Table 1 Baseline demographic data
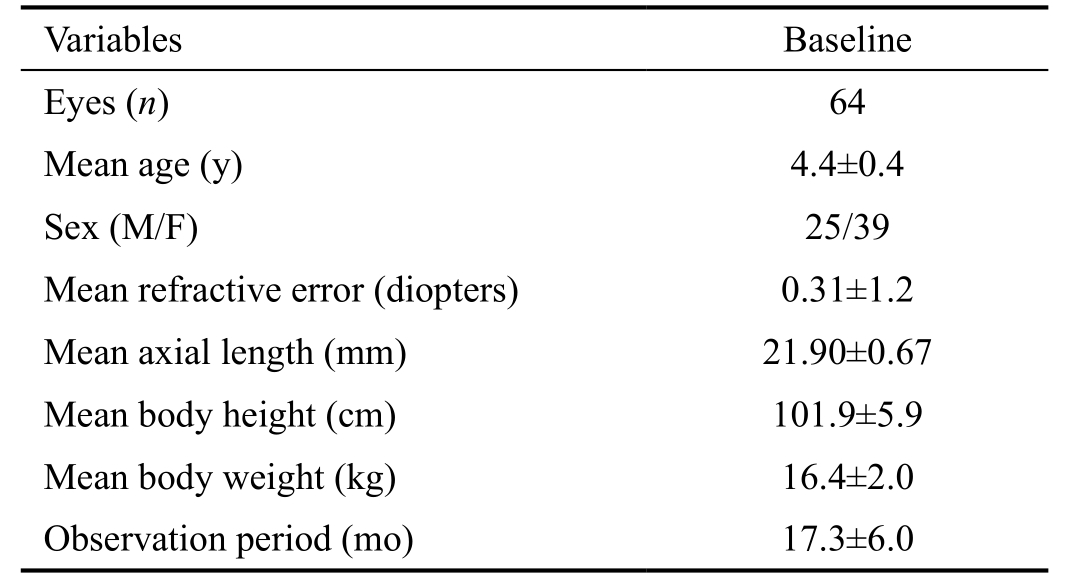
Data are presented as means±standard deviations.
Eiko Ohsugi1,2, Yoshinori Mitamura2, Kayo Shinomiya2, Masanori Niki2, Hiroki Sano2, Toshihiko Nagasawa1,2, Yukiko Shimizu1, Daisuke Nagasato1,2, Hitoshi Tabuchi1,2
1Department of Ophthalmology, Saneikai Tsukazaki Hospital,Himeji 671-1227, Japan
2Department of Ophthalmology, Institute of Biomedical Sciences, Tokushima University Graduate School, Tokushima 770-8503, Japan
Approximately 80%-90% of all blood to the eye for nourishment of outer layers of the retina, including photoreceptor cells, passes through the choroid. An understanding of the choroidal structure has rapidly advanced since Spaide et al[1]demonstrated that enhanced depth imaging optical coherence tomography (EDI-OCT) could obtain clear images of the choroid. The capabilities of OCT were further improved by swept-source OCT (SS-OCT), which uses a swept wavelength laser with a central wavelength of 1050 nm as the light source. This wavelength is longer than the 840-nm light source utilized by conventional spectral-domain OCT (SDOCT), which results in lower signal attenuation in tissues, thus enabling the acquisition of clearer images of the choroid[2-3].
Since the introduction of SS-OCT, increasing number of studies have examined choroidal thickness in normal and diseased eyes. The choroid in healthy individuals becomes thinner with increasing age[4-8]. We previously reported that the choroid was thicker in children than in adults[9], which was inconsistent with another study that failed to observe such a significant difference[10]. Furthermore, one study reported that the choroid in children thickened with increasing age[11].As these were cross-sectional comparative studies, individual differences such as age, rate of development, increasing myopia, and racial differences might account for these differences. To the best of our knowledge, no longitudinal studies to date have determined choroidal thickness in young children in Asia.
The purpose of this study was to determine whether choroidal thickness in healthy young Japanese children changed during a mean follow-up period of about 1.5y. We also determined the correlations between the ocular and systemic parameters and the choroidal thickness.
We reviewed the medical records of 64 eyes of 34 healthy children with a mean age of 4.4±0.4y (52.6±5.1mo), which ranged from 3.6 to 5.8y (43-69mo), who were examined at the Saneikai Tsukazaki and Tokushima University Hospitals as a part of group medical examinations for their preschool (Table 1).All children had SS-OCT evaluations at the baseline and follow-up period.
All procedures used in this study were approved by the institutional review boards of Saneikai Tsukazaki and Tokushima University Hospitals and conformed to the tenets of the Declaration of Helsinki. Informed consent was obtained from the legal guardians of all children after an explanation of the nature and possible complications of the study was provided.
All subjects underwent standard ophthalmologic examinations including measurements of the best-corrected visual acuity(BCVA), intraocular pressure by applanation tonometry,refractive error (spherical equivalent) by autorefractometry(ARK1; Nidek, Gamagori, Japan), and axial length by the IOL MasterTM(Carl Zeiss Meditec, Jena, Germany). The eyes were also examined by slit-lamp biomicroscopy and indirect ophthalmoscopy. All examinations were performed on the same day. The BCVA was measured with a standard Japanese Landolt visual acuity chart.
Children with a history of ophthalmologic surgery or ophthalmologic disease and those with systemic disease were excluded. Children with refractive errors greater than or equal to ±6 diopters (D) and those in whom clear OCT images could not be obtained owing to poor fixation were also excluded. As a result, 4 eyes of 4 subjects were excluded because of poor image quality due to poor fixation.
The same examinations and measurements were performed on these children at a mean follow-up period of 17.3±6.0mo(approximately 1.5y) with a range of 12 to 35mo. Changes in measurements between the baseline and the end of the followup period were determined. Changes in measurements were defined as the baseline values subtracted from the values at the final visit. Changes in choroidal thickness in nine Early Treatment Diabetic Retinopathy Study (ETDRS) sectors(i.e., the central sector, the inner and outer temporal, superior,inferior, and nasal sectors) were determined. In addition,systemic and ocular factors that were significantly correlated with the changes in choroidal thickness were determined.
Table 1 Baseline demographic data
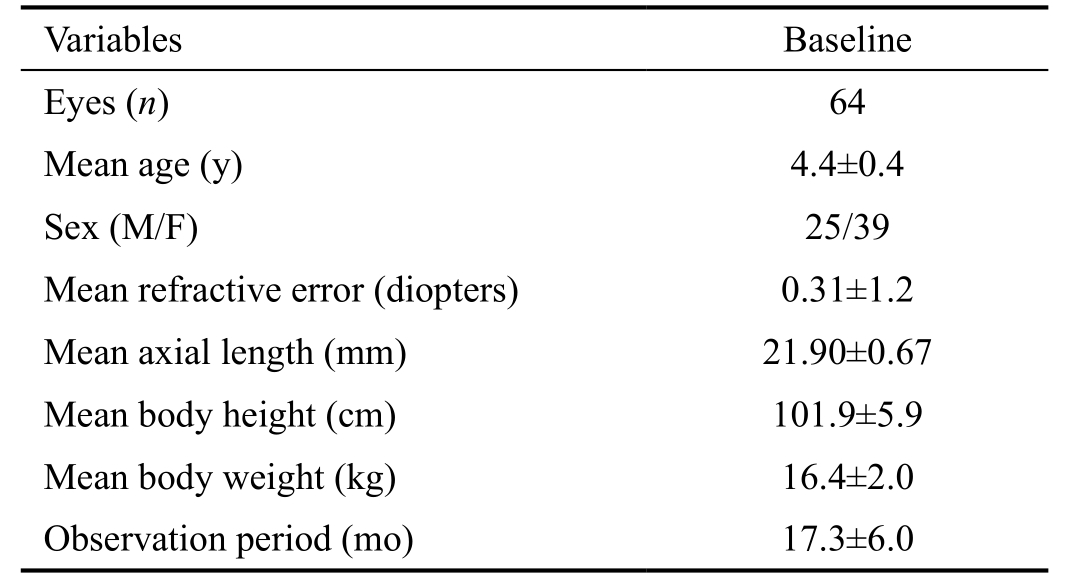
Data are presented as means±standard deviations.
Swept-source Optical Coherence TomographyMacular areas of the eyes were examined with an SS-OCT instrument(DRI OCT-1; Topcon, Tokyo, Japan). The light source of the SS-OCT system is a wavelength-tunable laser centered at 1050 nm, with an approximately 100-nm tuning range. After pupillary dilation with 1% cyclopentolate hydrochloride,evaluations with SS-OCT were performed by trained examiners. The 3D volumetric raster scan protocol was used,and each 3D scan covered an area of 6 mm×6 mm centered on the fovea with 512 A-scans ×256 B-scans. To improve image quality, we averaged four consecutive B-scan images of the same area. Advantage of infrared (IR) light source of SS-OCT is reduction of eye movements during the scans. Because of the high photographing speed of 100 000 A-scan/s, it took 1.31s to obtain a series of OCT images of 3D scan. All examinations were performed from 15:00 to 17:00 o’clock to reduce the effects of diurnal variations in choroidal thickness.
Choroidal ThicknessEach B-scan OCT image was obtained by averaging four consecutive B-scans, and 64 B-scan images were used to create a choroidal thickness map with an area of 6 mm×6 mm by semiautomatic segmentation. Each OCT image was examined by trained analyzers to ensure proper tracing of the chorioscleral border. In case of an error, manual segmentation was performed in a masked fashion (Figure 1).The embedded software measured the distance between the outer border of the retinal pigment epithelium and the surface of the chorioscleral border as the choroidal thickness. The ETDRS grid was used for choroidal thickness map, and mean values for regional thicknesses were calculated for each of the nine sectors of the ETDRS grid. The inner and outer rings,with diameters of 1-3 and 3-6 mm, respectively, were divided into superior, inferior, temporal, and nasal quadrants.

Figure 1 Swept-source optical coherence tomography Images showing the choroidal thickness maps of a healthy 4-year-old boy obtained at baseline (A, B) and after 12mo (C, D). The 3D raster scan protocol with 512 A-scans ×256 B-scans was used to obtain 3D imaging data of a 6 mm×6 mm area. Manual segmentation was performed only in cases where the built-in software delineated an erroneous chorioscleral border(A). A choroidal thickness map of an area 6 mm in diameter that was centered on the fovea was created by analyzing B-scan images of the 3D data set. The mean choroidal thickness map was obtained for each sector of the ETDRS grid map. A topographic map of choroidal thickness was automatically generated by the OCT software. Note that the choroidal thickness is thinner after the 12-month follow-up period (B, D).
Statistical AnalysisOcular parameters of both eyes as well as systemic parameters were used for statistical analyses.Generalized estimating equations (GEE) were used to revise the data for clustering and dependency. To examine whether the change in the thickness in each of the sectors was significant, the Bonferroni method for multiple comparisons was used on inter-group paired comparison for each of the change. In addition, univariate analysis was used to examine the effect of changes per year in body height, body weight, and axial length on the change per year in choroidal thickness. A stepwise multivariate analysis was used to extract factors that had significant independent effects. For all analyses, the link function was set as a linear model, and the model included subjects as a cluster variable. For the in fluence of the right and left eyes to be eliminated, they were used as within-subject variables. For this purpose, a working correlation matrix was specified as independent. All analyses were performed with the SPSS statistical software version 20.0 (SPSS Japan, Tokyo,Japan). P<0.05 was considered statistically significant for all analyses performed.
Comparison of Choroidal Thickness Between Baseline and After Follow-upThe choroidal thickness was analyzed for all subjects with good fixation and clear SS-OCT images.The body height, body weight, and axial length increased significantly during the follow-up period of 1.5y (all P<0.001). No significant differences were found in the refractive error and the body mass index between the baseline and the end of follow-up.
The choroidal thickness in the central sector was 301.8±8.6 µm at the baseline, which was reduced significantly to 286.6±8.0 µm at the end of the follow-up period (P<0.001; Table 2). The mean choroidal thicknesses of the inner ring and outer ring were also significantly thinner at the end of the follow-up period (P<0.001, P<0.005, respectively). Finally, the meanchoroidal thickness in all nine sectors of the ETDRS grid was significantly lower at the end of the follow-up period (all P<0.05; Table 2).
Table 2 Comparison of choroidal thickness between baseline and the end of the follow-up period
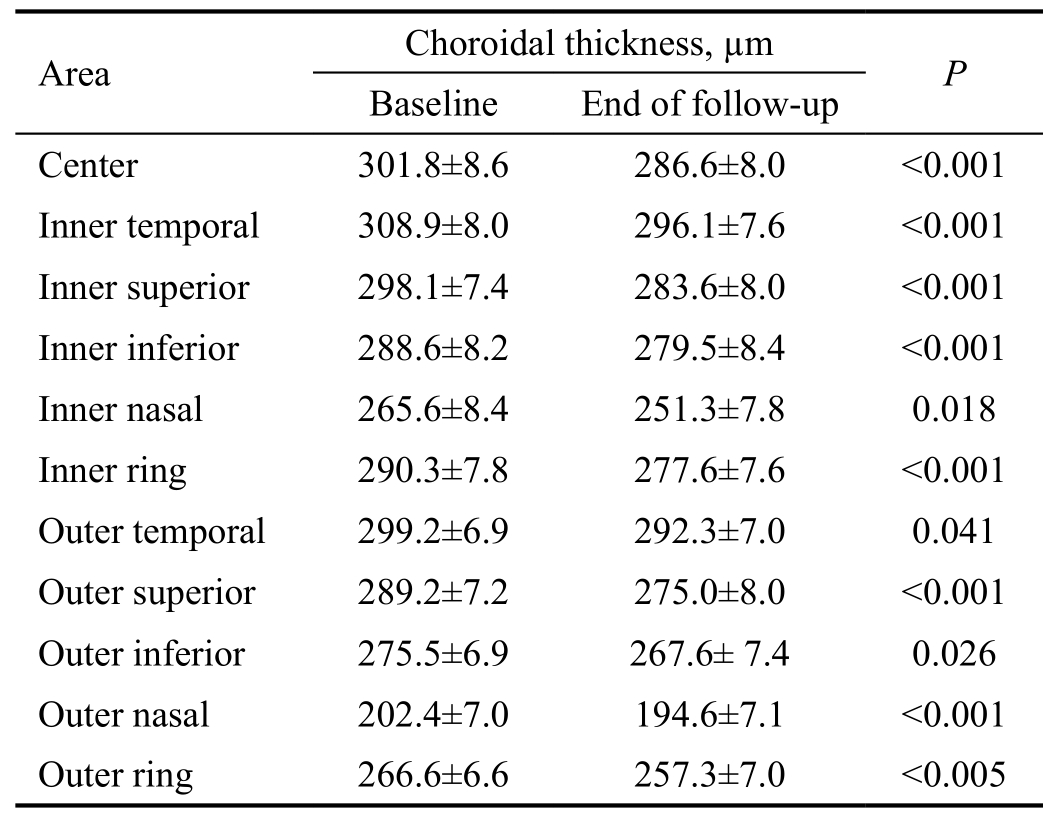
Data are presented as means±standard deviations.
Comparison of Choroidal Thinning in Central, Inner Ring,and Outer Ring SectorsThe choroidal thinning was largest in the central sector, followed by the inner and outer ring sectors. The extent of the thinning in the central and outer ring sectors was significant (P<0.05; Figure 2).
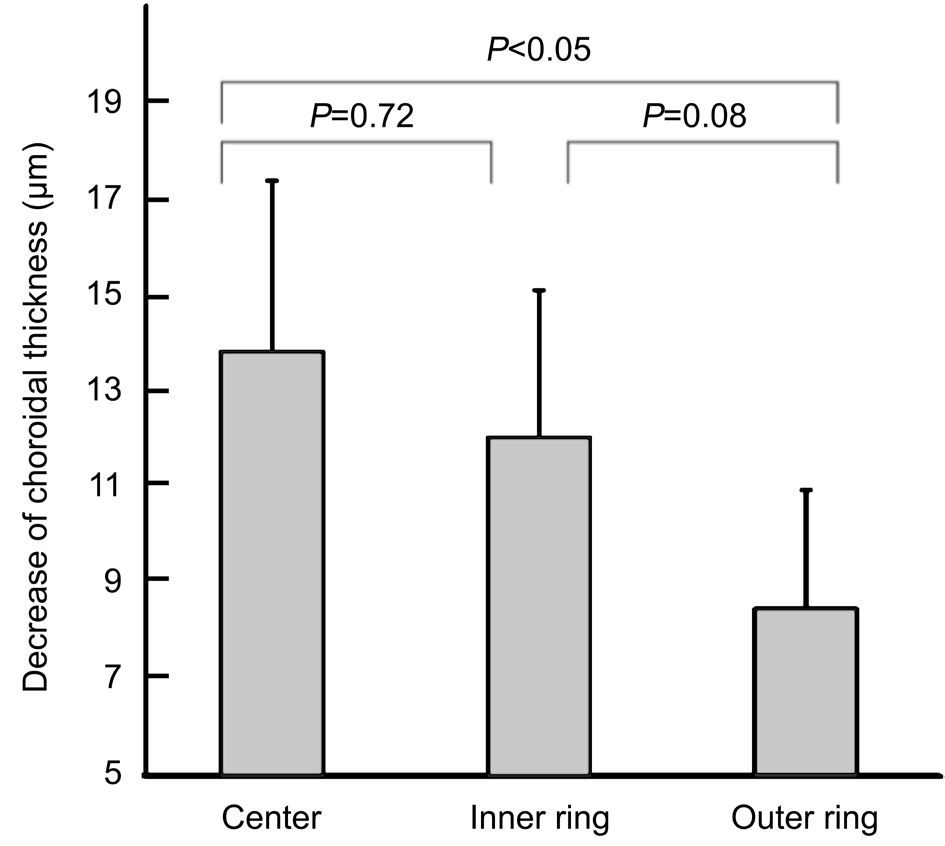
Figure 2 Changes in the choroidal thickness of the central, inner ring, and outer ring sectors in 64 eyes of 34 healthy children Decreases in choroidal thickness are largest in the central sector,followed by the inner and outer ring sectors. There is a significant difference in the decrease of the choroidal thickness between the central and outer ring sectors (P<0.05).
Correlations Between Changes of Choroidal Thickness and Systemic and Ocular ParametersThe correlations between the axial length, age, sex, body height, and body weight at the baseline and the change per year in choroidal thickness were examined by GEE. The baseline age, body height, and body weight were significantly and negatively correlated with the changes in choroidal thickness in the central, inner ring,and outer ring sectors (all P<0.05). In addition, the sex was significantly correlated with the change per year in choroidal thickness in the central and inner ring sectors (P<0.05), and the male children had the larger decrease in choroidal thickness.The stepwise multivariate analysis revealed that the change in choroidal thickness of the central sector was significantly correlated with the sex and body height (P<0.05 for both).
Significant correlations between the changes per year in body height, body weight, and axial length and the change per year in choroidal thickness were determined by GEE. Significant negative correlations were observed between the change per year in axial length and the change per year in choroidal thickness in the inner and outer ring sectors (P=0.007 and P<0.001, respectively). In addition, the correlation between the change per year in axial length and the change per year in choroidal thickness was examined with correction for baseline age, which revealed significant negative correlations in the central, inner ring, and outer ring sectors (P<0.05, P<0.01, and P<0.001, respectively; Table 3).
Earlier SD-OCT studies showed that the choroid was significantly thicker in eyes with central serous chorioretinopathy and Vogt-Koyanagi-Harada disease[12-14]and that the choroid was significantly thinner in eyes with pathologic myopia[15].Conversely, the choroidal thickness was reported to depend on the subtype in eyes with age-related macular degeneration[16].Thus, choroidal thickness can be an important parameter for evaluating ocular diseases, and determining the normal development of choroidal thickness is crucial in determining any deviations from its normal developmental course.
Table 3 Relationship between the changes of body height, body weight, and axial length per year and the change in choroidal thickness per year
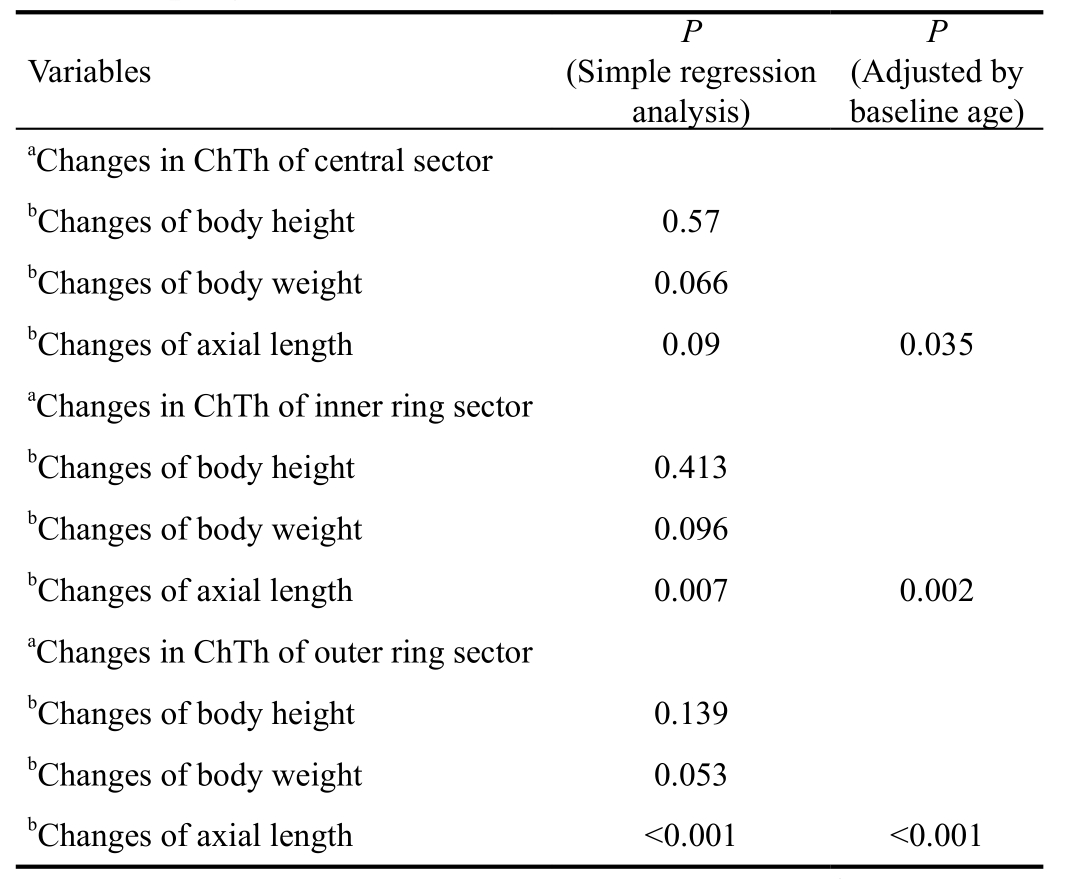
ChTh: Choroidal thickness.aDependent variables;bIndependent variables.
A cross-sectional study by Read et al[11]conducted in children between the ages of 3 and 12y (mean, 8.2y) showed that the choroidal thickness increased from early childhood to adolescence. Zhang et al[17]studied 972 children between the ages of 6 and 18y with a mean age of 11.3y and reported that a thicker subfoveal choroid was significantly associated with shorter axial length, male sex, and younger age in a multivariate analysis. Thus, cross-sectional studies of the chronological changes in choroidal thickness in children were inconsistent.
A longitudinal study by Read et al[18]in 2015 investigated the chronological changes in choroidal thickness in healthy children aged 10 to 15y by EDI-OCT. They reported that there was a significant increase in choroidal thickness over an 18-month period in these children. These findings appear to contradict our findings; however, their study cohort included children who were older than those in the current study.
In an earlier cross-sectional study of 3- to 15-year-old children(mean age, 7.9y), we reported that the choroid was thinner in older children in the central, inner ring, and outer ring sectors of the ETDRS grid[9]. In addition, we reported that the choroidal thinning was more rapid in the central area than in the inner and outer rings. In the current longitudinal study of children with a mean age of 4.5y, we found a significant decrease in the thickness in all nine sectors on the ETDRS grid after a 1.5-year follow-up period. The thinning of the choroid in the central area was significantly greater than that of the outer area. These findings lend further support to the findings of our previous cross-sectional study.
The longitudinal study by Read et al[18]reported a significant negative association between the changes in subfoveal choroidal thickness and the changes in axial lengths for all subjects. Their finding is consistent with our results demonstrating that there was a significant correlation between the change per year in choroidal thinning and the change per year in the axial elongation. However, Read et al[18]concluded that the pediatric choroidal thickness increased over time,which appeared to be contradictory to the age-associated increase in axial length. Moreover, Moreno et al[19]reported that the choroid was very thick in infancy, which raises the possibility that the choroid might become thinner with increasing age during childhood. Overall, our findings suggest that the choroid becomes thinner over time during childhood,in parallel with the increase in axial length.
One potential reason for the inconsistency between our findings and those of Read et al[18]is the difference in the ages of the subjects between the two studies; whereas Read et al[18]studied children between the ages of 10 and 15y, our study included younger children aged 3 to 5y. Another potential reason is the high prevalence of myopia in the Japanese population, although our cohort subjects were young with an average refractive error of 0.31±1.2 D, which did not change significantly at the follow-up examination. Read et al[18]reported that axial elongation could cause choroidal thinning,and the axial length did indeed increase significantly in our cohort. In fact, cross-sectional studies conducted on Asian populations reported the thinning of the choroid[9,17,20].
A study of adults with high myopia found that the choroid was significantly thinner in eyes with longer axial lengths[21].Fontaine et al[22]reported that the subfoveal choroidal thickness increased in nonmyopic patients and decreased in myopic patients over a 15-month period in children with ages ranging from 2 to 16y. Although myopia is known to progress during childhood, particularly during adolescence, the subjects in our study were younger, preschool-aged children with a mean refractive error of 0.32±1.21 D. Although the majority of the cohort subjects did not have myopia, a significant choroidal thinning was observed, which suggested that Japanese preschoolers might be at a potential risk of developing myopia and that choroidal thinning might be occurring at a relatively early stage of myopia.
We previously reported that the intraclass correlation coefficient was high between two observers during analysis of choroidal thickness using SS-OCT, indicating that measurement of choroidal thickness was highly reproducible with semiautomatic segmentation[1].
There are several limitations in our study. First, both the age range and the sample size were small, and the follow-up period varied among subjects. In addition, this study included only Japanese children, and a generalization of our results for all children is not appropriate. Thus, longitudinal studies with larger sample sizes and broader age ranges, and children from different ethnicities are necessary for an accurate evaluation of chronological changes in choroidal thickness.
In conclusion, the choroidal thickness among Japanese children with a mean age of 4.4y decreased over a mean period of 1.5y. These findings can be used as an important parameter to investigate the choroid in young children with ocular diseases.
Conflicts of Interest: Ohsugi E,None;Mitamura Y,None;Shinomiya K,None;Niki M,None;Sano H,None;Nagasawa T,None;Shimizu Y,None;Nagasato D,None;Tabuchi H,None.
REFERENCES
1 Spaide RF, Koizumi H, Pozzoni MC. Enhanced depth imaging spectraldomain optical coherence tomography.Am J Ophthalmol2008;146(4):496-500.
2 Potsaid B, Baumann B, Huang D, Barry S, Cable AE, Schuman JS,Duker JS, Fujimoto JG. Ultrahigh speed 1050nm swept source/Fourier domain OCT retinal and anterior segment imaging at 100,000 to 400,000 axial scans per second.Opt Express2010;18(19):20029-20048.
3 Puvanathasan P, Forbes P, Ren Z, Malchow D, Boyd S, Bizheva K. Highspeed, high-resolution Fourier-domain optical coherence tomography system for retinal imaging in the 1060 nm wavelength region.Opt Lett2008;33(21):2479-2481.
4 Ikuno Y, Kawaguchi K, Nouchi T, Yasuno Y. Choroidal thickness in healthy Japanese subjects.Invest Ophthalmol Vis Sci2010;51(4):2173-2176.
5 Hirata M, Tsujikawa A, Matsumoto A, Hangai M, Ooto S, Yamashiro K, Akiba M, Yoshimura N. Macular choroidal thickness and volume in normal subjects measured by swept-source optical coherence tomography.Invest Ophthalmol Vis Sci2011;52(8):4971-4978.
6 Ding X, Li J, Zeng J, Ma W, Liu R, Li T, Yu S, Tang S. Choroidal thickness in healthy Chinese subjects.Invest Ophthalmol Vis Sci2011;52(13):9555-9560.
7 Ouyang Y, Heussen FM, Mokwa N, Walsh AC, Durbin MK, Keane PA, Sanchez PJ, Ruiz-Garcia H, Sadda SR. Spatial distribution of posterior pole choroidal thickness by spectral domain optical coherence tomography.Invest Ophthalmol Vis Sci2011;52(9):7019-7026.
8 Manjunath V, Taha M, Fujimoto JG, Duker JS. Choroidal thickness in normal eyes measured using Cirrus HD optical coherence tomography.Am J Ophthalmol2010;150(3):325-329.
9 Nagasawa T, Mitamura Y, Katome T, Shinomiya K, Naito T, Nagasato D, Shimizu Y, Tabuchi H, Kiuchi Y. Macular choroidal thickness and volume in healthy pediatric individuals measured by swept-source optical coherence tomography.Invest Ophthalmol Vis Sci2013;54(10):7068-7074.
10 Ruiz-Medrano J, Flores-Moreno I, Peña-García P, Montero JA, Duker JS, Ruiz-Moreno JM. Macular choroidal thickness profile in a healthy population measured by swept-source optical coherence tomography.Invest Ophthalmol Vis Sci2014;55(6):3532-3542.
11 Read SA, Collins MJ, Vincent SJ, Alonso-Caneiro D. Choroidal thickness in childhood.Invest Ophthalmol Vis Sci2013;54(5):3586-3593.
12 Kuroda S, Ikuno Y, Yasuno Y, Nakai K, Usui S, Sawa M, Tsujikawa M, Gomi F, Nishida K. Choroidal thickness in central serous chorioretinopathy.Retina2013;33(2):302-308.
13 Hamzah F, Shinojima A, Mori R, Yuzawa M. Choroidal thickness measurement by enhanced depth imaging and swept-source optical coherence tomography in central serous chorioretinopathy.BMC Ophthalmol2014;14:145.
14 Maruko I, Iida T, Sugano Y, Oyamada H, Sekiryu T, Fujiwara T, Spaide RF. Subfoveal choroidal thickness after treatment of Vogt-Koyanagi-Harada disease.Retina2011;31(3):510-517.
15 Wang S, Wang Y, Gao X, Qian N, Zhuo Y. Choroidal thickness and high myopia: a cross-sectional study and meta-analysis.BMC Ophthalmol2015;15:70.
16 Jirarattanasopa P, Ooto S, Nakata I, Tsujikawa A, Yamashiro K, Oishi A, Yoshimura N. Choroidal thickness, vascular hyperpermeability, and complement factor H in age-related macular degeneration and polypoidal choroidal vasculopathy.Invest Ophthalmol Vis Sci2012;53(7):3663-3672.
17 Zhang JM, Wu JF, Chen JH, Wang L, Lu TL, Sun W, Hu YY, Jiang WJ, Guo DD, Wang XR, Bi HS, Jonas JB. Macular choroidal thickness in children: the shandong children eye study.Invest Ophthalmol Vis Sci2015;56(13):7646-7652.
18 Read SA, Alonso-Caneiro D, Vincent SJ, Collins MJ. Longitudinal changes in choroidal thickness and eye growth in childhood.Invest Ophthalmol Vis Sci2015;56(5):3103-3112.
19 Moreno TA, O’Connell RV, Chiu SJ, Farsiu S, Cabrera MT, Maldonado RS, Tran-Viet D, Freedman SF, Wallace DK, Toth CA. Choroid development and feasibility of choroidal imaging in the preterm and term infants utilizing SD-OCT.Invest Ophthalmol Vis Sci2013;54(6):4140-4147.
20 Lee JW, Song IS, Lee JH, Shin YU, Lim HW, Lee WJ, Lee BR.Macular choroidal thickness and volume measured by swept-source optical coherence tomography in healthy Korean children.Korean J Ophthalmol2016;30(1):32-39.
21 Flores-Moreno I, Ruiz-Medrano J, Duker JS, Ruiz-Moreno JM. The relationship between retinal and choroidal thickness and visual acuity in highly myopic eyes.Br J Ophthalmol2013;97(8):1010-1013.
22 Fontaine M, Gaucher D, Sauer A, Speeg-Schatz C. Choroidal thickness and ametropia in children: a longitudinal study.Eur J Ophthalmol2017:0.
Correspondence to:Yoshinori Mitamura. Department of Ophthalmology, Institute of Biomedical Sciences, Tokushima University Graduate School, 3-18-15 Kuramoto, Tokushima 770-8503, Japan. ymitaymitaymita@yahoo.co.jp
Received:2017-10-26 Accepted: 2018-02-05
Abstract ● AlM: To investigate the changes in the choroidal thickness in healthy pediatric children in a longitudinal study, and to determine the ocular and systemic parameters that were significantly correlated with the changes in the choroidal thickness.● METHODS: This study included 64 eyes of 34 healthy Japanese children with a mean age (±SD) of 4.4 (±0.4)y (range,3.6-5.8y) at baseline. Swept-source optical coherence tomography (SS-OCT) was used to record images of the retina and choroid at the baseline and after a mean followup period of about 1.5y. The 3D raster scan protocol was used to construct the choroidal thickness map. Mean choroidal thickness was calculated for each of the nine sectors of the Early Treatment Diabetic Retinopathy Study grid. Best-corrected visual acuity, axial length,body height, and weight were also measured. Changes in measurements were defined as the baseline values subtracted from the values at the final visit. A generalized estimating equation was used to eliminate the effect of within-subject intereye correlations.● RESULTS: The mean central choroidal thickness was significantly reduced during the follow-up period (baseline,301.8±8.6 µm; final visit, 286.6±8.0 µm, P<0.001). The decrease in the choroidal thickness was greatest in the central sector, followed by the sectors of the inner and outer rings. The inner and outer rings had diameters of 1 to 3 mm and 3 to 6 mm, respectively. The changes in the choroidal thickness in the central, inner ring, and outer ring sectors were significantly and negatively correlated with the age, baseline body height, baseline body weight,and elongation of the axial length.● CONCLUSlON: These results indicate that the choroidal thickness among preschool-aged Japanese children decreased significantly during the follow-up period. The choroidal thinning is significantly associated with the elongation of axial length. These characteristics should be considered in the evaluation of choroidal thickness in younger children with retinochoroidal disorders.
● KEYWORDS:choroidal thickness; longitudinal study;pediatrics; swept-source optical coherence tomography
DOl:10.18240/ijo.2018.07.17
Citation:Ohsugi E, Mitamura Y, Shinomiya K, Niki M, Sano H, Nagasawa T, Shimizu Y, Nagasato D, Tabuchi H. Changes in choroidal thickness in healthy pediatric individuals: a longitudinal study. Int J Ophthalmol 2018;11(7):1179-1184