Table 1 Visual acuity chart
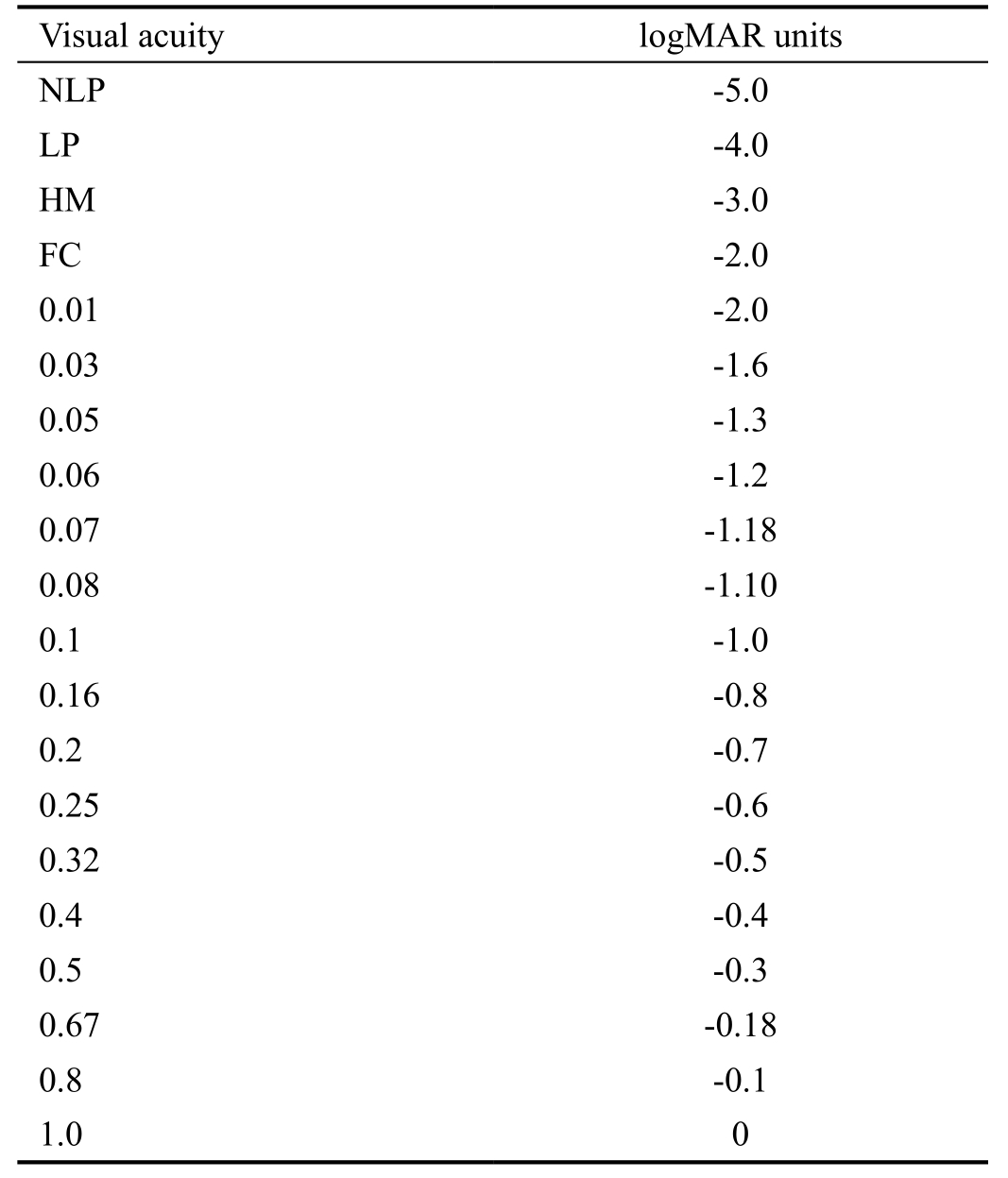
NLP: No light perception; LP: Light perception; HM: Hand movement; FC: Finger counting.
Ying-Jie Ma1, Bo Yu2, Yun-Hai Tu2, Bang-Xun Mao1, Xin-Yi Yu1, Wen-Can Wu2
1Eye Hospital of Wenzhou Medical University, Wenzhou 325000, Zhejiang Province, China
2Department of Orbital and Oculoplastic Surgery, Eye Hospital of Wenzhou Medical University, Wenzhou 325000, Zhejiang Province, China
Traumatic optic neuropathy (TON) is a relatively rare but potentially severe complication of head injury. It occurs in about 2.5% of midface fractures and 10% of craniofacial fractures[1-2]. The initial clinical findings of TON include decrease of visual acuity (VA), presence of relative afferent pupillary defect.
TON can be caused by direct or indirect injury. Direct optic injury usually results from optic nerve avulsion or laceration, or from direct fracture of the optic canal. Indirect traumatic optic neuropathy (ITON) is caused by increased intracanalicular pressure after an injury, which usually initiates a cascade of molecular and chemical mediators leading to secondary disorders such as intraneural edema, haematoma, altered microvasculature or cerebrospinal fluid circulation, and interruption of direct axoplasmic transport[3]. The prognosis of direct optic injury is usually quite poor. But indirect injuries,such as edema, hematoma or moderate bony optic nerve compression, may derive benefit from treatment[4].
The management for ITON is still controversial. Endoscopic trans-ethmosphenoid optic canal decompression (ETOCD) was a new treatment for it which raised up this decade by some eye nose and throat doctors. The identification of prognostic signs during the hospital admission of such patients has important implications, as such signs may be used to justify medical or surgical treatment depending on the expected outcome[5].Furthermore, patients suffered from ITON may show some benefit from treatment versus observation alone.In this case series, we set out to investigate a possible correlation between VA prognosis and the presence at baseline of various orbital and ocular signs in patients affected by ITON.
Ethics ApprovalThe study was authorized by The Eye Hospital of Wenzhou Medical University and followed the principles outlined in the Declaration of Helsinki (2008). It was approved by the Institutional Ethics Committee [KYK (2016)18; Medical Ethics Committee, Wenzhou Medical University,Wenzhou, Zhejiang Province, China].
Clinical DataThree hundred and twenty two cases with unilateral ITON aging from 18-64 year-old were indentified from the electronic medical record system of Eye Hospital of Wenzhou Medical University from July 1st, 2012 to July 1st,2015. ITON was diagnosed based on severe reduction or loss in VA accompanied by a relatively afferent papillary defect after a closed head injury and the ITON could not be explained by other causes. If necessary, visual field examination and visual evoked potential (VEP) were performed for diagnosis.High-resolution computed tomography (CT) scan of the head and the orbit was performed in all patients. All cases after admission were administered by methylprednisolone (20 mg/kg·d)and mouse-derived nerve growth factor (NGF; 30 µg/mL·d; Staidson Beijing) for 3d. And then patients whose VA showed no improvement after intravenous treatment were recommended to ETOCD. Patients were followed up to 3mo after surgery.Patients with bilateral ITON were not included because these patients may accompany by cranial cerebral injury or optic chiasm injury. Patients had craniocerebral operations because of severe brain injury were also excluded in our study. Patients had previous treatment were excluded as well.
A total 224 patients were included in this study. There were 35 patients excluded, who gained VA improvement after 3d of methylprednisolone and NGF and didn’t subjected to ETOCD. Another 17 patients with no VA improvement refused the surgery. Of 11 patients who had incomplete preoperative exam were excluded from all analyses. Follow-up data were incomplete for 35 patients who were excluded from all analyses as well.
We recorded the age of these 224 patients, VA before treatment,VA at the 3mo after surgery, time to medical treatment,together with other complications like brain injury, orbital fracture and optic canal fracture (OCF). VA was measured with Snellen Chart. Visual results were converted into logarithm of minimum angle of resolution (logMAR) unit for the purpose of analysis based on an extended scale to assess the effect of surgical decompression (Table 1)[6]. Improvement degree of visual acuity (IDVA) was calculated according to Chen et al’s[6]equation: Improvement degree=postoperative logMAR-preoperative logMAR (0.12-preoperative logMAR);20/15 (logMAR=0.12) is considered to be perfect vision.
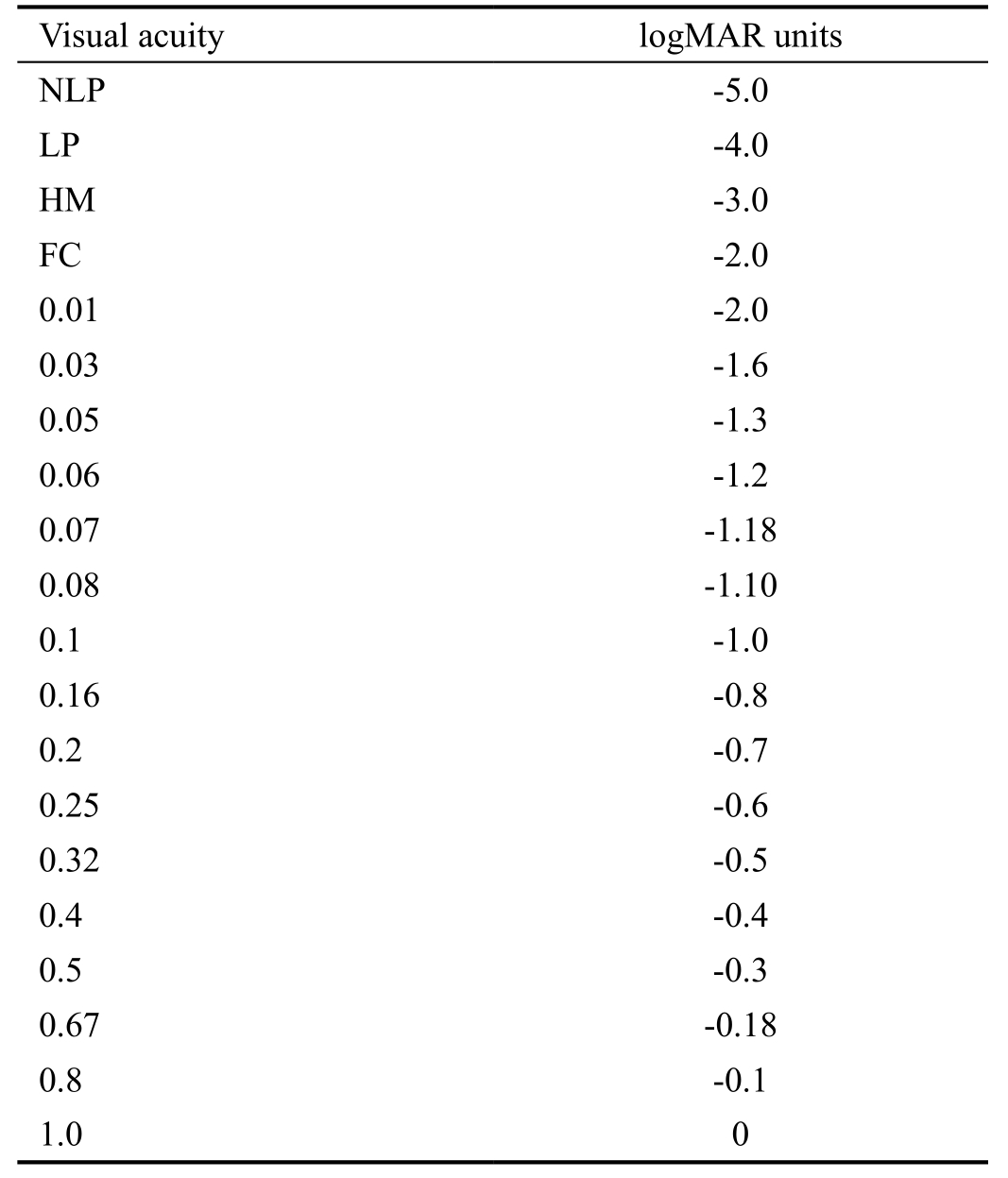
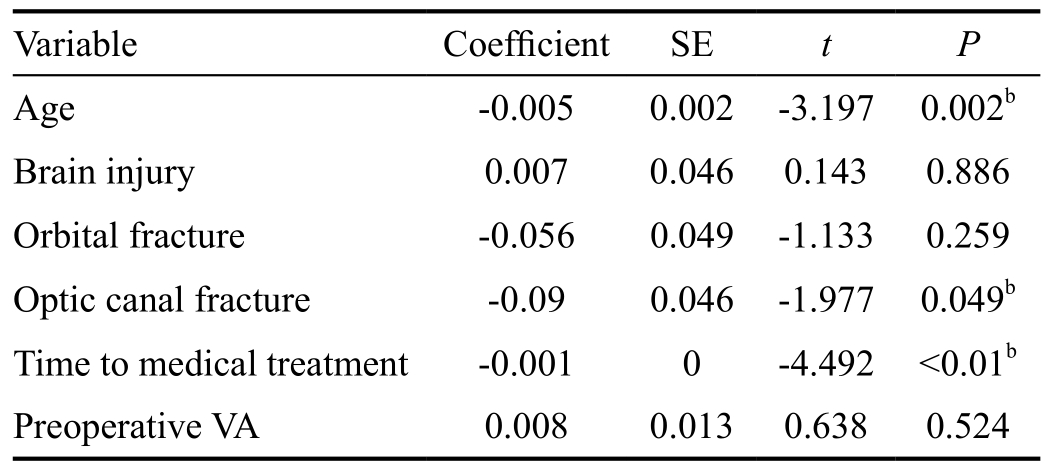
Surgical ProcedureAll of the procedures were performed under general anesthesia by a single orbital surgeon (Wu WC). During endoscopic optic nerve decompression, a routine endoscopic sphenoethmoidectomy was performed using the Messerklinger technique with preservation of the middle turbinate. The sphenoid face is opened widely, and the bulge of the optic nerve canal is identified along the lateral wall of the sphenoid sinus, superior to the carotid artery. In some patients, the optic canal may be identified initially ina posterior ethmoid or Onodi cell, which can be identified on preoperative CT scan. Identification and opening of the Onodi cell is important to provide adequate surgical exposure and allow full access to the optic canal. In some children, the sphenoid sinus were not fully developed, in order to locate the optic nerve canal, the navigation system were used during surgeries. After complete sphenoethmoidectomy, the lesser wing of the sphenoidal bone and the medial wall of the optic canal, which spans from the orbital aperture to the cranial cavity, were thinned with a microdrill and removed with a microcurrette. Then, the periorbita of the orbital apex, annulus of Zinn and the optic nerve sheath were incised with a sharp 9#MVR knife. Finally, the operating field of the optic canal was covered by a piece of sterile gelatin sponge that was immersed in dexamethasone (5 mg2/mL) and mouse-derived NGF (30 µg/mL). Postoperative care included administering methylprednisolone (20 mg/kg·d) for 4d, ceftriaxone (2.0 g/d)for 5d and NGF (30 µg/mL·d) for 1mo. To further decrease the pressure of optic canal and decrease the complications,we performed punctuated optic nerve sheath splitting in this study. This procedure is different from the traditional way of slitting the optic nerve sheath. In our procedure, 5 to 6 small intermittently punctuated incision was made to the optic nerve sheath to further release the pressure with little risk of complications. In the meanwhile, the splitting can create extra space for local administration of dexamethasone and mousederived NGF (Figure 1).
Table 1 Visual acuity chart
NLP: No light perception; LP: Light perception; HM: Hand movement; FC: Finger counting.
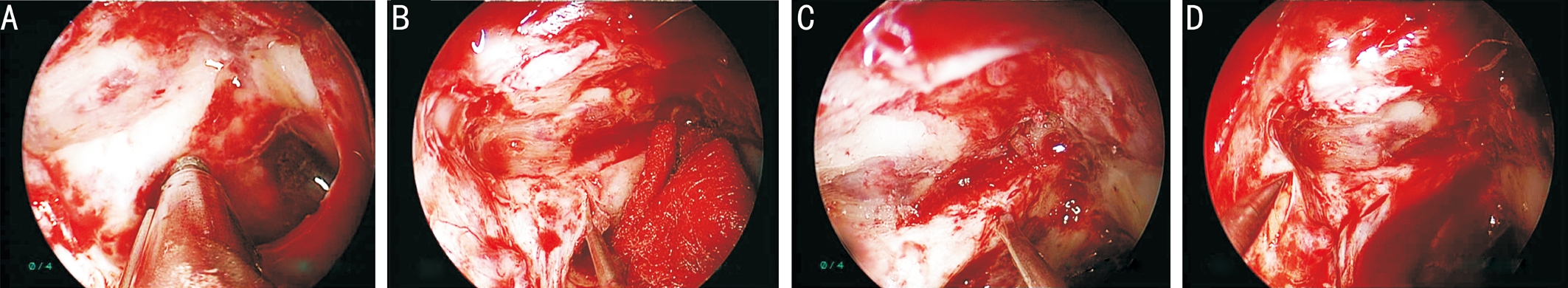
Figure 1 The surgical procedures of ETOCD A: The medical wall of optic canal was thinned by a microdrill; B: The thinned medial wall of optic canal was removed by a microcurrette; C: The optic nerve sheath was incised to create 5 to 6 small intermittently punctuation; D: The periorbita of the orbital apex and annulus of Zinn was split with a sharp 9# MVR knife.
Statistical AnalysisStatistical analyses were performed with SPSS 17.0 software (SPSS Inc., Chicago, IL, USA).Multiple linear-regression analysis was performed to identify independent predictors for postoperative visual and improvement degree of VA in patients. Paired t-test was performed to compare patients’ VA before and after surgery.Independent t-test was performed to compare the improvement degree of VA between patients with OCF and those without OCF. Results were considered significant at P<0.05.
Among the 224 surgical cases (224 eyes), 199 were male and 25 were female. The mean age of all cases was 34.21±12.77y.One hundred and fifteen cases affected right eye while 109 cases affected left eye. The most common cause of ITON in our study was fall (105/224), followed by car accident (89/224)and assaults (30/224). Totally 86 patients had mild brain injury after trauma. Orbital fracture was found in 143 patients. There were 43 cases with OCF shown on image scan and another 37 detected during the surgery (Table 2).
VA before surgery ranged from -5.0 to -0.1, with a mean value of -3.18±1.79. VA after surgery ranged from -5.0 to 0, with a mean value of -2.32±1.75. Postoperative VA was significantly higher than preoperative one (t=-10.622, P<0.05). Time to medical treatment ranged from 1-540d, with a mean time of 30.07±67.9d. IDVA ranged from -1.79 to 0.98, with a mean value of 0.25±0.32.
Multiple linear-regression analysis was conducted to identify variables that may independently predict the postoperative VA and IDVA. The results showed that age, time to medical treatment and preoperative VA were independent predictors for postoperative VA. The existence of OCF was also an independent predictor for poor postoperative VA. In contrast,brain injury and orbital fracture did not seem to be independent predictors for VA after surgery. Age and time to medical treatment were independent predictors for IDVA. The existence of OCF was also an independent predictor for lower IDVA. In contrast, preoperative VA, brain injury and orbital fracture did not seem to be independent predictors for IDVA (Tables 3, 4).Mean value of IDVA in patients with OCF was 0.19±0.30.Mean value of IDVA in patients without OCF was 0.29±0.35.IDVA in cases without OCF was significant higher than those with OCF (t=2.272, P<0.05). During the surgery, 11 patientsdeveloped cerebrospinal fluid rhinorrhea. Nine of them were repaired by mucosal flap transplantation uneventfully during surgery and two resolved from strict bed rest in a 30 degree of head-up and feet-down position. Four experienced cavernous sinus hemorrhage during the surgery, which was controlled by pressing and packing hemostasis. No other severe complications were observed.
Table 2 Clinical characteristic of 224 surgical cases n (%)
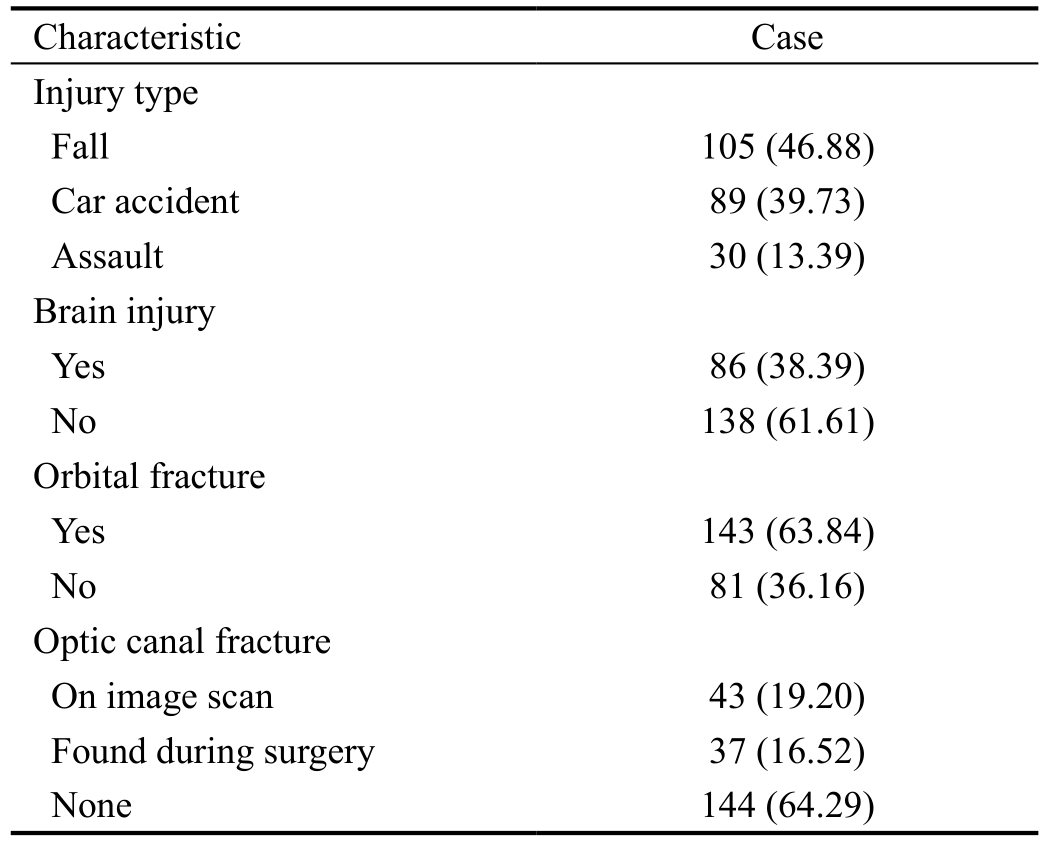
Table 3 Multiple linear regression to predict postoperative VA
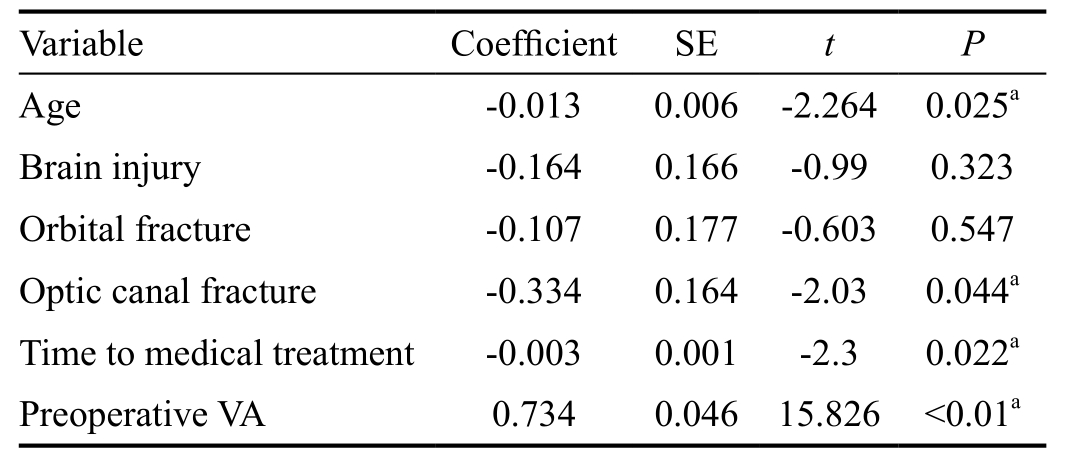
VA: Visual acuity; SE: Standard error.aIndicate independent predictor for VA after surgery (P<0.05).
Table 4 Multiple linear regression to predict IDVA
IDVA: Improvement degree of visual acuity; VA: Visual acuity; SE:Standard error.bIndicate independent predictor for IDVA (P<0.05).
ITON is a rare but serious complication after head trauma.Motor vehicle is the most common cause of ITON, followed by bicycle accident, falls and assaults[7-8].
Treatment for ITON remains controversial and no definite conclusion has been reached yet. According to previous studies, the VA improvement rate of high-dose steroid treatment, and high-dose steroid combined with optic canal decompression (OCD) were 4.3%-44%, 60.9%-71.1%[6,9-10]. OCD with or without combination of steroid is generally thought to be more effective in visual improvement than steroid treatment only. OCD physically decompresses the nerve within the canal, thereby creating the space for the nerve to swell,limiting the damaging effect of compression and helping the re-establishment of optic nerve function[6]. Endoscopic approach of OCD is gaining its preference for its decreased morbidity, preservation of olfaction, ideal cosmetic results without external scarring, an excellent view of the orbital apex as compared with intracranial approaches[9].
In our study, we find out that older in age, longer time to medical treatment and bad preoperative VA were independent factors for VA prognosis. Older in age and longer time to medical treatment were independent predictors for IDVA.Younger patients always have better potentiality and ability to rehabilitation which leaded to better prognosis. This finding is consistent with previous studies[11-12]. Early treatment is also thought to be a better prognostic factor. We believe that early treatment can reduce post-traumatic edema, contusion necrosis, and vasospasm, and thus aid functional recovery. It is likely that more axons will recover function if the treatment started early[13-14]. The baseline VA is also thought to be a strong predictor of prognosis. It is indicated that the residual vision is crucial for VA prognosis and patients with eyesight left may benefit more from the surgical intervention, since no residual vision implies the probable degeneration and apoptosis of ganglionic cells of the retina[15]. However, we found that preoperative visual was a strong predictor of VA prognosis but had no correlation with IDVA. This interesting finding suggests that better baseline vision doesn’t mean better improvement in VA after surgery. Patients with better VA before surgery sometimes had less level of VA improvement than those with poor VA before surgery.
The correlation between OCF and VA prognosis of ITON has been identified in previous researches[14,16-17]. This also seems to be applicable in our study. Existing of OCF was found to be an poor prognostic factor for VA prognosis and IDVA in our study. Patients with OCF had lower IDVA than those without OCF. Apart from indicating the severity of the injury, OCF itself can cause devastating damage to optic nerve by bony fragment injury and/or structural deformation,followed by increased intracanalicular pressure or even intracanalicular hematoma[5]. That’s the reason why prompt surgical intervention should be advocated once OCF is identified[18-19]. The correlation between the existence of orbital fractures and prognosis of ITON is still unclear. Cook et al[20]and Tsai et al[19]thought that the existence of orbital fracture was associated with large external forces, which lead to more severe optic nerve injury. However, Song et al[21]found no correlation between orbital fracture and prognosis of ITON.No correlations was detected either between orbital fracture and VA prognosis or between orbital fracture and IDVA in our study. We presume that large external forces caused by orbital fracture do not always conduct to optic nerve. Researches are needed to further prove the correlation among orbital fracture,OCF and optic nerve injury.
No correlation was detected between brain injury and prognosis (VA prognosis and IDVA) as well in our study. The relevant research was limited. We presumed that brain injury did not seem to related with optic nerve injury. In addition, we excluded cases with bilateral ITON and severe brain injury.This may be another reason of this result.
Traditional ETOCD still has some limitation. It is believed to be much more difficult performing ETOCD in cases with abnormal anatomical structure, especially those with undeveloped sphenoid and posterior ethmoid sinuses. In our study, 13 patients of 224 (5.8%) had undeveloped sphenoid sinus which make it dif ficult to identify the optic nerve canal bulge. Traditional way of optic nerve canal splitting would increase the risk of complications like cerebrospinal fluid leakage, ophthalmic artery injury and optic nerve injury.
In order to improve the effectiveness and safety of surgery,several modifications of surgical procedure were made in our study: 1) image navigation system was used for these patients whose sphenoid sinuses were not fully developed, to locate the optic nerve canal under image-guided system (Figure 2); 2)punctuated incision was made when split the optic nerve canal.This procedure is different from the traditional way of slitting the optic nerve sheath, which is associated with complications like cerebrospinal fluid leakage, ophthalmic artery injury, and optic nerve injury. In our procedure, 5 to 6 small intermittently punctuated incisions were made to the optic nerve sheath to further release the pressure with little risk of complications.Meanwhile, the splitting can create extra space for local administration of dexamethasone and mouse-derived NGF.The medicine would accumulate in sphenoid sinus for slow releasing and promote optic nerve rehabilitation continually.We also decompress the orbit apex by opening the periorbital of the orbital apex and annulus of Zinn to further decrease intracanal pressure.
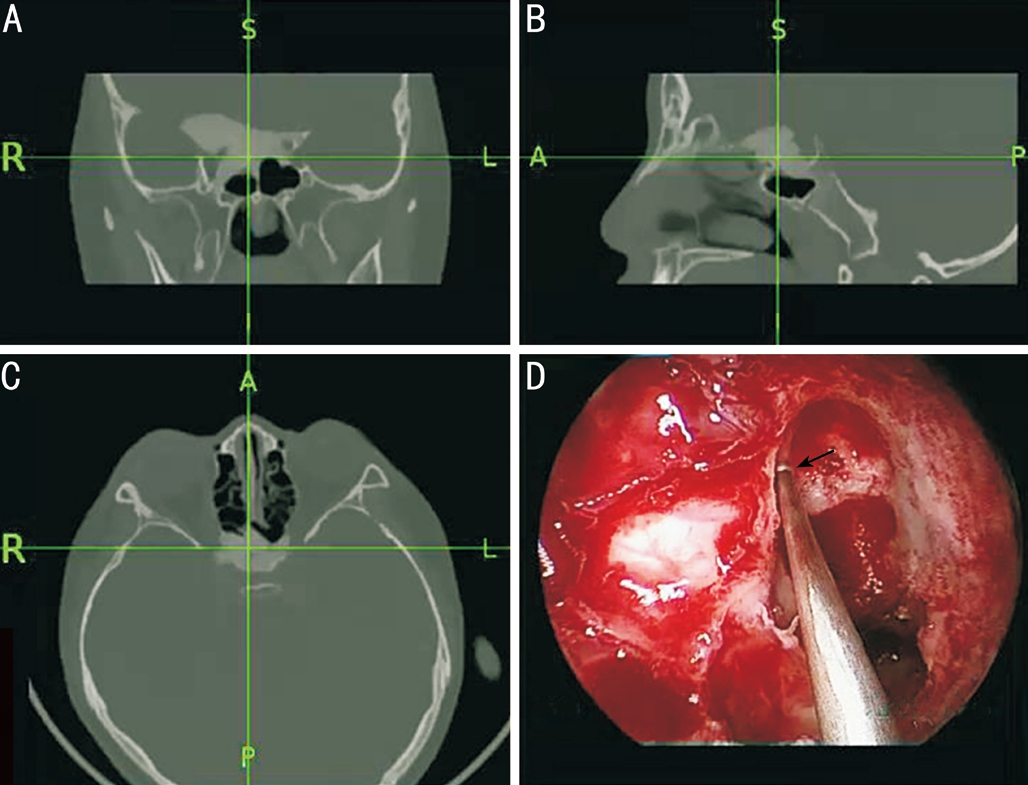
Figure 2 The image navigation system used on one patient with undeveloped sphenoid sinus A: Coronal; B: Sagittal; C: Axial. The intersection point of the two crossing green indicates the location of optic canal; D: Surgical image under navigation system (The black arrow indicates the optic canal).
Patients suffered from ITON without OCF before ETOCD have better surgical outcome than those with OCF. Older in age, longer time to medical treatment and existence of OCF are independent factors for poor VA prognosis and lower IDVA. Preoperative VA is independent factor for VA prognosis only. No severe complication is encountered. Large-sampled controlled prospective researches are needed to further prove the rationality of ETOCD for patients with ITON and to work out the exact surgical indication.
The authors thank Dr. Jie-Liang Shi and Ben Chen, for providing medical care for the patients and collecting the clinical data.
Authors’ contributions:Wu WC: design, analysis, writing and final approval; Ma YJ: design, data collection, writing the paper, analysis of data and final approval; Yu B: design,analysis, writing the paper, revising the paper and final approval; Tu YH: analysis, writing and final approval; Mao BX: data collection, writing and final approval; Yu XY: data collection, writing and final approval.
Foundations:Supported by the Natural Science Foundation of China (No.81371028); Natural Science Foundation of Zhejiang Province, China (No.LY12H12006) and the Guided Innovation Project of the Eye Hospital of Wenzhou Medical University(No.YNCX201104).
Conflicts of Interest: Ma YJ,None;Yu B,None;Tu YH,None;Mao BX,None;Yu XY,None;Wu WC,None.
REFERENCES
1 Anderson RL, Panje WR, Gross CE. Optic nerve blindness following blunt forehead trauma.Ophthalmology1982;89(5):445-455.
2 He Z, Li Q, Yuan J, Zhang X, Gao R, Han Y, Yang W, Shi X, Lan Z.Evaluation of transcranial surgical decompression of the optic canal as a treatment option for traumatic optic neuropathy.Clin Neurol Neurosurg2015;134:130-135.
3 Steinsapir KD, Goldberg RA. Traumatic optic neuropathy: an evolving understanding.Am J Ophthalmol2011;151(6):928-933.e2.
4 Li H, Zhou B, Shi J, Cheng L, Wen W, Xu G. Treatment of traumatic optic neuropathy: our experience of endoscopic optic nerve decompression.J Laryngol Otol2008;122(12):1325-1329.
5 Kamala KS, Sumathi V, Ariga M, Krishna KK. Visual outcome following endoscopic optic canal decompression in compressive and traumatic optic neuropathy- a prospective observational study.Scholars Journal of Applied Medical Sciences2016:1940-1945.
6 Chen CT, Huang F, Tsay PK, Tsai YJ, Lin CH, Chen YC, Chen YR.Endoscopically assisted transconjunctival decompression of traumatic optic neuropathy.J Craniofac Surg2007;18(1):19-26;discussion 27-28.
7 Sosin M, Cruz CDL, Mundinger GS, Bojovic B, Christy MR. Traumatic optic neuropathy: an 8-year experience of management and outcomes analysis.Plastic & Reconstructive Surgery2014;134:17.
8 Wang DH, Zheng CQ, Qian J, Barr JJ, Anderson AG Jr. Endoscopic optic nerve decompression for the treatment of traumatic optic nerve neuropathy.ORL J Otorhinolaryngol Relat Spec2008;70(2):130-133.
9 Xu R, Chen F, Zuo K, Ye X, Yang Q, Shi J, Chen H, Li H. Endoscopic optic nerve decompression for patients with traumatic optic neuropathy:is nerve sheath incision necessary?ORL J Otorhinolaryngol Relat Spec2014;76(1):44-49.
10 Levin LA, Joseph MP, Rizzo JF 3rd, Lessell S. Optic canal decompression in indirect optic nerve trauma.Ophthalmology1994;101(3):566-569.
11 Lee V, Ford RL, Xing W, Bunce C, Foot B. Surveillance of traumatic optic neuropathy in the UK. Eye (Lond) 2010;24(2):240-250.
12 Dhaliwal SS, Sowerby LJ, Rotenberg BW. Timing of endoscopic surgical decompression in traumatic optic neuropathy: a systematic review of the literature.Int Forum Allergy Rhinol2016;6(6):661-667.
13 Yan W, Chen Y, Qian Z, Selva D, Pelaez D, Tu Y, Wu W. Incidence of optic canal fracture in the traumatic optic neuropathy and its effect on the visual outcome.Br J Ophthalmol2017;101(3):261-267.
14 Levin LA. Intrinsic survival mechanisms for retinal ganglion cells.Eur J Ophthalmol1999;9(Suppl 1):S12-S16.
15 Carta A, Ferrigno L, Salvo M, Bianchi-Marzoli S, Boschi A, Carta F. Visual prognosis after indirect traumatic optic neuropathy.J Neurol Neurosurg Psychiatry2003;74(2):246-248.
16 Wang BH, Robertson BC, Girotto JA, Liem A, Miller NR, Iliff N,Manson PN. Traumatic optic neuropathy: a review of 61 patients.Plast Reconstr Surg2001;107(7):1655-1664.
17 Levin LA, Baker RS. Management of traumatic optic neuropathy.J Neuroophthalmol2003;23(1):72-75.
18 Volpe NJ, Levin LA. How should patients with indirect traumatic optic neuropathy be treated?J Neuroophthalmol2011;31(2):169-174.
19 Tsai HH, Jeng SF, Lin TS, Kueh NS, Hsieh CH. Predictive value of computed tomography in visual outcome in indirect traumatic optic neuropathy complicated with periorbital facial bone fracture.Clin Neurol Neurosurg2005;107(3):200-206.
20 Cook MW, Levin LA, Joseph MP, Pinczower EF. Traumatic optic neuropathy.A meta-analysis.Arch Otolaryngol Head Neck Surg1996;122(4):389-392.
21 Song Y, Li H, Ma Y, Li W, Zhang X, Pan X, Tan G. Analysis of prognostic factors of endoscopic optic nerve decompression in traumatic blindness.Acta Otolaryngol2013;133(11):1196-1200.
Co- first authors:Ying-Jie Ma and Bo Yu
Correspondence to:Wen-Can Wu. Department of Orbital and Oculoplastic Surgery, Eye Hospital of Wenzhou Medical University, No.270 West Xueyuan Road, Wenzhou 325000,Zhejiang Province, China. 172015841@qq.com
Received:2017-07-04 Accepted: 2018-03-27
Abstract ● AlM: To investigate a possible correlation between visual acuity (VA) prognosis and the presence at baseline of various orbital and ocular signs in patients affected by indirect traumatic optic neuropathy (lTON).● METHODS: From July 1st, 2012 to July 1st, 2015, 224 adults diagnosed with lTON who underwent endoscopic transethmosphenoid optic canal decompression (ETOCD) were reviewed. Visual outcome before and after treatment were taken into comparison.● RESULTS: Accompanied older in age, longer time to medical treatment and existence of optic canal fracture (OCF)were the independent predictors for poor postoperative VA and lower improvement degree of visual acuity (lDVA),while worse preoperative VA was predictive factor for poor postoperative VA only. Mean value of lDVA in patients with OCF was 0.19±0.30. Mean value of lDVA in patients without OCF was 0.29±0.35. lDVA in cases without OCF was significant higher than those with OCF (t=2.272, P<0.05).● CONCLUSlON: Patients suffered from lTON without OCF before ETOCD have better surgical outcome than those with OCF. Older in age, longer time to medical treatment and existence of OCF are independent factors for poor VA prognosis and lower lDVA. Preoperative VA is independent factor for VA prognosis only.
● KEYWORDS:trans-ethmosphenoid optic canal decompression;indirect traumatic optic neuropathy; adults; visual acuity;improvement degree of visual acuity
DOl:10.18240/ijo.2018.07.24
Citation:Ma YJ, Yu B, Tu YH, Mao BX, Yu XY, Wu WC.Prognostic factors of trans-ethmosphenoid optic canal decompression for indirect traumatic optic neuropathy. Int J Ophthalmol 2018;11(7):1222-1226