Dear Editor,
I, Dr. Widya Artini from the Department of Ophthalmology,Faculty of Medicine University of Indonesia, Cipto Mangunkusumo Hospital, would like to submit two case reports on bilateral panuveitis in patients with human immunodeficiency virus (HIV) /acquired immune deficiency syndrome (AIDS).
There has been a gradual increase in the number of HIV-positive patients in Indonesia. It was estimated that there were approximately 697 000 people living with HIV in 2016,and it is assumed that the number will increase gradually over the next years by up to 11.6%[1]. Previous studies have reported that the prevalence of HIV-induced uveitis in the AIDS population was 4%[2-4]. Ocular opportunistic infections are most frequently associated with cytomegalovirus (CMV),syphilis and tuberculosis (TBC) infections in patients with HIV[5-7]. Ocular infection of both syphilis and CMV infections in HIV patients may manifest as panuveitis. We have therefore presented here two cases with similar HIV-related panuveitis managed with timely and thorough investigations which successfully prevented the patients’ loss of vision.
Case 1
A 65-year-old Malay male, complained of acute blurred vision in his right eye during the last week of October 2015.We had no previous record of his ocular history. The patient was known to have a history of controlled arthritis which commenced 5y ago, also of condyloma acuminatum, which was treated 3y ago with the oral antiviral (gancyclovir).
An eye examination revealed that his visual acuity was 1/300 with intraocular pressure (IOP) of 30 mm Hg in the right eye,while in the left eye, his visual acuity was 6/9 with IOP of 14 mm Hg. Slit lamp examination of the right eye revealed conjunctival injection and clear cornea with several round, fine keratic precipitates in the centre of the cornea. It also showed the anterior chamber with cells grade 2 and flare grade 2,posterior synechia, and an immature cataract of the nuclear lens LOCH2 (Figure 1). Examination of the right retina revealed a cloudy vitreous and hazy finding. No inflammation was found in the left eye, however, an immature cataract was detected and the fundus showed that the cup-to-disc ratio was 0.3, while the retinal vascular was within normal limits. Gonioscopy showed that the anterior chamber angle was open in both eyes, while ultrasonography revealed mild haziness (Figure 2). The patient was diagnosed with panuveitis, ocular hypertension of the right eye and cataracts in both eyes.
The right eye was treated with corticosteroid eye drops (prednisolone acetate 1%) every three hours, to control inflammation, beta blocker eye drops (timolol 0.5%) and brinzolamide eye drops twice per day. Oral medication, methylprednisolone 16 mg twice per day was also recommended. Routine blood tests were performed, including TORCH and immunological blood tests for HIV. Chest X-ray, ear, nose, throat (ENT) examination, and immunological and internal medical examinations were also carried out.
On the 5th day, the patient complained that he had lost the vision in both eyes and an eye examination revealed that the visual acuity of both his right and left eyes was 1/300. The IOP were 18 mm Hg (OD) and 15 mm Hg (OS). Results of a biomicroscopy examination of both eyes complied with the results of the previous examination of his right eye, i.e. there was no improvement detected on his right eye.
Fundus examination of both eyes showed hazy vitreous and the retina was cloudy. Paracentesis was performed for polymerase chain reaction (PCR) analysis to detect viral DNA in the aqueous humor of the right eye. During treatment, the patient experienced a viral rash all over his body. The patient returned for a follow-up visit three days later and both the TORCH blood test and HIV test showed positive results. Results also showed high levels of IgM and IgG CMV antibodies. CMV vitreous tap result was also positive with CD4 cell count of 160 cells/µL. A diagnosis of panuveitis caused by CMV and HIV was further established. Additional oral treatment was provided using valganciclovir (valcyte®) with an initial dose of 900 mg daily for three weeks along with highly active antiretroviral therapy (HAART) to suppress HIV infection.Oral steroid was discontinued, however, the application of eye drops was continued.
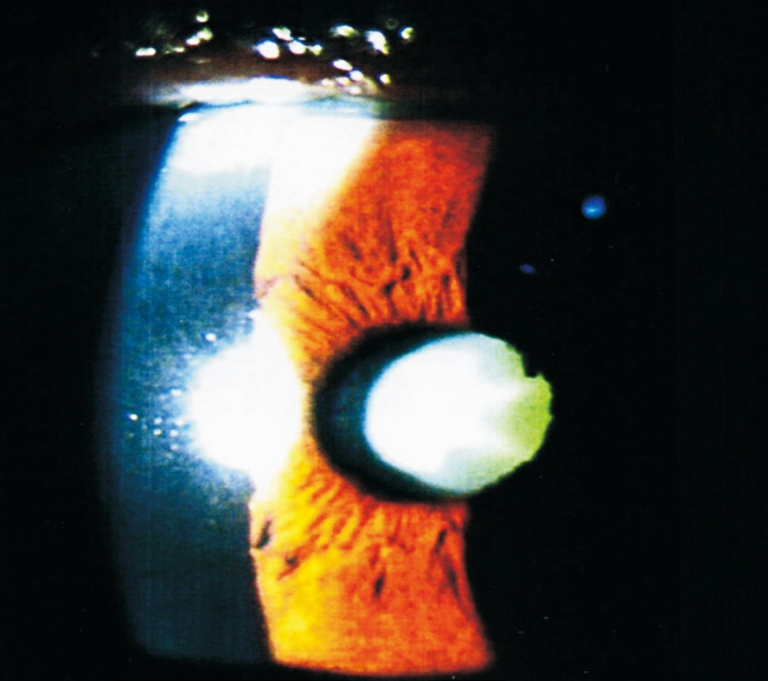
Figure 1 Biomicroscopic examination of right eye central cornea revealed some fine keratic precipitates and posterior synechia.
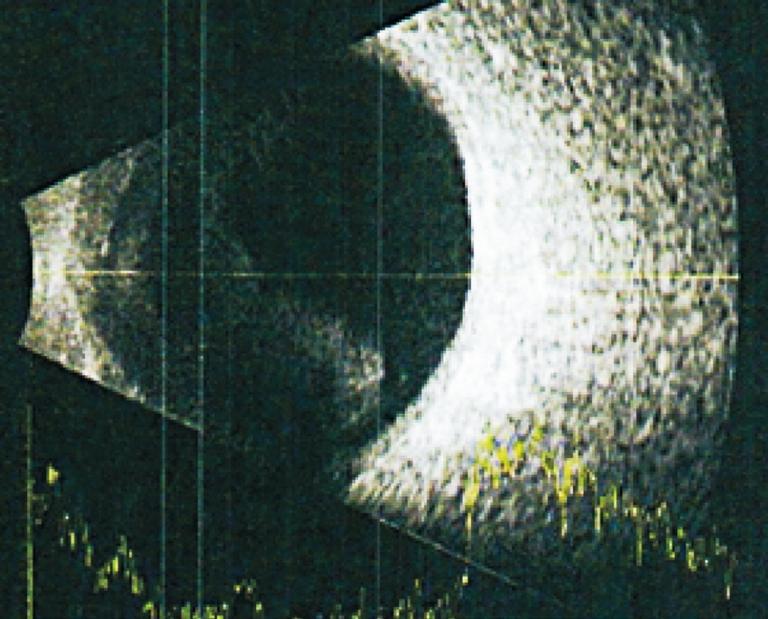
Figure 2 Ultrasound examination of the right eye in posterior segment revealed moderate opacity of vitreous.
Three weeks following the HAART and antiviral treatment,improvement was seen in both eyes. Visual acuity in his right eye was 6/40 with an IOP of 14 mm Hg, while the visual acuity of his left eye was 6/12 with an IOP of 14 mm Hg.Biomicroscopic examination showed a healthy conjunctiva and clear cornea with no cell or flare detected in the anterior chamber. The fundus became clear and cup-to-disc ratio was 0.4 without nasalization. Optical coherence tomography (OCT)examination showed cystoids macular edema (Figure 3). Eye drop steroid medication was reduced to four times per day and timolol treatment discontinued. Nevertheless, valganciclovir was continued at a dose of 450 mg twice per day for a further 20mo. Visual acuity of the right eye remained at 6/40 and in the 3rd month, cataract surgery was performed with good results. The visual acuity improved to 6/7.5, while visual acuity of the left eye returned to 6/7.5. The patient continued with maintenance therapy using efavirenz®, lamivudine® and tenofovir® medications. Panuveitis regressed up to the 20th month follow-up with no flare-up and a CD4 cell count of 500 cells/µL.
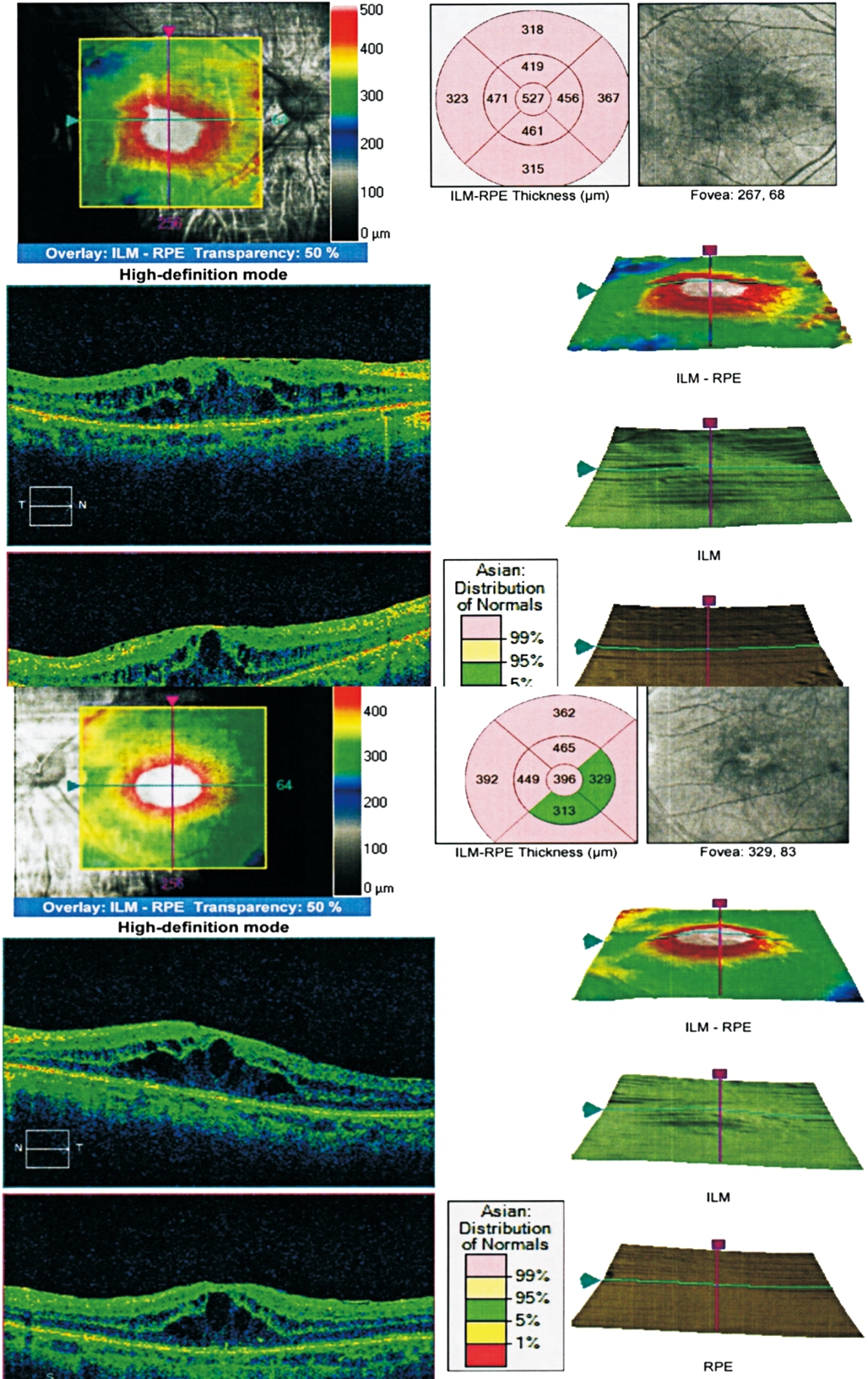
Figure 3 Cystoid macular edema was shown in OCT findings for both eyes three weeks following the HAART and antiviral treatment.
Case 2
A 47 year old married Malay male patient who complained of worsening blurred vision in both eyes commencing approximately two months before admission. One year prior to the first hospital visit, the patient complained of an intermittent episode of seeing black spots in his left eye. The patient was known to have a history of promiscuity and tattoos.
An ophthalmologic examination showed that his visual acuity was 1/60 for both eyes. It also showed cells +3 and flare +3 in the anterior chamber without posterior synechia, with positive papillary light reflex in both eyes. Fundus examination revealed hazy vitreous, and other detailed structures of the retina were only superficially examined (Figure 4). The diagnosis showed posterior uveitis in both eyes due to suspected toxoplasma,CMV, syphilis infections and/or AIDS. Further laboratory investigation for uveitis was planned for the patient.

Figure 4 First visit appearance of ocular funduscopy examination revealed severe bilateral vitreous opacities and details on both retinas were difficult to determine.
The laboratory examination demonstrated a positive result for the HIV test, with negative results for IgG and IgM antitoxoplasma antibodies; negative results for IgG and IgM antiherpes simplex virus (HSV) 1 antibodies, positive results for IgG and IgM anti-HSV 2 antibodies, positive result on syphilis serology tests (treponema pallidum haemagglutination assay and fluorescent treponemal antibody-absorbed test),positive result for IgG anti-CMV antibody, negative result for IgM anti-CMV antibody and CD4+ T-lymphocyte cell count was 261 cells/mL. Chest X-ray and Mantoux test showed no abnormalities. The patient was examined by both a dermatovenerologist and an internist and was diagnosed with posterior uveitis in both eyes caused by syphilis.
He was treated with benzathine penicillin 2.4 million units twice a day with an interval of 1wk apart. The patient was also treated with duviral® 1 tablet daily (zidovudine® 300 mg and lamivudine® 150 mg) and efavirenz® 600 mg daily; HAART therapy was also started, followed by oral steroid treatment for 3d. After 1wk, revealed improvement in anterior segment,however from posterior examination on both eyes still showed dense vitreous opacity due to severe inflammation (Figure 5).In the following 2wk, his visual acuity was 6/20 for the right eye and 6/18 for the left eye. No cells or flare could be found in the anterior chamber of either eye. The vitreous was clear and the fundus showed no exudates or bleeding, however,there was dilatation of retinal vascular and disc pallor of optic nerve head (Figure 6). The systemic medical treatment were continued for several weeks, and after 3mo there was significant improvement on both eyes with visual acuity of the right eye was 6/7.5 and 6/9 on the left eye. Anterior and posterior segments showed clear condition on both eyes(Figures 7, 8).
We were able to determine from these two cases that ocular manifestation should be taken into account whenever treating HIV/AIDS patients with possible opportunistic infection.Panuveitis is the earliest ocular manifestation found in patients with AIDS[3]. It should be noted that uveitis in patients presenting with HIV/AIDS may be more severe than in those with other infections, and may also result in greater sequelae. Previous studies have shown that HIV is a common co-infection of multiple ocular tissues, such as the retina,conjunctiva, cornea and iris of patients with AIDS[3,7-8]. It has been also reported that the HIV virus is able to replicate in CD4-positive T lymphocytes, macrophages, endothelial cells,dendritic cells, monocytes, astrocytes and microglial cells[9].
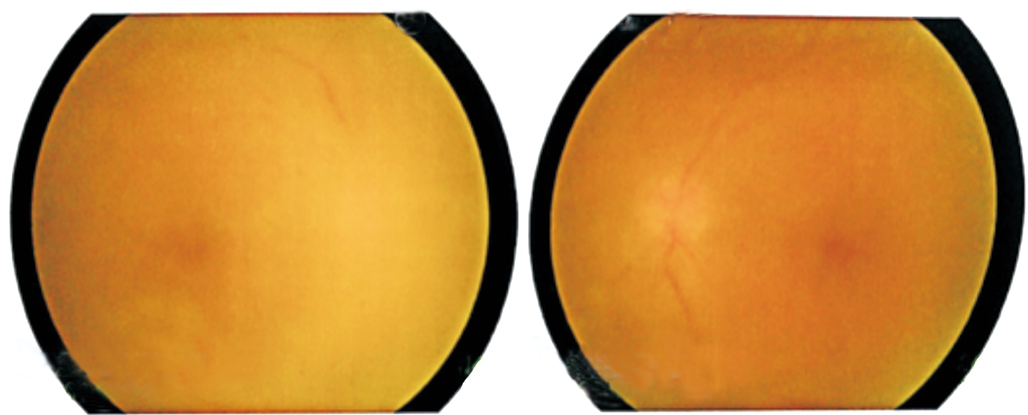
Figure 5 Funduscopy examination on both eyes 1wk later still showed dense vitreous opacity due to severe inflammation.
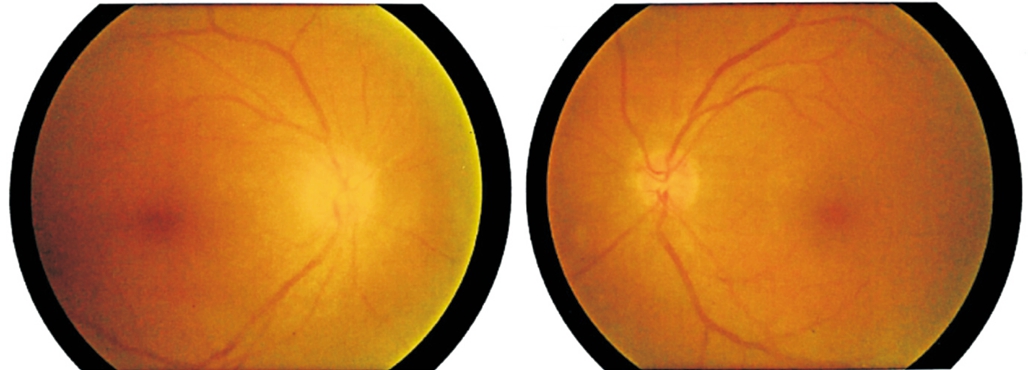
Figure 6 Fundus condition after 1mo after treatment showed disc pallor of optic nerve head in the right eye and was normal in the left eye without sign of hemorrhage or exudates. Mild sheathed and dilated retinal vessels were seen in both eyes.
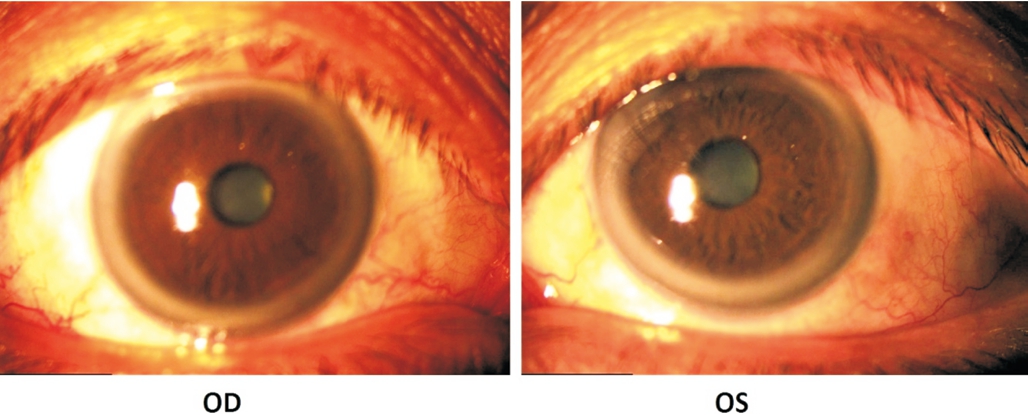
Figure 7 Anterior segment of both eyes improved after 3mo of treatment.
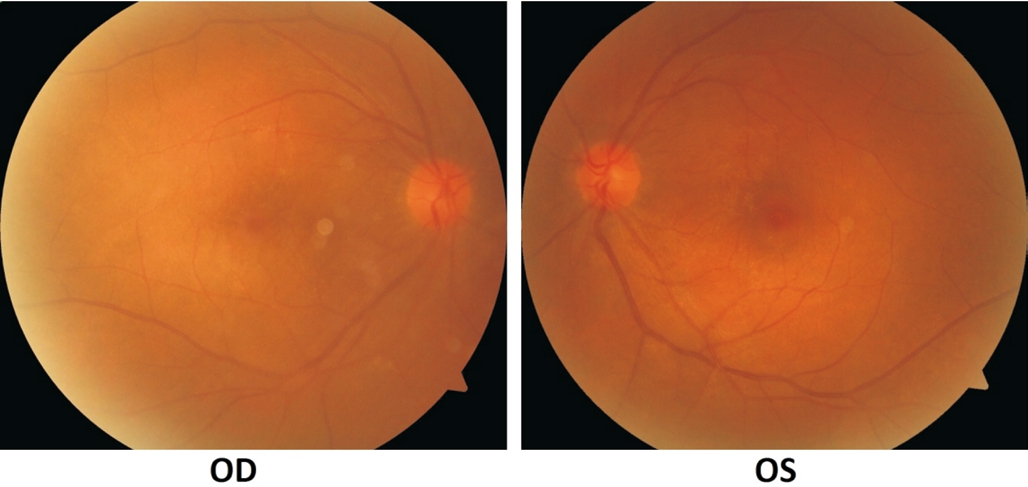
Figure 8 Fundus appearance of both eyes after 3mo of treatment.
Kunavisarut et al[9] have noted that panuveitis may occur in patients presenting with HIV without any other opportunistic infection. It may appear as a mild inflammatory reaction in the anterior chamber with detected HIV-1 RNA in intraocular fluid. Panuveitis may not always be severe nor show sudden symptoms or acute signs. Therefore, progress may well exacerbate unnoticed.
It has been reported that improved immune function may occur after completing HAART thus altering inflammatory response in eye tissues[3,10-11]. However, in cases with proven opportunistic infection, the underlying cause must be treated immediately with utmost care using the combined HAART treatment. Improvement of inflammation should ensue rapidly and the visual acuity restored significantly.
The first patient in this case presented with infection in both eyes. There was a moderate anterior inflammatory symptom in both eyes and several inflammatory cells within the anterior chamber. In the second case, there were similar clinical manifestations and differentiation of the cause of opportunistic infection was rendered difficult since there were no characteristic symptoms. Both cases had no previous history of HIV infection or HAART. Therefore, it was essential to perform a thorough blood serologic test to determine viral or other infections featuring in all cases with panuveitis. It is also recommended to include humor aqueous tap for PCR analysis to detect viral DNA or other infections in order to unambiguously identify the definitive cause[12].
In the first case presented by HIV/AIDS patient with CMV-associated uveitis, steroid treatment was ceased and substituted with oral gancyclovir and intravitreous injection of antiretroviral to overcome further severe inflammatory reaction in the posterior segment. Oral treatment alone often exerts no significant response. Oral treatment was given for 20mo in order to suppress CMV replication and, thus,prevent relapse and prolonged CMV infection. The oral treatment was combined with HAART to suppress HIV replication in peripheral blood and increase the number of CD4+ T lymphocyte cells. This should subsequently result in improvement of the immune system[3,9,11]. Jabs et al[3] have reported that combined treatment using long-term modern antiretroviral (HAART) for HIV/AIDS patients with CMV-associated retinitis may bring about immune recovery reaction uveitis (IRU) and the incidence of immune recovery uveitis was 2.2/100 person-years (PYs).
Patients without immune recovery had a mortality of 44.4/100 PYs following diagnosis of CMV retinitis, whereas those with immune recovery had a mortality of 2.7/100 PYs (P<0.001).Therefore, it can be concluded that HAART treatment is absolutely essential[3]. It is also important to notice that CMV infection is associated with a 60% increase in mortality among persons living with AIDS[3,13-14]. Moreover, higher CMV loads are usually associated with greater risks of mortality[15-16].
Our cases suggest that HAART treatment without anti-CMV treatment may bring about delayed recovery. Therefore, a long-term additional systemic anti-CMV treatment is essential,resulting in a better outcome than repetitive intravitreous injections to prevent recurrent vitritis and retinitis. Due to the nature of systemic infection, the propensity of CMV to transactivate HIV and CMV’s own intrinsic immunosuppressive effect, systemic treatment that inhibits CMV replication may well improve immune function and survival of patients[11,13,16-18].
Once sustained immune recovery has been adequately reached, the specific immunity against CMV is then restored.The parameter requires a minimum of 150 absolute CD4+ T lymphocytes/mL detected in the blood stream and the replication of CMV can be controlled by the immune system. Therefore,anti-CMV therapy is no longer necessary[11,19]. Intravitreous injection of anti-CMV may be needed in the case that vitritis occurs. However, the treatment is only administered when there is an indication[11].
In the second case, optimal intensive treatment for syphilis infection was administered, either by intramuscular injection or oral treatment along with immediate HAART treatment.Routine tests should be recommended for HIV-related syphilis infections as HIV infection is strongly correlated to the reemergence of infectious syphilis and increased risk of neurosyphilis. In addition to panuveitis, the most common ocular manifestation may include peripheral retinitis or necrotizing retinitis that usually causes diagnostic confusion with acute retinal necrosis resulting from CMV retinitis[13].
A multidisciplinary approach is recommended by collaborating with a genitourinary physician who can provide combined treatment for treating the systemic infection, including HIV.Moreover, additional treatment using oral prednisolone at a dose of 60 mg daily for 3d may improve the healing process of retinitis. The condition often resolves within 3-4d, resulting in typical sequelae of retinal pigment epithelial atrophy[7]. The sequelae has also been reported in our cases, i.e. the fundus became clear and retinal abnormality appeared. Hughes et al[7]have also reported that there is a strong correlation between HIV co-infection and syphilitic retinitis, found in 100% of HIV-infected patients. They have also reported that panuveitis is not an early clinical manifestation of HIV infection.
The common complications that occur in all cases of patients with HIV-related panuveitis are secondary glaucoma, ocular hypertension, cataracts, cystoid macular edema, epiretinal membrane formation, visual impairment and blindness.An intensive follow-up and multidisciplinary approach in collaboration with internists and venereologists will bring about optimal outcomes. Long-term ocular and systemic follow-up is mandatory as a relapse or re-infection may occur.In conclusion, timely and appropriate treatment is essential in the management of patients with bilateral panuveitis and opportunistic HIV infections. A routine test consists of a complete serologic blood test, HIV test, Mantoux tuberculin skin test and chest X-ray, all of which should be performed for each patient presenting with uveitis. Moreover, a multidisciplinary approach to manage the underlying cause is of utmost significance. Early diagnosis and timely treatment using combined HAART and therapy for opportunistic infections may result in a substantial recovery in visual acuity.
ACKNOWLEDGEMENTS
Authors’ contributions: Artini W encountered the first patient and collaborated with Sjamsoe S in handling the comprehensive management of the patient. Susiyanti M encountered the second patient and was responsible for the overall therapy. All authors participated in the compilation of this manuscript.
Conflicts of Interest: Artini W, None; Sjamsoe S, None;Susiyanti M, None.
REFERENCES
1 Komisi penanggulangan AIDS Nasional. Informasi Dasar Penanggulangan HIV dan AIDS di Indonesia. Available at: http://www.aidsindonesia.or.id/repo/perpustakaan/InformasiDasarPenanggulanganHIVAIDSIndonesiaSeri1.pdf.
2 Levinson RD, Vann R, Davis JL, Friedberg DN, Tufail A, Terry BT, Lindley JI, Holland GN. Chronic multifocal retinal infiltrates in patients infected with human immunodeficiency virus. Am J Ophthalmol 1998;125(3):312-324.
3 Jabs DA, Ahuja A, Natta MLV, Lyon AT, Yeh S, Danis R. Longterm outcomes of cytomegalovirus retinitis in the era of modern antiretroviral therapy : results from a united states cohort. Ophthalmology 2015;122(7):1452-1463.
4 Copeland RA. Ocular manifestations of HIV infection. Available at:http://emedicine.medscape.com/article/1216172-overview.
5 Lestari YD, Sitompul R, Edwar L, Djoerban Z. Ocular diseases among HIV/AIDS patients in Jakarta, Indonesia. Southeast Asian J Trop Med Public Health 2013;44(1):62-71.
6 Farrell PL, Heinemann MH, Roberts CW, Polsky B, Gold JW, Mamelok A. Response of human immunodeficiency virus-associated uveitis to zidovudine. Am J Ophthalmol 1988;106(1):7-10.
7 Hughes EH, Guzowski M, Simunovic MP, Hunyor AP, McCluskey P.Syphilitic retinitis and uveitis in HIV-positive adults. Clin Exp Ophthalmol 2010;38(9):851-856.
8 Shalaby IA, Dunn JP, Semba RD, Jabs DA. Syphilitic uveitis in human immunodeficiency virus-infected patients. Arch Ophthalmol 1997;115(4):469-473.
9 Kunavisarut P, Sirirungsi W, Pathanapitoon K, Rothova A. Clinical manifestations of human immunodeficiency virus-induced uveitis.Ophthalmology 2012;119(7):1455-1459.
10 Arantes TE, Garcia CR, Saraceno JJ, Muccioli C. Clinical features and outcomes of AIDS-related cytomegalovirus retinitis in the era of highly active antiretroviral therapy. Arq Bras Oftalmol 2010;73(1):16-21.
11 Stewart MW. Optimal management of cytomegalovirus retinitis in patients with AIDS. Clin Ophthalmol 2010;4:285-299.
12 Rothova A, de Boer JH, Ten Dam-van Loon NH, Postma G, de Visser L, Zuurveen SJ, Schuller M, Weersink AJ, van Loon AM, de Groot-Mijnes JD. Usefulness of aqueous humor analysis for the diagnosis of posterior uveitis. Ophthalmology 2008;115(2):306-311.
13 Chhablani JK, Biswas J, Sudharshan S. Panuveitis as a manifestation of ocular syphilis leading to HIV diagnosis. Oman J Ophthalmol 2010;3(1):29-31.
14 Ahmed I, Ai E, Chang E, Lucky A. Ophthalmic manifestations of HIV.Available at: http://hivinsite.ucsf.edu/InSite?page=kb-04-01-12.
15 Jabs DA, Holbrook JT, Van Natta ML, Clark R, Jacobson MA,Kempen JH, Murphy RL. Risk factors for mortality in patients with AIDS in the era of highly active antiretroviral therapy. Ophthalmology 2005;112(5):771-779
16 Jabs DA, Martin BK, Forman MS, Ricks MO; Cytomegalovirus Retinitis and Viral Resistance Research Group. Cytomegalovirus (CMV) blood DNA load, CMV retinitis progression, and the occurrence of resistant CMV in patients with CMV retinitis. J Infect Dis 2005;192(4):640-649.
17 Goldberg DE, Wang H, Azen SP, Freeman WR. Long term visual outcome of patients with cytomegalovirus retinitis treated with highly active antiretroviral therapy. Br J Ophthalmol 2003;87(7):853-855.
18 Jacobson MA, Stanley H, Holtzer C, Margolis TP, Cunningham ET.Natural history and outcome of new aids-related cytomegalovirus retinitis diagnosed in the era of highly active antiretroviral therapy. Clin Infect Dis 2000;30(1):231-233.
19 Jacobson MA, Schrier R, McCune JM, Torriani FJ, Holland GN,O’Donnell JJ, Freeman WR, Bredt BM. Cytomegalovirus (CMV)-specific CD4+ T lymphocyte immune function in long-term survivors of AIDS-related CMV end-organ disease who are receiving potent antiretroviral therapy. J Infect Dis 2001;183(9):1399-1404.