthalmol 2015;133(4):413-420.
42 Gup ta P, Cheung CY, Saw SM, Bhargava M, Tan CS, Tan M, Yang A, Tey F, Nah G, Zhao P, Wong TY, Cheng CY. Peripapillary choroidal thickness in young Asians with high myopia. Invest Ophthalmol Vis Sci 2015;56(3):1475-1481.
43 Aka gi T, Hangai M, Kimura Y, Ikeda HO, Nonaka A, Matsumoto A,Akiba M, Yoshimura N. Peripapillary scleral deformation and retinal nerve fiber damage in high myopia assessed with swept-source optical coherence tomography. Am J Ophthalmol 2013;155(5):927-936.
44 Ohno-Matsui K, Shimada N, Yasuzumi K, Hayashi K, Yoshida T, Kojima A, Moriyama M, Tokoro T. Long-term development of significant visual fi eld defects in highly myopic eyes. Am J Ophthalmol 2011;152(2):256-265.
Received:2017-10-23
Accepted:2018-05-18
DOl:10.18240/ijo.2018.05.25
Citation: Pan T, Su Y, Yuan ST, Lu HC, Hu ZZ, Liu QH. Optic disc and peripapillary changes by optic coherence tomography in high myopia. Int J Ophthalmol 2018;11(5):874-880