INTRODUCTION
Uncorrected refractive errors (REs) are the leading cause of low vision and the second cause of blindness worldwide[1] and one of the most important causes of correctable visual impairment[2]. REs affect people of all ages and have been reported in more than 60% of subjects over 40 years of age and in more than 20% of students[3]. About 153 million individuals are visually impaired due to REs, of which 8 million are blind[1]. Blurred vision can be relieved, in most cases, by neutralizing it with spectacles, contact lenses,or refractive surgery. Nevertheless, the high prevalence of REs and the costs of their correction make these conditions a substantial public health and economic problem in many parts of the world[4]. Providing eye care services to the many persons who use or need refractive correction involves substantial expenses[2] and imposes a huge financial burden on societies[5].Studies measuring the economic burden on the society are limited in developed countries[6-11]; thus we aimed to estimate the economic burden of common corrective methods in order to introduce more cost-saving scenarios from patients’perspective.
SUBJECTS AND METHODS
This investigation is a study of 120 RE patients of at least 23 years of age and free of any comorbidity was collected by consecutive sampling from those referring to Farabi Eye Hospital, a third level center in Iranian referral system. The sample comprised who underwent refractive surgery 18mo before enrollment. This time was chosen to ensure follow-up was complete, there were no more related costs, and clinical outcomes were stable. Mean of both pre- and postoperativedecimal best spectacle corrected visual acuity of the patients were 1.0 and mean pre- and postoperative decimal uncorrected visual acuity were 0.32 and 0.8, respectively. Also, none of these patients had used spectacle or contact lens after surgery.This study was adherence to the guidelines of the Declaration of Helsinki and the Ethical Board of Tehran University of Medical Sciences and Iranian Ministry of Health approved the study proposal and we obtained a written free and informed consent from the participants.
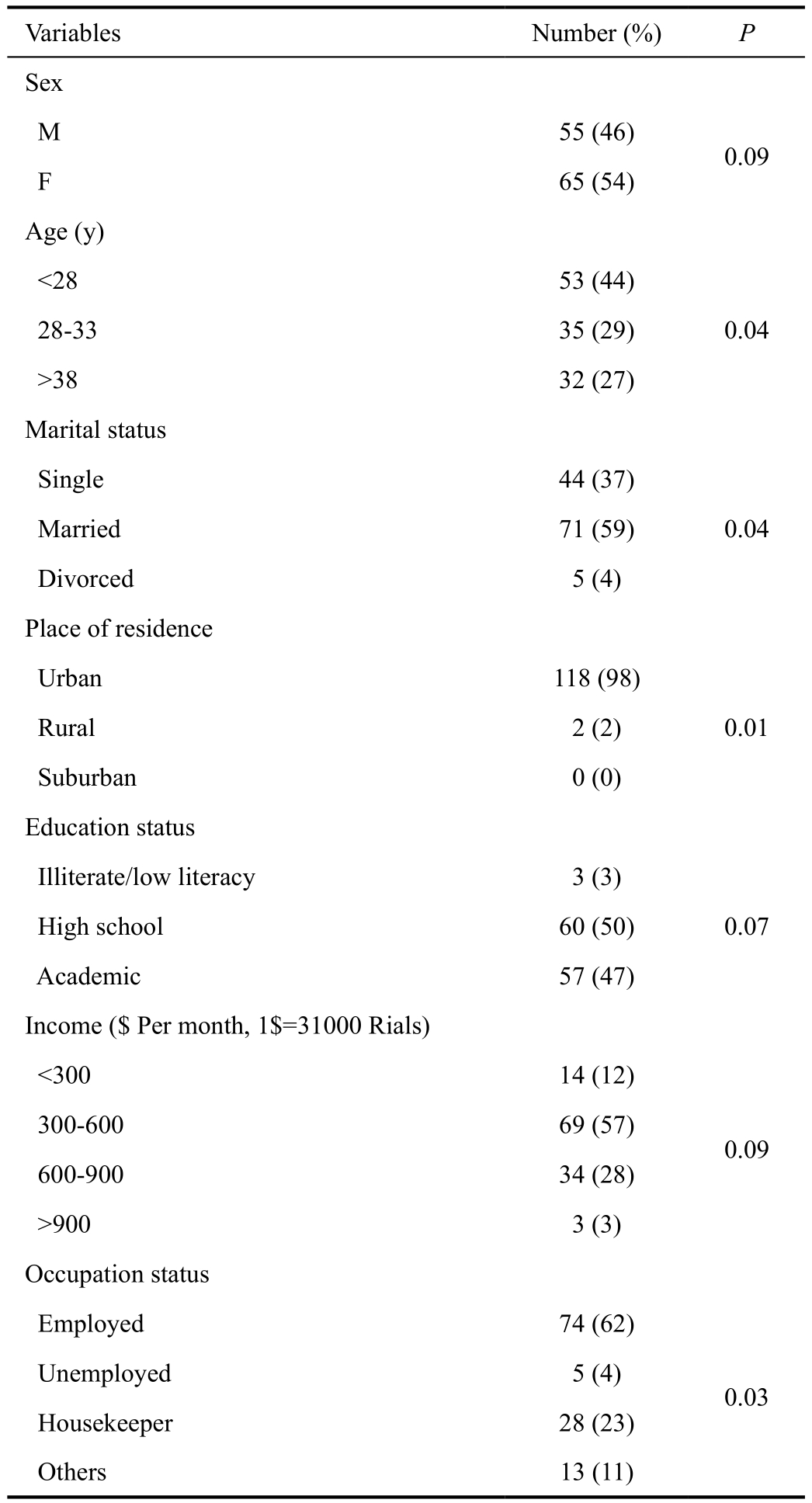
Table 1 Expected value, uncertainty range and distribution types of models parameters among Iranian people with REs

REs: Refrcutive errors; SC: Spectacle; CL: Contact lenses; RS: Refractive surgery; MSE: Mean spherical equivalence.
Studied Conditions and Modalities We studied the imposed costs related to three common corrective methods for REs including spectacles, contact lenses, and refractive surgery,and also their combinations compared with actual spectacles,contact lenses and refractive surgery combined in the society.Contact lenses included soft and hard lenses. RE in the current study was defined as myopia [spherical equivalent refraction less than -0.5 diopter (D)], hyperopia (spherical equivalent more than 0.5 D) and astigmatism (cylinder power of ≥-0.5 D).Based on expert panel opinions, we assumed that refractive surgery is performed between 23 and 35 years old.
In order to obtain a country prevalence rate for myopia,hyperopia, and astigmatism for calculating the economic burden of correction for Iranian RE patients, we performed a systematic review based on 13 published population-based studies by age groups (49 488 cases) in different Iranian provinces that adhered to above cut-offs between 1995 to 2015. We searched Medline, Web of Science, and Cochrane databases as well as the reference lists of retrieved articles to identify studies that met the inclusion criteria.
Costs The cost-of-illness (COI) approach was used to assess the individual and social impact of REs[12]. Indirect costs, which is estimated using the human capital approach, determines lost productivity due to the complication, maintenance, repair and travel costs as a measure of patients’ and caregivers’ lost earnings[13]. In this method, we multiplied the number of lost working days attributed to correction scenarios in the average wage of Iranians. The required parameters are shown in Table 1.Future earnings were discounted at 3% level.
We used the below formula to discount the cost values in which, the ‘n’ equal number of intended years and ‘R’ is discounted rate. Present value=Future value/(1+R)n. The bottom-up method was used for assessing direct costs in both one-year and lifetime horizons[14-15]. In this approach, cost estimation is based on the medical resource consumption of the individual patient. Among the three major studied correction methods, the just spectacle is covered by basic insurance.Supplementary insurance policies partly cover refractive surgery costs only for functionally blind patients.
Elements of direct costs include costs incurred for receiving correction, ophthalmologist and optometrist visit fees, drugs,educational courses, and usual follow-ups. For the first three items, we used the 2013 official tariffs for different correction methods fixed by the government, and for latter items, a questionnaire was used.
Study Process After determining and defining cost elements,detailing them, and designing a suitable closed questionnaire,face-to-face interviews were conducted to gather the required data including costs, lost days, complications and insurance coverage related to any studied vision correction method.Required micro and macroeconomic data including health care discount rate as 3%, exchange rate of US dollar (US$)to Iranian Rial (IRR) as 31 000, monthly per capita income as US$648, ophthalmologist and optometrist visit tariffs in public and private sectors, average refractive surgery fee and drug prices were derived from the National Central Bank,the Statistical Center of Iran, and the Ministry of Health. We used expert opinion to estimate the percentage of RE patients receiving refractive surgery. Collected data was entered in EXCEL software (Microsoft Corporation, Redmond, WA,USA) spreadsheets for analysis and computations. In 2014, life expectancy in Iran was 73y[16]. Monte Carlo simulation was used to extrapolate lifetime survival to derive the lifetime REs economic burden after receiving REs cares based on 18mo follow-up results. The basic considered assumptions for this projection, that are applied in our economic base model, are;the studied economic and epidemiological factors including inflation rate, RE prevalence rate and also effectiveness and complication rate of studied modalities will continue in the future as they have behaved in the past[17], clinically recommended age ranges for people with RE disorders is between 21 to 35 years old and also on average, Iranian people for the first time are wearing the spectacle, contact lenses,and undergoing the refractive surgery at 15, 21, and 28 years old, respectively. The detailed data and probabilities about receive, use, follow-up and opportunity costs of spectacles,contact lenses and refractive surgery in Iran are shown in Table 1 that are extracted from the primary analysis of current investigation.
Statistical and Sensitivity Analysis To comparison the means of two and more than two groups, we used Student t-test and one-way ANOVA test statistics, respectively. Also, we applied the Pearson’s Chi-squared test for comparing the differences between frequencies. All P-values quoted were two-tailed and was presumed statistically significant when the values are below 0.05.
To deal with uncertainty about data, deterministic and probabilistic sensitivity analyses were performed. In a deterministic analysis including one and two-way, each sensible parameter of the model was subject to a variation of ±15% and the model,results were compared to the value of the base case. In a deterministic sensitivity analysis type named the optimistic or pessimistic sensitivity analysis, we compared three major studied scenarios in different ages against status quo and also we added the indirect costs to direct costs in a separate analysis and compared these two scenarios. For probabilistic sensitivity analysis and to scaling-up the samples, we used the Monte Carlo simulation with 5000 iterations at each model parameter with 95% confidence interval (CI).
RESULTS
Results showed no significant gender, education and income differences in refractive surgery use, but there were significant differences in favor of younger, urban residents, married and also employed participants (Table 2).
Refractive Error Types, Corrections, and Complications Of the 120 RE patients corrected with refractive surgery,60.83% and 24.17% had myopia and hyperopia, respectively,and the rest of them had astigmatism. About 69.17%, 19.17%and 5.83% of cases had used spectacle, spectacle along with contact lenses, or only contact lenses, respectively, before receiving refractive surgery.
Contact lenses use had the highest complication rate (46.66%)and infection was responsible for half of these cases; rates were 30.83% and 11.32% for refractive surgery and spectacles,respectively. Since the mean age at first use of spectacles,contact lenses, and refractive surgery was 15.5, 21.8 and 28.6y,respectively, lifetime horizons for using them were about 58,52 and 45y, respectively.
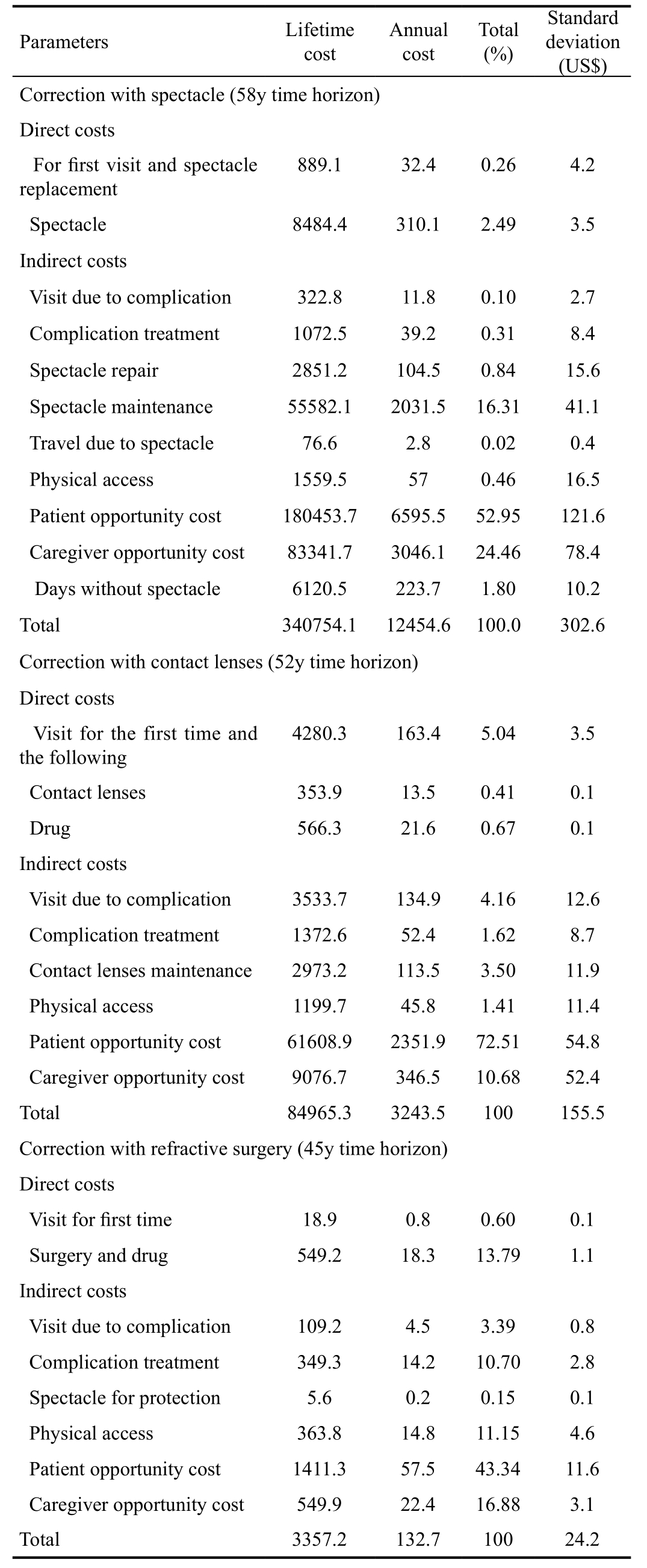
Refractive Errors Correction Costs Correction with spectacle imposes a total direct cost of US$342.5 (±8.41) per year and US$9373.5 (±230.1) per lifetime to each patient. These figures for the contact lenses were obtained US$198.3 (±0.12) and US$5203.1 (±256.3) and for refractive surgery were obtained US$19.1 (±1.2) and US$568.1 (±64.6), respectively (Table 3).Adding the indirect cost to these costs increased incurred yearly total costs by the spectacle, contact lenses, and refractive surgery to US$12454.6, 3243.5 and 132.7 respectively.
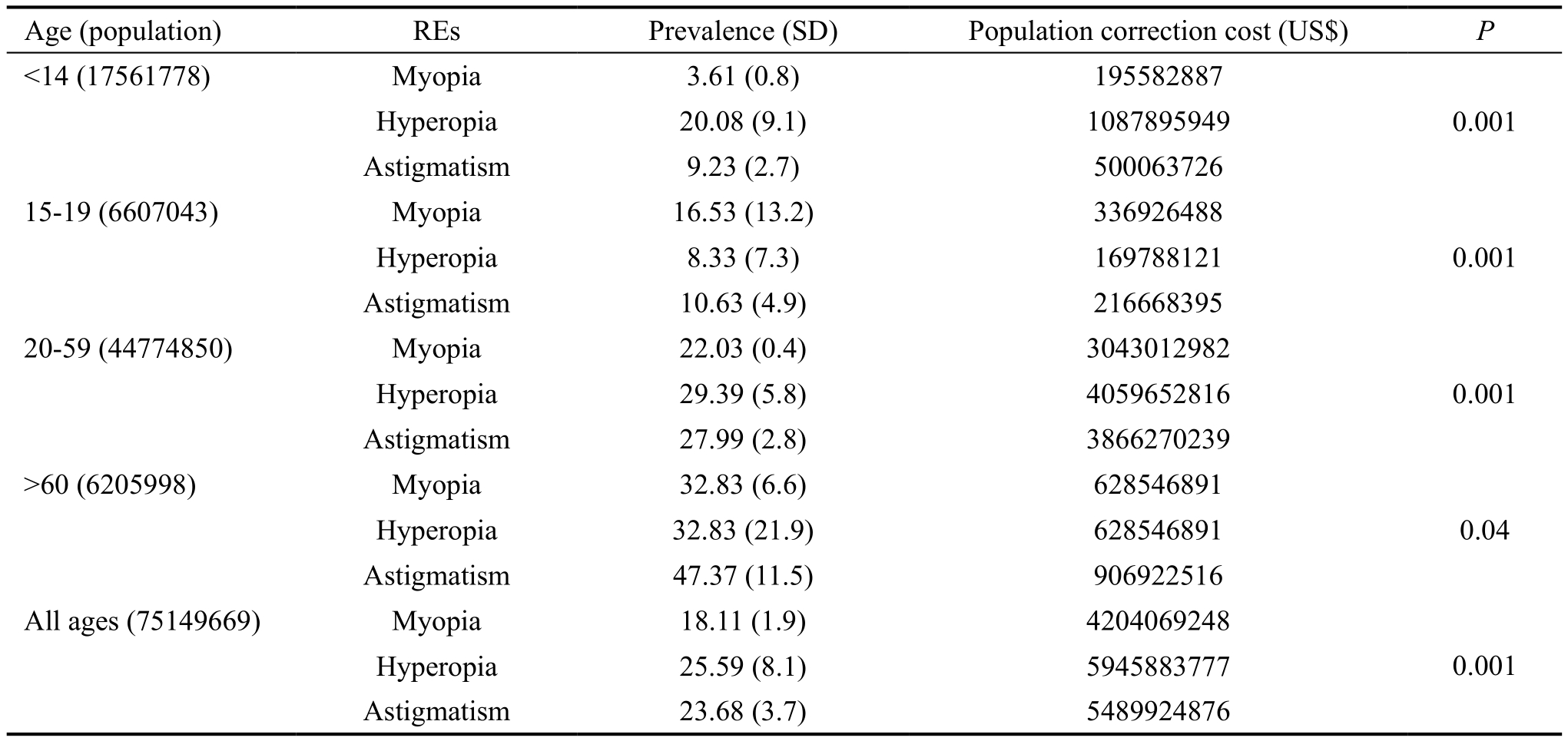
Based on systematic review results presented in Table 4,multiplying the expected total cost for any RE type by patient number provides an estimate of the RE-related ophthalmicexpenditure in 2013. The Iranian population is divided into four groups of elementary and middle school children, high school children, between 20 and 59y, and over 60-yearold patients. Actual annual imposed cost is estimated by a weighted average of correction cost by studied a corrective method which was US$340.3 per patient per year.
Table 2 Demographic characteristic of participants
Overall, based on age-adjusted prevalence rates, astigmatism had the highest share of REs economic burden with a lifetime direct cost of slightly less than US$5.49 billion,while hyperopia and myopia imposed less than US$5.24 and 4.2 billion on patients, respectively. These shares were not the same for all age groups; the economic burden quota was highest in 15-19-year-old with myopia, under 14 and 20-59-year-old groups with hyperopia, and elderly peoples with astigmatism. There were significant differences in the incurred costs among RE types. Overall, the annually imposed cost on each individual Iranian patient with REs is US$308.5.
Table 3 Cost components of REs correction methods
DISCUSSION
The present study was designed to seek the imposed economic burden of different correction modalities on the people with REs. The most interesting finding was that refractive surgery with a high certainty selected as the most cost-saving technique compared with spectacles and contact lenses from the patient’sperspective. This result is completely consistent with those of Javitt and Chiang[18] that showed excimer laser photorefractive keratectomy (PRK) as a refractive surgery method, is a less expensive investment than both daily wear and extended wear soft contact lenses in a 20y’ time period in the United States.
Table 4 Prevalence and population correction direct cost of REs by age groups in Iran
Average adjusted annual direct costs of REs corrections by spectacles and contact lenses were respectively about 18 and 10 times of that for refractive surgery. Given to total costs,in all studied scenarios, the main share of total costs was indirect and they comprised 93.89%, 97.25%, and 91.62%of the total costs associated with contact lenses, spectacles,and refractive surgery, respectively. In contrast to spectacles and contact lenses modalities, refractive surgery, a one-time payment is made early on, and then its costs are prorated in all benefited years and finally imposed a lower annual cost on the users. In addition, refractive surgery involves no maintenance,replacement, loss or repair costs which support our results.
Since the vast majority of subjects were urban residents,Iranian rural residents have very little utilization of these services, causes of which should be studied. We also found that refractive surgery utilization significantly correlated with a higher education level and being employed. Also, contrary to our previous assumption, there was no significant relation with income status, so we called it a normal service, not a luxury one. Also, we did not observe a significant difference between two sexes in this regard. The gender and occupation-results are in accord with those obtained by Gupta and Naroo[19].
We observed an inverse relation between utilization rates of different correction methods and their complication rates. The low rate of contact lenses use compared to spectacles could be attributed to the wider range of its complication and severity.Higher education, better financial status and also eye health status can explain using 70% of spectacles in patients with REs.
Overall, based on the 2011 total population in Iran and obtained RE prevalence rates in our systematic review, myopia, hyperopia and astigmatism respectively imposed an average US$4.2, 5.2 and 5.5 billion annually, of which, respectively 15%, 10.6%,and 16.5% is incurred by the elderly, whereas these ratios for elementary and middle school children are 4.6%, 18.3% and 9.1%, and for high school children they are 8%, 2.8% and 3.9%, respectively and rest of the correction cost is imposed on the 20-59-year-old population. Average imposed cost on any Iranian patient with REs was obtained as US$308.5, while this value for Singapore school children was calculated as US$148 in 2009[20].
Deterministic sensitivity analysis showed that discount rate,the percentage of contact lenses use, initial age at receiving refractive surgery, and productivity loss due to refractive surgery were the key variables that had the highest impact on the total cost of different studied scenarios. The annually imposed cost ranges between US$125.3 and 796 with a 2%change in discount rate. One day variation in productivity loss due to refractive surgery increases the total cost range from US$170.9 to 285. In measuring the actually imposed cost by all three correction methods, the percentage of patients receiving refractive surgery had an important effect on the incurred cost by the Iranian society such that a 7% change in refractive surgery rate among patients leads to a US$ 54 difference of US$ 340.3.
Starting with spectacles and switching to contact lenses as early as eligible imposes the highest cost on patients with REs.The total cost of this expensive and pessimistic scenario was US$431.3. The lowest cost, US$43.1 was when patients started with spectacles and received refractive surgery as early as eligible which is our optimistic scenario. Costs are high when the only spectacles are used; this cost increases when contactlenses use is added while it can be addressed if replaced through refractive surgery. The patients use a combination of methods, and at present, Iranian patients spend US$340.3 per year and US$9310.65 per lifetime for the treatment of REs.
Table 5 Epidemiological and economic burden of diseases and its components and definitions

YLL: Years of life lost; YLD: Years lost due to disability.
Probabilistic sensitivity analysis indicated that annual correction expenditure per patient by spectacles, contact lenses,refractive surgery, and actual combination of these corrective methods were US$350.5 (95%CI: 348.16-352.84), 184.9 (95%CI: 184.73-185.01), 18.1 (95%CI: 17.96-18.24), and 343.6(95%CI: 341.45-345.75), respectively.
Globally, uncorrected RE imposes approximately 268 838 international million dollars[5]. The burden of myopia has been studied in different countries. In the United States, the annual burden was US$2 billion in 1983[21] and US$4.6 billion in 1994[18] for correcting myopia, and it was US$8.1 billion in 1990 for correcting products such as contact lenses, spectacles and eyeglasses frames for all types of REs[22]. Estimates for Singaporean myopic patients were more than US$248 million[20].Since we included indirect costs and lifetime horizons in the current study, our results are not directly comparable with these studies.
A similar study reported an average cost of US$1707.4 for type 2 diabetes in Iran[23]. In another study, the total annual cost per patient for chronic hepatitis B, cirrhosis, and hepatocellular carcinoma was reported US$3094.5, US$17483 and US$32 958 during 2012, respectively[24]. As shown, REs imposes lower costs in comparison with the mentioned diseases. Rein et al[8] have reported that among major ophthalmic diseases,REs have a higher financial burden in under 60-year-old but rank second in over 60-year-old after cataract develops.Other high ranking ophthalmic diseases, in descending order,were glaucoma, age-related macular edema, and diabetic retinopathy.
Disease imposes not only an economic burden but also an epidemiologic burden that its definitions and components are illustrated in Table 5. Next logical step is identifying the more cost-effective type of refractive surgery, i.e. PRK, laser in situ keratomileusis (LASIK), phakic intraocular lens implants, and refractive lenses. In response to cost questions about using spectacles, contact lenses, and refractive surgery and their observed complications, we were faced with recall bias. In order to minimize its effect, in addition to using the bottomup approach costing, we developed a comprehensive list of potential complications and asked participants to check mark the one they had experienced.
Other limitations of this study are the relatively small sample size and uncertainties regarding variables, were minimized by scaling-up the sample numbers to 5000 subjects through Bayesian-based probabilistic sensitivity analysis. Although we extrapolated the 18mo followed-up cost data to lifetime period, but the findings must be interpreted with caution and considered the underpinned hypothesis. Refractive surgery outcome is generally stabilized during the 6 to 12mo followup (LASIK course is shorter and that of PRK is longer). Longterm studies have shown that the outcome is generally stable in the coming decade[25-27]. So considering an 18mo’ time course postoperative seems to have enough strength to be generalized beyond decades. Valuation of different modalities, in addition to the very direct costs, is influenced by long-term course and stability of the outcome, life expectancy, complication rates,etc. Related rates of complication for instance “corneal ectasia”is much more in younger age refractive surgery. So considering different lifetime horizons change results. But our assumption of over 25 years age and less than 30 seems to have a very good potential for routines of refractive surgery everywhere.
Nonetheless, the current study is the first investigation to measure the burden of an ophthalmic condition in a developing country and introduces a well defined and detailed burden of disease in economic terms. The inclusion of longevity, indirect correction costs and using sensitivity analysis are some other advantages of this study because the direct cost for a short time period alone is more likely to have misleading results.
In conclusion, our observation on the 18mo postoperative course of refractive surgery (which was generalized to the whole life) revealed a huge economic burden of REs on the Iranian society and strongly recommends the refractive surgery as the most cost-saving method to correction of the disorder. This has a loud public health message which needs to be scrutinized by health purchaser, especially health insurances organization.
ACKNOWLEDGEMENTS
The authors would like to thank the Hormoz Chams Research Chair in Public Health Ophthalmology, Farabi Eye Hospital and Eye Research Center, Tehran University of Medical Sciences.
Foundation: Supported partially by Hormoz Chams Research Chair in Public Health Ophthalmology, Allama Tabatabaei Award, National Elite Foundation (http://bmn.ir/).
Conflicts of Interest: Mohammadi SF, None; Alinia C,None; Tavakkoli M, None; Lashay A, None; Chams H,None.
REFERENCES
1 Resnikoff S, Pascolini D, Mariotti SP, Pokharel GP. Global magnitude of visual impairment caused by uncorrected refractive errors in 2004. Bull World Health Organ 2008;86(1):63-70.
2 Vitale S, Ellwein L, Cotch MF, Ferris FL 3rd, Sperduto R. Prevalence of refractive error in the United States, 1999-2004. Arch Ophthalmol 2008;126(8):1111-1119.
3 Ziaei H, Katibeh M, Solaimanizad R, Hosseini S, Gilasi HR, Golba fian F, Javadi MA. Prevalence of refractive errors; the yazd eye study. J Ophthalmic Vis Res 2013;8(3):227-236.
4 Kempen JH, Mitchell P, Lee KE, Tielsch JM, Broman AT, Taylor HR,Ikram MK, Congdon NG, O'Colmain BJ; Eye Diseases Prevalence Research Group. The prevalence of refractive errors among adults in the United States, Western Europe, and Australia. Arch Ophthalmol 2004;122(4):495-505.
5 Smith TS, Frick KD, Holden BA, Fricke TR, Naidoo KS. Potential lost productivity resulting from the global burden of uncorrected refractive error. Bull World Health Organ 2009;87(6):431-437.
6 Taylor HR, Pezzullo ML, Keeffe JE. The economic impact and cost of visual impairment in Australia. Br J Ophthalmol 2006;90(3):272-275.
7 Frick KD, Gower EW, Kempen JH, Wolff JL. Economic impact of visual impairment and blindness in the United States. Arch Ophthalmol 2007;125(4):544-550.
8 Rein DB, Zhang P, Wirth KE, Lee PP, Hoerger TJ, McCall N, Klein R,Tielsch JM, Vijan S, Saaddine J. The economic burden of major adult visual disorders in the United States. Arch Ophthalmol 2006;124(12):1754-1760.
9 Frick KD, Foster A. The magnitude and cost of global blindness: an increasing problem that can be alleviated. Am J Ophthalmol 2003;135(4):471-476.
10 Javitt JC, Zhou Z, Willke RJ. Association between vision loss and higher medical care costs in Medicare beneficiaries: costs are greater for those with progressive vision loss. Ophthalmology 2007;114(2):238-245.11 Wittenborn JS, Zhang X, Feagan CW, Crouse WL, Shrestha S, Kemper AR, Hoerger TJ, Saddine JB. The economic burden of vision loss and eye disorders among the United States population younger than 40 years.Ophthalmology 2013;120(9):1728-1735.
12 Sullivan SD, Ramsey SD, Lee TA. The economic burden of COPD.Chest 2000;117(2 suppl):5S-9S.
13 Kigozi J, Jowett S, Lewis M, Barton P, Coast J. Estimating productivity costs using the friction cost approach in practice: a systematic review. Eur J Health Econ 2016;17(1):31-44.
14 Hodgson TA, Meiners MR. Cost-of-illness methodology: a guide to current practices and procedures. Milbank Mem Fund Q Health Soc 1982;60(3):429-462.
15 Truong TP, Hensher DA. Measurement of travel time values and opportunity cost from a discrete-choice model. Econ J 1985:438-451.
16 Zare H, Gaskin DJ, Anderson G. Variations in life expectancy in Organization for Economic Co-operation and Development countries-1985-2010. Scand J Public Health 2015:43(8):786-795.
17 Armstrong JS. Extrapolation for time-series and cross-sectional data.Principles of forecasting: Springer; 2001:217-243.
18 Javitt JC, Chiang YP. The socioeconomic aspects of laser refractive surgery. Arch Ophthalmol 1994;112(12):1526-1530.
19 Gupta N, Naroo SA. Factors influencing patient choice of refractive surgery or contact lenses and choice of centre. Cont Lens Anterior Eye 2006;29(1):17-23.
20 Lim MC, Gazzard G, Sim EL, Tong L, Saw SM. Direct costs of myopia in Singapore. Eye (Lond) 2009;23(5):1086-1089.
21 Vitale S, Sperduto RD, Ferris FL 3rd. Increased prevalence of myopia in the United States between 1971-1972 and 1999-2004. Arch Ophthalmol 2009;127(12):1632-1639.
22 Levit KR, Lazenby HC, Cowan CA, Letsch SW. National health expenditures, 1990. Health Care Financ Rev 1991;13(1):29-54.
23 Javanbakht M, Baradaran HR, Mashayekhi A, Haghdoost AA,Khamseh ME, Kharazmi E, Sadeghi A. Cost-of-illness analysis of type 2 diabetes mellitus in Iran. PLoS One 2011;6(10):e26864.
24 Kavosi Z, Zare F, Jafari A, Fattahi MR. Economic burden of hepatitis B virus infection in different stages of disease; a report from southern iran. Middle East J Dig Dis 2014;6(3):156-161.
25 O'Brart DP, Shalchi Z, McDonald RJ, Patel P, Archer TJ, Marshall J. Twenty-year follow-up of a randomized prospective clinical trial of excimer laser photorefractive keratectomy. Am J Ophthalmol 2014;158(4):651-663. e1.
26 Guerin MB, Darcy F, O'Connor J, O'Keeffe M. Excimer laser photorefractive keratectomy for low to moderate myopia using a 5.0 mm treatment zone and no transitional zone: 16-year follow-up. J Cataract Refract Surg 2012;38(7):1246-1250.
27 Ide T, Toda I, Fukumoto T, Watanabe J, Tsubota K. Outcome of a 10-year follow-up of laser in situ laser keratomileusis for myopia and myopic astigmatism. Taiwan J Ophthalmol 2014;4(4):156-162.