INTRODUCTION
Biometry is the important step for measurement of intraocular lens (IOL) degree, which includes axial length (AL) and cornea curvature[1]. The AL is indispensable variable for theoretical IOLs power calculation[2]. Cornea curvature can only be measured by optic biometry, but there are two methods of the measurement of AL: ultrasound and optical biometers. Immersion ultrasound is an accurate method for AL measurement determination, and considered better than applanation ultrasound method[3]. Although ultrasound AL measurements have been the gold standard for a long time,the Lenstar LS 900 uses optical low coherence reflectometry(OLCR) technology, with an 820-mm super luminescent diode,to measure the AL of the eyes, and noncontact optical biometry measurement without risk of infection and indentation[4]. This study aimed to compare the agreement of biometry parameters with immersion ultrasound and low coherence reflectometry in cataractous eyes.
SUBJECTS AND METHODS
Patients This prospective clinical study enrolled adult patients intended for cataract surgery. Only 1 eye of each patient was included in this study as the study eye. The decision was based on the recommendation of the referring physician on which eye needed surgery first. Inclusion criteria were as follows:no ocular abnormalities such as keratoconus, no ocular injury or surgery, no obvious opacity in refracting media except for cataract. The research protocol was reviewed and approved by the Ethics Committee of Tianjin Eye Hospital. Each adult patient was examined on the same day with the Lenstar LS 900 and the immersion ultrasound. The same examiner performed all the measurements in the same patient. The study was performed in accordance with the European Guidelines for Good Clinical Practice and the Declaration of Helsinki. Prior to this study, all patients provided informed consent.
Ultrasound Biometry AL was measured respectively by immersion B-ultrasound (IB) and immersion A-ultrasound(IA) with A/B ocular ultrasound apparatus (10 MHz central frequency, MD-2300, MEDA Co., Ltd. Tianjin, China). The anterior boundary of AL was located on the surface of corneal vertex, and the posterior boundary of AL was located on the surface of the scleral. Five measurements were taken each eye with three instruments. Operation process was in strict accordance with the technical specification of hand hygiene disinfection and disinfection for medical staff (2012 version)drafted by National Health and Family Planning Commission of People’s Republic of China. Defaults of segmented sound velocities were: cornea 1620 m/s, lens 1641 m/s and aqueous humor and vitreous 1532 m/s[5-6]. Temperature of examination room was maintained at 25℃-27℃ to eliminate interference factor.
Lenstar LS 900 Biometry The Lenstar LS 900 optical biometer (Haag-Streit AG, Koeniz, Switzerland) is based on OLCR technology, using an 820-nm super luminescent diode by 32 reference points orientated in 2 circles. Here were operation steps: 1) patients seated in front of biometer,placed the mandibular jaw on throat mold; 2) patients were told to look at red fixation target inside; 3) the biometer got parameters automatically when reference points clearly presented on the corneal surface. The results were averaged after 3 times measurement, the standard deviation (SD) of AL should not be more than 0.05 mm[7].
Statistical Analysis The mean values and SD for each group were obtained. The agreement of the AL measurements, using the method of Bland-Altman, was evaluated by comparing the mean (x-axis) and the differences between the devices(y-axis)[8]; the 95% limits of agreement (LoA) were calculated by the mean difference (MD)±1.96 SD. If the values of AL followed a Gaussian distribution, they were calculated using a paired t-test. If not, the values were calculated by the Wilcoxon matched-pairs test. The Pearson product moment correlation coefficient (r) was used to statistically evaluate the correlation. Statistical analysis was performed using SPSS software (version 18.0, SPSS, Inc.). A P value less than 0.05 was considered statistically significant.
RESULTS
Eighty eyes of 80 patients (39 men and 41 women) were included in the study scheduled for cataract surgery. The mean age was 59.20±6.57y (ranged 55 to 83y). The values of ALcould be got from all 80 eyes by IB and IA (Group 1), the difference of AL measurements between IA and IB was of no statistical significance (P=0.97); MD in AL measurements was -0.031 mm (P=0.26; 95%CI, -0.09 to 0.02); the excellent correlation was showed between IA and IB (r=0.98, P<0.0001;Table 1).
Table 1 Characteristics of measurement data with statistical analysis for all eyes comparing the Lenstar to the immersion ultrasound mean±SD

IB: Immersion B-ultrasound; IA: Immersion A-ultrasound; AL: Axial length. aPearson correlation coefficient, all P<0.0001; bt-test.
Figure 1A shows a Bland-Altman plot of the agreement was excellent (95% LoA, -0.52 to 0.46 mm). Forty-five of eighty eyes with results of AL measurements, which can be obtained by three methods (Group 2); among those eyes,the difference of AL measurements between IA and IB was of no statistical significance (P=0.18); the MD in AL measurements was -0.042 mm (P=0.09; 95%CI, -0.09 to 0.007); the excellent correlation was showed between IA and IB (r=0.99, P<0.0001; Table 1). Figure 1B shows a Bland-Altman plot of the agreement (95% LoA, -0.36 to 0.28 mm).The difference of AL measurements between IA and Lenstar was of no statistical significance (P=0.51); the MD in AL measurements was -0.019 mm (P=0.71; 95%CI, -0.08 to 0.12); the excellent correlation was showed between IA and Lenstar (r=0.96, P<0.0001). Figure 1C shows a Bland-Altman plot of the agreement (95% LoA, -0.65 to 0.69 mm).The difference of AL measurements between IB and Lenstar was of no statistical significance (P=0.07); the MD in AL measurements was 0.061 mm (P=0.20; 95%CI, -0.03 to 0.16);the excellent correlation was showed between IB and Lenstar(r=0.96, P<0.0001). Figure 1D shows a Bland-Altman plot of the agreement (95% LoA, -0.55 to 0.68 mm).
DISCUSSION
The refractive outcome is dependent on many factors after phacoemulsification cataract surgery. They include AL measurement, keratometry, anterior chamber depth, IOL power formulae. Of these factors, accurate AL measurements were shown to be the major factor to the predictability the outcome of IOL power calculation[9].
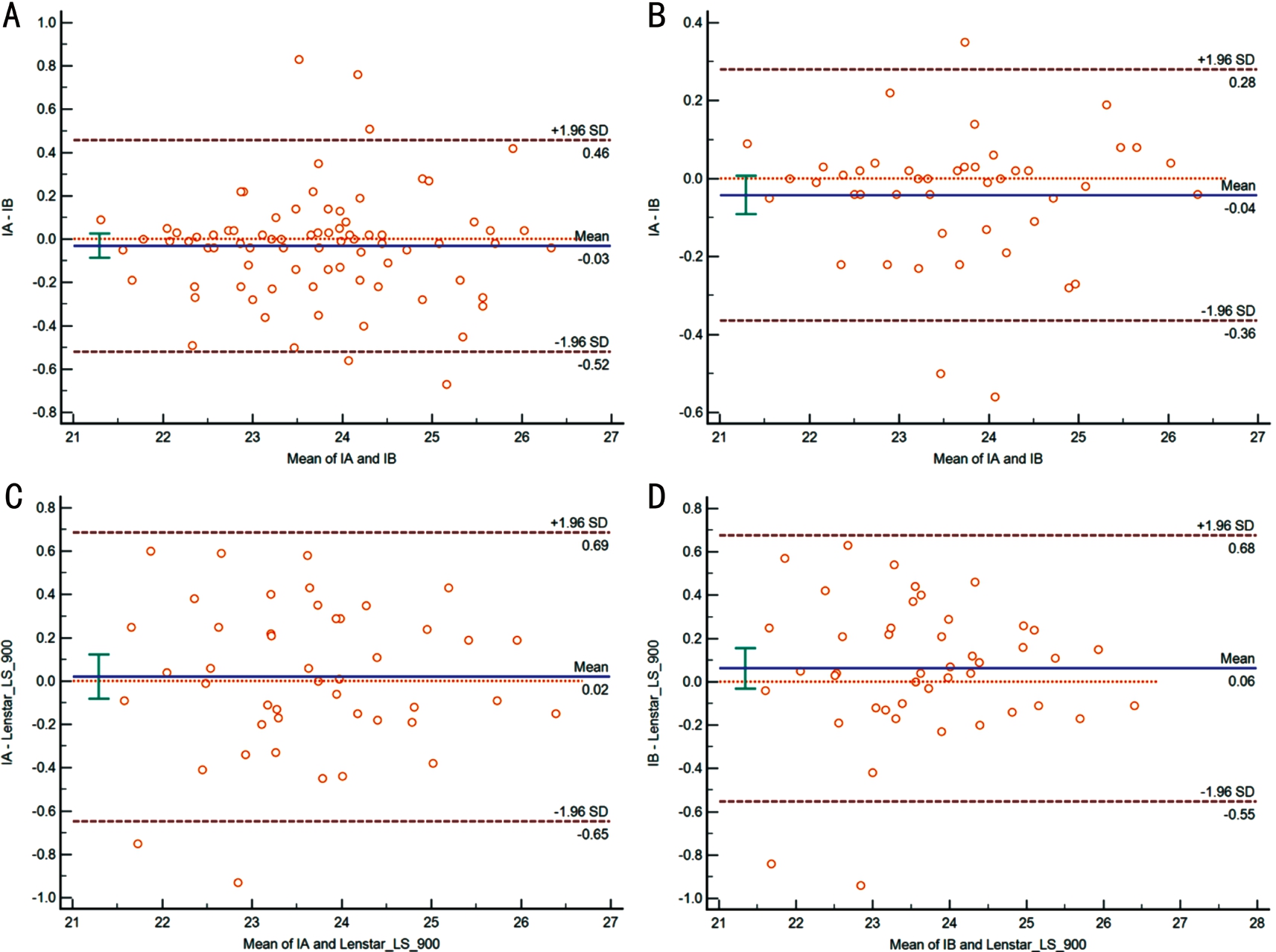
Figure 1 Bland-Altman plot of the agreement in AL measurements among the three operators A: IA and IB in all 80 eyes; B: IA and IB in 45 eyes; C: IA and Lenstar in 45 eyes; D: IB and Lenstar in 45 eyes.
The study was designed to compare the biometry results of AL in cataract eyes by three methods: IB biometry, IA biometry and Lenstar LS 900 optical biometry. To date, no previous study has employed this objective method to explore the comparition of AL and other parameters between these three methods. With the improvement of cataract surgical technique,the expectation of postoperative visual function is much higher than before[10]. The postoperative visual function depends on accurate biometry of AL[11]. Optical coherence biometry and ultrasound biometry are both important and popular means of biometry[12]. Immersion ultrasound is an accurate method for AL measurement determination, and considered better than applanation ultrasound method. In addition to having a relatively short learning curve, immersion ultrasound is much less limited by media density (e.g. posterior subcapsular cataract) and the technician expertise than optical methods.But for the eyes with posterior staphyloma, the optical methods were considered to be superior than ultrasound methods because of the former can more precise localization of the fovea. Our results showed that the highly correlation(r>0.9 for all comparisons) among the three techniques for AL measurements. No statistically significant differences were found among the three techniques for all eyes (P>0.05). Our results are accord with prior studies comparing ultrasound methods with optical methods[4,13]. Different techniques had been compared in health, cataract, pseudophakic, aphakic, and silicon oil- filled eyes, and the results are comparable between techniques[9,14-17]. Although coherence reflectometry is simple and easy to operate (e.g. IOLMaster and Lenstar), the limitation could not be ignored. It had been reported that the IOLMaster and Lenstar LS 900 had similar, for AL measurement, failure rates for cataractous eyes due to refractive medium opacity[18].Compared with optics method, the ultrasound method is less influenced by condition of refractive medium[19], of which the contact A-ultrasound is most widely used in clinic. However,due to the fusion of ultrasound probe wave and cornea wave,the contact A-ultrasound could not identify the primary wave representing the corneal apex, which might get shorter AL than actual situation. On the other hand, the contact A-ultrasound could compress the cornea, and the result of AL was underestimate by 0.14 to 0.47 mm compared to immersion ultrasound techniques[20-21]; additionally, study has shown that an error of 100 μm in AL measurement could result in 0.28 D of postoperative refractive error[22]. Our results showed good agreement between the three methods and the MD in AL measurements with narrow 95% LoA.
Lenstar LS 900 optical biometer, with an 820-mm super luminescent diode, is based on OLCR technology[4]. Because optical characteristic of 820-mm super luminescent diode,eyes with serious refractive medium opacity, it cannot obtain the measurements of AL[23]. In order to solve this problem, the immersion method came into being, which could eliminate the pressure of probe on cornea and interference of probe wave, including IA and IB biometry[24]. Compared with IA,IB has its intrinsic advantage: biometry parameters of IA are based on waveform and amplitude, which could only provide one-dimensional image, also difficult to precisely judge real AL. In contrast to this, IB could provide real-time two-dimensional images, the position of refracting media could be identified directly, which could get more accurate biometry results than IA, especially when refractive medium appeared membraniform opacity[25]. In our study, Lenstar LS 900 could not get measurements of AL for some cataract patients.Especially in cataracts with posterior subcapsular opacification,no determinable signal was reflected. By analysing the causes of failure, we hope to provide guidance for ophthalmologists to choose reasonable examinations in the future.
In conclusion, measurements with the OLCR correlated well with IB and IA. But in the eyes with serious refractive medium opacity, the measurements of AL could not be achieved or existed deviations when using OLCR device. But IB could give us two-dimensional image, including the information of morphology and position of intraocular tissues, especially under the condition of refractive medium opacity, it might provide more reliable result.
ACKNOWLEDGEMENTS
For statistical analysis and experimental design, we acknowledge Zheng Zhao (Scientific Education Section of Tianjin Eye Hospital) and also would like to thank Ai-Ping Li (Equipment Division of Tianjin Eye Hospital) for maintenance of equipment.
Foundation: Supported by the Key Projects of the Bureau of Health, Tianjin (No.2015KR05).
Conflicts of Interest: Li Y, None; Li HX, None; Liu YC,None; Guo YT, None; Gao JM, None; Wu B, None; Zhang N, None; Liu D, None; Yuan XY, None.
REFERENCES
1 Sheard R. Optimising biometry for best outcomes in cataract surgery.Eye (Lond) 2014;28(2):118-125.
2 Kane JX, Van Heerden A, Atik A, Petsoglou C. Intraocular lens power formula accuracy: comparison of 7 formulas. J Cataract Refract Surg 2016;42(10):1490-1500.
3 Ademola-Popoola DS, Nzeh DA, Saka SE, Olokoba LB, Obajolowo TS. Comparison of ocular biometry measurements by applanation and immersion A-scan techniques. J Curr Ophthalmol 2015;27(3-4):110-114.
4 Buckhurst PJ, Wolffsohn JS, Shah S, Naroo SA, Davies LN, Berrow EJ.A new optical low coherence reflectometry device for ocular biometry in cataract patients. Br J Ophthalmol 2009;93(7):949-953.
5 Hoffer KJ. Ultrasound velocities for axial eye length measurement. J Cataract Refract Surg 1994;20(5):554-562.
6 Holladay JT. Standardizing constants for ultrasonic biometry,keratometry, and intraocular lens power calculations. J Cataract Refract Surg 1997;23(9):1356-1370.
7 Abu El Einen KG, Shalaby MH, El Shiwy HT. Immersion B-guided versus contact A-mode biometry for accurate measurement of axial length and intraocular lens power calculation in siliconized eyes. Retina 2011;31(2):262-265.
8 Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986;1(8476):307-310.
9 Rohrer K, Frueh BE, Walti R, Clemetson IA, Tappeiner C, Goldblum D. Comparison and evaluation of ocular biometry using a new noncontact optical low-coherence reflectometer. Ophthalmology 2009;116(11):2087-2092.
10 Nemeth G, Nagy A, Berta A, Modis L Jr. Comparison of intraocular lens power prediction using immersion ultrasound and optical biometry with and without formula optimization. Graefes Arch Clin Exp Ophthalmol 2012;250(9):1321-1325.
11 Haigis W, Lege B, Miller N, Schneider B. Comparison of immersion ultrasound biometry and partial coherence interferometry for intraocular lens calculation according to Haigis. Graefes Arch Clin Exp Ophthalmol 2000;238(9):765-773.
12 Hoffer KJ. Clinical results using the Holladay 2 intraocular lens power formula. J Cataract Refract Surg 2000;26(8):1233-1237.
13 Santodomingo-Rubido J, Mallen EA, Gilmartin B, Wolffsohn JS. A new non-contact optical device for ocular biometry. Br J Ophthalmol 2002;86(4):458-462.
14 Holzer MP, Mamusa M, Auffarth GU. Accuracy of a new partial coherence interferometry analyser for biometric measurements. Br J Ophthalmol 2009;93(6):807-810.
15 Cruysberg LP, Doors M, Verbakel F, Berendschot TT, De Brabander J,Nuijts RM. Evaluation of the Lenstar LS 900 non-contact biometer. Br J Ophthalmol 2010;94(1):106-110.
16 Cinar Y, Cingu AK, Sahin M, Sahin A, Yuksel H, Turkcu FM, Cinar T,Caca I. Comparison of optical versus ultrasonic biometry in keratoconic eyes. J Ophthalmol 2013;2013:481238.
17 Nemeth J, Fekete O, Pesztenlehrer N. Optical and ultrasound measurement of axial length and anterior chamber depth for intraocular lens power calculation. J Cataract Refract Surg 2003;29(1):85-88.
18 McAlinden C, Wang Q, Pesudovs K, Yang X, Bao F, Yu A, Lin S, Feng Y, Huang J. Axial length measurement failure rates with the IOLMaster and Lenstar LS 900 in eyes with cataract. PLoS One 2015;10(6):e0128929.
19 Yang Q, Chen B, Wang L, Li Z, Huang Y. Diagnostic accuracy of the immersion high-frequency B-scan ultrasonography in chemical injured eyes. Zhonghua Yan Ke Za Zhi 2014;50(8):589-592.
20 Trivedi RH, Wilson ME. Axial length measurements by contact and immersion techniques in pediatric eyes with cataract. Ophthalmology 2011;118(3):498-502.
21 Schelenz J, Kammann J. Comparison of contact and immersion techniques for axial length measurement and implant power calculation. J Cataract Refract Surg 1989;15(4):425-428.
22 Olsen T. Theoretical approach to intraocular lens calculation using Gaussian optics. J Cataract Refract Surg 1987;13(2):141-145.
23 Srivannaboon S, Chirapapaisan C, Chonpimai P, Loket S. Clinical comparison of a new swept-source optical coherence tomography-based optical biometer and a time-domain optical coherence tomography-based optical biometer. J Cataract Refract Surg 2015;41(10):2224-2232.
24 Turhan SA, Toker E. Predictive accuracy of intraocular lens power calculation: comparison of optical low-coherence reflectometry and immersion ultrasound biometry. Eye Contact Lens 2015;41(4):245-251.
25 Yang Q, Chen B, Peng G, Li Z, Huang Y. Accuracy of immersion B-scan ultrasound biometry in high myopic patients with cataract.Zhonghua Yan Ke Za Zhi 2014;50(1):32-36.