Evaluation of artificial tears on cornea epithelium healing
Ying Zhang1,2, Xiao-You Lu2, Ren-Jian Hu1, Fang-Li Fan1, Xiu-Ming Jin1
1Eye Center, Second Affiliated Hospital of Zhejiang University School of Medicine, Hangzhou 310000, Zhejiang Province,China
2Department of Ophthalmology, Zhejiang Xiaoshan Hospital,Hangzhou 310000, Zhejiang Province, China
INTRODUCTION
Human cornea is composed of epithelium, Bowman layer, stroma, Descenet membrane and endothelium.Epithelium is necessary for developing shape, structure,and resistance to external injury. Epithelium defects can be triggered by adverse events of local and/or systemic drug,trauma, surgery in addition with ocular surface diseases.Inadequate healing of the epithelium will lead corneal infection, ulcers, perforations, leukoma, neovascularization,haze, and/or blindness[1-2]. In general, a small area of corneal epithelial injury can be repaired spontaneously. However,major injuries need treatment as soon as possible to promote corneal re-epithelialization and avoid corneal trauma and neovascularization[3].
In order to evaluate the healing support provided by eye surface treatment, numerous studies over the last 70y have investigated corneal epithelium wound healing[4]. In recent years, accelerating corneal epithelial wound healing and treating persistent corneal epithelial defect got more and more attention. Corneal epithelium healing is a complex process involving intercellular signaling and interactions between cells and the extracellular matrix, proteases, growth factors, as well as epithelial and stromal cytokines[5-6]. In the absence of re-epithelialization, the corneal ulcer forms until perforation.Perforation is the final outcome of cellular degradation procedure resulting from chronic in flammation[7-9]. Formation of tight junctions between epithelial cells is an important step in restoring corneal epithelial integrity to protecting cornea from pathogens, infection and ulcer[10-13]. Artificial tears are often used in treatment of corneal epithelium defect clinically[14]. The corneal epithelium can self-repair. However,there are various eye drops to promote repair of corneal epithelium, it is dif ficult to distinguish the contribution from self-repair or eye drops in the accelerating corneal epithelial healing. People have not reached an agreement on this point yet.
There were only a few researches assessed the effects of different artificial tears on corneal re-epithelialization[10-13,15-17].However, the re-epithelialization results of various artificial tears on corneal epithelium defect were still unknown. The study investigates the efficacy of different artificial tears in promoting corneal epithelial healing using a rabbit corneal epithelial scrape wound model.
MATERIALS AND METHODS
Thirty-five one-year-old New Zealand white rabbits (17 males and 18 females) from Zhejiang Academy of Medical Sciences, weighing 2.5-3.0 kg, were used in this study. Rabbits were anesthetized with auricular vein injection of 3% pellto barbitalum natricum (1.5-2 mL/kg). The central corneal epithelial was marked by corneal trephine, 6 mm in diameter,removed with a Gill corneal knife, leaving the stroma intact,resulting in an epithelium scrape wound 6 mm in diameter in the right eye (Figure 1). Rabbits were randomly divided into seven treatment groups (five rabbits per group): 0.1%hyaluronate (HA), 0.3% HA, Tears Naturale Free®(TNF),0.4% polyethylene glycol (PEG), 0.5% carboxymethyl cellulose (CMC), 0.9% normal saline (NS), and blank control group. The blank control group received nothing. Treatments were administered topically to wounded eyes immediately after surgery, with subsequent administrations 4 times a day (at 8 a.m., 12 p.m., 4 p.m., 8 p.m.). Samples were observed at 0,24, 36, 48, 60 and 72h post-wounding. This study had obtained prior approval of the study protocol by the Ethics Committee of the School of Medicine, Zhejiang University of China. All rabbits were kept in a barrier environment and fed regularly.All applicable institutional and governmental regulations concerning the ethical use of rabbits were followed.
The surface of the cornea was observed at 12.5× magnification using a slit-lamp biomicroscope (YZ5S, Suzhou six six visual Polytron Technologies Inc.) and viewed under blue light following instillation of 1% sodium fluorescein and took pictures at 0, 24, 36, 48, 60 and 72h post-wounding. In fact,after 36h post-wounding, frequent transits were observed,which helped to observe corneal epithelial healing time at the early stage. The efficacy of different artificial tears in promoting corneal epithelial healing was expressed as the percentage reduction in the fluorescein-stained area compared to 0h. The area of the re-epithelialized corneal wound was measured and examined using Image-Pro Plus 6.0. The cornea was analyzed by histological analysis at 72h post-wounding.The other four New Zealand white rabbits with removed central corneal epithelium in 6 mm diameter were divided into two groups randomly and received 0.3% HA drops and 0.9% NS drops respectively. Cornea was inspected by electron microscopy examination at 24 and 72h respectively.
Statistical AnalysisStatistical data analysis were compared between artificial drops groups and blank group using the independent samples t-test. In addition, comparison among artificial drops groups used Tamhane’s T2 test. All P-values were two-sided, and P<0.05 was considered to be statistically significant. All results were expressed with the mean±SD with five samples among each group.
RESULTS
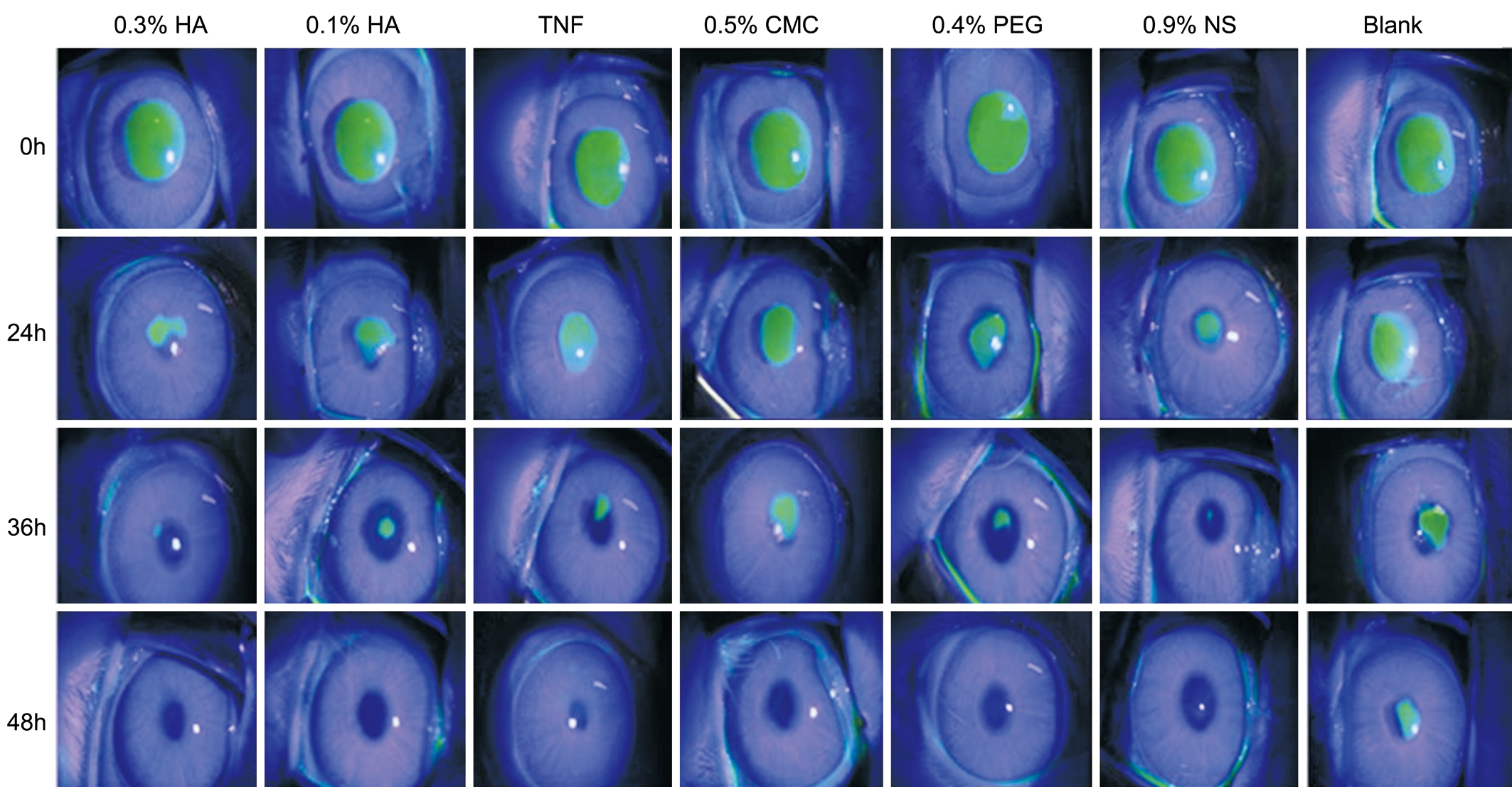
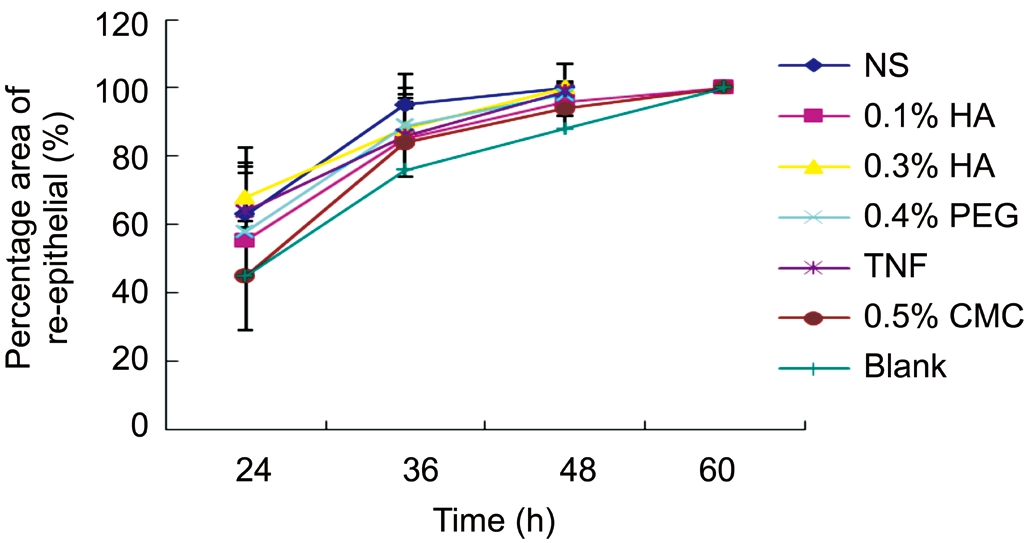
Representative images of corneal fluorescein staining of the wound area in rabbits’ corneas following treatment with 0.1%HA, 0.3% HA, TNF, 0.4% PEG, 0.5% CMC, and 0.9% NS were shown in Figure 1. Image analysis of the wound area was presented as the percentage healed at 24, 36 and 48h in Figure 2.All corneal wounds were completely re-epithelialized in less than 72h, though the blank control group took longer than the other groups. Re-epithelialization completion occurred in 3 rabbits at 48h of the 0.3% HA group and in 2 rabbits within the 0.1% HA group. However, it was not found in any other groups or in the control group at 48h.
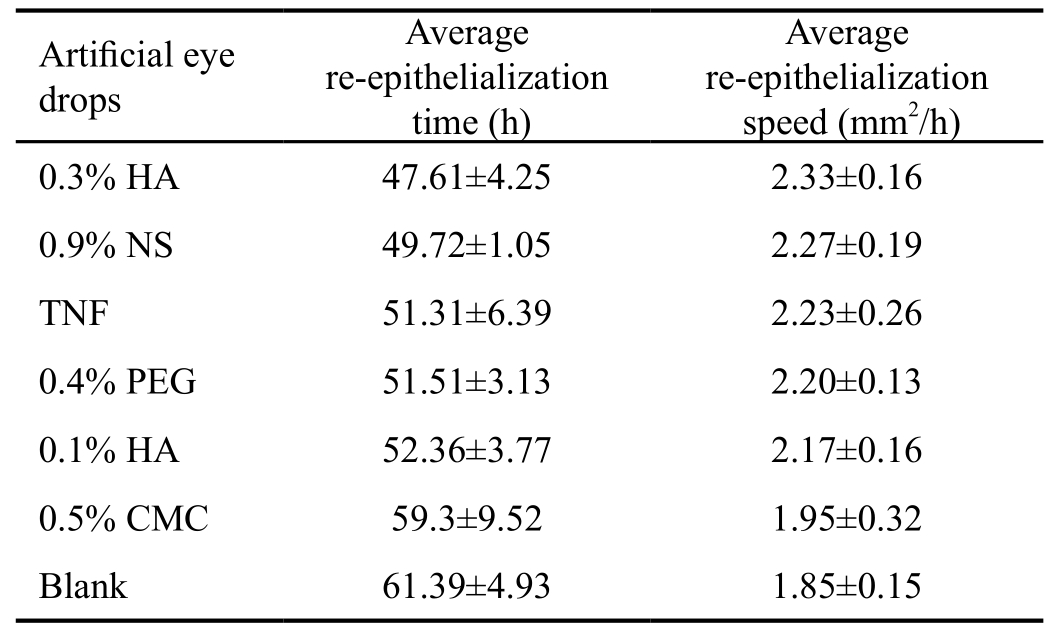
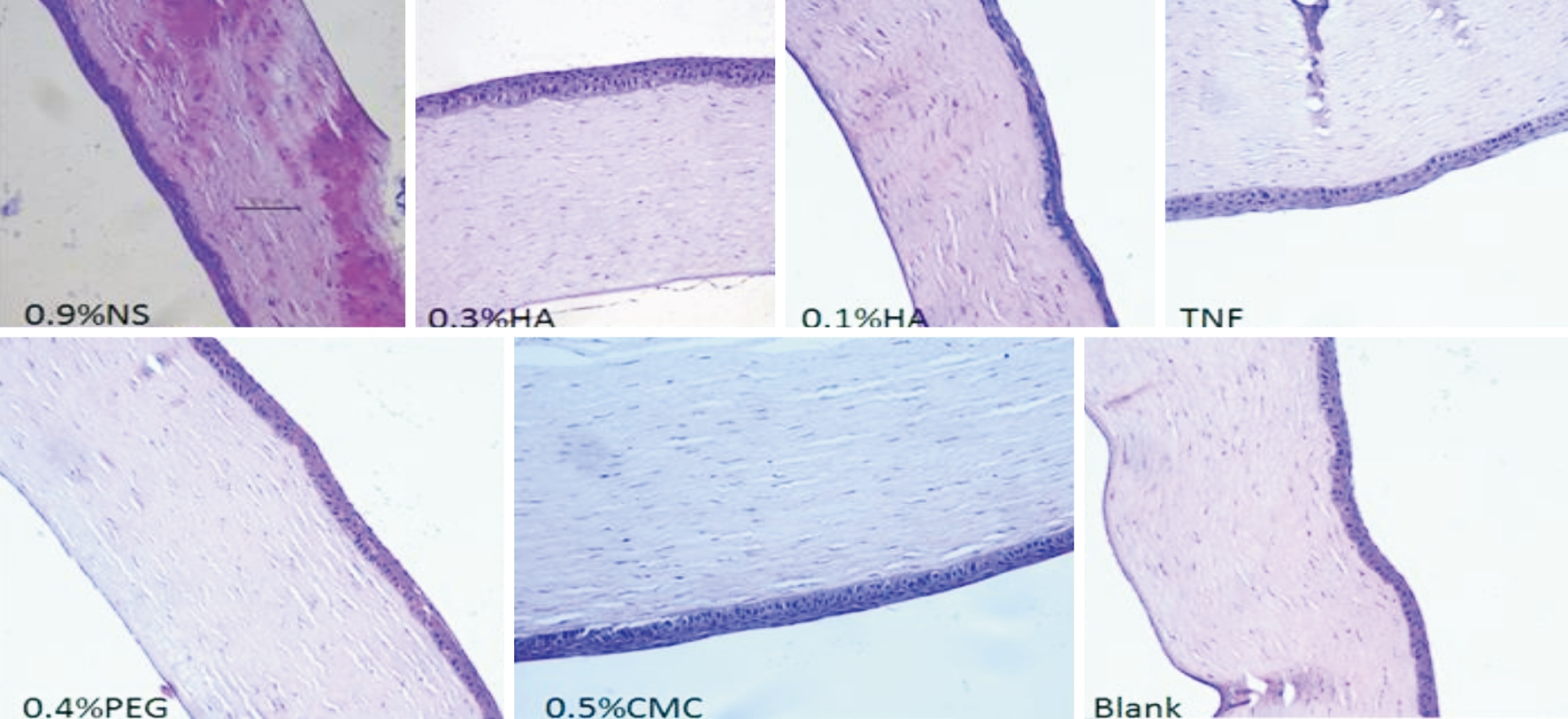
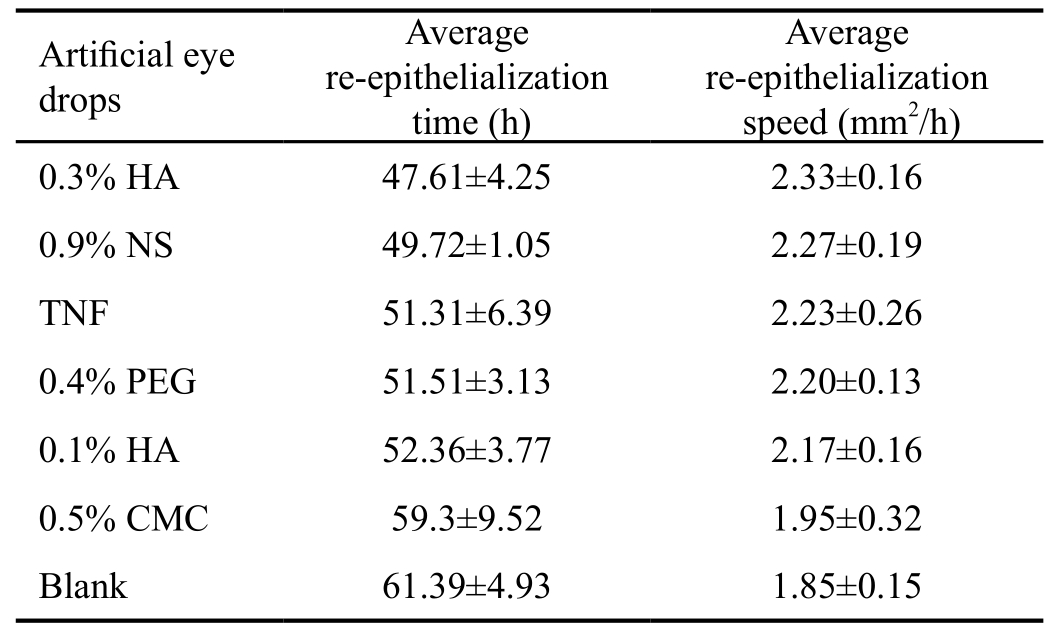
During the first 24h post-wounding, the 0.3% HA, TNF, and 0.9% NS groups were significantly faster than other groups in reducing the size of the wound area. The percentage area of re-epithelialization was 68%±10% with 0.3% HA, 64%±16%with TNF, and 63%±12% with 0.9% NS. At 36h postwounding, 0.4% PEG group had accelerated the rate of reepithelialization. The percentage area of re-epithelialization in the 0.4% PEG treatment group was 89%±9%, followed by 0.3% HA (88%±8%) and TNF (86%±10%). At 48h postwounding, corneal epithelium was nearly completing reepithelialization at 0.3% HA and 0.9% NS treatment groups(Figure 2). The average re-epithelialization time of 0.3% HA and NS group were 47.61±4.25h and 49.72±1.05h respectively,followed by 0.1% HA, TNF, 0.4% PEG, 0.5% CMC, and the blank control group remained the last. Compared to the blank control group, there was a significant difference among 0.3%HA, 0.9% NS, 0.4% PEG, and TNF (P<0.05) groups. No significant difference was found between the 0.9% NS group versus the other treatment groups (P>0.05). The rate of reepithelialization was 2.18±0.20 mm2/h with 0.3% HA and 2.09±0.03 mm2/h with 0.9% NS group, followed by 0.1% HA,TNF, 0.4% PEG, 0.5% CMC and blank control group (Table 1).In order to further assessing the microstructure during corneal epithelial healing, we performed histological at 72h postwounding among all groups. Histological examination of epithelium of rabbit corneas showed all corneal epithelial completed re-epithelialization at 72h post-wounding, with the cells adjoined form an intact layer (Figure 3). The 0.3%HA-treated corneas and the 0.9% NS group corneas were examined by scanning electron microscopy at 24 and 72h post-wounding. We found these two groups had similar results at 24h post-wounding with a few vesicles were visible. The vesicle sizes varied in the cytoplasm of the 0.9% NS-treated corneas at 72h, barely in 0.3% HA-treated corneas (Figure 4).Representative photomicrographs of rabbit corneal epithelial wounds viewed under blue light following instillation of 1%sodium fluorescein at 0, 24, 36, 48, 60 and 72h post-wounding.The efficacy of different artificial tears on promoting corneal epithelial healing varied (Figure 1).
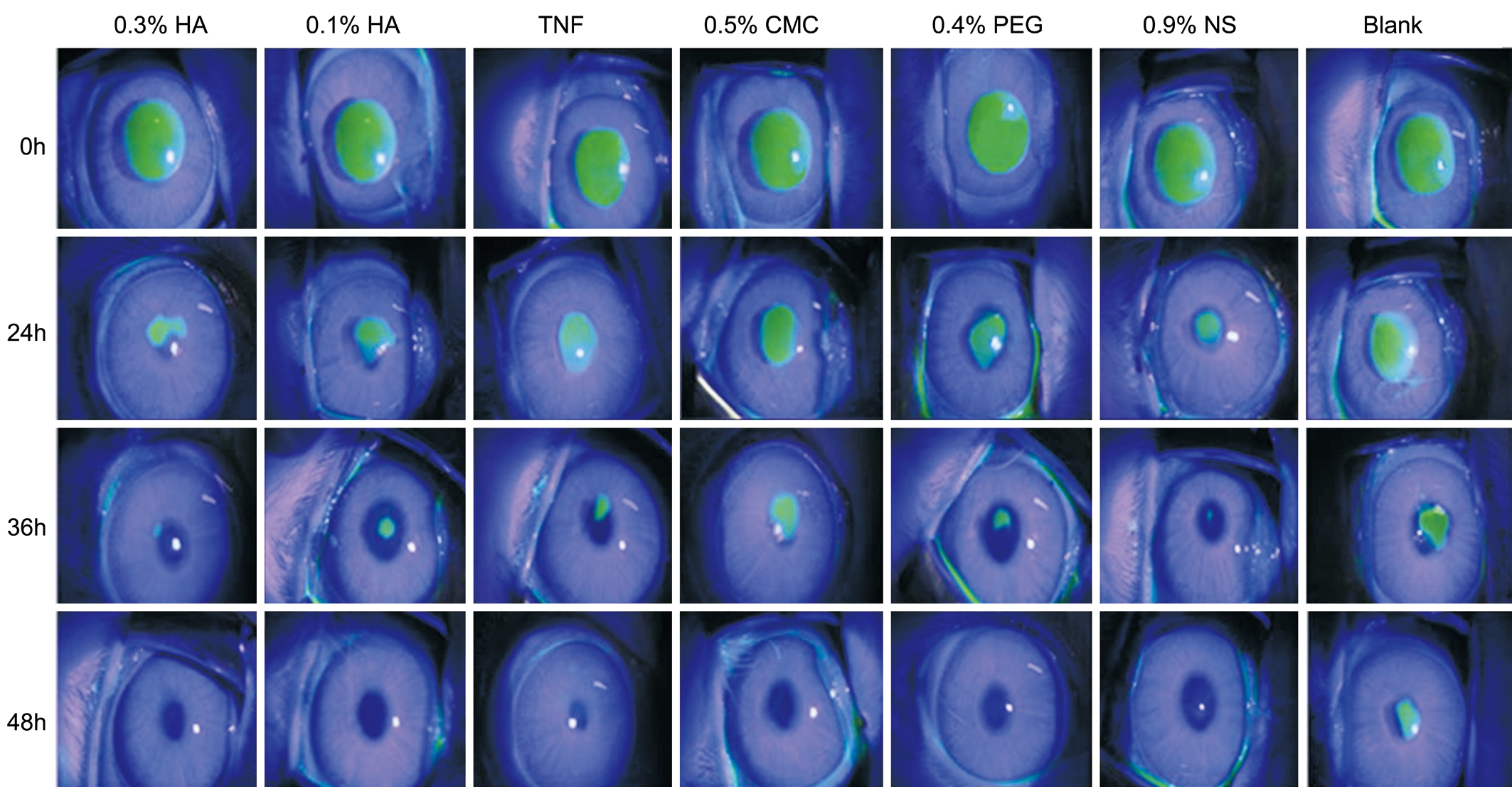
Figure 1 Representative photomicrographs of rabbit corneal epithelial wounds at 0, 24, 36 and 48h post-wounding At 24h postwounding, re-epithelialization was a little different among different eye drops. At 36h post-wounding, NS and 0.3% HA group represented the better ability to repairing (12.5× magnification).
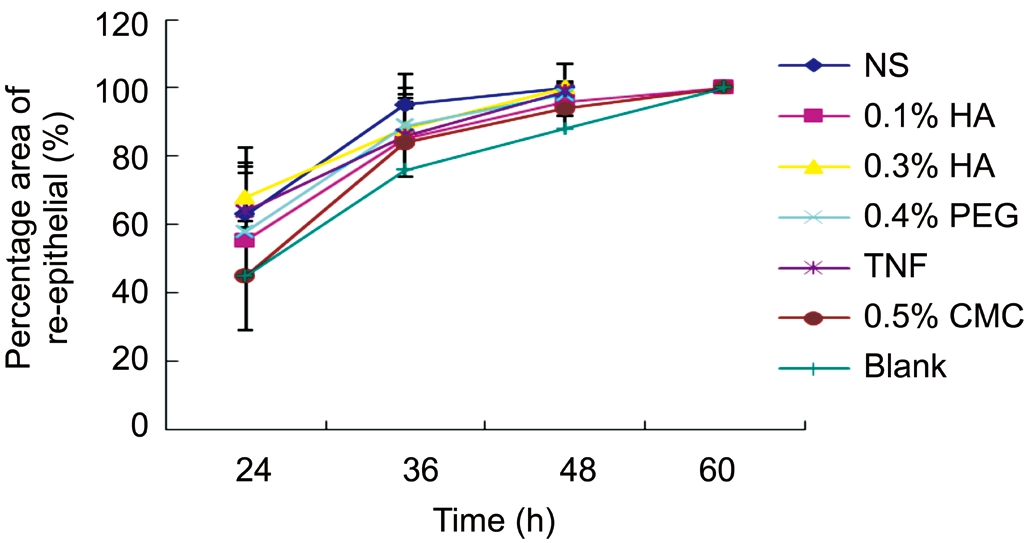
Figure 2 Percentage area of re-epithelial at 0, 24, 36 and 48h postwounding The percentage area of re-epithelialization was similar among 0.3% HA, TNF and NS group at 24h post-wounding. At 36h post-wounding, PEG group accelerated the rate of re-epithelialization.
The average re-epithelialization speed and time to complete the re-epithelialization with different artificial tears and untreated control group were analyzed by independent samples t-test(mean±SD). Compared to the untreated control group, there was a significant difference using 0.3% HA, 0.9% NS, 0.4%PEG, and TNF (P<0.05).
DISCUSSION
This study evaluated the effect of different artificial eye drops and 0.9% NS on treating ocular surface using rabbit
Table 1 Average re-epithelialization speed and time with different artificial tears
?
HA: Hyaluronate; NS: Normal saline; TNF: Tears Naturale Free;PEG: Polyethylene glycol; CMC: Carboxymethyl cellulose.model. Rabbits have been used to study corneal wound healing for decades. As the rabbit cornea was similar in size to the human’s, it helped researchers to use the same instruments and evaluation methods as human being[18-19].Epidemiological studies have revealed several risk factors for corneal scratching, such as infection, mechanical scratching,dry environment, blepharitis, immunological disease, and tiredness[1-2]. Rabbits immediately closed their eyes upon losing their corneal epithelium, which contributed to reducing scratch wounds.
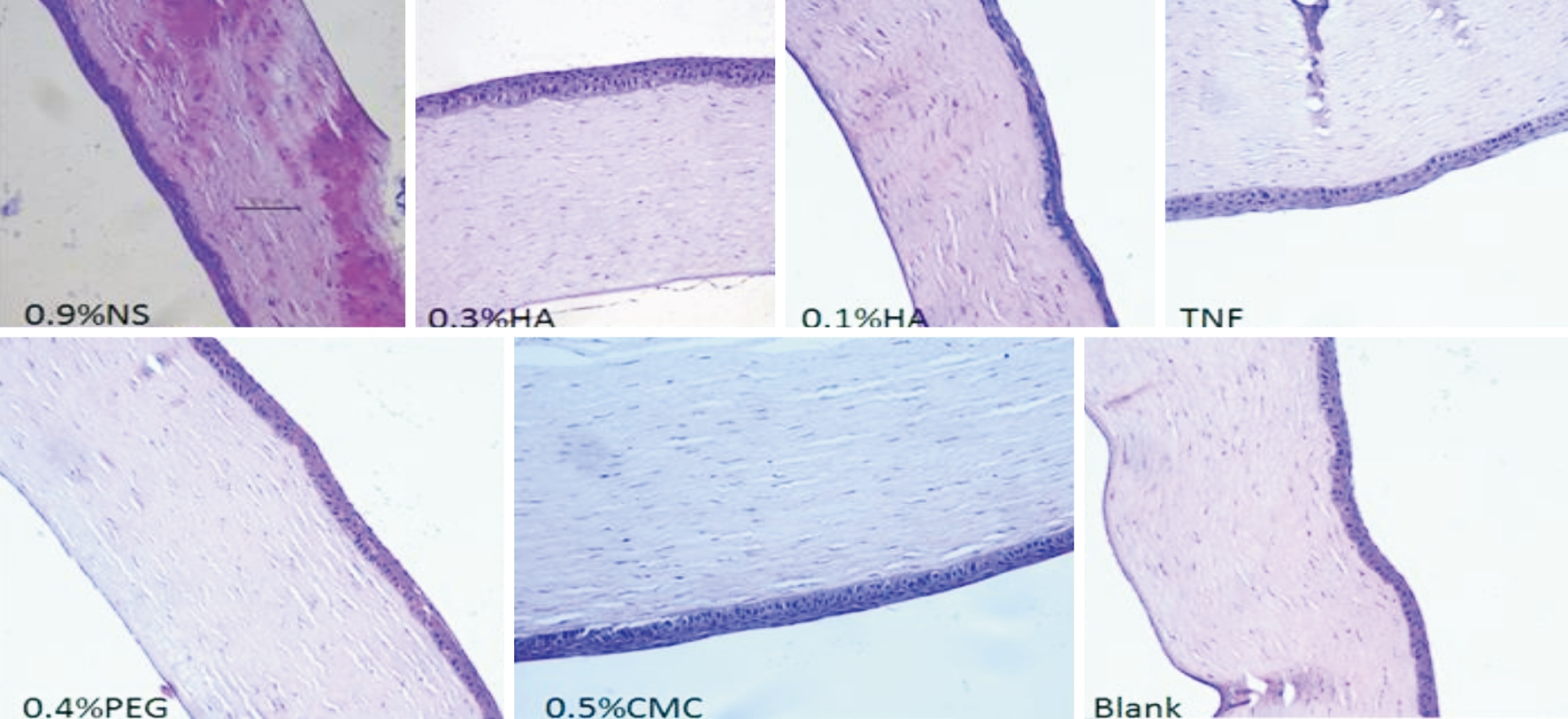
Figure 3 Histological examination of corneas at 72h post-wounding Sections were stained with hematoxylin and eosin. Re-epithelialization was complete with cells adjoining to form an intact layer (50× magnification).
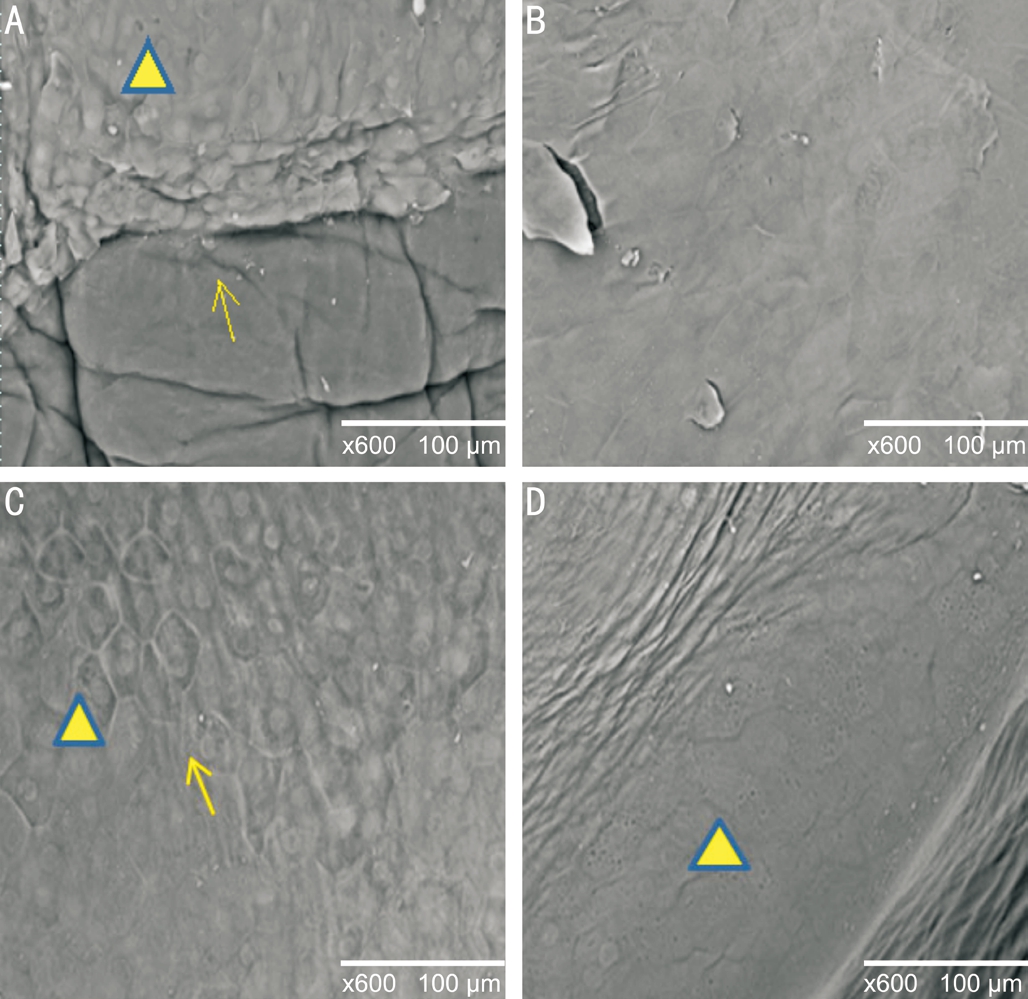
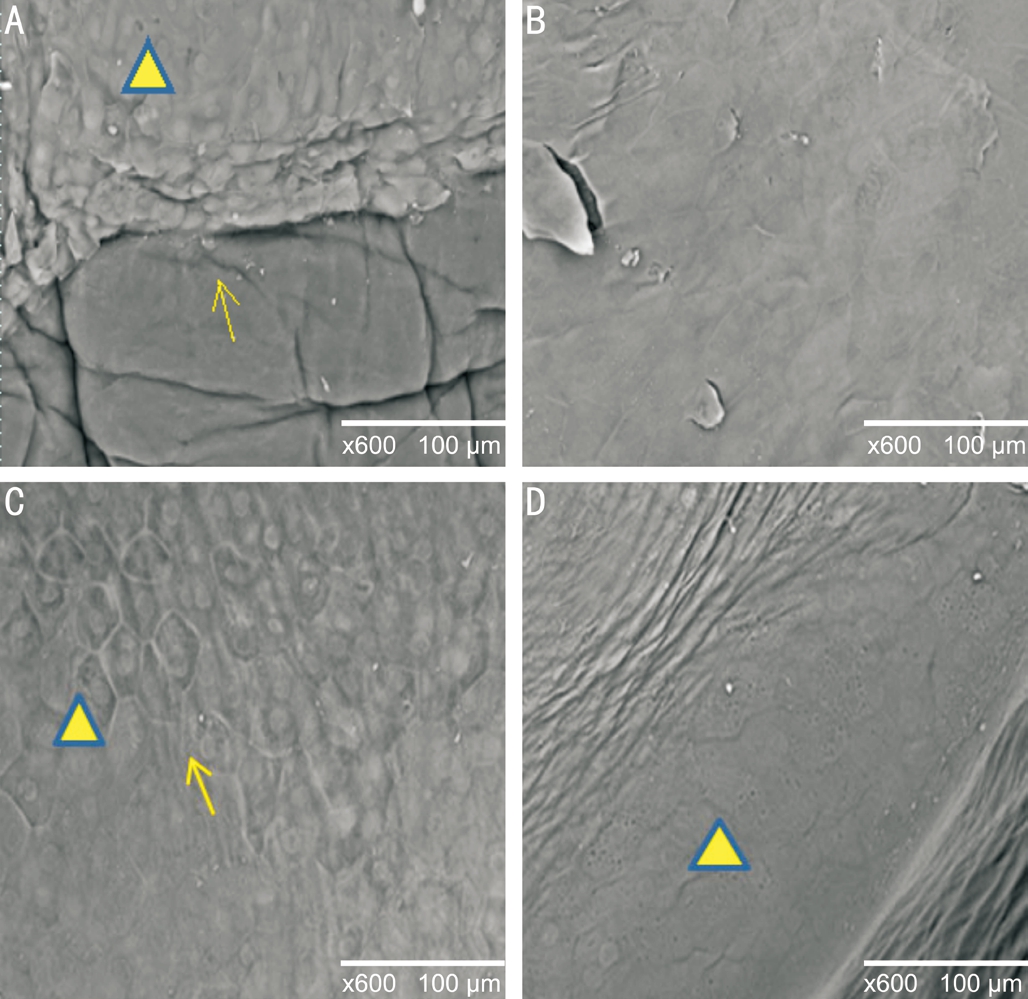
Figure 4 Scanning electron microscopy of 0.3% HA and NS group A: At 24h post-wounding, there was an obvious dividing line(arrow) in the epithelial cell layers of the 0.3% HA group, basement membrane exposure, and a few vacuoles (triangle); B: At 72h postwounding, 0.3% HA treatment group completed re-epithelialization;C: At 24h post-wounding, basement membrane was covered by regenerative epithelium (arrow), with only a few vacuoles can be seen (triangle); D: At 72h post-wounding, a large number of vacuoles presented in the cytoplasm of cells in the NS group (triangle).
It was concluded that the corneal epithelium could selfrepair, and corneal epithelium healing was a complex process involving intercellular signaling, interactions between cells,the extracellular matrix, proteases, growth factors, as well as epithelial and stromal cytokines[5-6]. How artificial tears help corneal re-epithelialization was still not fully understood.It was known that artificial tears help to reduce friction by providing lubrication, offer some resistance to infection, as well provide nourishment and strengthen junctions between cells[10-13].The results of this study revealed that the corneal epithelial wound healing rate, average re-epithelialization time and speed significant improved with topically application of artificial eye drops and 0.9% NS group, which is better than blank group.Furthermore, we found that different treatments resulted in different re-epithelialization speeds. At the first 24h postwounding, 0.3% HA, 0.9% NS, and TNF displayed greater reepithelialization ability. At 36h post-wounding, 0.4% PEG had increased the rate of re-epithelialization. We hypothesized that different artificial tears stimulated corneal re-epithelialization via different mechanisms. However, certain factors played a role, for instance, moisture retention, viscosity, and the dilution of inflammatory factors. This study showed that artificial tears can promote corneal re-epithelium after mechanical scraping, whether in average re-epithelialization time or speed, there were significant difference compared with the blank group. The mechanism by which HA stimulates corneal epithelial healing is yet to be fully determined. Numerous studies have demonstrated that HA promotes healing in vitro of human corneal epithelial scratch wounds in addition to its water retention and its positive biological functions on corneal epithelial cells[15,20-22]. HA has been shown the ability to reduce the tear evaporation rate, strengthen tear film stability[20,23]. The result of HA on intracellular signaling and cell behavior are managed by binding to specific cell-surface receptors, including CD44 and the receptor for hyaluronanmediated motility, the motivation of these receptors modulate cell proliferation and migration[21]. Indeed, these receptors have been found in the human cornea and may be involved in wound healing[24-25]. Some scholars had showed that HA could stimulate corneal epithelial migration independent of fibronectin and epidermal growth factor[23]. The hyaluronan to the culture medium increases the length of the path of the corneal epithelial layer in a dose-dependent manner[23]. Other reporters have claimed that the beneficial effects of 0.3% HA were better than those of 0.3% HA and 0.4% PEG, 0.3% HA could significant improve corneal epithelial wound healing rate, corneal sensitivity and nerve fiber density[26-28]. However,this phenomenon was undetected in this study. It is possible due to the number of samples among each testing group.
The study also showed that TNF, 0.1% HA, and 0.4% PEG promote re-epithelialization better than the blank control group. The reports had showed that 0.4% PEG eye drops were significantly better than 0.5% CMC eye drops in reducing corneal wounding area. PEG 0.4% could extend tear film break-up time and promote epithelial healing, and it was also stated that this was nothing to do with its high viscosity[16].PEG 0.4% can accelerated corneal epithelial cells proliferation by shortening the proliferation cycle of cells and increasing the expression of basic fibroblast growth factor and epidermal growth factor gene[16]. The study have not indicated that 0.4% PEG drop eyes ameliorate ocular surface damage better than CMC. Garrett et al[12]claimed that CMC (0.2% and 1.0%) could accelerate the process of re-epithelialization, the difference was statistically significant compared to phosphate buffer solution. Some scholars have recently proposed the possibility of using CMC as collagen cross-linking for keratoplasty[29]. The study have not indicated that 0.5% CMC drop eyes ameliorate ocular surface damage better than blank.To the best of our knowledge, there was little published about TNF in corneal healing. However, glycerol,a constituent part of TNF has great moisturizing capability. Glycerol may be an effective approach to enhance epithelial recovery. Further studies are needed. To further examine the microstructure of cornea re-epithelialization, histological examination and scanning electron microscopy were done at 72h postwounding. Histological analysis showed re-epithelialization was completed, with cells adjoining to form an intact layer.
The study showed at 72h post-wounding, the re-epithelium morphology in 0.3% HA group was consistent with normal corneal epithelium, different from 0.9% NS group. At 72h post-wounding, slit-lamp and light microscope both indicated cornea epithelium was completely regenerated. The scanning electron microscopy revealed that 24h post-wounding, there were few vacuoles expressed in corneal epithelial, whether 0.9% NS or 0.3% HA group. By 72h post-wounding, there were presented abundant vacuoles lipid droplets in NS group,however, could not be found in 0.3% HA and normal corneal epithelial cells. Scholars have pointed out that due to the lack of oxygen, small vacuoles and droplets can be seen in corneal epithelial[27,30]which was similar to what was found in NS group. It was difficult to explore the sources, physical and chemical properties of vacuoles, which has never been reported including action mechanism and physic chemistry character.It was clearly that hypoxia of corneal epithelial cells appeared in regeneration of corneal epithelium of 0.9% NS group at 72h post-wounding, which was significant difference from normal corneal epithelial cell. The study showed that, in some sense,the epithelial cells of the 0.9% NS group was not yet healed at 72h post-wounding. The expression and the definite molecular mechanism should be further investigated.
In conclusion, this study demonstrated that artificial tears can promote corneal re-epithelium varied in efficacy, artificial eye drop better than blank group. There was no statistical significance among different artificial tears. Large sample data are necessary to evaluate the efficacy of this treatment protocol in clinical practice, and molecular mechanisms. In the process of corneal healing, corneal epithelium cells suffered from hypoxia caused by NS.
ACKNOWLEDGEMENTS
Foundations:Supported by National Natural Science Foundation of China (No.81070705; No.81270974).
Conflicts of Interest: Zhang Y,None;Lu XY,None;Hu RJ,None;Fan FL,None;Jin XM,None.
REFERENCES
1 Suzuki K, Satio J, Yanai R, Yamada N, Chikama T, Seki K, Nishida T. Cell-matrix and cell-cell interactions during corneal epithelial wound healing.Prog Retin Eye Res2003;22(2):113-133.
2 Klenkler B, Sheardown H. Growth factors in the anterior segment: role in tissue maintenance, wound healing and ocular pathology.Exp Eye Res2004;79(5):677-688.
3 Yan L, Wu W, Wang Z, Li C, Lu X, Duan H, Zhou J, Wang X, Wan P,Song Y, Tang J, Han Y. Comparative study of the effects of recombinant human epidermal growth factor and basic fibroblast growth factor on corneal epithelial wound healing and neovascularzation in vivo and in vitro.Ophthalmic Res2013;49(3):150-160.
4 Poon AC, Geerling G, Dart JK, Fraenkel GE, Daniels JT. Autologous serum eyedrops for dry eyes and epithelial defects: clinical and in vitro toxicity studies.Br J Ophthalmol2001;85(10):1188-1197.
5 Okada Y, Reinach PS, Kitano A, Shirai K, Kao WW, Saika S.Neurotrophic keratopathy; its pathophysiology and treatment.Histol Histopathbol2010;25(6):771-780.
6 Mantelli F, Nardella C, Tiberi E, Sacchetti M, Bruscolini A, Lambiase A. Congenital corneal anesthesia and neurotrophic keratitis: diagnosis and management.Biomed Res Int2015;2015:805876.
7 Shukla D. Semaphorin 7a in herpetic neurotrophic keratitis.Invest Ophthalmol Vis Sci2015;56(2):1108.
8 Weyns M, Koppen C, Tassignon MJ. Scleral contact lenses as an alternative to tarsorrhaphy for the long-term management of combined exposure and neurotrophic keratopathy.Cornea2013;32(3):359-361.
9 Leiper LJ, Ou J, Walczysko P, Kucerova R, Lavery DN, West JD,Collinson JM. Control of patterns of corneal innervation by Pax6.Invest Ophthalmol Vis Sci2009;50(3):1122-1128.
10 Lin T, Gong L. Sodium hyaluronate eye drops treatment for super ficial corneal sbrasion caused by mechanical damage: a randomized clinical trial in the People’s Republic of China.Drug Des Devel Ther2015;9(1):687-694.
11 Tosi GM, Marigliani D, Bacci T, Balestrazzi A, Martone G, Polito MS. Impact of intraoperative topical hydroxypropyl methylcellulose 2% versus sodium hyaluronate 1.2% on corneal reepithelialization after intentional epithelial debridement during vitrectomy.Cornea2014;33(9):942-945.
12 Garrett Q, Xu S, Simmons PA, Vehige J, Xie RZ, Kumar A, Flanagan JL, Zhao Z, Willcox MD. Carboxymethyl cellulose stimulates rabbit corneal epithelial wound healing.Curr Eye Res2008;33(7):567-573.
13 Lopez Bernal D, Ubels JL. Artificial tear composition and promotion of recovery of the damage corneal epithelium.Cornea1993;12(2):115-120.
14 Watson SL, Daniels JT, Geerling G, Dart JK. Clinical trials of therapeutic ocular surface medium for moderate to severe dry eye.Cornea2010;29(11):1241-1246.
15 Johnson ME, Murphy PJ, Boulton M. Effectiveness of sodium hyaluronate eyedrops in the treatment of dry eye.Graefes Arch Clin Exp Ophthalmol2006;244(1):109-112.
16 Cohen S, Martin A, Sall K. Evaluation of clinical outcomes in patients with dry eye disease using lubricant eye drops containing polyethylene glycol or carboxymenthylcellulose.Clin Ophthalmol2014;8:157-164.
17 Kymionis GD, Liakopoulos DA, Grentzelos MA, Tsoulnaras KI, Detorakis ET, Cochener B, Tsilimbaris MK. Effect of the regenerative agent poly (carboxymethylglucose sulfate ) on corneal wound healing after corneal cross-linking for keratocoms.Cornea2015;34(8):928-931.
18 Ghanem VC, Karajosé N, Ghanem RC, Coral SA. Photorefractive keratectomy and butter fly laser epithelial keratomileusis: a prospective,contralateral study.J Refract Surg2008;24(7):671-684.
19 Pallikaris IG, Papatzanaki ME, Stathi EZ, Frenschock O, Georgiadis A.Laser in situ keratomileusis.Lasers Surg Med1990;10(5):463-468.
20 Doughty MJ, Glavin S. Efficacy of different dry eye treatments with artificial tears or ocular lubricants: a systematic review.Ophthalmic Physiol Opt2010;29(6):573-583.
21 Turley EA, Noble PW, Bourguignon LY. Signaling properties of hyaluronan receptors.J Biol Chem2002;277(7):4589-4592.
22 Calikoglu E, Sorg O, Tran C, Grand D, Carraux P, Saurat JH, Kaya G. UVA and UVB decrease the expression of CD44 and hyaluronate in mouse epidermis, which is counteracted by topical retinoids.Photochem Photobiol2006;82(5):1342-1347.
23 Nishida T, Nakamura M, Mishima H, Otori T. Hyaluronan stimulates corneal epithelial migration.Exp Eye Res1991;53(6):753-758.
24 Weigel PH. Hyaluronan synthase. The mechanism of initiation at the reducing end and a pendulum model for polysaccharide translocation to the cell exterior.Int J Cell Biol2015;2015(26):367579.
25 García-Posadas L, Contreras-Ruiz L, Arranz-Valsero I, López-García A, Calonge M, Diebold Y. CD44 and RHAMM hyaluronan receptors in human ocular surface in flammations.Graefe’s Arch Clin Exp Ophthalmol2014;252(8):1289-1295.
26 Di G, Qi X, Zhao X, Zhang S. Efficacy of sodium hyaluronate in murine diabetic ocular surface diseases.Cornea2017;36(9):1133-1138.
27 Lopez-de la Rosa A, Pinto-Fraga J, Blazquez Arauzo F, Urbano Rodriguez R, Gonzalez-Garcia MJ. Safety and efficacy of an artificial tear containing 0.3% hyaluronic acid in management of moderate-to-severe dry eye disease.Eye Contact Lens2017;43(6):383-388.
28 Dai Y, Zhao XW, Chen P, Yu Y, Wang Y, Xie LX. Neuropeptide FF promotes revovery of corneal nerve injury associated with hyperglycemia.Invest Ophthalmol Vis Sci2015;56(13):7754-7765.
29 Ahn JI, Kuffova L, Merrett K, Mitra D, Forrester JV, Li F, Grif fith M.Crosslinked collagen hydrogels as corneal implants: effects of sterically bulky vs. non-bulky carbodiimides as crosslinkers.Acta Biomater2013;9(8):7796-7805.
30 Esgin H, Erda N. Endothelial polymegethism and pleomorphism induced by daily-wear rigid gas-permeable contact lenses.CLAO J2002;28(1):40-43.
Correspondence to:Xiu-Ming Jin. Eye Center, Second Affiliated Hospital of Zhejiang University School of Medicine,Hangzhou 310000, Zhejiang Province, China. lzyjxm@zju.edu.cn
Received:2017-08-11 Accepted: 2018-03-02
Abstract ● AlM: To observe the efficacy of different artificial eye drops on corneal epithelium healing in rabbit.● METHODS: Thirty-five rabbits with 6 mm diameter central corneal epithelium removed were randomly assigned to six groups: 0.9% normal saline (NS) group, 0.1%hyaluronate (HA) group, 0.3% HA group, Tears Naturale Free®(TNF) group, 0.4% polyethylene glycol (PEG) group,0.5% carboxymethyl cellulose (CMC) group and blank control group. Treatments were administered topically four times daily. Corneal epithelium healing was evaluated by the percentage reduction in wound area at 24, 36, 48, 60,and 72h after removal of the corneal epithelium. Cornea re-epithelialization was also assessed by histological analysis and electron microscopy.● RESULTS: All corneal wounds completely re-epithelialized in less than 72h. The average re-epithelialization time was 47.61±4.25h in the 0.3% HA group and 49.72±1.05h in the 0.9% NS group, followed by 0.1% HA, TNF, 0.4% PEG, 0.5%CMC, and lastly by the control group. Compared to the control group, there were significant differences among 0.3% HA, 0.9% NS, PEG, and TNF (P<0.05) groups. At the first 24h, re-epithelialization at the 0.3% HA, TNF, and 0.9%NS treatment groups were significantly faster than the other groups. At 48h post-wounding, corneal epithelium is nearly completing re-epithelialization at 0.3% HA and 0.9%NS treatment groups. Electron microscopy revealed that there were a large number of vacuoles in the cells of the 0.9% NS group at 72h.● CONCLUSlON: Artificial tears promote corneal reepithelium varied in the efficacy. Obviously, all artificial eye drops better than blank group. ln the process of corneal healing, corneal epithelium cells suffered from hypoxia caused by NS.
● KEYWORDS:artificial tears; cornea; re-epithelialization;healing; rabbit; vesicles
DOl:10.18240/ijo.2018.07.04
Citation:Zhang Y, Lu XY, Hu RJ, Fan FL, Jin XM. Evaluation of artificial tears on cornea epithelium healing. Int J Ophthalmol 2018;11(7):1096-1101