Air tamponade in retinal detachment surgery followed by ultra-widefield fundus imaging system
Qian-Yin Chen1, Yun-Xia Tang1, Yan-Qiong He1, Hui-Min Lin1, Ru-Long Gao1, Meng-Yuan Li1,Jin-Tong Hou1, Hong-Jie Ma1,2, Jing-Lin Zhang1,2
1Guangzhou Aier Eye Hospital, Guangzhou 510010, Guangdong Province, China
2Aier School of Ophthalmology, Central South University,Changsha 410015, Hunan Province, China
INTRODUCTION
Rhegmatogenous retinal detachment (RRD) is commonly treated by scleral buckling, pars plana vitrectomy (PPV),pneumatic retinopexy or a combination techniques[1-2]. In the modern era, PPV has been a trend towards an important management of RRDs with identification of retinal breaks and removal of vitreous traction. Once the PPV is chosen,intraocular tamponade agents are used. Gases and silicone oils are the most commonly used types of tamponade agents[3-4].In China, perfluoropropane (C3F8) is the unique long-acting gas can be used for RRDs except when silicon oil is preferred.Since July 2015, the company has a full cessation production and sale C3F8. At present, there is no long-acting gas with China Food and Drug Administration certification in China,then silicone oil is used for RRDs management frequently.However, the use of silicone oil is associated with several common complications, including elevated intraocular pressure(IOP), cataract and corneal opacity. In addition, patients need to take reoperation with silicone oil removal. They will face anxiety of surgery and extra medical expense. Therefore,air would be another reasonable tamponade for treatment of RRDs.
Air filled in the vitreous cavity after the PPV is performed.The series of studies reported varies of results and the initial reattachment rate from 69.6% to 100%[5-11]. One of the main causes of retinal redetached was missed or new retinal breaks.
Intravitreal air would decrease the visibility of the retina due to strong reflections from the air bubble in the early postoperative period. Clinicians usually detect the missed or new retinal breaks until the air bubble getting smaller or disappeared.With the development of fundus photography, the Optos ultra-widefield imaging system makes retinal visualization and documenting in the gas-filled eyes[12-13]. It is useful in evaluating postoperative retinal breaks and retinal reattachment in gas- filled eyes[14-15].
The study was conducted to determine the efficiency of management of RRDs with PPV combined air tamponade and to detect the retinal break after PPV air tamponade by ultrawidefield fundus imaging. According to volume of air and the position of the bubble, the prone positioning may be briefest.
SUBJECTS AND METHODS
PatientsTwenty- five consecutive patients (25 eyes) with fresh primary RRD and causative retinal break were included from December 2016 to July 2017. The fresh RRD was considered as retinal detachment (RD) in 1mo without subretianl fibrosis and greater proliferative vitreoretinopathy (PVR). The retinal break was defined as a horseshoe tear and a hole on 8-4 o’clock presented. The exclusion criteria were: 1) RRDs with giant tears; 2) inferior breaks (5-7 o’clock); 3) retinal dialysis;4) acquired or secondary retinoschisis, pediatric RRDs; 5)PVR grade C or greater.
All patients were examined by slit-lamp biomicroscopy with a non-contact or contact wide angle lens to detect all retinal breaks preoperatively. The number, position (anterior,equatorial, and posterior to the equator), type (horseshoe tear or atrophic hole), size of retinal breaks and significant vitreous traction was determined. The study conducts followed the principles of the Declaration of Helsinki. Additionally, the study was conducted with approval from the Ethics Committee of Guangzhou Aier Eye Hospital.
Surgical ProcedureAll patients were operated on by a single surgeon (Zhang JL). The surgical method included a 23-gauge PPV performed with Accurus and Constellation Vision System (Alcon Laboratoties, Inc. Forth worth, TX,USA) and a noncontact wide viewing system (Volk Optical Inc., USA). After central and peripheral vitreous removal, all eyes underwent 360° scleral depression to shave vitreous base and removal of all vitreous traction on retinal tears. Fluid-air exchange was performed and vitreous fluid was aspirated with vitreous cutter. Perfluorodecalin would be used according to the position of the retinal breaks. Once the air bubble reached the area of the retinal breaks, subretinal fluid (SRF) under the retinal breaks were drained off by flute needle. At the end of the procedure, vitreous fluid and SRF was aspired with a flute needle to ensure complete air- fill of the cavity, and then laser retinopexy was performed. The sclerotomy was closed carefully to avoid air loss and the IOP was about 30 mm Hg at the end of the surgery. No complications developed during the surgical procedure.
Postoperative examinations were performed at 1, 3, 5, 7, 14d,and 1mo. Visual acuity (VA) was performed at 5, 7, 14d, and 1mo and last follow-up. Each patient was examined by slitlamp during the follow-up period. Air volume is estimated as a percentage of vertical diameter of eye seen through the dilated pupil with the plane of the cornea perpendicular to the ground[16]. Ultra-widefield scanning laser ophthamloscopic images (Daytona, Optos PLC, Scotland, UK) were captured from eyes in the primary and guided position at 1, 3, 5, 7,14d and last follow up. The investigation was detected the causative and treated retinal breaks, reattachments with intravitreal air and the volume of air bubble in the vitreous cavity. The identification of image was made by two specialists(Chen QY and He YQ). While the decision was not consisted,a third specialist (Tang YX) would detect and discuss to make the final decision
Statistical AnalysisA descriptive analysis has been carried out. All statistical procedures were performed with SPSS 21.0.
RESULTS
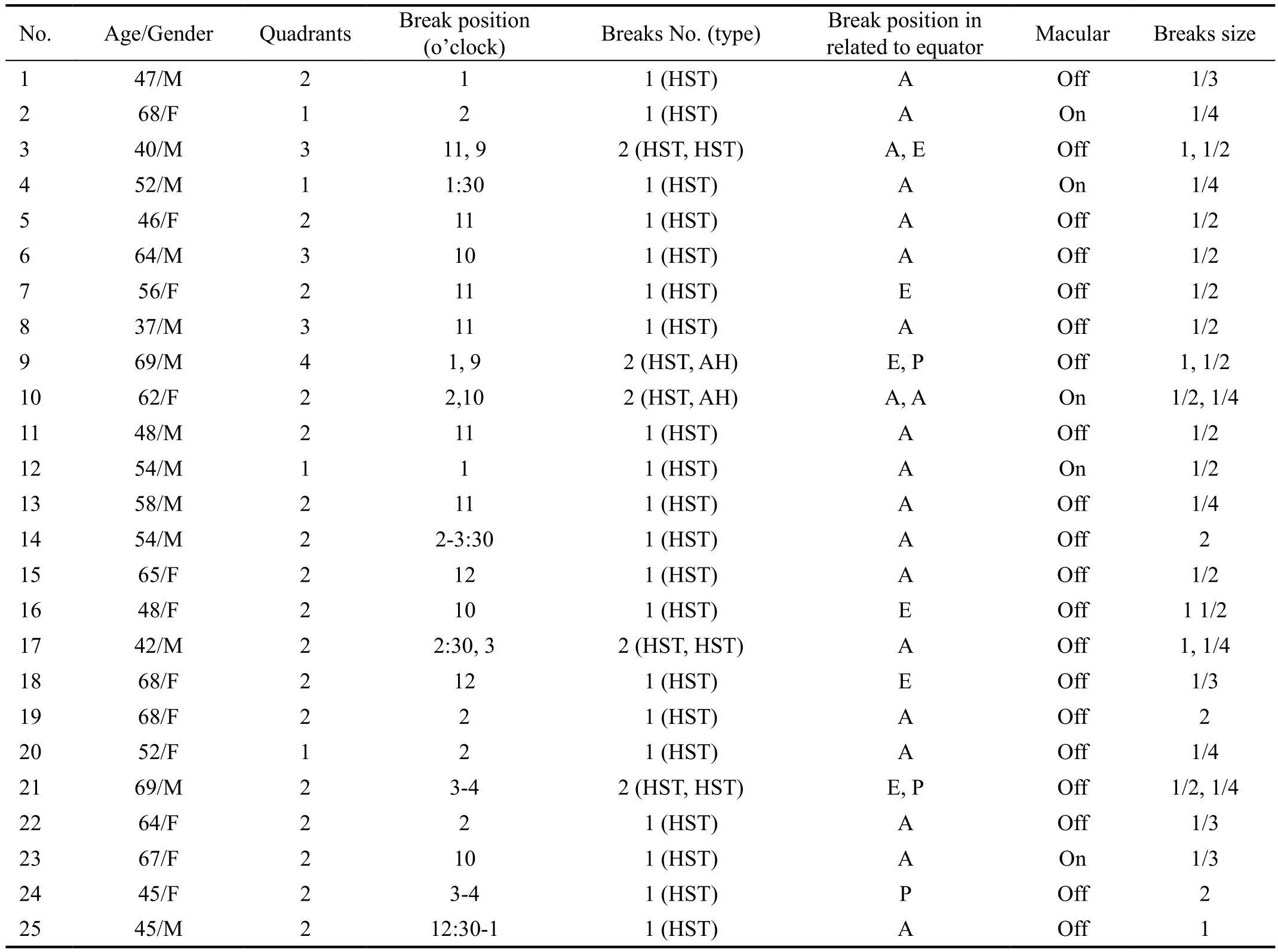
A total of 25 patients (25 eyes) suffered fresh RRDs with superior horsehole were included in this study. Thirteen patients were men (52%) and 12 were women (48%). Mean age was 55.52±10.28y (ranged from 37 to 69). Twenty-two phakic eyes (88%) and 3 pesudophakic eyes (12%) were presented. The mean number of quadrants affected was 2 (range, 1-4). All the retinal breaks were located between 8-4 o’clock. Twenty-two eyes (88%) had the macula detached preoperatively. All patients were underwent PPV combined with air tamponade. The preoperative clinical characteristics of patients were shown in Table 1.
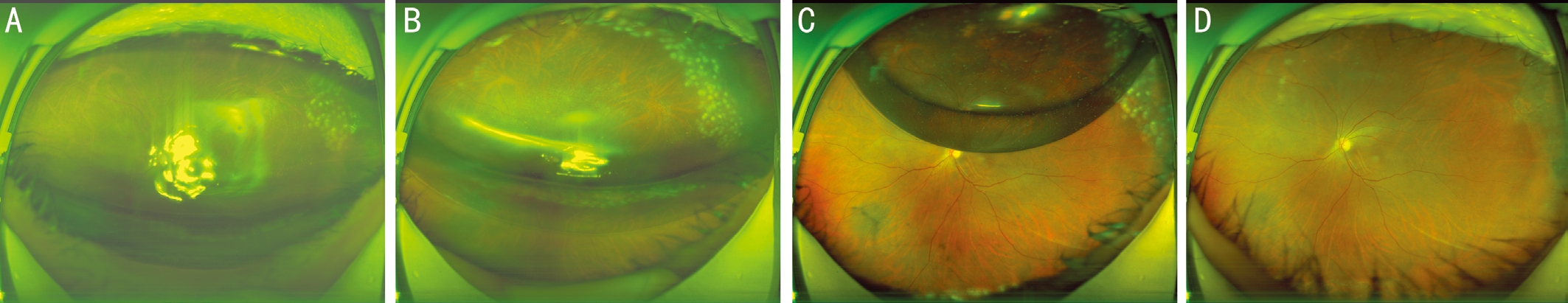
Initial reattachment was achieved in 25 cases. The mean follow-up was 6.8mo (range, 2-12mo). On the postoperative day (POD) 1, the air volume was >60%. The ultra-widefield images were acquired with regardless of the volume of air in vitreous cavity. They showed that the retina was reattached in all air- filled eyes postoperatively. The retinal break and laser burns in the superior were detected in 22 of 25 eyes (88%)under the air on POD 1. On the POD 3, the air volume was range from 40% to 60%. The ultra-widefield images showed that the retina was reattached in all air- filled eyes. A doublelayered image was seen in 25 of 25 eyes with intravitreal gas. Retinal breaks and laser burns around were seen in the intravitreal air, but only a missed retinal hole was found under intravitreal air bubble in 1 case (case 10). On the POD 5, the air volume was ≤30%. Air-bubble was seen in the superior area on the ultra-widefield images. On the POD 7, small bubble without effect was seen in 6 cases (24%) and bubble was completely disappeared in 4 cases (16%). Oval bubble in the superior area was observed in 15 cases (60%). Air disappeared completely on a mean of 9.84d postoperatively. On the POD 14 and 1mo follow-up, the air bubble was absorbed in all cases. Retinal attachment rate was 100%. The retinal breaks and choroaretinal scar were seen from the images (Figure 1).Final postoperative best-corrected visual acuity (BCVA) are range from 0.9 logMAR to 0.1 logMAR (mean 0.35 logMAR).Mean final postoperative BCVA improved significantly relative to mean preoperative (P<0.05). VA improved range 3-5d in macular-off cases. Final VA of 0.3 logMAR or better was seen in 13 eyes. No serious complications occurred during the surgery. Preoperative cataract of 2 cases was no aggravation.Lens feathering was found in 3 cases and disappeared on the 5thday after the operation.
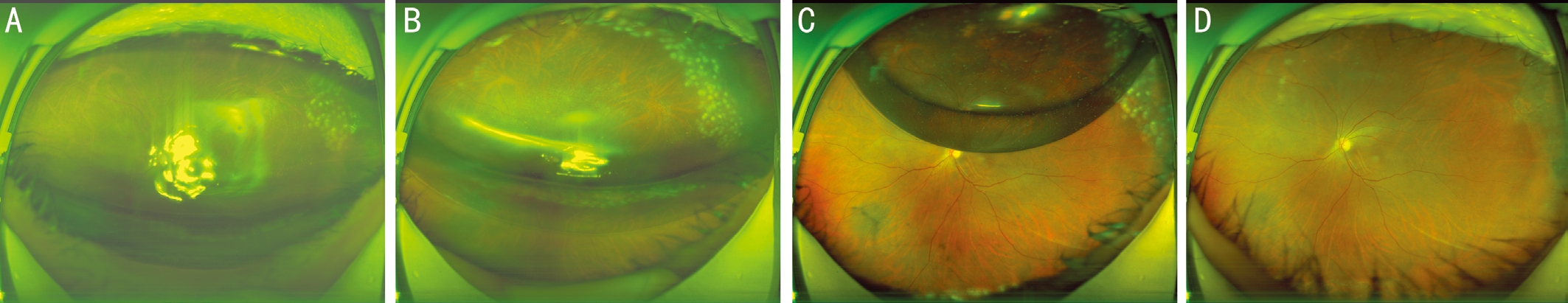
Figure 1 A 52-year-old female patient who diagnosed fresh RRD with a retinal break on 3-4 o’clock underwent PPV with air tamponade.The ultra-widefield colour fundus photographs of the left eye were shown A: On POD 1, the intravitreal air volume was about 75%. The image showed the retina was attached and retinal break in the temporal through the air bubble with the strong reflection. The eyelid was usually swelling due to the prone position on the early stage after the surgery so that the superior laser burns were invisible. B: On POD 3, the image showed the a double-layered of the bubble. The banana-shape was block the middle of the retina. It just showed a mirror image. C: On POD 5,the air bubble was getting smaller. The retina was attached and the laser burns around the retinal break were clear. D: On final follow-up, the air bubble was completely disappeared. The image showed the retina was attached and the laser scar around the retinal break.
Table 1 Characteristics of patient with primary RRD
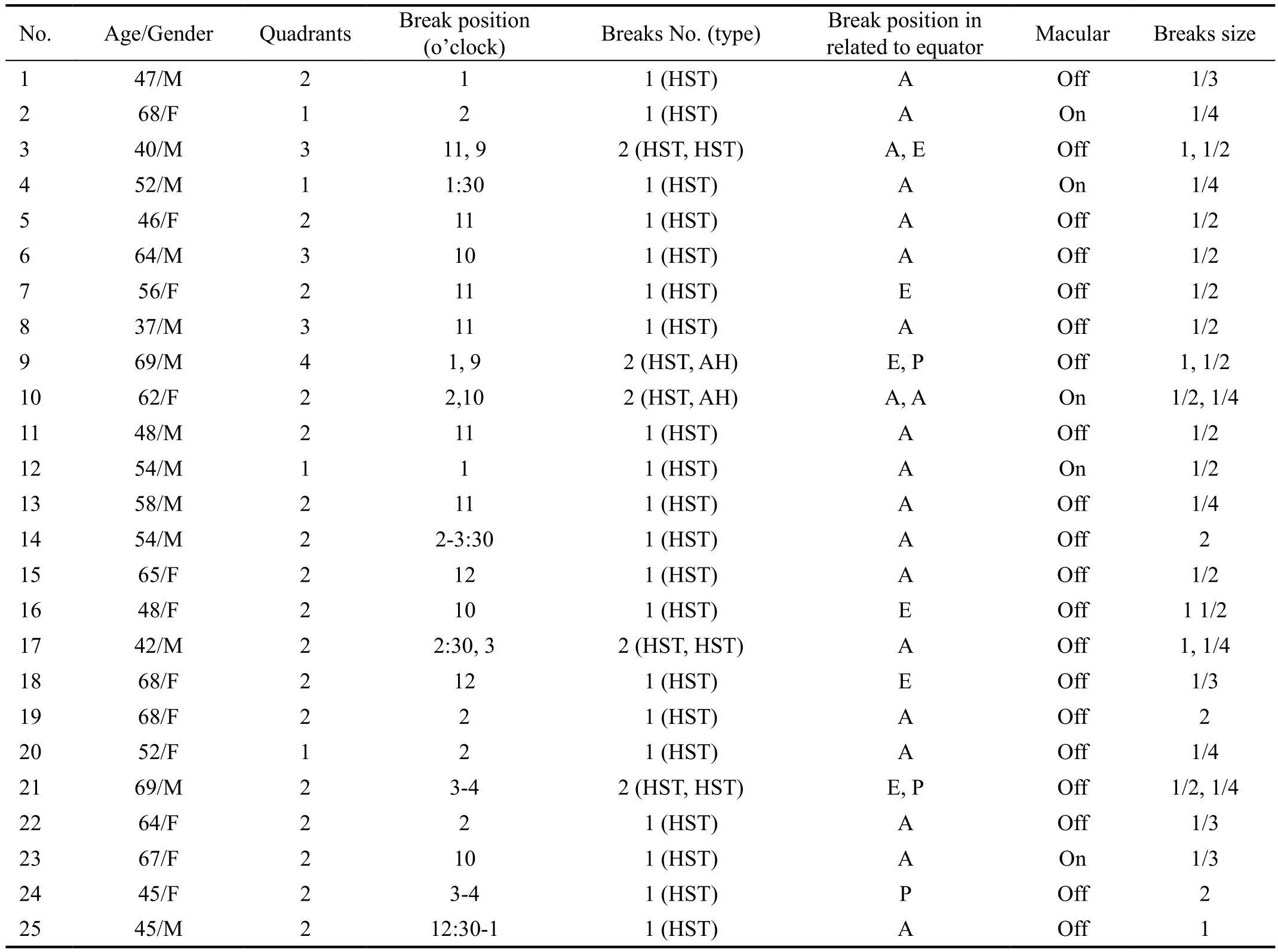
HST: Horseshoe tear; AH: Atrophic hole; A: Anterior; E: Equatorial; P: Posterior.
(o’clock) Breaks No. (type) Break position in related to equator Macular Breaks size 1 47/M 2 1 1 (HST) A Off 1/3 2 68/F 1 2 1 (HST) A On 1/4 3 40/M 3 11, 9 2 (HST, HST) A, E Off 1, 1/2 4 52/M 1 1:30 1 (HST) A On 1/4 5 46/F 2 11 1 (HST) A Off 1/2 6 64/M 3 10 1 (HST) A Off 1/2 7 56/F 2 11 1 (HST) E Off 1/2 8 37/M 3 11 1 (HST) A Off 1/2 9 69/M 4 1, 9 2 (HST, AH) E, P Off 1, 1/2 10 62/F 2 2,10 2 (HST, AH) A, A On 1/2, 1/4 11 48/M 2 11 1 (HST) A Off 1/2 12 54/M 1 1 1 (HST) A On 1/2 13 58/M 2 11 1 (HST) A Off 1/4 14 54/M 2 2-3:30 1 (HST) A Off 2 15 65/F 2 12 1 (HST) A Off 1/2 16 48/F 2 10 1 (HST) E Off 1 1/2 17 42/M 2 2:30, 3 2 (HST, HST) A Off 1, 1/4 18 68/F 2 12 1 (HST) E Off 1/3 19 68/F 2 2 1 (HST) A Off 2 20 52/F 1 2 1 (HST) A Off 1/4 21 69/M 2 3-4 2 (HST, HST) E, P Off 1/2, 1/4 22 64/F 2 2 1 (HST) A Off 1/3 23 67/F 2 10 1 (HST) A On 1/3 24 45/F 2 3-4 1 (HST) P Off 2 25 45/M 2 12:30-1 1 (HST) A Off 1 No. Age/Gender Quadrants Break position
DISCUSSION
PPV has become the more popular surgical procedure for the repair of RRD. Air tamponade is recommended agent after PPV for selected RRD. Several studies have reported satisfactory results with air tamponade[5,7-11,17]. Tan et al[10]found that there were no significant differences overall in the success rates between air and 20% sulfur hexafluoride (SF6) tamponade.But the author suggested that air tamponade should only be used in superior RDs. In contrast, Zhou et al[11]conducted a prospective, randomized, comparative study including 64 eyes with RDs and they reported that air had equivalent tamponade effects to C3F8in the surgical management of inferior RDs.
In our study, retinal breaks on 8-4 o’clock with vitreous traction RDs were selected. PPV and fluid-air exchange are performed in our all cases. According to the physical properties and dynamics of intraocular tamponade, air is nonexpansile and persists in the vitreous cavity for 5 to 7d[18]. Compared longacting gas tamponade, facedown position period and visual rehabilitation could be shorten. Our primary reattachment rate is 100% with favorable results. Vitreoretinal surgical expertise during the surgery is importance. First, the key to the surgery is to remove the vitreous around the retinal break completely and extent of peripheral vitrectomy. Peripheral retinal break and vitreous shaving as completely as possible was performed by wide-angle viewing system with rotation eyeball passively and 360° scleral depression. Second, SRF was drained off completely, which was the key to retinopexy with endolaser photocoagulation. Furthermore, usage of wide-angle viewing system can discover the retinal break in peripheral and SRF was drained with a flute needle in direct visualization. It may reduce the usage of perfluorodecalin, then retinopexy with endolaser photocoagulation during fluid-air exchange. Thus,it would simplify the surgical procedure and speed up the process. In addition, the authors suggest photocoagulation is superior to cryopexy. Theoretically, the enhance adhesion between neurosensory retina and retinal pigment epithelium(RPE) will occur within 24h after laser photocoagulation.Nevertheless the adhesion after the croyexy in the same situation will occur at least 1wk[19-20].
Previous studies indicated that one of the risk factors of redetachment were new or missed retinal breaks[11,21-22]. In the gas- filled eye after the retinal surgery with PPV, the reflection of the light becomes scattered. Non-contact lens (90 D) or three-mirror contact lens can assist the surgeons to find out the retinal breaks. But it’s difficult to recongnize because of the air-bubble scatter and unable to document. Traditional fundus camera can obtain the images of posterior retina in some cases. But the retinal breaks are typically in periphery.Though the instrument cooperation and patient moves their eyes during the photography and several photos are taken for creating a montage, 96° of retina will be covered. Traditional fundus camera just capture portions of peripheral retina and the images are not clear[23]. Recently advancements in widefield photography have dramatically improved the ability to image the peripheral retina. Optos ultra-widefield image system(Daytona, Optos PLC, Scotland, UK) is based on confocal scanning laser ophthalmoscopy. The Optos utilizes green laser with 532 nm wavelength and red laser with 633 nm wavelength as light source respectively, with an optical elliptical mirror to create images of the extending to peripheral retina. So the device provides a 200° view of the retina and capture 82% of the retina in a single image without mydriasis. Due to the Optos can penetrate to the retina layer and the choroid layer, it is less affected by scattering reflected light, the final formation of highresolution retinal images. It allows surgeons to evaluate the retina far beyond the equator of the fundus[12,24].
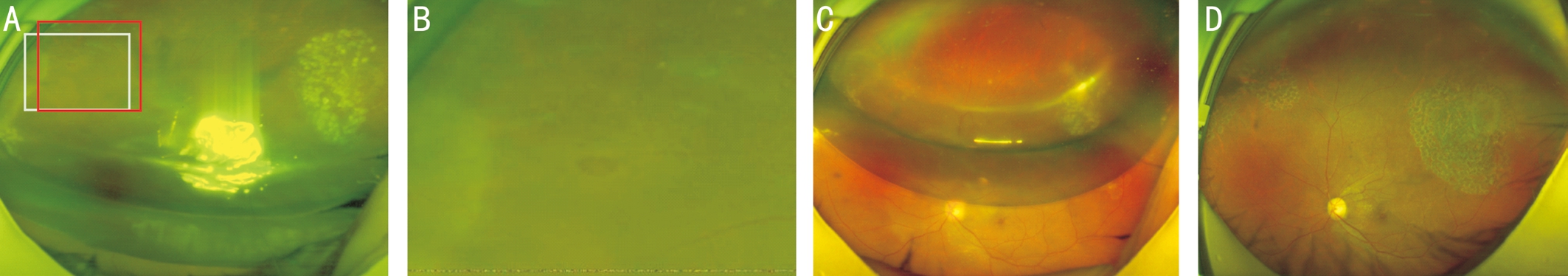
In our study, ultra-widefield image system was a useful facility for monitoring retinal breaks after PPV with air tamponade.On POD 1, the air volume was >60%. It’s difficult to detect information from the ultra-widefield images in 4 cases. One case was not recognizable due to peripheral break on 12 o’clock which was blocked by cortical cataract preoperatively(case 15). Three cases were difficult to recognize due to feather-like subcapsular lens opacity enhance scattering of light of the air bubble. The typically subcapsular feathering may cause by oxidative stress to the lens. It may be reversible by diligent prone positioning. On POD 1, patients were required to remain facedown position. On POD 3, the air bubbles become smaller gradually. The images showed that the bubble was divided into two components with oval area in the superior and banana-shaped area in the inferior[14]. The retinal breaks and laser burns were detected through the ovalshaped air bubble in superior area. The banana-shaped was a mirror image of inferior retina, especially peripheral retina. It is caused by light reflection from gas-liquid interface (Figure 2).Inoue et al[14]reviewed ultra-widefield fundus images in 40 eyes of 40 patients who had undergone vitrectomy with gas tamponade for RD. In the primary position, the rate of detecting tears in the superior area in eyes with gas volume of ≥60% was significantly higher than gas volume <60%.They can detect the superior retinal breaks from the images which capture under the gas-bubble when the gas volume≥60%. It’s the similar result in our study. With the bananashaped appearing, light reflection from gas-liquid interface would disturb the estimating retinal breaks in banana-shaped area. Nakao et al[25]analyzed Optos high-quality fundus autofluorescence (FAF) images of 18 eyes with unilateral macular holes (MHs), who underwent vitrectomy with SF6tamponade. On POD 2, 6 of 18 eyes (33.3%) could not obtain a clear FAF image could due to the gas-liquid interface being in the MH area. Changing the orientation of the patient’s face or the eye fixation may improve the Optos image quality. It help surgeons detect more retinal breaks and decide the release of the patient from facedown posturing. Patients could take a seat position or side-lying position replaced of facedown position. Positioning would be changed depend on the retinal breaks and air volume in patients’ follow-up.

Figure 2 Three days postoperative ultra-widefield images of a 68-year-old female patient A: The colour fundus image of the left eye shows attached retina with double-layer bubble: oval-shape superiorly and banana-shape inferiorly. The laser burns seen in the banana-shape area are mirror image of peripheral retina what are not visible inferiorly. B: Green laser image of the patient from panel A, which showed retinal vessels and the laser burns were seen clearly even under the air bubble. C: Red laser image of the patient from panel A, which showed the mirror image of vortex vein due to the light reflection (white arrow). The vortex vein and choroid vein are in inferior area beyond the equatorial (red arrow).
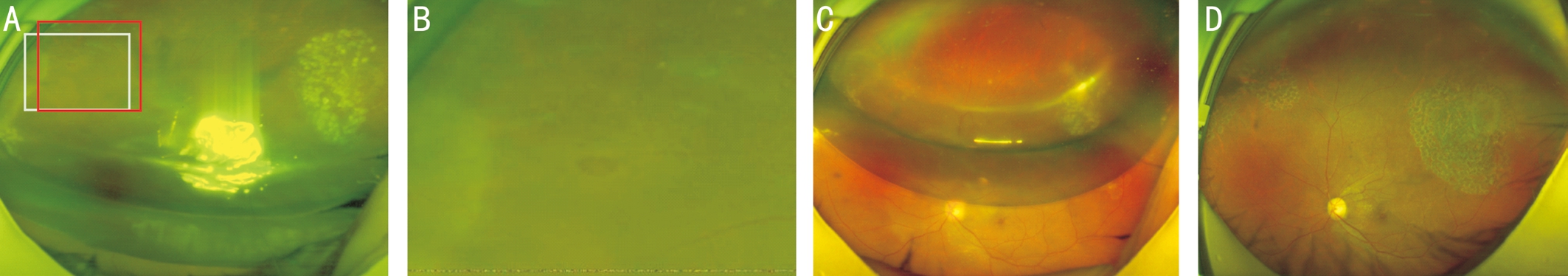
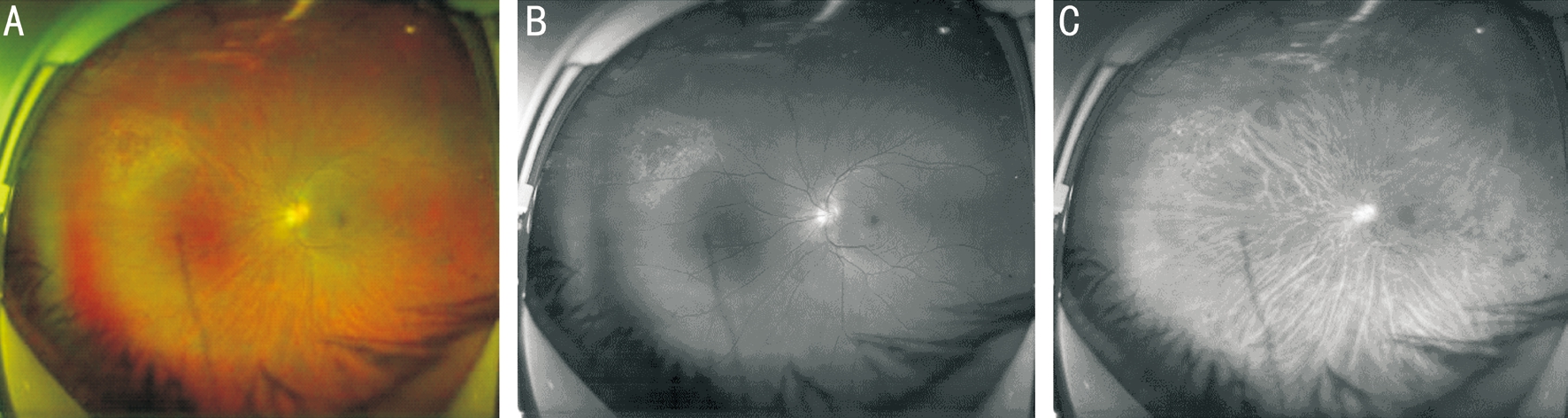
Figure 3 A 54-year-old male patient who diagnosed fresh RRD with a retinal break on 1-2 o’clock underwent PPV with air tamponade.The ultra-widefield colour fundus photographs of the left eye were shown A: One-day postoperative colour fundus image shows attached retina and laser burns on 1-2 o’clock. But a missed retinal hole was also detected on the nasal retina in superior area (white box). B: Magnified fundus image (A) shows the missed retinal hole under the air. C: Three-day postoperative colour fundus image shows laser burns around the missed retinal hole (red box). D: Final follow-up image shows the retina is attached and the laser scar around the retinal breaks.
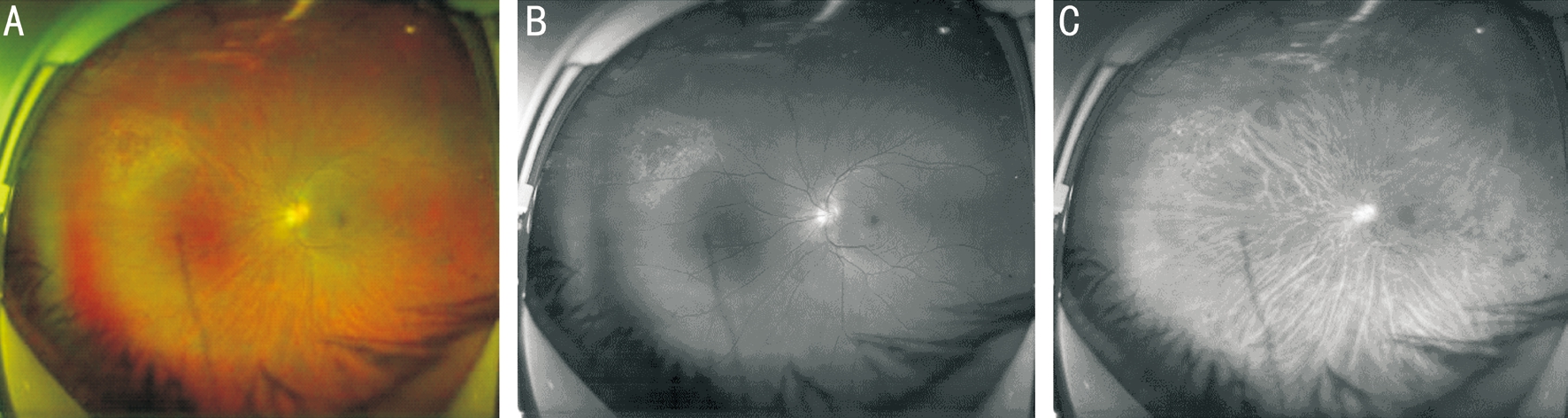
Figure 4 A 48-year-old female patient underwent PPV with air tamponade on 14d postoperatively A: The ultra-widefield colour photograph shows retina attachment and laser scar with pigmentation around the retinal break on 10 o’clock; B: The green laser photograph shows the retinal break and laser scar clearly in the retina layer; C: The red laser photograph shows cloudy laser scar in the RPE layer, and the retinal break was not detected.
In case 10, a missed retinal hole was detected on ultrawidefield image on the POD 1, at the meanwhile intravitreal air was approximately 50%. The air bubble presses against the hole effectively and no RD. Because of the reflected air bubble, laser can’t focus the retinal break on the first day. We performed the retinal photocoagulation treatment and followup closely was necessary (Figure 3).
On the POD 14 and 1mo, Optos ultra-widefield images were documented. There were no missed and new retinal breaks and no RD in all cases. The images showed the retinal breaks and choroaretinal scar around the treated breaks. Separating into two wavelength laser scans provide further information. The green laser can describe better images of the retinal break and laser burns. The red laser can penetrate into the deeper layers of the retina and the choroid. The images showed the choroidal vessels and vortex vein (Figure 4).
In conclusion, we report that PPV with air tamponade is an effective management for fresh RRD with superior retinal breaks. The ultra-widefield fundus imaging system is a useful tool in following up after the retinal surgery. It can detect postoperative retinal breaks, especially the new or missed hole in air- filled eyes. Patients may be allowed to facedown position and acquired visual rehabilitation in shorter time.
There were strict indications in our cases selection. Firstly,fresh RRD with severe synchysis or vitreous traction induced horse hole. Secondly, superior break at 8 to 4 o’clock were selected. RRDs with the above condition can be effectively managed by PPV combined with air tamponade. But our study has limitations. We need more cases and long-term observation.
ACKNOWLEDGEMENTS
Conflicts of Interest: Chen QY,None;Tang YX,None;He YQ,None;Lin HM,None;Gao RL,None;Li MY,None;Hou JT,None;Ma HJ,None;Zhang JL,None.
REFERENCES
1 Hwang JC. Regional practice patterns for retinal detachment repair in the United States.Am J Ophthalmol2012;153(6):1125-1128.
2 Nemet A, Moshiri A, Yiu G, Loewenstein A, Moisseiev E. A review of innovations in rhegmatogenous retinal detachment surgical techniques.J Ophthalmol2017;2017:4310643.
3 Rizzo S, Barca F. Vitreous substitute and tamponade substances for microincision vitreoretinal surgery.Dev Ophthalmol2014;54:92-101.
4 Janco L, Vida R, Bartos M, Villemova K, Izak M. Gases in vitreoretinal surgery.Cesk Slov Oftalmol2012;68(1):3-8,10.
5 Escoffery RF, Olk RJ, Grand MG, Boniuk I. Vitrectomy without scleral buckling for primary rhegmatogenous retinal detachment.Am J Ophthalmol1985;99(3):275-281.
6 van Effenterre G, Haut J, Larricart P, Abi-Rached J, Vachet JM. Gas tamponade as a single technique in the treatment of retinal detachment: is vitrectomy needed? A comparative study of 120 cases.Graefes Arch Clin Exp Ophthalmol1987;225(4):254-258.
7 Heimann H, Bornfeld N, Friedrichs W, Heibig H, Kellner U, Korra A, Foerster MH. Primary vitrectomy without scleral buckling for rhegmatogenous retinal detachment.Graefes Arch Clin Exp Ophthalmol1996;234(9):561-568.
8 Hotta K, Sugitani A, Uchino Y. Pars plana vitrectomy without longacting gas tamponade for primary rhegmatogenous retinal detachment.Ophthalmologica2004;218(4):270-273.
9 Martinez-Castillo V, Verdugo A, Boixadera A, Garcia-Arumi J,Corcostegui B. Management of inferior breaks in pseudophakic rhegmatogenous retinal detachment with pars plana vitrectomy and air.Arch Ophthalmol2005;123(8):1078-1081.
10 Tan HS, Oberstein SY, Mura M, Bijl HM. Air versus gas tamponade in retinal detachment surgery.Br J Ophthalmol2013;97(1):80-82.
11 Zhou C, Qiu Q, Zheng Z. Air versus gas tamponade in rhegmatogenous retinal detachment with inferior breaks after 23-gauge pars plana vitrectomy: a prospective, randomized comparative interventional study.Retina2015;35(5):886-891.
12 Mackenzie PJ, Russell M, Ma PE, Isbister CM, Maberley DA.Sensitivity and specificity of the Optos optomap for detecting peripheral retinal lesions.Retina2007;27(8):1119-1124.
13 Kernt M, Schaller UC, Stumpf C, Ulbig MW, Kampik A, Neubauer AS. Choroidal pigmented lesions imaged by ultra-wide-field scanning laser ophthalmoscopy with two laser wavelengths (Optomap).Clin Ophthalmol2010;4:829-836.
14 Inoue M, Koto T, Hirota K, Hirakata A. Ultra-widefield fundus imaging in gas- filled eyes after vitrectomy.BMC Ophthalmol2017;17(1):114.
15 Witmer MT, Cho M, Favarone G, Chan RV, D'Amico DJ, Kiss S. Ultrawide-field autofluorescence imaging in non-traumatic rhegmatogenous retinal detachment.Eye (Lond)2012;26(9):1209-1216.
16 Wong RF, Thompson JT. Prediction of the kinetics of disappearance of sulfur hexafluoride and perfluoropropane intraocular gas bubbles.Ophthalmology1988;95(5):609-613.
17 Pak KY, Lee SJ, Kwon HJ, Park SW, Byon IS, Lee JE. Exclusive use of air as gas tamponade in rhegmatogenous retinal detachment.J Ophthalmol2017;2017:1341948.
18 Vaziri K, Schwartz SG, Kishor KS, Flynn HW Jr. Tamponade in the surgical management of retinal detachment.Clin Ophthalmol2016;10:471-476.
19 Folk JC, Sneed SR, Folberg R, Coonan P, Pulido JS. Early retinal adhesion from laser photocoagulation.Ophthalmology1989;96(10):1523-1525.
20 Yoon YH, Marmor MF. Rapid enhancement of retinal adhesion by laser photocoagulation.Ophthalmology1988;95(10):1385-1388.
21 Mudvari SS, Ravage ZB, Rezaei KA. Retinal detachment after primary pneumatic retinopexy.Retina2009;29(10):1474-1478.
22 Martinez-Castillo VJ, Garcia-Arumi J, Boixadera A. Pars plana vitrectomy alone for the management of pseudophakic rhegmatogenous retinal detachment with only inferior breaks.Ophthalmology2016;123(7):1563-1569.
23 Witmer MT, Kiss S. Wide- field imaging of the retina.Surv Ophthalmol2013;58(2):143-154.
24 Shoughy SS, Arevalo JF, Kozak I. Update on wide-and ultra-widefield retinal imaging.Indian J Ophthalmol2015;63(7):575-581.
25 Nakao S, Arita R, Sato Y, Enaida H, Ueno A, Matsui T, Salehi-Had H, Ishibashi T, Sonoda KH. Wide-field laser ophthalmoscopy for imaging of gas-filled eyes after macular hole surgery.Clin Ophthalmol2016;10:1623-1630.
Correspondence to:Jing-Lin Zhang. Guangzhou Aier Eye Hospital, Guangzhou 510010, Guangdong Province, China.zhjinglin@126.com
Received:2018-02-09 Accepted: 2018-04-25
Abstract ● AlM: To report the surgical result of pars plana vitrectomy(PPV) with air tamponade for rhegmatogenous retinal detachment (RRD) by ultra-widefield fundus imaging system.● METHODS: Of 25 consecutive patients (25 eyes) with fresh primary RRD and causative retinal break and vitreous traction were presented. All the patients underwent PPV with air tamponade. Visual acuity (VA) was examined postoperatively and images were captured by ultrawidefield scanning laser ophthalmoscope system (Optos).● RESULTS: lnitial reattachment was achieved in 25 cases(100%). The air volume was >60% on the postoperative day (POD) 1. The ultra-widefield images showed that the retina was reattached in all air- filled eyes postoperatively.The retinal break and laser burns in the superior were detected in 22 of 25 eyes (88%). A missed retinal hole was found under intravitreal air bubble in 1 case (4%). The air volume was range from 40% to 60% on POD 3. A doublelayered image was seen in 25 of 25 eyes with intravitreal gas. Retinal breaks and laser burns around were seen in the intravitreal air. On POD 7, small bubble without effect was seen in 6 cases (24%) and bubble was completely disappeared in 4 cases (16%). Small oval bubble in the superior area was observed in 15 cases (60%). There were no missed and new retinal breaks and no retinal detachment in all cases on the POD 14 and 1mo and last follow-up. Air disappeared completely on a mean of 9.84d postoperatively. The mean final postoperative bestcorrected visual acuity (BCVA) was 0.35 logMAR. Mean final postoperative BCVA improved significantly relative to mean preoperative (P<0.05). Final VA of 0.3 logMAR or better was seen in 13 eyes.● CONCLUSlON: PPV with air tamponade is an effective management for fresh RRD with superior retinal breaks. The ultra-widefield fundus imaging can detect postoperative retinal breaks in air- filled eyes. lt would be a useful facility for follow-up after PPV with air tamponade. Facedown position and acquired visual rehabilitation may be shorten.
● KEYWORDS:rhegmatogenous retinal detachment; air tamponade; ultra-widefield fundus imaging system
DOl:10.18240/ijo.2018.07.20
Citation:Chen QY, Tang YX, He YQ, Lin HM, Gao RL, Li MY, Hou JT, Ma HJ, Zhang JL. Air tamponade in retinal detachment surgery followed by ultra-widefield fundus imaging system. Int J Ophthalmol 2018;11(7):1198-1203