INTRODUCTION
X-linked retinoschisis (XLRS; OMIM: 312700) is a relatively common early onset retinal degenerative disease that affects males early in life[1]. XLRS may spontaneously regress or may be stationary or progressive.Roughly 20%[2] of all patients with XLRS may progress to retinal detachment (RD), and in up to one third of such patients[3],vitreous hemorrhage (VH) develops, which causes severe vision loss. Until now, no satisfying treatment has been available to halt the formation and development of schisis in patients with XLRS[4]. Surgical interventions are required for XLRS patients with severe complications such as RD and VH. In the fundus, different phenotypes are described:macular foveal schisis is regarded as the most typical change,radially oriented intraretinal foveomacular cysts are seen in a spoke-wheel configuration. In addition, approximately 50% of all cases have peripheral retinoschisis[1,3,5], some of which threatening the macula area around fovea. The optical coherence tomography (OCT) shows the splitting of retina usually located at the inner nuclear layer (INL), outer plexiform layer and outer nuclear layer (ONL), with small cystic spaces between the split retinal layers in the perifoveal region[6]. Do different phenotypes lead to different incidences of complications and prognosis? Our study aimed to examine a group of XLRS patients who underwent vitreoretinal surgery because of the severe complications with progressive XLRS.In the present study, we analyze the relationship of severe complications incidence rate and different phenotypes based on a modified classification scheme[7-8] according to its fundus and OCT image of XLRS. Our indications for surgery are discussed, and the results of our treatment are reported.
SUBJECTS AND METHODS
This was a retrospective study of 31 eyes of 25 patients treated with vitrectomy who were diagnosed with XLRS and suffered from severe complications. We retrospectively reviewed all of the case notes of children with XLRS who underwent vitreoretinal surgery in our department from March 2009 to March 2015, identifying 31 consecutive eyes. Patients were excluded if the follow-up was less than 1y. A total of 31 eyes were enrolled in this study from Shanghai Jiao Tong University Affiliated with XinHua Hospital (Shanghai). We confirmed XLRS based on clinical evidence, including patient symptoms,fundus changes, OCT, fluorescein fudus angiography (FFA),and electroretinography (ERG). Diagnostic criteria including:1) age of onset is under 15 years old; 2) severe impact in best corrected visual acuity (BCVA) (<20/60); 3) OCT images show the foveal cystic schisis, macular lammellar schisis with or without peripheral schisis; 4) ERG shows selectively reduced b wave. FFA results amplitude confirming the diagnosis.Baseline clinical characteristics and demographic data were collected from the medical records and included sex, age, eye examinations, diagnosis, and treatment. Preoperative data were obtained at the visit prior to surgical treatment and included BCVA, slit-lamp and both direct and indirect ophthalmoscopy,ERG and OCT. According to the presurgery results on ophthalmoscope and OCT, all of the eyes were divided into 4 groups based on a modified classification scheme[7-8], in which there were typical changes in fundus and/or in OCT. In the fundus, radially oriented intraretinal foveomacular cysts are seen in a spoke-wheel configuration in most cases (Figure 1),whereas OCT shows the most extended foveal schisis, with large, low, reflective cysts which are surrounded perifoveally by many smaller cysts, located in the INL and another deeper schisis appearing in the photoreceptolayer (Figure 2). The vascular changes were remarkable, appearing as extensive vascular sheathing in some cases (Figure 3). The incidence of preoperative complications was also analyzed preoperatively in the four different groups. Besides the cases when the complication occurred affect the result of OCT, we chose the data when it was first diagnosed.
The surgical procedures were all performed by one surgeon(Zhao PQ). All of the patients underwent pars plana vitrectomy without lensectomy associated with internal limiting membrane peeling. Photocoagulation was applied to the retinal holes and degeneration areas. Gas or silicone oil was used to fill the eyes in different situations. After surgery, the patients were reviewed at 1, 3 and 6mo, and further surgical interventions were performed when required.
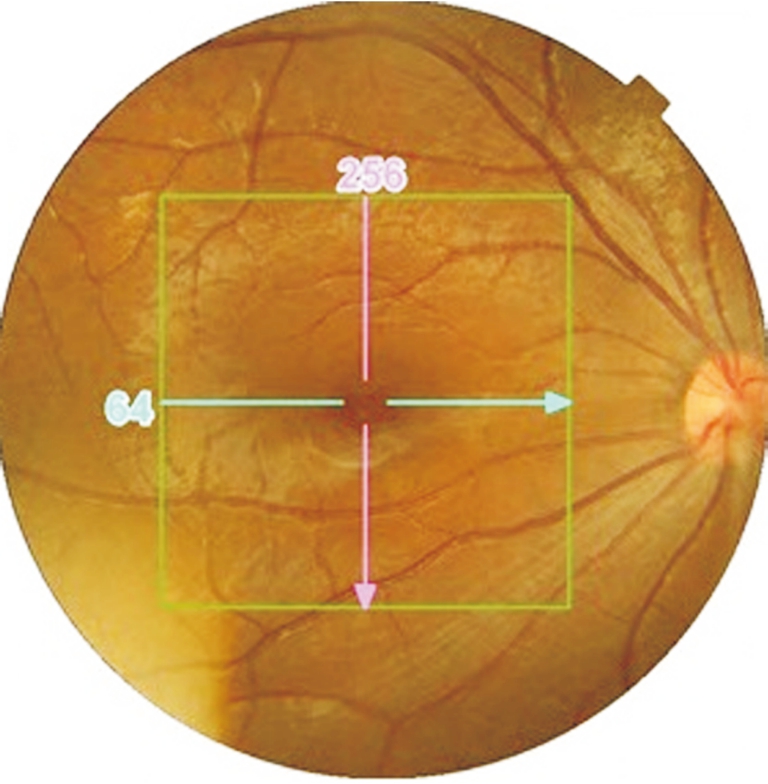
Figure 1 Fundus photograph of a patient in group A showing foveal schisis with a spoke-wheel pattern.

Figure 2 Topcon Dri-OCT image of a patient in group D showing foveal cystic retinoschisis in two different retinal layers.
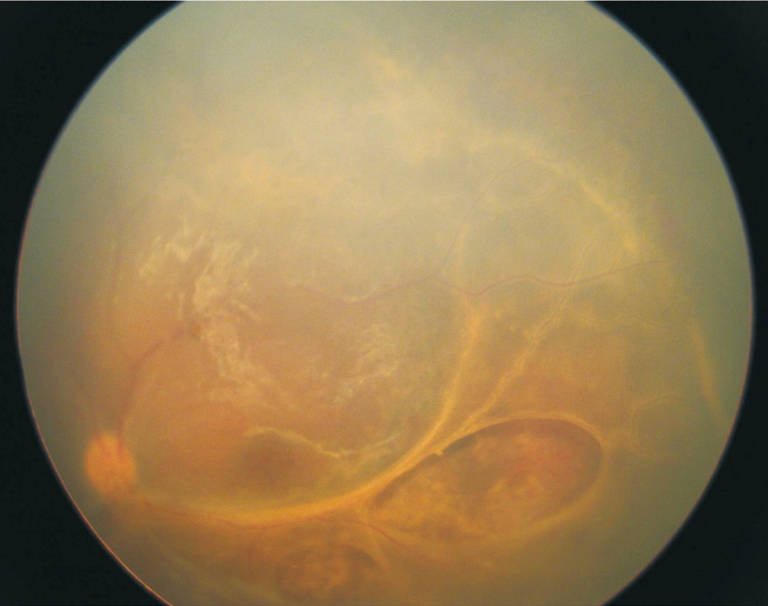
Figure 3 Fundus photograph of an XLRS patient in group D.Vascular changes are remarkable, appearing as extensive vascular sheathing.
We then obtained data from the postoperative clinical assessments and at each follow-up visit. BCVA, slit-lamp and direct and indirect ophthalmoscopy and OCT were performed in all of the participants at every visit after surgery (6 and 12mo follow-ups), at which we obtained information about visual function and anatomical replacement. At the last visit(12mo), we separated the patients into 4 groups. We calculated BCVA with a Snellen chart transferred the light perception(LP), hand move, and finger count to 1/800, 1/400, and 1/200,respectively, using statistics[9]. We compared the preoperative results and the data from 12-month follow-up visit by mean±standard deviation. “Favorable” outcomes were reported when BCVA increased by one line or more. Anatomically, the area of schisis was calculated by OCT, and we compared the preoperative and postoperative results; “favorable” outcomes were reported when the retina was flat when examined byophthalmoscope. The paired sample t-test, in SPSS statistical software, version 13.0 (Chicago, IL, USA), was used to compare the preoperative and postoperative data. P values of 0.05 or less were considered statistically significant.
Table 1 Classification scheme of XLRS mean±SD
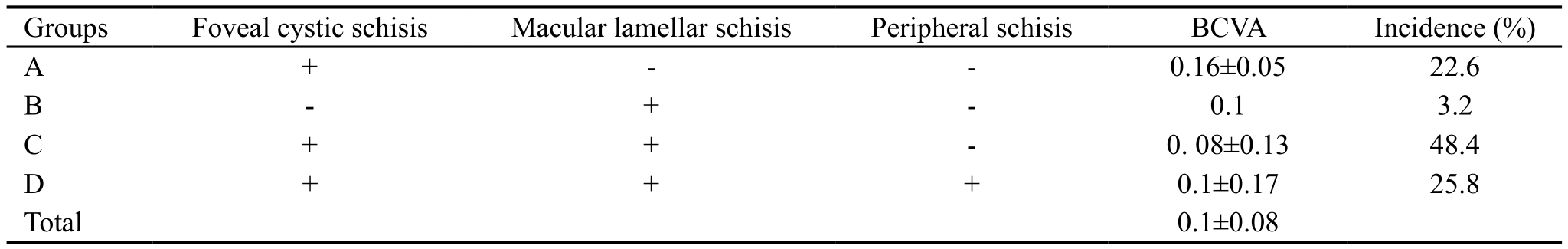
BCVA: Best corrected visual acuity.
RESULTS
All 25 of the patients were male (100%), and the mean age at presentation was 7.47 years old (range 5 to 15y). Among the 31 eyes, there were 7 eyes with VH, 8 eyes with RD and VH,and 16 eyes with rhegmatogenous retinal detachment (RRD).The presurgical BCVA was from LP to 0.25, and the mean was 0.1±0.08. According to the results of ophthalmoscopy and OCT, peripheral retinoschisis occurred in 8 eyes (25.8%),whereas foveal involvement was present in all of the affected patients (Table 1). In these 8 eyes, peripheral retinoschisis presented as a sharply delineated detachment of the inner retinal sheath, limited to the periphery or mid-periphery;2 of these 8 eyes presented several internal splits in the retina, which generated to vitreous veils. The incidence of complications preoperatively, respectively, in the four different groups is shown in Table 2. The most impressive outcome was that VH occurred in 5 of 8 eyes in group D (62.5%).
The mean follow-up period in this study was 37.2mo (range 12 to 58mo) and we recorded the data when 12-month after surgery as the last visit. After surgery, the patients achieved clear refractive media and good retinal replacement. At the last visit, 23 eyes (74.2%) had a “favorable” outcome with better visual acuity. Among these 23 eyes, 5 eyes were treated with photocoagulation before surgery because of the progressive extent of schisis; and dam-type endolaser was done for peripheral retinal holes and retinoschisis areas on 3 eyes in group D during the surgery (Figure 4). In this study, postoperative BCVA, anatomical replacement and the incidence of secondary complications were also reported(Table 3). The postoperative BCVA of our 31 eyes was significantly better in all of the four groups, with a mean final BCVA of 0.27±0.11. The difference was significant (t=-1.049, P=0.000), compared with the BCVA before surgery(0.1±0.08). Among the 8 eyes rated “unfavorable”, 3 eyes in group C and D were treated with a second vitreoretinal surgery because of tractional RD recurrence after the first surgery. The second surgeries in theses 3 eyes were performed successively at the 10, 12 and 15mo follow-ups, respectively. However,according to the postoperative BCVA, they were considered“unfavorable”.
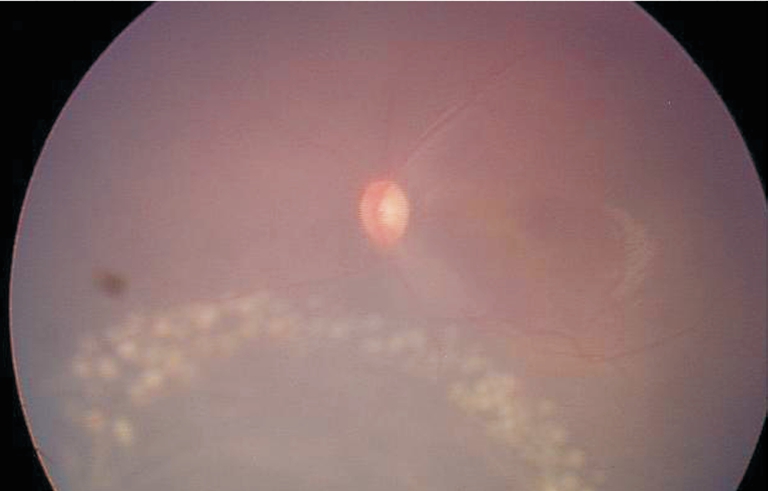
Figure 4 It was necessary to apply dam-type endolaser to the peripheral retinoschisis areas (one case in group D).
Table 2 Preoperative complications incidence n (%)
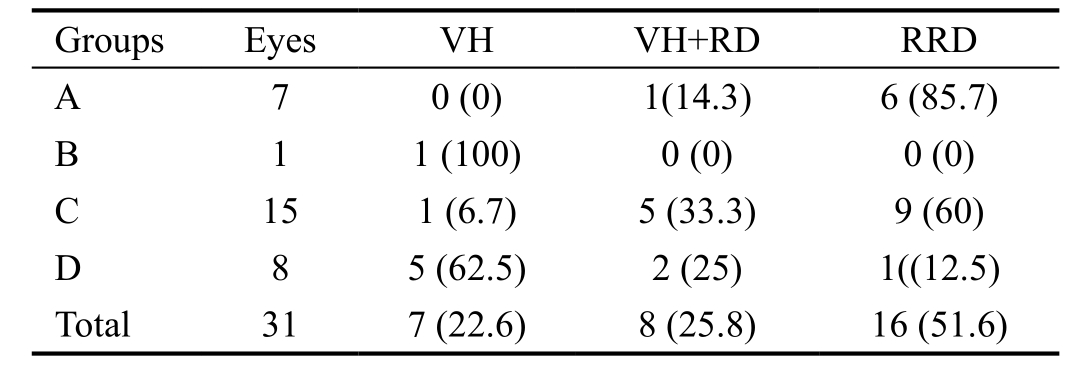
VH: Vitreous hemorrhage; RD: Retinal detachment; RRD:Rhegmatogenous retinal detochment.
Table 3 BCVA and retinal anatomical replacement n (%)
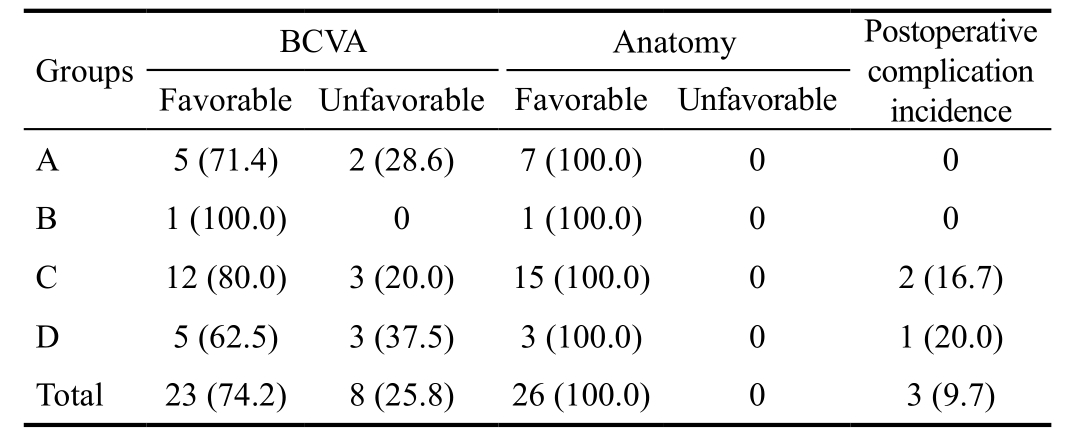
BCVA: Best corrected visual accity.
DISCUSSION
XLRS is one of the most common X-linked, recessively inherited, bilateral, blindness-inducing diseases. It is limited almost exclusively to male subjects[8]. The differential diagnosis of XLRS essentially depends on the stage of the disease.XLRS can be progressive or stationary, or it can spontaneously regress. In most cases, it remains static. However, it will lead to blindness if severe complications occur. In this study, we focused on XLRS stages suffering severe complications.The incidence of VH was approximately 50% (including RD+VH). VH can be seen in retinopathy of prematurity (ROP),intracranial hemorrhage, thrombophilic diseases, or retinal dysplasia[10-11]. The most important differential diagnosis is ROP. Patients with ROP will have a history of premature delivery and perinatal complications, and they will develop vascularization of the retinal periphery in the majority of eyes after involution of the disease[12-13]. In comparison, intraschisis or VH in XLRS results from the rupture of unsupported retinal vessels or rarely from neovascularization. Therefore, we do not use anti-VEGF drugs as we do in ROP before surgery. It is not difficult to distinguish these diseases, especially by using gene detection. Because the genotypes of XLRS have no significant connection with phenotype, we believe that the latter is more practical than the former. Furthermore, spectral domain OCT allowed high-resolution imaging and characterization of the features in XLRS, and it highlighted the variability of the same genetic disease[14]. Therefore, in this study, we chose to divide the eyes into 4 groups by phenotype, according to typical characteristics on fundus and OCT images.
The etiology of XLRS is unclear[15], but the vitreous dystrophy theory, the Müller cell theory of defects and the retinal vascular dystrophy theory are often mentioned. Due to inherited dystrophy in the interior retina, especially in the Müller cells or in the vitreous cortex, the interior retina is detached from the retinal nerve fiber layer (RNFL); thus, the incidences of secondary detachment and VH are 5% to 20%and 33%, respectively. Once these complications occurs,XLRS becomes a vision-threatening disease that requires early surgery in the majority of cases[2,16-17]. We found in this study that the eyes with the complication of VH were all in group D(combined peripheral schisis). With the presence of peripheral retinoschisis in the RNFL, vascular changes were prominent in these cases. The retinal vessels could remain running freely through the vitreous cavity if the inner sheet of the schisis degenerated. The extensive vascular sheathing with dendritic opacified retinal vessels; but no clear retinal neovascularization was found in our cases. The investigators believed that in some instances, VH was caused by traction on the retinal blood vessels[18]. Other less common signs of vitreous traction were tenting of the inner retinal layer (12%) or blood vessels (4%)and geographic areas of white without pressure (35%)[19]. Because the sample size of this study was small, we should perform more studies to confirm the presumptions about the relevance of peripheral schisis and VH. However, it would help to perform FFA of the peripheral schisis to provide the correct diagnosis and treatment.
During the course of XLRS, secondary complications,including RD and VH, can occur and may lead to poor outcomes. Thus, which phenotype of XLRS is the most dangerous and most easily causes severe complications? Our study aimed to study cases with severe complications, with foveal involvement occurring in 96.8% of eyes, whereas Wille[20] reported that macular retinoschisis occurred in all affected patients. In our report, foveal retinoschisis was present in 98% of involved individuals. Peripheral retinoschisis,which is characterized by intraretinal splitting involving the nerve fiber layer[1,21], occurred in approximately 25.8% of eyes (group D), which is less than the 50% that Pachydaki and Young[22] reported. In our study, the inner layer of the peripheral schisis was immobile and elevated in a stable configuration. In only one case, the original area of detachment was caused by a combination of inner and outer layer holes in areas of retinoschisis. Using primarily scleral buckling,external drainage of subretinal fluid was popular for treating RRD in XLRS. However, currently, this technique is usually performed only for more peripheral breaks. Considering that scleral buckling cannot relieve the traction on the retina thoroughly as well as the limitations of globe growth, we prefer vitrectomy[4], especially if the outer-layer holes are large and posterior. At the same time, inner layer retinotomy, internal drainage of schisis fluid and subretinal fluid, internal limiting membrane peeling, endolaser, gas-fluid exchange with longacting gases and postoperative positioning of the patient, and use of heavy per fluorocarbon liquids to tamponade the schisis and detachment were used during surgery. It is clear that a variety of surgical techniques have yielded successful results,although it is also obvious that the best method for treating RRD associated with XLRS has not yet been determined. As we know, a perfect internal limiting membrane peel plays an important role in relieving the traction on the retina[23-25]. As we showed in this study, successful vitreoretinal surgery in these affected eyes led to good outcomes. To achieve better BCVA in children, lens-sparing vitrectomy, combined with internal limiting membrane peeling, was performed in every case. Luna et al[26] reported that peripheral retinal laser photocoagulation before lens-sparing vitrectomy for ROP eyes affected surgical outcomes. We also believe that it would work in XLRS. In our study, 5 eyes underwent photocoagulation before surgery.During the surgery, the surgeon considered it difficult to manipulate the vitreous in the eyes that underwent pre-surgical laser photocoagulation, although all of them had “favorable”outcomes. We also had 8 eyes in which BCVA did not improve after surgery. Among these 8 eyes, 6 (75%) had foveal cystic schisis pre-surgically. We believe the bad outcomes were also related to repeated surgeries and to long-term detachment,which leads to photoreceptor apoptosis[27].
We also had 3 cases that underwent a second surgery, all in groups C and D, in patients with foveolamellar changes.Because it is the most changeable phenotype, we should pay greater attention to it and undertake longer follow-ups.Although a perfect internal limiting membrane peeling was important in these two groups, dam-type endolaser was necessary for peripheral retinal holes and retinoschisis areas(mostly in group D), which were effectively prevented from extending to the macula. Furthermore, we will continue to investigate whether photocoagulation can form a barrier against the progression of schisis as soon as we find schisis enlarging toward the posterior. The limitations of our study included its nonrandomized, retrospective design and the potential for selection bias. The sample size was small, which would have increased the likelihood of type II statistical errors. Despite these limitations, we found significant BCVA improvements up to 3y after surgery, so we would like to conduct more research to find the ideal timing for photocoagulation and to estimate its safety and effectiveness.
ACKNOWLEDGEMENTS
Conflicts of Interest: Zhao C, None; Zhang Q, None; Jin HY, None; Zhao PQ, None.
REFERENCES
1 Molday RS, Kellner U, Weber BH. X-linked juvenile retinoschisis:clinical diagnosis, genetic analysis, and molecular mechanisms. Prog Retin Eye Res 2012;31(3):195-212.
2 Sikkink SK, Biswas S, Parry NR, Stanga PE, Trump D. X-linked retinoschisis: an update. J Med Genet 2007;44(4):225-232.
3 Kellner U, Brummer S, Foerster MH, Wessing A. X-linked congenital retinoschisis. Graefes Arch Clin Exp Ophthalmol 1990;228(5):432-437.
4 Yu H, Li T, Luo Y, Yu S, Li S, Lei L, Li J, Ding X, Yuan L, Tang S.Long-term outcomes of vitrectomy for progressive X-linked retinoschisis.Am J Ophthalmol 2012;154(2):394-402.
5 Kjellstrom S, Vijayasarathy C, Ponjavic V, Sieving PA, Andreasson S. Long-term 12 year follow-up of X-linked congenital retinoschisis.Ophthalmic Genet 2010;31(3):114-125.
6 Sborgia L, Recchimurzo N, Niro A, Sborgia G, Funno C, Boscia F,Alessio G. SD-OCT and microperimetric correlated changes inprogressive X-linked retinoschisis after vitrectomy: a case report. Retin Cases Brief Rep 2016;1(1):101-105.
7 Prenner JL, Capone A Jr, Ciaccia S, Takada Y, Sieving PA, Trese MT. Congenital X-linked retinoschisis classification system. Retina 2006;26(7 Suppl):S61-64.
8 Lesch B, Szabóo V, Kanya M, Somfai GM, Vamos R, Varsanyi B,Pamer Z, Knezy K, Salacz G, Janaky M, Ferencz M, Hargitai J, Papp A, Farkas A. Clinical and genetic findings in Hungarian patients with X-linked juvenile retinoschisis. Mol Vis 2008;14(8):2321-2332.
9 Scott IU, Schein OD, West S, Bandeen-Roche K, Enger C, Folstein MF. Functional status and quality of life measurement among opthalmic patients. Arch Ophthalmol 1994;112(3):329-335.
10 Kaur B, Taylor D. Fundus hemorrhages in infancy. Surv Ophthalmol 1992;37(37):1-17.
11 Meier P. Paediatric retinal detachment and hereditary vitreoretinal disorders. Klin Monblr Augenheilkd 2013;230(9):914-919.
12 Connolly BP, McNamara JA, Regillo CD, Tasman W, Sharma S.Visual outcomes after laser photocoagulation for threshold retinopathy of prematurity. Ophthalmology 1999;106(9):1734-1737.
13 Laatikainen L. Presumed vitelliform dystrophy with perimacular flecks and retinal detachment. Int Ophthalmol 1979;1(3):163-170.
14 Leng T. Two cases of X-linked retinoschisis with different spectral domain optical coherence tomography findings. Clin Ophthalmol 2012;6:1563-1565
15 Tantri A, Vrabec TR, Cu-Unjieng A, Frost A, Annesley WH Jr, Donoso LA. X-linked retinoschisis: a clinical and molecular genetic review. Surv Ophthalmol 2004;49(2):2l4-230.
16 Garcia-Arumi J, Corcostegui IA, Navarro R, Zapata MA, Berrocal MH. Vitreoretinal surgery without schisis cavity excision for the management of juvenile X linked retinoschisis. Br J Ophthalmol 2008;92(11):1558-1560.
17 Campbell JP, Skalet AH, Lauer AK. Vitreous veils associated with congenital x-linked retinoschisis. JAMA Ophthalmol 2015;133(8):151-155.
18 Cruzinigo YJ, Acaba LA, Berrocal MH. Surgical management of retinal diseases: proliferative diabetic retinopathy and traction retinal detachment. Dev Ophthalmol 2014;54:196-203.
19 Schulman J, Pevman GA, Jednock N, Larson B. Indications for vitrectomy in congenital retinoschisis. Br J Ophthalmol 1985;69(7):482-486.
20 Wille H. A family with vitreo-tapeto-retino-choroidal degeneration with dominant trasmission. Acta Ophthalmol (Copenh) 1980;58(1):148-157.
21 Al-Swaina N, Nowilaty SR. Macular hole in juvenile X-linked retinoschisis. Saudi J Ophthalmol 2013;27(4):283-286.
22 Pachydaki SI, Young LH. Genetic of hereditary vitreoretinal degenerations. Selmin Ophthalmol 2007;12(4):219-227.
23 Clark A, Balducci N, Pichi F, Veronese C, Morara M, Torrazza C,Ciardella AP. Swelling of the arcuate nerve fiber layer after internal limiting membrane peeling. Retina 2012;32(8):1608-1613.
24 Abdelkader E, Lois N. Internal limiting membrane peeling in vitreoretina surgery. Surv Ophthalmol 2008;53(4):368-396.
25 Deltour JB, Grimbert P, Masse H. Deterimental effects of active internal limiting membrane peeling during eperetinal membrane surgery:microperimetric analysis. Retina 2017;37(3):544-552.
26 Luna JD, Caribaux LJ, Reviglio VE, Juarez CP. Lens-sparing surgery for retinopathy of prematurity. Ophthalmology 2003;110(8):1669.
27 Ikeda T, Fujikado T, Tano Y, Tsujikawa K, Koizumi K, Sawa H,Yasuhara T, Maeda K, Kinoshita S. Vitrectomy for rhegmatogenous or tractional retinal detachment with familial exudative vitreoretinopathy.Ophthalmology 1999;106(6):1081-1085.