Characteristics, management, and outcome of squamous carcinoma of the conjunctiva in a single tertiary cancer center in Jordan
Ata Rajeh1, Fareed Barakat2, Samer Khurma1, Khaleel AlRawashdeh1, Osama H. Ababneh3, Ibrahim AlNawaiseh1, Mustafa Mehyar1, Ghadeer Abdeen4, Imad Jaradat5, Mona Mohammad1, Yacoub A. Yousef1
1Department of Surgery (Ophthalmology), King Hussein Cancer Centre (KHCC), Amman 11941, Jordan
2Department of Pathology, King Hussein Cancer Centre(KHCC), Amman 11941, Jordan
3Department of Ophthalmology, The University of Jordan and Jordan University Hospital, Amman 11941, Jordan
4Department of Medical Oncology, King Hussein Cancer Centre (KHCC), Amman 11941, Jordan
5Department of Radiation Oncology, King Hussein Cancer Centre (KHCC), Amman 11941, Jordan
INTRODUCTION
Ocular surface squamous neoplasia (OSSN) is a spectrum of conjunctival diseases that include conjunctival dysplasia, carcinoma in situ (CIS) and invasive squamous cell carcinoma (SCC)[1]. It may arise from dysfunctional limbal stem cells that have been altered by various mutagenic agents[2]. The incidence of OSSN ranges from 0.02 to 3.5 per 10 000, and it is mostly unilateral diseases[3-4]. Rarely bilateral OSSN can be seen in immunocompromised patients and eyes with uncontrolled atopic kerato-conjunctivitis, and it usually occurs in middle or older ages[1,4-6]. OSSN usually presents in the interpalpebral area either as a fleshy, gelatinous,elevated lesion or as a sessile, papillomatous lesion. Presence of feeding vessels, intrinsic vascularity, and a nodular lesion raise suspicion of invasive SCC, but no clear clinical criteria for differentiation between CIS and SCC are present[7]. SCC is locally invasive (can invade both the orbit and the eye globe), and can metastasis to regional lymph nodes[8]. The risk factors for OSSN include sun exposure, cigarette smoking,HIV, human papilloma virus (HPV16-18), ultraviolet-B radiation[9-11]. There is limited data about the features and outcome of management of OSSN in the Middle East thereforewe are describing herein the features and outcome of OSSN management in a single tertiary cancer center in Jordan [King Hussein Cancer Center (KHCC), Amman, Jordan].
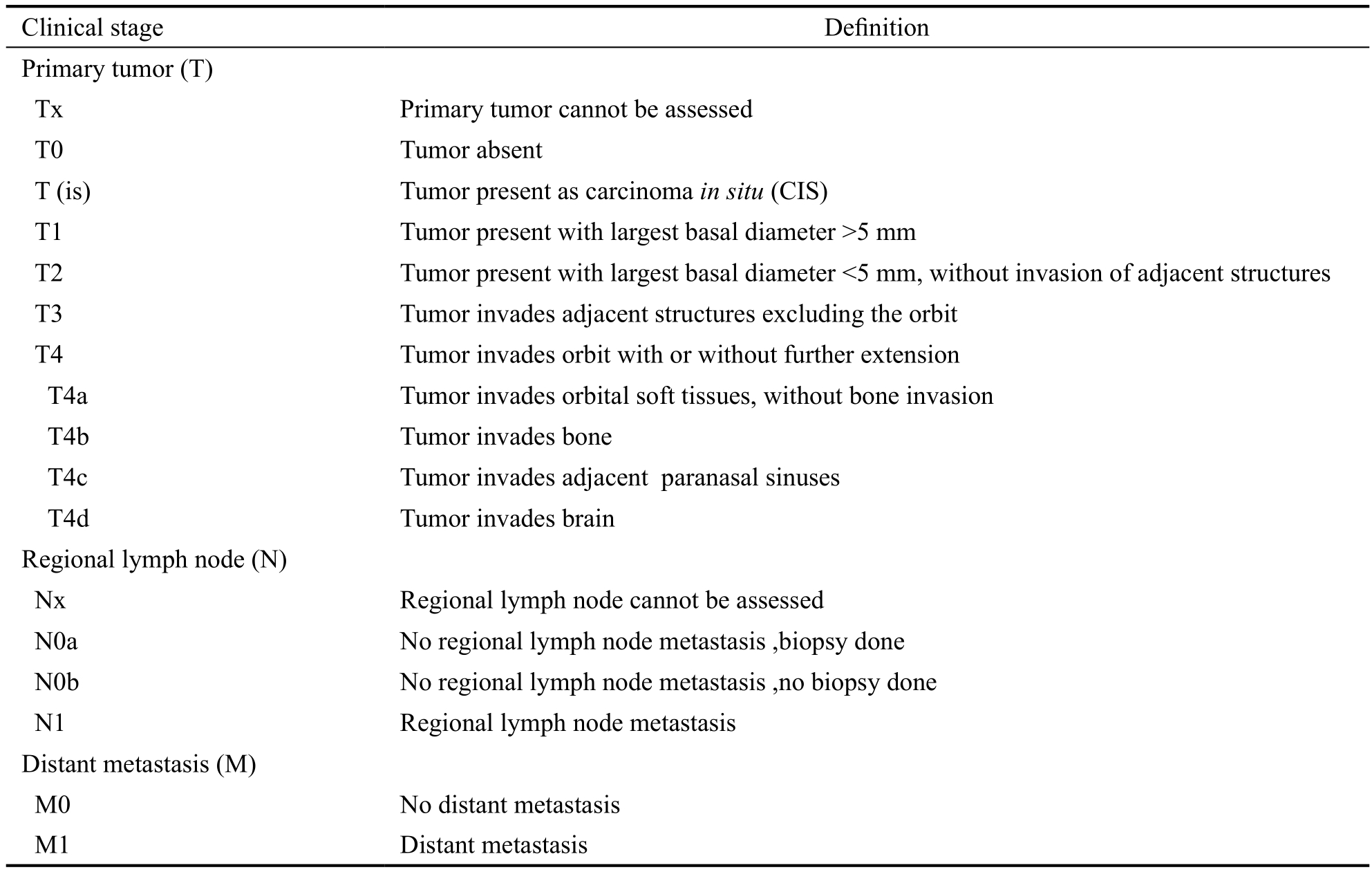
Table 1 Squamous cell carcinoma of the conjunctiva: definition of TNM staging[12]
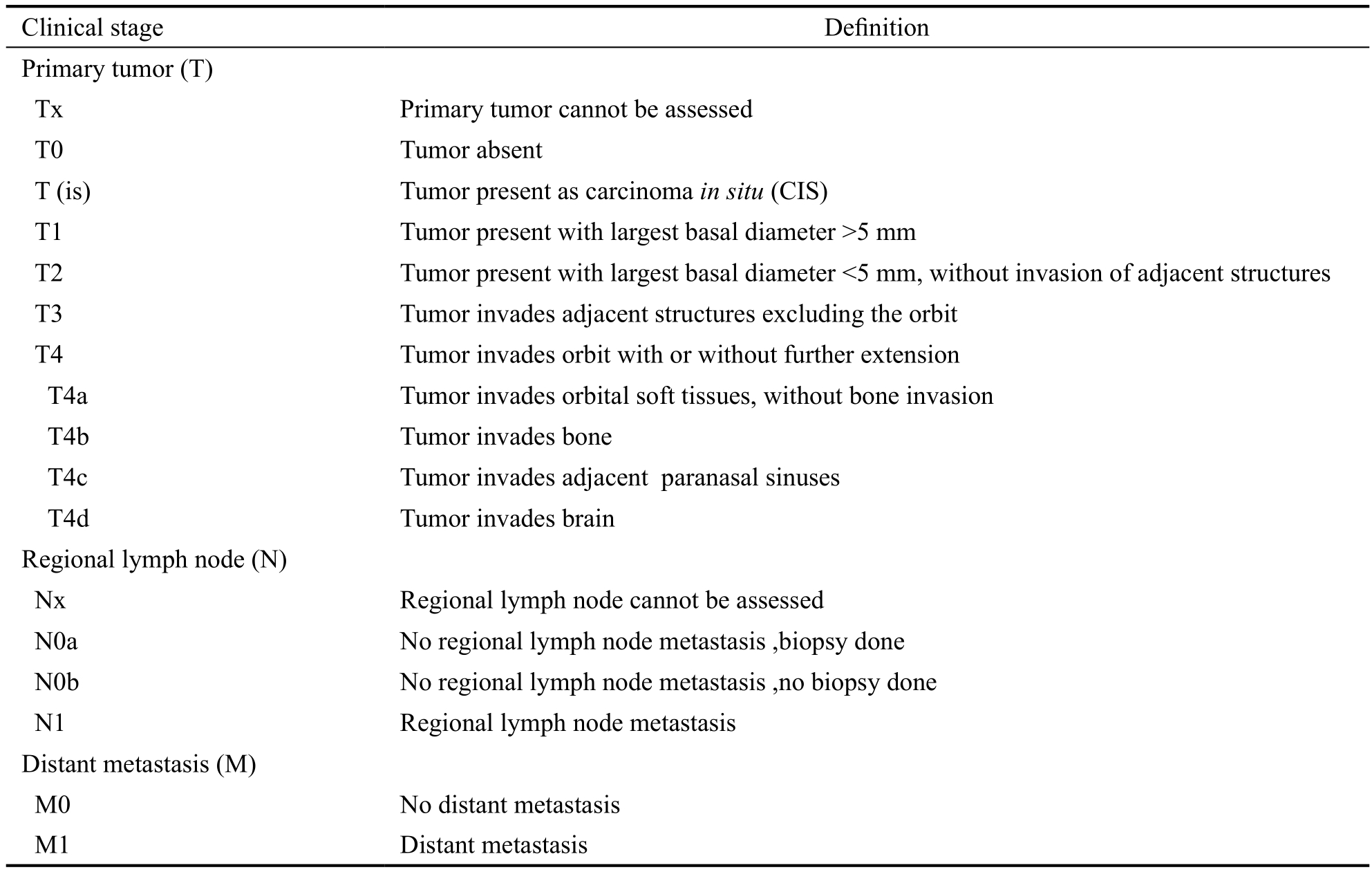
Clinical stage De finition Primary tumor (T)Tx Primary tumor cannot be assessed T0 Tumor absent T (is) Tumor present as carcinoma in situ (CIS)T1 Tumor present with largest basal diameter >5 mm T2 Tumor present with largest basal diameter <5 mm, without invasion of adjacent structures T3 Tumor invades adjacent structures excluding the orbit T4 Tumor invades orbit with or without further extension T4a Tumor invades orbital soft tissues, without bone invasion T4b Tumor invades bone T4c Tumor invades adjacent paranasal sinuses T4d Tumor invades brain Regional lymph node (N)Nx Regional lymph node cannot be assessed N0a No regional lymph node metastasis ,biopsy done N0b No regional lymph node metastasis ,no biopsy done N1 Regional lymph node metastasis Distant metastasis (M)M0 No distant metastasis M1 Distant metastasis
SUBJECTS AND METHODS
This study was approved by the Institutional Review Board at KHCC. It was a retrospective case series of 31 eyes for 31 consecutive patients between January 2009 and March 2016 who had conjunctival squamous neoplasia. Selection required access to patients' medical charts, pathologic records, radiology reports, and laboratory tests. Outcome measures included: age at diagnosis, gender, presenting symptoms and visual acuity at presentation. Evaluated clinical characteristics included:tumor location, laterality, invasion of nearby structures (cornea,fornix, lid, and orbit), presence of intraocular invasion, TNM staging[12], pathological features of the tumor; (invasiveness and tumor differentiation), treatment modalities, visual acuity,presence and site of metastasis, and mortality.
Inclusion and Exclusion CriteriaThe eligibility criteria for inclusion were eyes with pathologic diagnosis of conjunctival squamous neoplasia that was followed for at least 6mo after treatment.
Pathological Characteristics and De finitionsIn this study,the tumors were classified according to the pathology into 3 types: dysplasia, CIS and invasive SCC. Differentiation of SCC was divided into well, moderate, and poorly differentiated tumors[1]. The location of tumor was divided into: nasal,temporal, superior, and inferior quadrants. TNM staging was according to the 7thedition of the American Joint Committee on Cancer (AJCC) staging system (Table 1). Tumor invasion to the orbit was diagnosed by CT scan.
Tumor ManagementSurgical excision is the mainstay of OSSN treatment[13]. Localized tumors were treated by surgical excision with 2-3 mm safety margin followed by double freeze thaw cryotherapy for tumor margin and tumor bed[14-15].The excised specimens were sent for histopathological examination. Invasive SCC and CIS cases were treated after surgery by topical mitomycin 0.04% [protocol: two cycles of topical mitomycin (0.04%), that was applied four times daily for 14d per cycle separated by 2wk off-therapy in between].In this study, indications for enucleation included intra ocular invasion, for exenteration included orbital invasion, and for radiation included residual tumor and/or perineural invasion.
Statistical AnalysisDescriptive analysis was done using mean, median, and range. The P value was measured using the exact Fisher test to test the predictive power of each factor.P-value of less than 0.05 was considered significant.
RESULTS
Between January 2009 and March 2016, 35 eyes from 35 patients had the pathologic diagnosis of conjunctival neoplastic disease. Four eyes were excluded from this analysis because of lost follow up after less than 6mo post treatment.
Demographics and Clinical FeaturesThirty one eyes from 31 patients with a median age of 58y (range 28 to 84y) were studied. Tumors were in the right eye in 11 (35%) patients and in the left in 20 (65%) patients, and none of them had bilateral disease. Sixty- five percent of patients (n=20/31) were males.
Tumor involved the nasal quadrant in 22 eyes (71%), the temporal quadrant in 7 (23%) eyes, the superior quadrant in 1 (3%) eye, and the inferior quadrant in 1 (3%) eye. Nearby structural invasion was seen in 21 (68%) eyes; invasion to the cornea in 17 (55%) eyes, invasion to the fornix in 1 (3%)eye, invasion to the eyelid in 2 (6%) eyes. Tumor invasion to the orbit was seen at diagnosis only in 1 (3%) eye, and as recurrence in another 2 (6%) eyes (Table 2). The visual acuity at diagnosis range from hand motion to 20/20 [less than 20/200 in 3 (10%) eyes, between 20/200 and 20/40 in 6 (19%)eyes, and 20/40 or better in 22 (71%) eyes]. Systematically,2 (6%) patients had actinic keratosis, 1 (3%) had Xeroderma pigmentosum, 1 (3%) was on immunosuppressive therapy for his kidney transplant, and no one had HIV.
Staging and Pathological Features of the TumorsPathologically, CIS was seen in 12 cases (39%) and invasive SCC in 19 cases (61%), and no single case of conjunctival dysplasia was seen in this series. Out of the 19 (61%) eyes with invasive SCC; 2 (6.5%) cases were stage T1N0M0 stage,3 (10%) were stage T2N0M0, 11 (35%) cases were stage T3N0M0, 3 (10%) cases were stage T4 due to orbital invasion(2 were T4aN0M0, one was T4aN1M1 due to lymphatic and distant metastasis). Regarding tumor differentiation, the well, moderately, and poorly differentiated tumors account for 7cases (23%), 9 cases (29%) and 3cases (10%) of SCC patients respectively (Table 2).
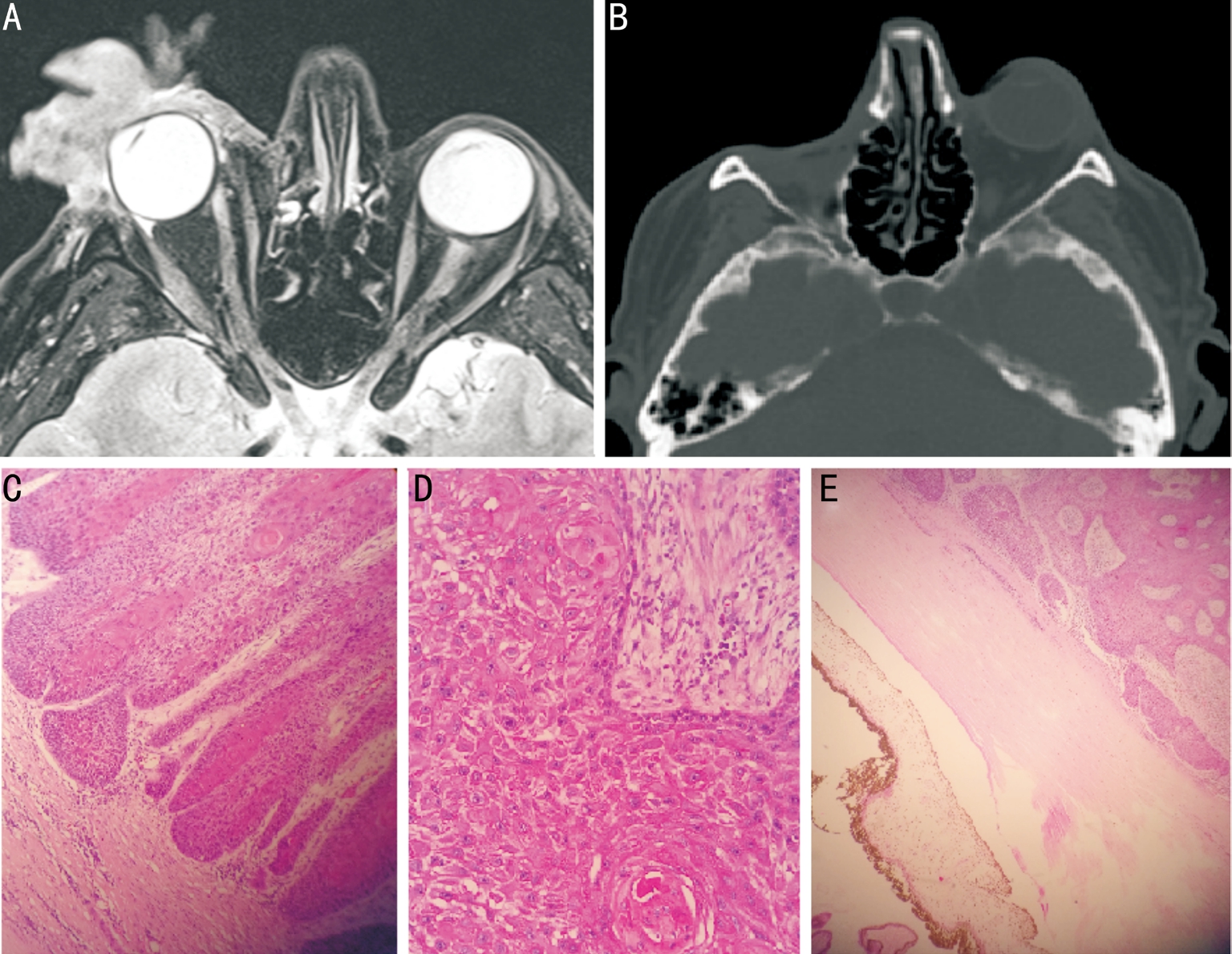
Tumor Primary TreatmentIn this series, 26 (84%) affected eyes were treated by surgical excision of the tumor (with 2-3 mm safety margin) and double freeze thaw cryotherapy for tumor margin and tumor bed. Two to four weeks after surgery,they received topical chemotherapy (mitomycin 0.04%) for 4wk. One eye was treated by orbital exenteration as primary treatment because of orbital invasion (Figure 1). No single eye in this series had intraocular invasion so no eye was treated by modified enucleation. Four (13%) cases were managed initially outside our center by surgical excision without cryotherapy or topical chemotherapy, and all of them were referred our tertiary center for management of tumor recurrence.
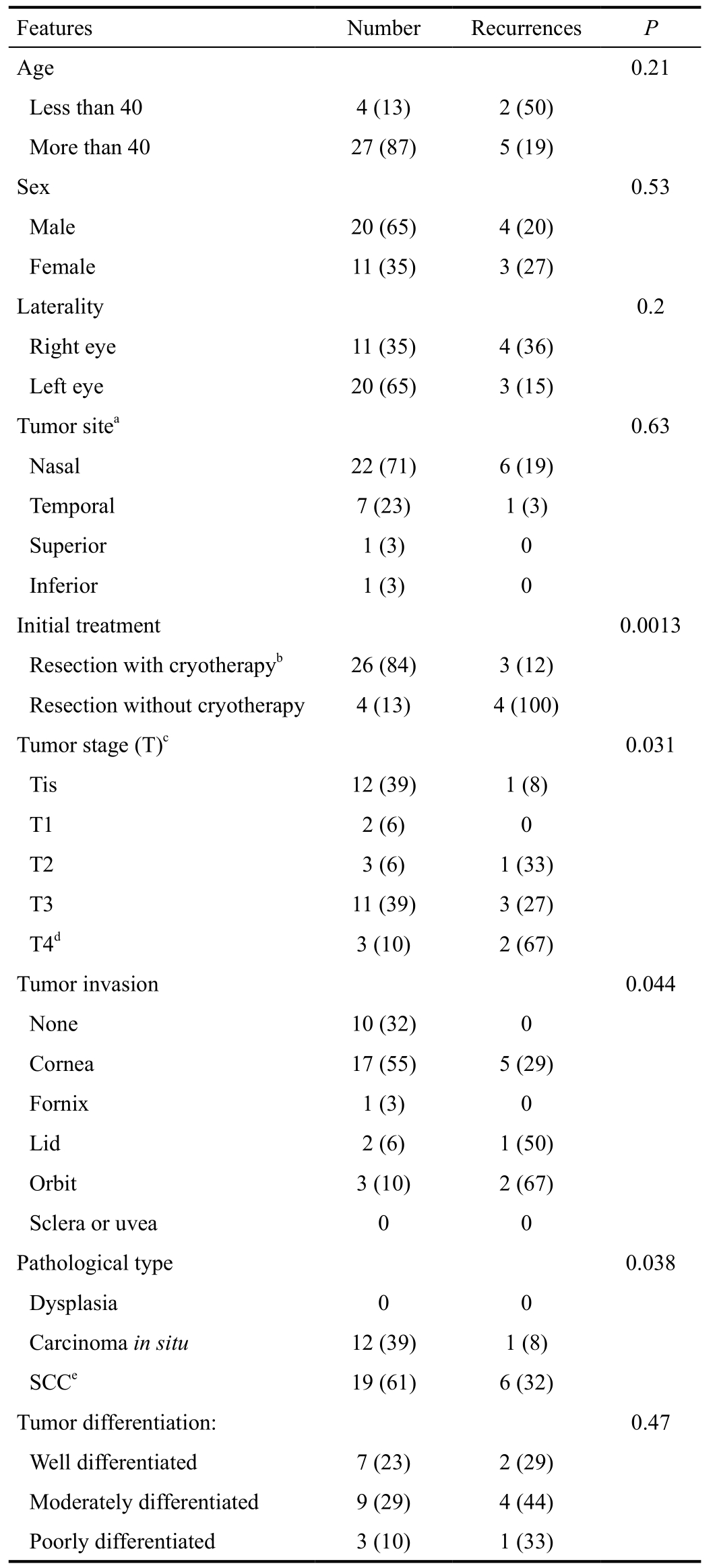
Statistical CorrelationsThe overall recurrence rate was 23%(n=7/31). The recurrence rate was not correlated significantly to age, gender, laterality, tumor site, or tumor differentiation(Table 2). However, tumor extension onto the nearby structures(P=0.044), tumor pathological type (P=0.038), and tumor TNM stage (P=0.031) were associated with a statistically significant higher risk of tumor recurrence (Table 2).
Tumor Clinical and Pathologic Features Versus RecurrenceThe higher the AJCC (T) stage and the more locally invasive tumors were more likely to develop recurrence (Table 2).Recurrence rate was seen in 8% of Tis tumors, and in 0, 33%,27%, and 67% of T1, T2, T3, and T4 tumors consecutively.T2-T4 tumors had significantly higher rate of recurrence(P=0.031) than Tis and T1 tumors. Similarly, tumors defined pathologically as invasive SCC had 32% recurrence rate that is significantly higher than the 8% recurrence rate for tumors pathologically defined as CIS (P=0.038).
Table 2 Demographics and tumor features and correlation with tumor recurrence rate n (%)
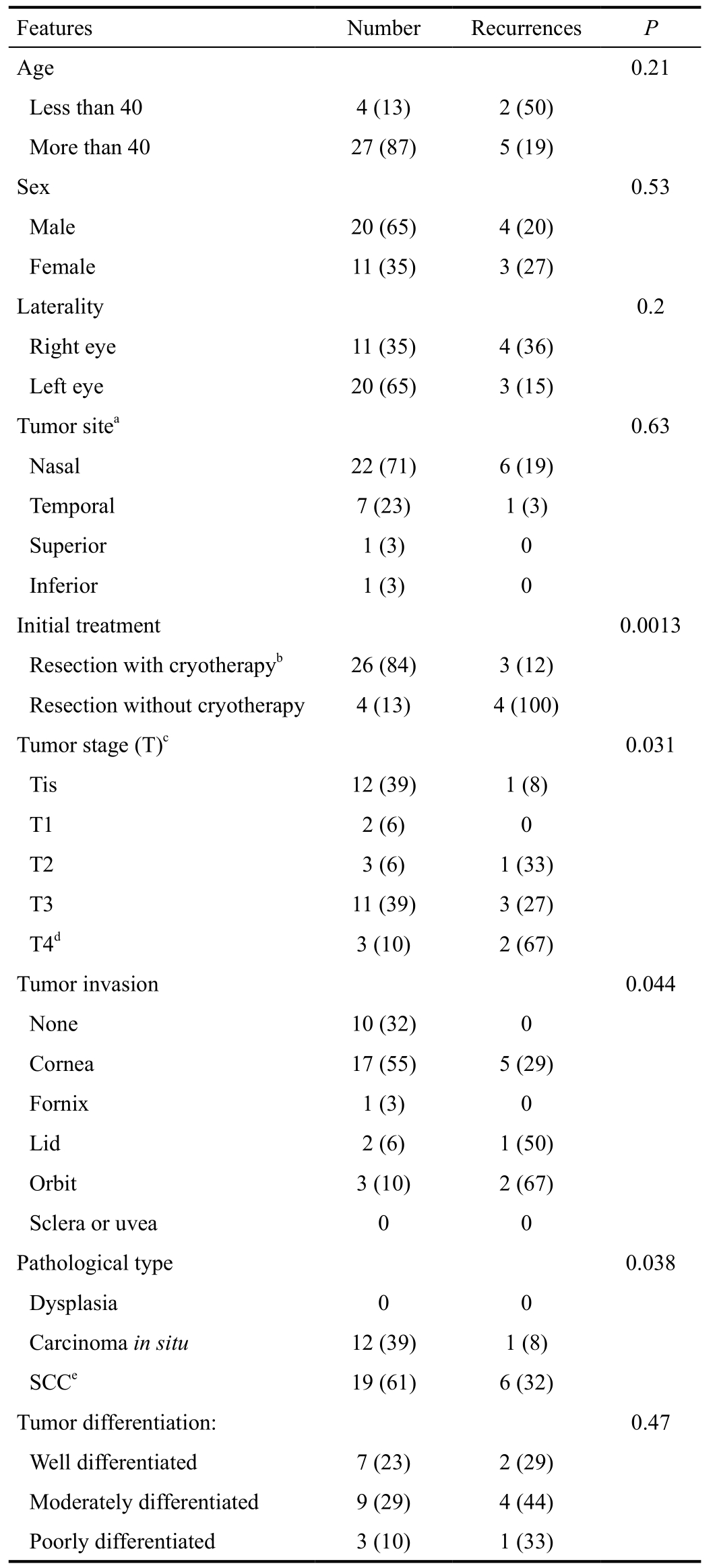
aThe same tumor may involve more than one quadrant at the same time;bThis treatment also was followed by topical chemotherapy.The case with primary exenteration is not included here;cT stage according to the 7thedition AJCC staging system[12];dThe 3 eyes with stage T4 had orbital soft tissue invasion;eSCC: Invasive squamous cell carcinoma.
?
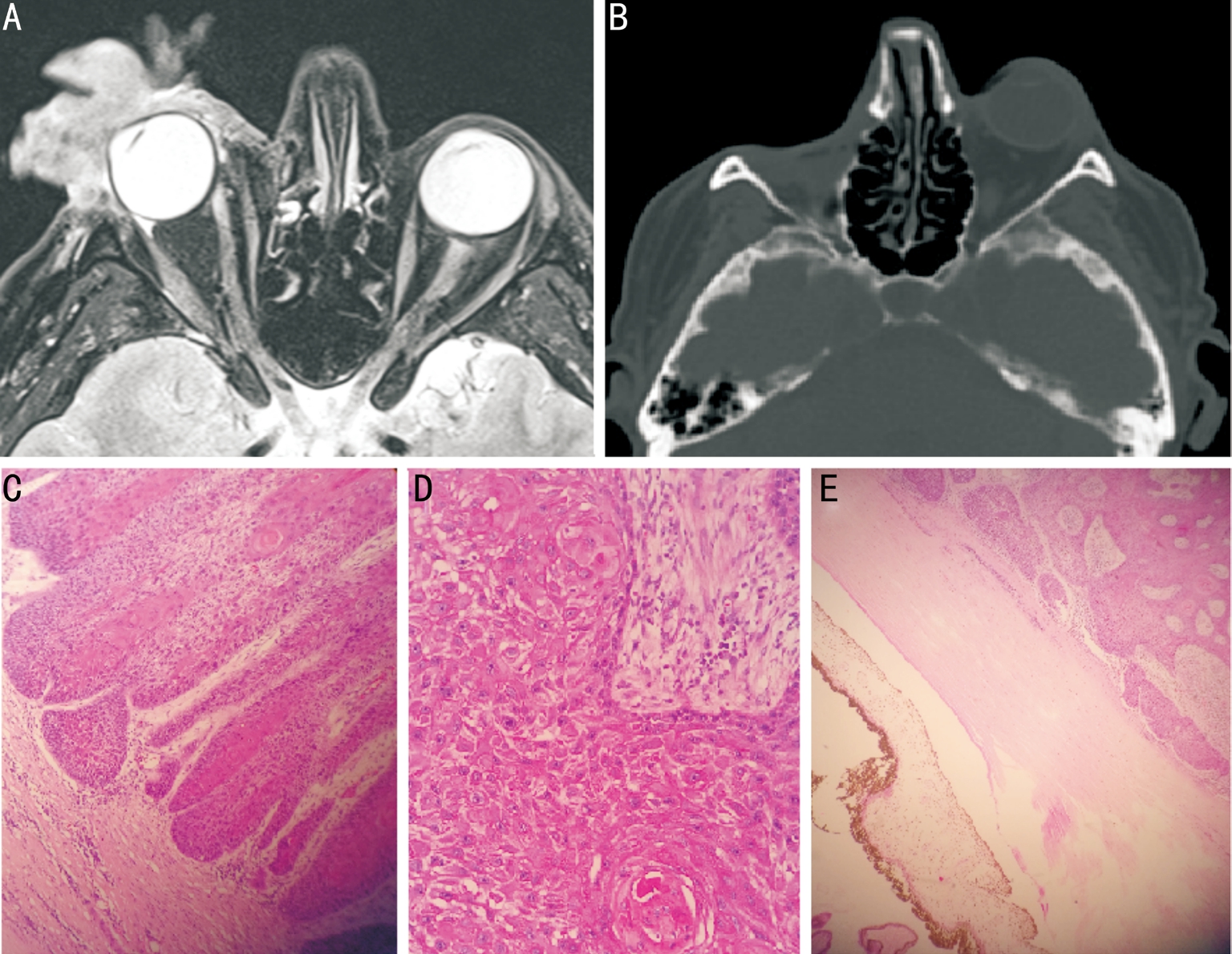
Figure 1 Radiologic and pathologic findings for a patient presented with orbital invasion of SCC because of 4y delay before treatment A: T2 axial MRI at diagnosis showed large exophytic right orbital mass with minimal intra orbital/extraconal and preseptal invasion; B: Orbit CT scan was done 6mo after exenteration, and revealed empty right orbital socket with no tumor recurrence; C: Pathologically, the tumor showed squamous pearls with keratin (H&E, 200×); D: Intra cellular bridges in well differentiated squamous cell carcinoma (H&E, 200×); E: The tumor was abutting the sclera from outside with no intra ocular invasion (H&E, 200×).
Primary Treatment Methods Versus RecurrenceOf the 31 tumors in this series, 30 cases were treated initially by excision. Subgroup analysis revealed that in the 4 eyes that was treated by primary tumor excision as the sole treatment(without cryotherapy or topical chemotherapy), recurrences were seen in all of them (100%), and therefore were referred to our tertiary cancer center. In 26 cases, the surgical excision was combined with cryotherapy and followed by adjuvant topical chemotherapy. In this group recurrence was seen in 12% (n=3/26) of cases, which is significantly less than the recurrence rate in tumors that treated by surgical excision alone (P=0.0013). One eye (3%) had orbital invasion and treated by primary exenteration. This patient developed was refusing treatment for 4y till he accepted to do exenteration.He had lymphatic metastasis 3mo after the surgery but no local recurrence, and passed away after 9mo with posterior reversible encephalopathy syndrome (PRES).
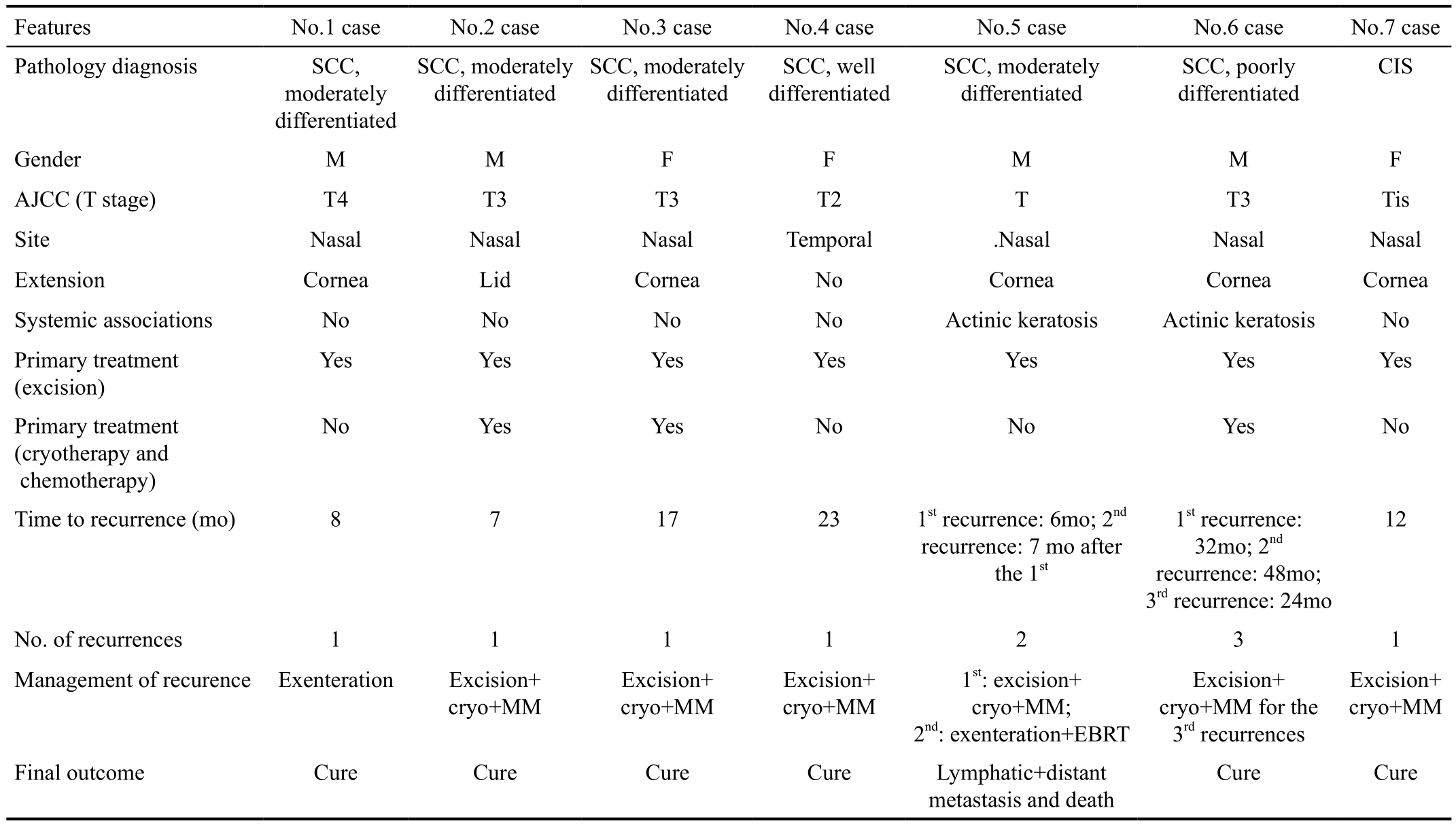
Follow up and Treatment of Tumor RecurrenceThe mean follow up in this series was 38mo (median 27mo; range, 12 to 106mo). Recurrence was seen in 7 (23%) cases. Six (86%)of them had the pathologic diagnosis of invasive SCC, and 1(14%) was CIS. Out of the 7 cases with recurrence, 4 cases(57% of total recurrences) were managed initially by surgical excision alone (outside our center). Two of them (one was Tis, and one was T2) presented with localized conjunctival recurrence and managed by excision with cryotherapy followed by topical mitomycin, and none of them had more recurrences. The third case was 43 years old male who was referred 8mo after surgery with orbital invasion and therefore was managed by orbital exenteration (Pathology showed no residual tumor or perineural invasion therefore no radiation therapy was applied), and then no recurrence or metastasis was detected over 2y of follow up (Table 3).
The 4threcurrent case was 63 years old male who had also actinic keratosis. He developed two recurrences after the primary surgery (first after 3mo, and second after 7mo).The first recurrence was managed by surgical excision with cryotherapy and topical chemotherapy, but there was orbital invasion at the 2ndrecurrence and managed by orbital exenteration followed by external beam radiation therapy. This patient later presented with lymph node and distant metastasis and passed away (Table 3).
Out of 27 patients who were managed initially in our center(26 cases by excision, cryotherapy, and topical mitomycin, and one case by primary exenteration due to orbital invasion), only 3 (11%) had local recurrence, and none of them was invading the orbit. Two eyes were successfully treated by another trial of surgical excision with cryotherapy and topical mitomycin,while the third one who was 67 years old male with actinic keratosis developed recurrence 3 times in his eye within 94mofollow up after the first surgery (1st, 2ndand 3rdrecurrences developed after 32mo,48mo and 72mo respectively).Recurrences were treated by more excision, cryotherapy and topical mitomycin and then no recurrence was seen over 3y follow up (Table 3).
Table 3 Recurrent cases of malignant conjunctival squamous carcinoma
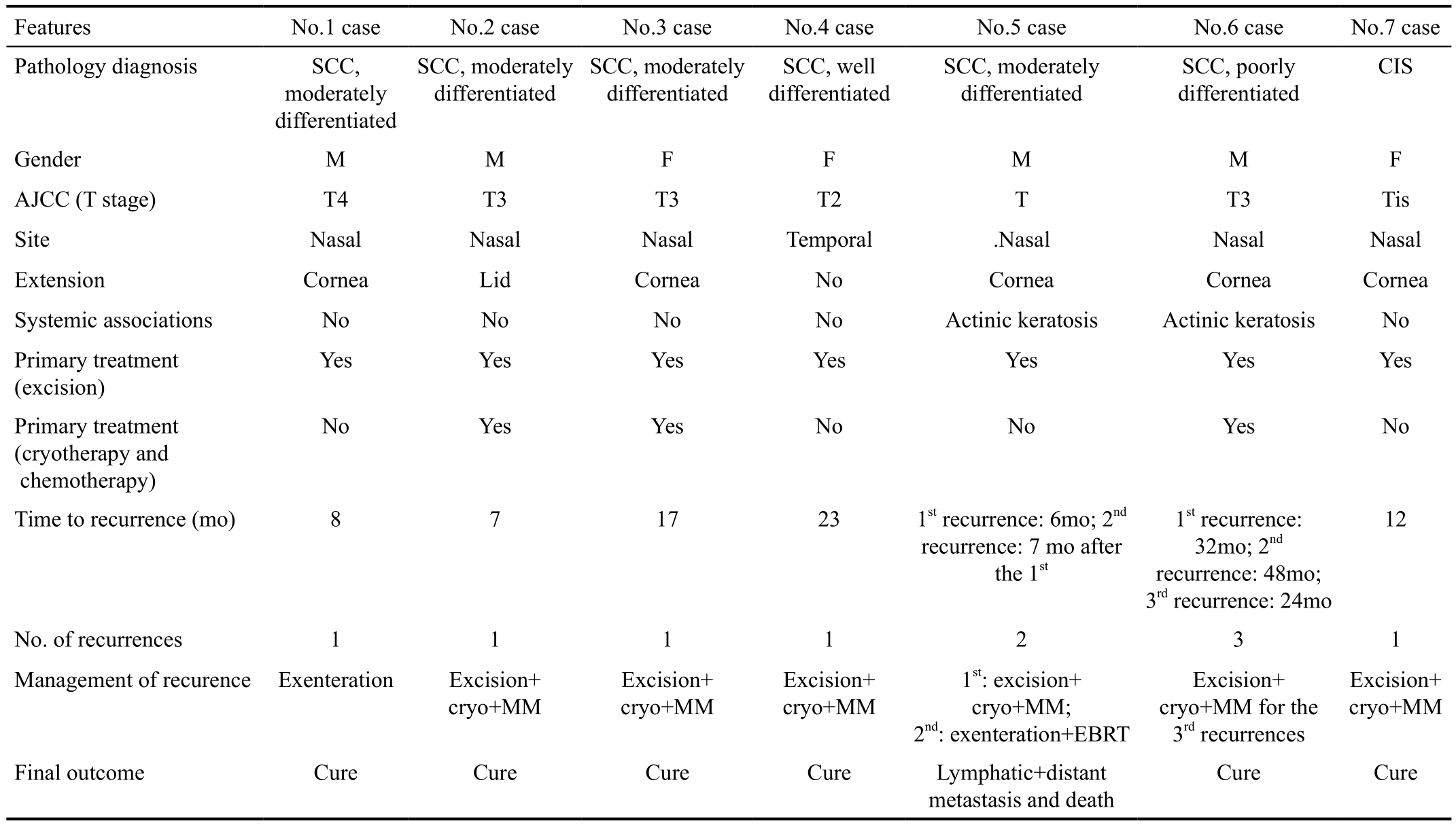
SCC: Squamous cell carcinoma; CIS: Carcinoma in situ; M: Male, F: Female; Cryo: Cryotherapy; MM: Topical mitomycin; EBRT: External beam radiation therapy.
Features No.1 case No.2 case No.3 case No.4 case No.5 case No.6 case No.7 case Pathology diagnosis SCC,moderately differentiated SCC, moderately differentiated SCC, moderately differentiated SCC, well differentiated SCC, moderately differentiated SCC, poorly differentiated CIS Gender M M F F M M F AJCC (T stage) T4 T3 T3 T2 T T3 Tis Site Nasal Nasal Nasal Temporal .Nasal Nasal Nasal Extension Cornea Lid Cornea No Cornea Cornea Cornea Systemic associations No No No No Actinic keratosis Actinic keratosis No Primary treatment(excision)Yes Yes Yes Yes Yes Yes Yes Primary treatment(cryotherapy and chemotherapy)No Yes Yes No No Yes No Time to recurrence (mo) 8 7 17 23 1strecurrence: 6mo; 2ndrecurrence: 7 mo after the 1st1strecurrence:32mo; 2ndrecurrence: 48mo;3rdrecurrence: 24mo 12 No. of recurrences 1 1 1 1 2 3 1 Management of recurence Exenteration Excision+cryo+MM Excision+cryo+MM Excision+cryo+MM 1st: excision+cryo+MM;2nd: exenteration+EBRT Excision+cryo+MM for the 3rdrecurrences Excision+cryo+MM Final outcome Cure Cure Cure Cure Lymphatic+distant metastasis and death Cure Cure
Tumor recurrence was detected as early as 6mo to 32mo after last treatment (mean 15mo). Four cases (57%) of the recurrences were detected within 12mo from treatment, 2 cases (29%) were detected within the second year of follow up, and only 1 (14%) eye had recurrence within the 3rdyear after treatment. No significant change in visual acuity was seen except in the 3 eyes that were exenterated.
Disease related mortality developed in 2 cases (6%). Both of them had orbital invasion treated by exenteration (described above). One of them developed lymph node and distant metastasis at the same time, and the second one developed lymphatic metastasis. Orbital invasion was very significant risk factor for metastasis and death (P=0.0065).
DISCUSSION
SCC has been found to be the most common conjunctival malignancy[16], and it is life threatening if not treated adequately. Significant predictors for tumor recurrence are tumor invasion to adjacent structures, pathologic characteristics, higher AJCC T-stage of the disease, and inadequate primary treatment. Recurrence is not correlated significantly to age, gender, laterality, or tumor differentiation at presentation, and in line with previous reports, a slight male predominance (65% were males) was noted in this series, likely related to increased occupational exposure to sunlight[3]. While local invasion has been reported to be the most prevalent mechanism of tumor spread, and comprise in previous studies about 12% to 16% (regarding orbital invasion)of invasive cases[17-19], it is not the case in some recent studies,where Chauhan et al[20]found orbital invasion was present in nearly 31% (14/44 of SCC cases). However, in our series,orbital involvement was seen in 6% of all cases, and 10% of invasive cases. In terms of metastasis in our series, 2 (6%)died with metastasis; both of them had lymphatic metastasis,and one of these 2 patients had additional lung metastasis.However, while these ratio are nearly similar to what reported by Yousef and Finger[21], in their study, finding lymph node and distant metastasis at 1% and 0 respectively, there are higher proportions as reported by Chauhan et al[20], being at 12%and 6% for lymph node and distant metastasis respectively.The more severe pathological types of conjunctival squamous carcinoma, as found by Galor et al[22], seem to recur at higher rates[21], being about 13% for CIS and 22.2% for SCC.When adjunctive cryotherapy is used with surgical excision,recurrence rates of OSSN were reduced by almost 50%(instead of 13% at 1y and 31% at 5y, recurrence rate became 8%and 16% at 1 and 5y respectively)[22]. Others found the recurrence rate still the same throughout 1, 2, and 5y after management with adjunctive cryotherapy, being at 7.1%[23]. However rather than combining recurrence results as a whole under OSSN category, it is better to separate between recurrences related to SCC and those related to non-invasive types. In this series,the overall recurrence rate was 23%; only 8% for carcinoma in situ tumors, and 32% for squamous cell carcinoma (while this overall high recurrence SCC rate explained by the cases which treated initially outside our center, which all recurred later, this is not the case regarding patients treated from the start by us, who had recurrences of only 3/19 cases, 15.7%).We may explain our relatively low risk of recurrence, by the fact that most of our cases were treated from the beginning by a combination of surgical excision with cryotherapy and topical chemotherapy. In fact the only case of recurrent CIS in our series was treated initially outside our center by surgical excision without cryotherapy or chemotherapy. Of interest, all patients who treated initially by excision alone had recurrence, even a case of carcinoma in situ, this could be related to selection bias toward referring advanced and recurrent cases for our tertiary cancer center, but it can also be because of inadequate primary treatment that lacks adjunctive cryotherapy, and inadvertent invagination of tumor tissue by general ophthalmologists who are not expert with malignant tumors.
In general, it is difficult to define scleral involvement accurately (which is a risk factor for both tumor recurrence and intraocular invasion), so in the authors’ center, the scleral base is treated with double freeze cryotherapy in addition to the margin[15], and this may explain why no single cases had intraocular recurrence in our series. In this series, orbital invasion was the most important predictive factor for tumor metastasis and death (P=0.0065), therefore conjunctival tumors should be eradicated before getting to the point of orbital invasion, which may be more likely to happen after recurrence[2 out of 7 recurrent cases (29%) developed orbital invasion,while only one case presented initially with orbital invasion and that’s due to patient denial and 4y delay between signs and treatment], and unfortunately the only way to remove orbital SCC with safety margin is by exenteration, that harbors bad psychological and cosmetic impact on patient and his family. According to the seventh edition of the AJCC staging system, the present case series showed that the recurrence rate was higher in advanced AJCC T-stage tumors mainly T4 tumors. This suggests the need for more aggressive treatment for tumors in advanced stages. However, this study suggests that T3 tumors had lower recurrence rate than T2 tumors,that’s may be because of the low number we had in this small series. Clearly, AJCC staging was helpful in this analysis and will allow others to compare their scientific results with those presented in this study[12]. This study described and analyzed the characteristics of malignant squamous conjunctival tumors in a tertiary cancer center in the Middle East, and examined the possible predictive factors for tumor recurrence. Although this is unique work, it is retrospective and of small size. Therefore,a larger and more comprehensive multicenter regional study should be performed to describe better the features of this rare disease and the efficacy of the various treatment methods and treatment-specific recurrence rates in the Middle East.
In conclusion, conjunctival squamous carcinoma is more common in males. Advanced AJCC T-stage, tumor local invasion, more pathologically aggressive tumors, and surgical treatment alone (without adjuvant therapy) were associated with higher risk for recurrence, and orbital invasion is the most important poor prognostic factor for metastasis and death. Treatment strategies should be affected by tumor characteristics at presentation.
ACKNOWLEDGEMENTS
We acknowledge the support of the Eye Cancer Foundation Inc. (New York, NY, USA. http://eyecancerfoundation.net)and the International Council of Ophthalmology (ICO) for Dr. Rajeh for the Ocular Oncology Fellowship. This research was supported by the Research Council, King Hussein Cancer Center (Amman, Jordan), and we thank Mr. Raed Marashdeh from King Hussein Cancer Center for solving all issues related to logistics.
Conflicts of Interest: Rajeh A,None;Barakat F,None;Khurma S,None;AlRawashdeh K,None;Ababneh OH,None;AlNawaiseh I,None;Mehyar M,None;Abdeen G,None;Jaradat I,None;Mohammad M,None;Yousef YA,None.
REFERENCES
1 Dandala PP, Malladi P, and Kavitha. Ocular Surface Squamous Neoplasia (OSSN): a retrospective study.J Clin Diagn Res2015;9(11):NC10-NC13.
2 Gichuhi S, Ohnuma S, Sagoo MS, Burton MJ. Pathophysiology of ocular surface squamous neoplasia.Exp Eye Res2014;129:172-182.
3 Asadi-Amoli F, Ghanadan A. Survey of 274 patients with conjunctival neoplastic lesions in Farabi Eye Hospital, Tehran 2006-2012. J Curr Ophthalmol2015;27(1-2):37-40.
4 Gichuhi S, Sagoo MS, Weiss HA, Burton MJ. Epidemiology of ocular surface squamous neoplasia in Africa.Trop Med Int Health2013;18(12):1424-1443.
5 Shah A, Espana EM, Singh AD. Ocular surface squamous neoplasia associated with atopic keratoconjunctivitis.Ocul Oncol Pathol2017;3(1):22-27.
6 Halkud R, Shenoy AM, Naik SM, Chavan P, Sidappa KT, Biswas S.Xeroderma pigmentosum: clinicopathological review of the multiple oculocutaneous malignancies and complications. Indian J Surg Oncol2014; (2):120-124.
7 Honavar SG, Manjandavida FP. Tumors of the ocular surface: a review.Indian J Ophthalmol2015;63(3):187-203
8 Mittal R, Rath S, Vemuganti GK. Ocular surface squamous neoplasia-Review of etio-pathogenesis and an update on clinico-pathological diagnosis.Saudi J Ophthalmol2013;27(3):177-186.
9 Di Girolamo N. Association of human papilloma virus with pterygia and ocular-surface squamous neoplasia.Eye(Lond)2012;26(2):202-211.
10 Carrilho C, Gouveia P, Yokohama H, Lopes JM, Lunet N, Ferro J, Ismail M, Walboomers J, Sobrinho-Simões M, David L. Human papillomaviruses in intraepithelial neoplasia and squamous cell carcinoma of the conjunctiva: a study from Mozambique.Eur J Cancer Prev2013;22(6):566-568.
11 McClellan AJ, McClellan AL, Pezon CF, Karp CL, Feuer W, Galor A.Epidemiology of ocular surface squamous neoplasia in a Veterans Affairs population.Cornea2013;32(10):1354-1358.
12 The AJCC Ophthalmic Oncology Task Force. Carcinoma of the conjunctiva. In: Edge SE, Byrd DR, Carducci MA, Compton CA, eds.AJCC Cancer Staging Manual. 7th ed. New York: Springer; 2009:531-533.
13 Gichuhi S, Macharia E, Kabiru J, Zindamoyen AM, Rono H, Ollando E, Wanyonyi L, Wachira J, Munene R, Onyuma T, Jaoko WG, Sagoo MS,Weiss HA, Burton MJ. Toluidine blue 0.05% vital staining for diagnosis of ocular surface squamous neoplasia in Kenya.JAMA Ophthalmol2015;133(11):1314-1321.
14 Gichuhi S, Sagoo MS. Squamous cell carcinoma of the conjunctiva.Community Eye Health2016;29(95):52-53.
15 Kashkouli MB, Heirati A, Pakdel F, Kiavash V, Naseripour M,Aghamohammadi F. Long-term follow-up of invasive ocular surface squamous cell carcinoma treated with excision, cryotherapy, and topical mitomycin C.Graefes Arch Clin Exp Ophthalmol2012;250(10):1527-1532.
16 Bunya V, Chang V. Ocular surface squamous neoplasia. American Academy of Ophthalmology Review: Assigned status Up to Date by Vatinee Bunya, MD on December 17, 2015.
17 Erie JC, Campbell RJ, Liesegang TJ. Conjunctival and corneal intraepithelial neoplasia.Ophthalmology1986;93(2):176-183.
18 Iliff WJ, Marback R, Green WR. Invasive squamous cell carcinoma of the conjunctiva.Arch Ophthalmol1975;93(2):119-122.
19 Tunc M, Char DH, Crawford B, Miller T. Intraepithelial and invasive squamous cell carcinoma of the conjunctiva: analysis of 60 cases.Br J Ophthalmol1999;83(1):98-103.
20 Chauhan S, Sen S, Sharma A, Tandon R, Kashyap S, Pushker N,Vanathi M, Sharma N. American Joint Committee on Cancer Staging and clinicopathological high-risk predictors of ocular surface squamous neoplasia: a study from a tertiary eye center in India .Arch Pathol Lab Med2014;138(11):1488-1494.
21 Yousef YA, Finger PT. Squamous carcinoma and dysplasia of the conjunctiva and cornea; an analysis of 101 cases. Ophthalmology2012;119(2):233-240.
22 Galor A, Karp CL, Oellers P, Kao AA, Abdelaziz A, Feuer W, Dubovy SR. Predictors of ocular surface squamous neoplasia recurrence after excisional surgery.Ophthalmology2012;119(10):1974-1981.
23 Li SA, Shih CY, Rosen L, Steiner A, Milman T, Udell IJ. Recurrence of ocular surface squamous neoplasia treated with excisional biopsy and cryotherapy.Am J Ophthalmol2015;160(2):213-219.e1.
Correspondence to:Yacoub A. Yousef. Consultant Ocular Oncologist King Hussein Cancer Centre, Queen Rania Street P.O. Box 1269 Al-Jubeiha, Amman 11941, Jordan. yyousef@khcc.jo Received: 2017-06-04 Accepted: 2017-08-31
Abstract ● AlM: To evaluate the features and outcome of management of malignant conjunctival squamous tumors in King Hussein Cancer Center (a referral tertiary cancer center in the Middle East).● METHODS: Retrospective case series of 31 eyes for 31 patients with conjunctival squamous neoplasia. Main outcome measures included: age, gender, laterality, tumor location, pathological features, tumor stage, treatment modality, and outcome.● RESULTS: Twenty (65%) patients were males and median age was 58y. Twenty-two (71%) eyes had the tumor in the nasal quadrant. Tumor invasion to nearby structures was seen in 19 (61%) eyes, including the cornea, fornix, eyelid,and orbit in 17 (55%), 1 (3%), 2 (6%), and 3 (10%) eyes,respectively. Eye salvage was achieved by surgical excision with cryotherapy followed by topical chemotherapy in 28 (90%) eyes, and orbital exenteration was necessary in 3 (10%) eyes due to orbital tumor invasion. Tumor recurrence was seen in 7 (23%) eyes, and the significant predictive factors for recurrence were tumor extension onto the nearby structures (P=0.04), tumor invasiveness(P=0.038), and tumor TNM stage (P=0.031). No significant change in visual acuity was seen, and disease related mortality was 6% (2 patients, both had orbital invasion by invasive squamous carcinoma).● CONCLUSlON: Conjunctival squamous carcinoma is more common in males. Advanced American Joint Committee on Cancer (AJCC) T-stage, tumor local invasion, more pathologically aggressive tumors, and surgical treatment alone (without adjuvant therapy) are associated with higher risk for recurrence, and orbital invasion is the most important poor prognostic factor for metastasis and death. Treatment strategies should be affected by tumor characteristics at presentation.
● KEYWORDS:conjunctiva; squamous cell carcinoma; metastasis
DOl:10.18240/ijo.2018.07.10
Citation:Rajeh A, Barakat F, Khurma S, AlRawashdeh K, Ababneh OH, AlNawaiseh I, Mehyar M, Abdeen G, Jaradat I, Mohammad M,Yousef YA. Characteristics, management, and outcome of squamous carcinoma of the conjunctiva in a single tertiary cancer center in Jordan. Int J Ophthalmol 2018;11(7):1132-1138