Long-term effect of triamcinolone acetonide in the treatment of upper lid retraction with thyroid associated ophthalmopathy
Dong-Dong Xu1, Yu Chen2, Hai-Yan Xu1, Hui Li1, Zhu-Hua Zhang2, Yu-Hua Liu1
1Department of Ophthalmology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences &Peking Union Medical College, Beijing 100730, China
2Department of Radiology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing 100730, China
INTRODUCTION
Thyroid associated ophthalmopathy (TAO) is an autoimmune disorder that targets the tissues of the orbit[1]. Upper eyelid retraction (ULR) is the most common lid manifestation in patients with Graves’ disease and has been used as part of the diagnostic criteria for the disease[2]. Although most signs of TAO can be attributed to inflammatory swelling and fibrosis of the extraocular muscles, the pathophysiological basis for the lid retraction is not clear. Immunologically reactive inflammation might cause lid retraction in the early stages of the disease[3].Most patients become distressed due to a cosmetically transformed appearance, even for mild eyelid retraction[4].There are now several techniques used to treat this disease,including Botox and filler injections and surgeries in the burntout stage[5-7]. Botox treatment is temporary and sometimes leads to strabismus and ptosis, which is unacceptable to patients. Fillers such as hyaluronic acid gel were recently used for several patients, but a larger sample is still required to test for its efficiency and potential complications[6]. Theoretically,Botox and filler injections may not affect the improvement of eyelid soft-tissue inflammation. Surgical options have significant risks as well as unpredictable courses and outcomes in some cases.
It has been found that repeated subconjunctival triamcinolone acetonide (TA) is a good modality in treating ULR, which was introduced in 2007[8]. Most patients experienced improvement in ULR. Although this method has been described in several documents[9-12], the long-term effects and adverse effects of a large cohort of patients have not been previously reported.Thus, this study was to evaluate both the short-term and longterm effects of repeated subconjunctival TA injections in treating eyelid retraction with TAO.
SUBJECTS AND METHODS
This retrospective clinical study was conducted from 2009 to 2016. The documents of 97 patients (126 eyes) were reviewed.The patients fit the following inclusion criteria: mild to moderate TAO with features of either unilateral or bilateral lid retraction; clinical activity score≤3[10]; age of 18 years or older; absence of other systemic disease; absence of myopathy,severe proptosis, optic neuropathy, cornea ulcer, and recent glucocorticoid administration. Exclusion criteria were previous treatment for TAO with steroids or radiation, and compressive optic neuropathy. All patients were informed of the benefits and possible side effects of the treatment. After informed consent was obtained, patients were evaluated pre- and posttreatment by taking measurements of the upper margin reflex distance (MRD1, the distance between the upper-lid margin and the pupil center), lid aperture, lagophthalmos and proptosis. The upper eyelid positions above (positive value)and below (negative value) the superior limbus were measured in millimeters. These measurements were repeated three times,and the mean value was recorded. The ophthalmological examination included best-corrected visual acuity (BCVA)for distance, intraocular pressure (IOP) (in primary position),pupil reflexes, ocular motility and fundoscopy with direct ophthalmoscopy. Proptosis was measured by the same Hertel exophthalmometer, and photographs were taken before and after the treatment.
The treatment was conducted in a procedure room in an outpatient setting under topical anesthesia. A volume of 0.5 mL(40 mg/mL) TA solution (Kunming Jida Pharmaceutical Co.,Ltd., China) was injected into the subconjunctival area 5 mm above the upper edge of the everted tarsus. The treatment was repeated monthly and stopped if the retraction completely resolved. The patients were treated less than 10 times.
Magnetic resonance imaging (MRI) was performed using a general electric 3.0T MRI system (GE Signa VH/I EXCITEII 3.0T, General, electric medical systems, Milwaukee, WI,USA). MRI was performed with coronal T1-weighted (T1W) and T2-weighted patient fat-suppressed fast spin-echo (T2W-FS)images. Contrast-enhanced images (T1W-C) were obtained with Gadopentetate Dimeglumine (BEILU pharmaceutical Co., Ltd., Beijing, China) consisting of axial, coronal and sagittal fat-suppressed T1-weighted images and were acquired on a plane parallel to the optic nerve. Imaging analysis were assessed by experienced radiologist (Chen Y), who were unaware of the clinical findings. The ULR indexes were measured as follows: the brightest signal intensity on coronal T1W, T2W-FS and T1W-C images and the largest areas of coronal T1W-C images. This measured signal intensity of the ULR was set in proportion to that of the ipsilateral temporalis muscle to calculate the signal intensity ratio (SIR). The temporalis muscle was selected due to its structural similarity and close anatomical relationship to the extra-ocular eye muscles and missing inflammation in TAO.
The patients were divided into the cured group, the improved group and the ineffective group based on the final treatment effectiveness. Patients in the cured group had a final MRD1 of ˂4 mm for both eyes, and the difference of the MRD1 between the two eyes was ˂1 mm. Patients in the improved group had an MRD1 that decreased after treatment. The MRD1 of one or both eyes was ≥4 mm, or the difference of the MRD1 between two eyes decreased but was still ≥1 mm. Patients in the ineffective group had an MRD1 that didn’t change or increased rather than decreased, and the differences between the two eyes did not decrease. The non-cured group consisted of the improved group and the ineffective group.
The grading scales of the eyelid retraction for patients were classified as grade 1 and grade 2. For grade 1, lid retraction of the patient was ≤1 mm; while those whose lid retraction was ˃1 mm belong to grade 2. Relapse means that the eyes of the patients get normal for at least 3mo and then get retracted again.
The authors certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research.
Statistical AnalysisNumeric variables with normal distributions were compared using a Student’s t-test (paired and independent). Variables with non-normal distributions, as described by the median (minimum, maximum), were tested using the Wilcoxon signed-rank test. Fisher’s exact test and a Chi-square test were used for rate comparisons. A P value ˂0.05 at a 95% confidence interval was considered statistically significant. The analysis was performed using SPSS version 10.1 (SPSS Inc, Chicago, IL, USA).
RESULTS
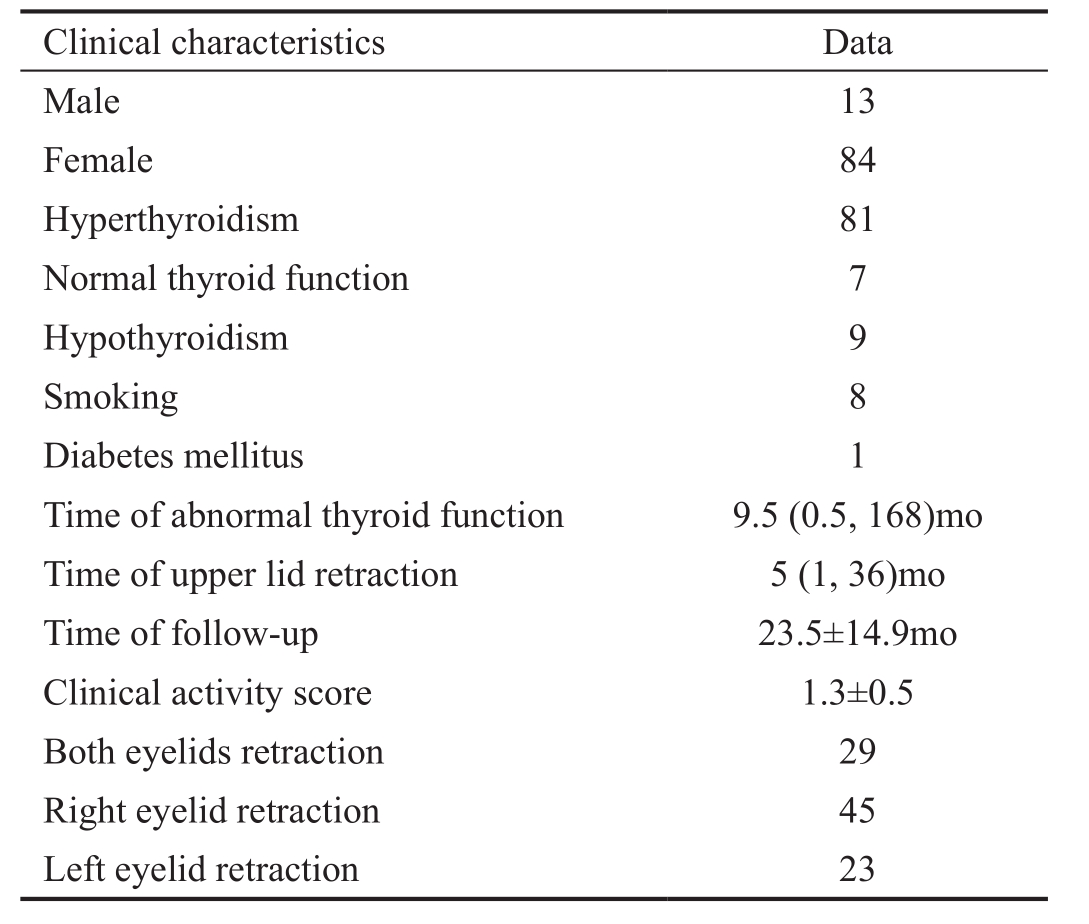
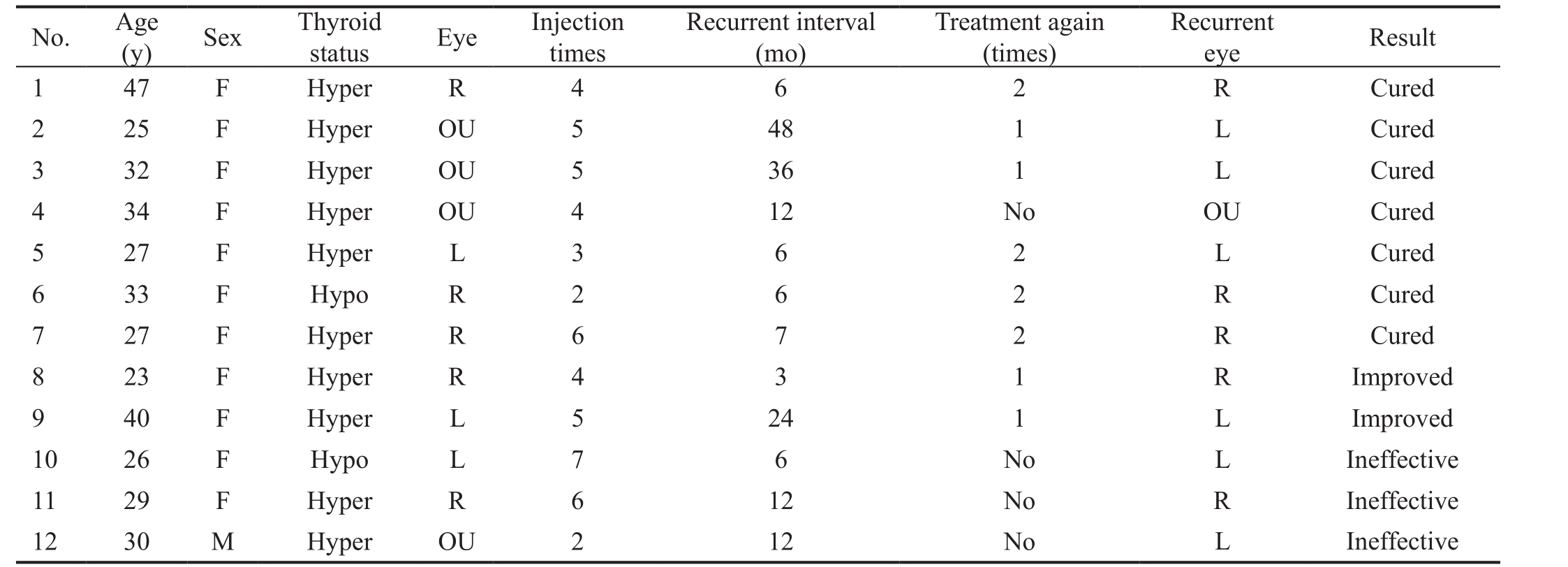
The mean age of patients in the study population was 32.5±8.9y. The characteristics of the patients are summarised in Table 1.
Table 1 Demographics of the patients
Clinical characteristics Data Male 13 Female 84 Hyperthyroidism 81 Normal thyroid function 7 Hypothyroidism 9 Smoking 8 Diabetes mellitus 1 Time of abnormal thyroid function 9.5 (0.5, 168)mo Time of upper lid retraction 5 (1, 36)mo Time of follow-up 23.5±14.9mo Clinical activity score 1.3±0.5 Both eyelids retraction 29 Right eyelid retraction 45 Left eyelid retraction 23
The patients were treated with subconjunctival injections monthly, and the medium injection times were 5 (1, 10).Injection times for cured group was 4.66±1.74, and for noncured group was 5.17±2.08 (P˂0.05). Sixty-three (64.9%)patients were assigned to the cured group, 22 (22.7%) patients were in the improved group, 12 (12.4%) patients in the ineffective group. The clinical activity score decreased from 1.25±0.55 at the first examination to 0.01±0.1 at the final examination.
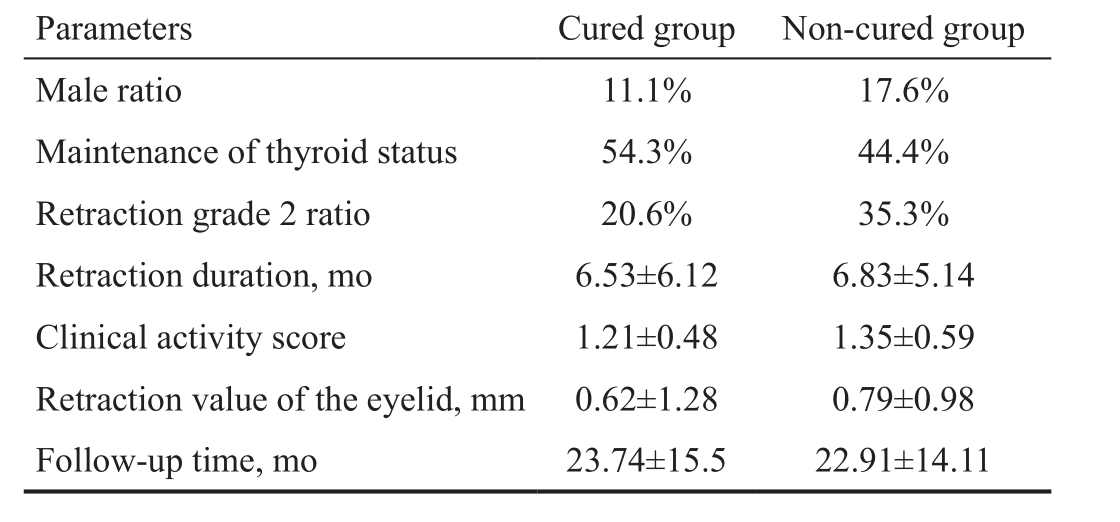
There are no significant differences between cured and noncured group before treatment (Table 2).
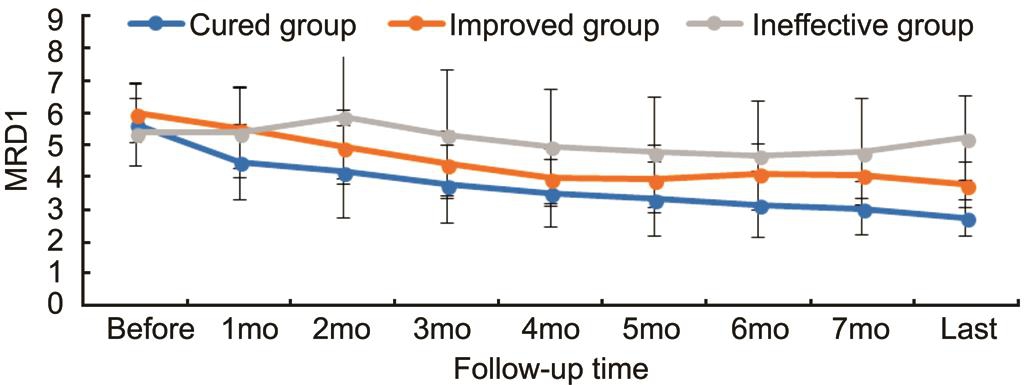
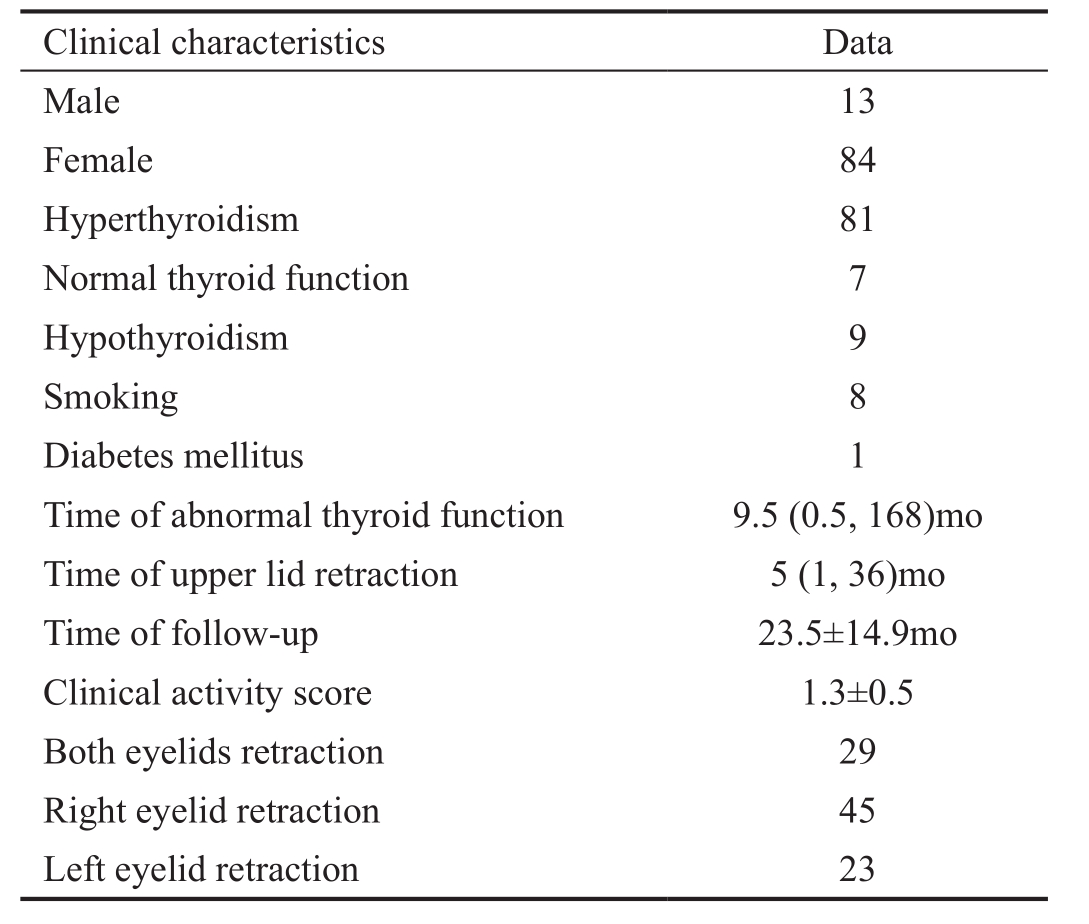
The MRD1 decreased from 5.46±1.03 mm before treatment to 2.74±0.47 mm at the final follow-up in the cured group(P˂0.05). In the improved group, the MRD1 changed from 6±0.71 mm to 3.77±0.57 mm (P˂0.05). For the ineffective group, the MRD1 was 5.4±0.83 mm before treatment, and it was 5.23±1.01 mm at the final follow-up (P˃0.05). Lid retraction (LR) decreased from 1±0.71 mm to -2.26±0.47 mm in the cured group (P˂0.05). In the improved group, the LR changed from 1±0.71 to -1.23±0.57 mm (P˂0.05). In the ineffective group, the LR was 0.4±0.83 before treatment, and the final LR was 0.23±1.01 mm (P˃0.05). Proptosis changed from 16.74±2.12 mm to 17.34±2.0 mm (P˃0.05). IOP changed from 16.43±2.4 mm Hg to 17.58±2.55 mm Hg (P˃0.05). The MRD1 of the patients are shown in Figure 1.
The MRD1 significantly reduced between the baseline measurements and 1-month measurements after the initiation of treatment in the cured and improved groups (P˂0.001). The values did not change significantly after 4mo in the improved group, while they continued to decrease in the cured group. For the ineffective group, the MRD1 did not change significantly after treatment.
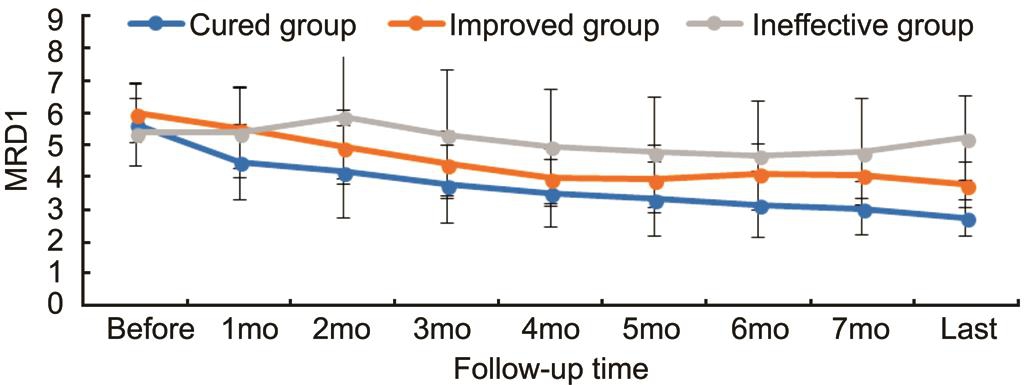
Figure 1 MRD1 change in three groups.
Table 2 Clinical characteristics of cured and non-cured group before treatment
Parameters Cured group Non-cured group Male ratio 11.1% 17.6%Maintenance of thyroid status 54.3% 44.4%Retraction grade 2 ratio 20.6% 35.3%Retraction duration, mo 6.53±6.12 6.83±5.14 Clinical activity score 1.21±0.48 1.35±0.59 Retraction value of the eyelid, mm 0.62±1.28 0.79±0.98 Follow-up time, mo 23.74±15.5 22.91±14.11
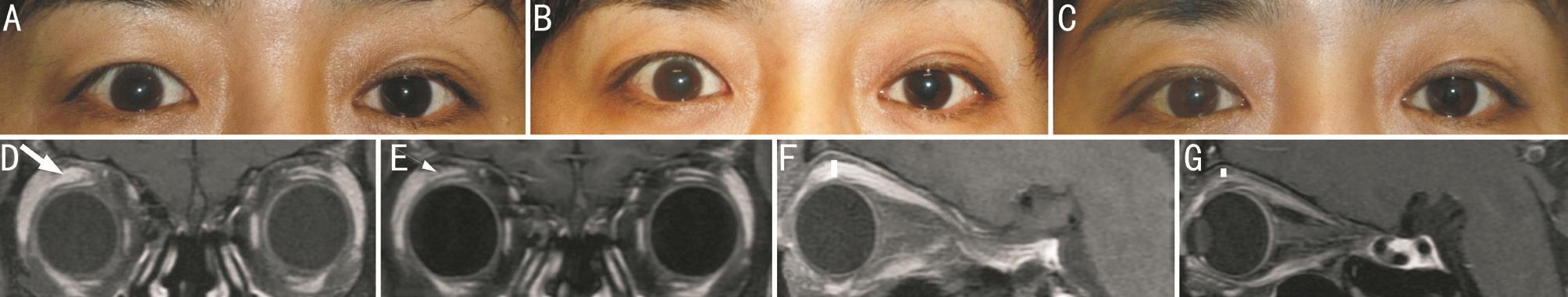
Forty-one patients underwent MRI examinations before and 6mo after treatment. A statistically significant difference was observed between the baseline and post-treatment values of the mean muscle thickness for the levator (2.95±0.99 mm vs 2.04±0.63 mm, P˂0.05). The levator muscle area was 27.27±10.5 mm2before the treatment, while this decreased to 18.3±7.04 mm2(P˂0.05) after the treatment. The coronal surface area of the levator before and after treatment was 25.96±8.57 mm2and 17.67±6.24 mm2in the cured group,27.57±9.23 mm2and 19±7.76 mm2in the improved group and 36.78±18.83 mm2and 21.5±8.52 mm2in the ineffective group.The photos and MRI results of a patient with right upper lid retraction before and after treatment were shown in Figure 2.In the cured group, the T2W SIR, T1W SIR, T1W-C SIR,levator thickness and levator area values were 1.67±0.44,0.76±0.1, 1.44±0.42, 2.86±0.88 mm and 25.96±8.7 mm2,respectively, before treatment. In the non-cured group, they were 2.11±0.97, 0.65±0.1, 1.58±0.52, 3.11±1.19 mm and 29.74±13.19 mm2, respectively. These values were compared between the cured group and the non-cured group separately.The differences were insignificant. In the cured group, T2W SIR was 1.42±0.34 after treatment (P˂0.05 vs pre-treatment).In the non-cured group, T2W SIR was 1.58±0.42 after treatment (P˃0.05 vs pre-treatment).
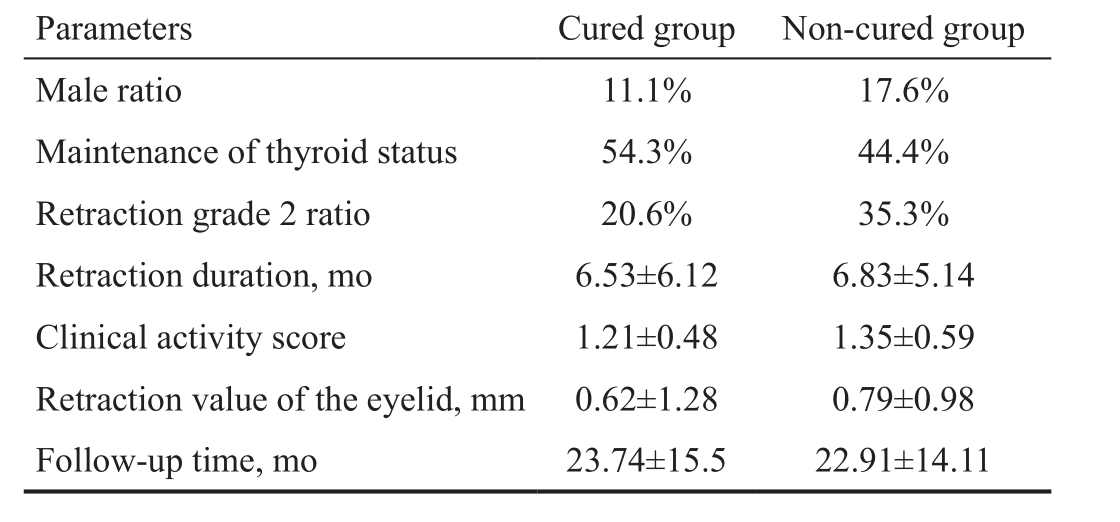
Twelve patients (12.4%) relapsed after treatment (Table 3).Some patients were treated with subconjunctival TA injections again. Seven patients completely recovered, two patients improved and three patients did not improve and were assigned to the ineffective group. Trigger events for relapses included fluctuating thyroid levels in two patients.
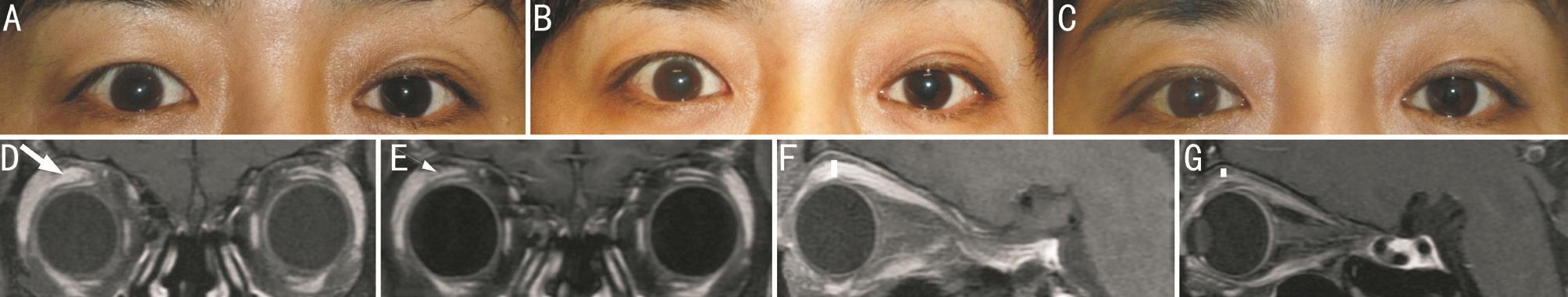
Figure 2 Complete recovery of the right upper lid retraction and MRI imaging of the patient A: Before treatment; B: Two months after the initiation of treatment; C: At last follow-up; D: The enlargement of the right levator palpebrae superioris (LPS) muscle area before treatment(thick arrow); E: Reduction of the LPS area after treatment (thin arrow); F: Thickening of the LPS with sagittal MRI before treatment (thick line segment); G: Thinning of the LPS after treatment (thin line segment).
Table 3 Demographics of the recurrent patients
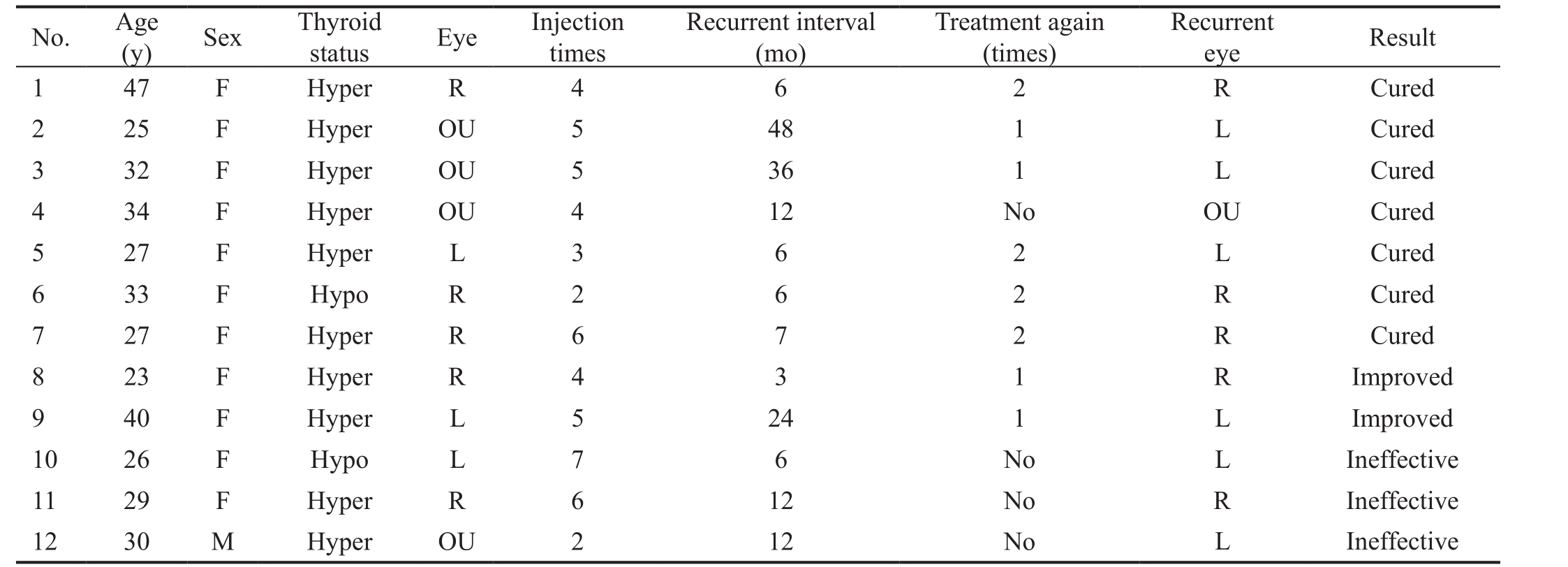
Hyper: Hyperthyroidism; Hypo: Hypothyroidism; OU: Both eyes; R: Right eye; L: Left eye.
No. Age(y) Sex Thyroid status Eye Injection times Recurrent interval(mo)Treatment again(times)Recurrent eye Result 1 47 F Hyper R 4 6 2 R Cured 2 25 F Hyper OU 5 48 1 L Cured 3 32 F Hyper OU 5 36 1 L Cured 4 34 F Hyper OU 4 12 No OU Cured 5 27 F Hyper L 3 6 2 L Cured 6 33 F Hypo R 2 6 2 R Cured 7 27 F Hyper R 6 7 2 R Cured 8 23 F Hyper R 4 3 1 R Improved 9 40 F Hyper L 5 24 1 L Improved 10 26 F Hypo L 7 6 No L Ineffective 11 29 F Hyper R 6 12 No R Ineffective 12 30 M Hyper OU 2 12 No L Ineffective
Side effects included menstrual cycle disturbances in 31(32%) patients. The symptoms and signs gradually regressed about three months after the final injections. Eighteen patients(18.6%) which were under topical anti-glaucomatous drugs for a total of 6-12mo, experienced elevations in IOP. Sixteen patients withdrew from the topical medicine gradually, and their IOP remained normal. Two patients underwent selective laser trabeculoplasty because their IOP could not be controlled by topical drugs, and then their IOPs returned to normal without medicine. Eight patients experienced body weight increases. Three patients developed hirsutism. Two patients(2.1%) complained of cramps in their calf muscles. One patient suffered from upper eyelid sulcus, but the patient completely recovered six months later. No patients with steroid-induced cataract was found.
DISCUSSION
TAO is an autoimmune disease that can affect the orbital tissues and the thyroid gland. It has been reported that ULR is the most common clinical sign of TAO[2]. In some TAO patients, ULR can exhibit spontaneous improvement[13]. It was found that in 50% of patients who formerly had conspicuous eyelid changes, ophthalmopathy was still obvious at the 15-year follow-up[14]. Persistent ULR was quite common,and the rate of spontaneous improvement was 17.4% in a previous study[8]. This can lead to emotional and psychological disturbances for patients due to cosmetic appearance changes[4].There have been several studies on subconjunctival injections of TA to treat ULR with subconjunctival injections of TA.Chee et al[9]reported a case series of four patients and found that two patients completely recovered, and one patient improved under this method. Lee et al[10]evaluated 30 patients with ULR associated with thyroid eye disease. The patients were given subconjunctival TA injections at 2-week intervals.The mean number of injections per patient was 2.67, and the follow-up time was 260.97±91.10d. The results showed that 19 of 22 patients in the congestive phase responded to the TA injection, while six of eight patients in the fibrotic phase did not respond to the TA injection[10]. Lee et al[11]investigated the efficacy of subconjunctival TA in treating upper lid retraction by conducting a prospective, single-blind randomised clinical study. The follow-up period was six months. Of the patients,75% achieved success at six months after 3-week intervals of injections. Only 37% of patients’ eyes returned to normal under observation only[11]. In a recent paper, Hamed-Azzam et al[12]found that 7/9 eyes suffering from lid retraction benefitted from the fornix subconjuctival TA injections during a 6-month follow-up[12]. The longest follow-up period reported in previous literature is 260.97±91.10d. The long-term effects and adverse effects of a large cohort of patients have not been reported previously. In this study, the patients were evaluated for 23.45±14.91mo. The rate of complete recovery was 64.9%,and the rate of improvement was 22.7%. The results and those from the above documents show that subconjunctival TA injection is an effective and long-lasting method in the treatment of ULR with TAO.
In the cured and improved group, the MRD1 was significantly reduced between the baseline measurements and 1-month measurements after the initiation of treatment. In the improved group, the values did not significantly change after four months, while they continued to decrease in the cured group. In the ineffective group, the MRD1 did not change significantly after treatment. When comparing the cured and non-cured group with pre-injection clinical values, no significant prognosis factor was found to be associated with successful outcomes. This was different from Lee et al’s[11]results, which showed that patients with a high degree of exophthalmos, retraction and swelling at pre-injection might experience limited effects from steroid injections on eyelid retraction and/or swelling for either a short-term or long-term injection period. Different conditions and success criteria between studies might be the reason for the difference.
MRI is a good objective tool for the diagnosis and followup of TAO[15]. Although computed tomography (CT) and ultrasonography (US) are widely used in the diagnosis of TAO,the soft-tissue spatial resolution of MRI is better than that obtained with CT and US. We find levator superioris enlarged,T2W SIR increased and contrast enhancement increased before treatment. Thinning of the levator superioris muscle and a reduction of the coronary muscle area after TA treatment was found during the MRI examinations. It has been reported that the levator was enlarged in ULR patients with TAO[16].The histopathological changes in TAO consist primarily of inflammation of the extraocular muscles and the orbital fat.Steroids can reduce muscle and soft-tissue edema, inhibit further inflammatory disease progression and prevent chronic fibrosis, thus decreasing the levator diameter with a consequent improvement of lid retraction. These results support the proposition that lid retraction in TAO is an immuno-reactive inflammation process and can be treated with TA. The effect was achieved through the reduction of tissue edema, but the degree and duration of active ophthalmopathy may limit the effects of lid retraction treatment.
The MRI indexes between the cured and non-cured groups were compared. T2W SIR was significantly lowered after treatment in the cured group, while it was insignificant in the non-cured group. T2W SIR is an inflammatory sign and could demonstrate a significant difference between active and inactive Graves’ ophthalmopathy groups[17]. The levator tended to be thicker and the T2W SIR higher in the noncured group compared with the cured group, though they were not significant in the statistical analysis. Only 41 patients underwent MRI examinations before and after the treatment. A study that includes a higher number of patients could perhaps illustrate whether the T2 value and levator thickness are truly significantly different between the two groups. The patients in the non-cured group were prone to experiencing more severe immunoreactive inflammation than the cured group.And the inflammation lasted longer in the non-cured group.The injection dosage intervals and injection times were not different in this study. For these types of patients, 20 mg TA at 4-week intervals might not be sufficient to achieve normal lid positions. The intervals could be shortened, and the dosage could be raised for these patients. Further studies regarding the optimal dosage, injection volume and injection intervals should be conducted in the future.
It was observed during the MRI examinations that the levators of some patients in the ineffective group were thinner after treatment.Though edema and inflammation can be alleviated with or without treatment, the adhesion of fibrotic complications at the Müller muscle, levator and surrounding tissues occurred in the ineffective patients. Thus, the lid retraction persisted.
Although TA was used to treat patients due to its anti-inflammation effect, local glucocorticoid can lead to ptosis in some uveitis patients[18]. The pathophysiological mechanism is presumed to be its myocyte apoptosis[19]. No studies have investigated the effect of subconjunctival TA on levator or Müller muscle histopathology. It is not clear whether the injected TA induced levator or Müller muscle myopathy. Some patients suffered from lid retractions for a long period of time, and they also benefited from the treatment, which may be due to muscle myopathy.
The relapse rate of ULR has not been reported previously. It was found that 12.4% of patients suffered from a relapse of the ULR after quiescence with subconjunctival TA treatment.Trigger events for a relapse included fluctuating thyroid levels in two patients. Thyroid eye disease is known to reactivate after a variable interval of quiescence, and the recurrence rate of thyroid eye disease was 15.7%[20]. Considering the characteristics of the disease, patients should be informed of the recurrence probability and should have their eye conditions monitored regularly.
TA could be detected in the plasma with posterior subtenon TA injections[21]. The pharmacokinetics of subconjunctival TA injections have not been reported previously. Considering the rich blood vessels and the lymphatic circulation in the anterior episclera and conjunctiva, TA might be absorbed into the blood through circulation more quickly. For the patients in this study, the most commonly seen side effect was menstrual fluctuation, which might be caused by the effect of the drug on the hypothalamic-pituitary-ovarian axis or possibly by a direct effect on the ovary[22]. Subconjunctival TA could lead to a high aqueous TA level and may contribute to a higher incidence of IOP elevation after local ocular TA application[21].Of the patients in this study, 18.6% experienced elevations of IOP. The reported rate of IOP elevation with intraocular and periocular TA varies in the literature[23-24]. These patients should be monitored carefully because medically unresponsive IOP elevation might occur as late as six months following periocular TA injection[25].
There are some limitations in this study. First, this study was retrospective in nature and shares the inherent limitations of all retrospective studies. Second, there was no control group under long-term observation. Third, the number of patients who underwent MRI examinations was low due to economic limitations. The injection protocols, such as dosage and injection intervals, were the same for all patients. Further studies based on additional initial MRI examination results are mandatory to determine the optimal dosage, injection volume and injection intervals.
In conclusion, a repeated subconjunctival injection of TA is an effective and relatively safe treatment for ULR due to TAO.The levator thickness can become thinner with treatment,which might be related to the anti-inflammation effect of the medicine. Patients should be monitored regularly for recurrences and side effects.
ACKNOWLEDGEMENTS
The authors thank Duan M from Radiology Department of Peking Union Medical College Hospital for data analysis.
Foundation:Supported by the National Natural Science Foundation of China (No.81271043).
Conflicts of Interest:Xu DD, None; Chen Y, None; Xu HY,None; Li H, None; Zhang ZH, None; Liu YH, None.
REFERENCES
1 Khong JJ, McNab AA, Ebeling PR, Craig JE, Selva D. Pathogenesis of thyroid eye disease: review and update on molecular mechanisms. Br J Ophthalmol 2016;100(1):142-150.
2 Cruz AA, Ribeiro SF, Garcia DM, Akaishi PM, Pinto CT. Graves upper eyelid retraction. Surv Ophthalmol 2013;58(1):63-76.
3 Grove AS Jr. Upper eyelid retraction and Graves’ disease. Ophthalmology 1981;88(6):499-506.
4 Choi YJ, Lim HT, Lee SJ, Lee SY, Yoon JS. Assessing Graves’ophthalmopathy-specific quality of life in Korean patients. Eye (Lond)2012;26(4):544-551.
5 Costa PG, Saraiva FP, Pereira IC, Monteira ML, Matayoshi S. Comparative study of Botox injection treatment for upper eyelid retraction with 6-month follow-up in patients with thyroid eye disease in the congestive or fibrotic stage. Eye (Lond) 2009;23(4):767-773.
6 Kohn JC, Rootman DB, Liu W, Goh AS, Hwang CJ, Goldberg RA.Hyaluronic acid gel injection for upper eyelid retraction in thyroid eye disease: functional and dynamic high-resolution ultrasound evaluation.Ophthalmic Plast Reconstr Surg 2014;30(5):400-404.
7 Lee J, Lee H, Park M, Baek S. Modified full thickness graded blepharotomy for upper eyelid retraction associated with thyroid eye diseases in Ease Asians. Ann Plast Surg 2016;77(6):592-596.
8 Xu D, Liu Y, Xu H, Li H. Repeated triamcinolone acetonide injection in the treatment of upper-lid retraction in patients with thyroid-associated ophthalmopathy. Can J Ophthalmol 2012;47(1):34-41.
9 Chee E, Chee SP. Subconjunctival injection of triamcinolone in the treatment of lid retraction of patients with thyroid eye disease: a case series. Eye (Lond) 2008;22(2):311-315.
10 Lee JM, Lee H, Park M, Baek S. Subconjunctival injection of triamcinolone for the treatment of upper lid retraction associated with thyroid eye disease. J Craniofac Surg 2012;23(6):1755-1758.
11 Lee SJ, Rim TH, Jang SY, Kim CY, Shin DY, Lee EJ, Lee SY, Yoon JS. Treatment of upper eyelid retraction related to thyroid-associated ophthalmopathy using subconjunctival triamcinolone injections. Graefes Arch Clin Exp Ophthalmol 2013;251(1):261-270.
12 Hamed-Azzam S, Mukari A, Feldman I, Saliba W, Jabaly-Habib H,Briscoe D. Fornix triamcinolone injection for thyroid orbitopathy. Graefes Arch Clin Exp Ophthalmol 2015;253(5):811-816.
13 Bartley GB, Fatourechi V, Kadrmas EF, Jacobsen SJ, Ilstrup DM,Garrity JA, Gorman CA. Clinical features of Graves’ ophthalmopathy in an incidence cohort. Am J Ophthalmol 1996;121(3):284-290.
14 Hales IB, Rundle FF. Ocular changes in Graves’ disease: a long-term follow-up study. Q J Med 1960;29:113-126.
15 Kirsch E, Hammer B, von Arx G. Graves’ orbitopathy: current imaging procedures. Swiss Med Wkly 2009;139(43-44):618-623.
16 Chen Y, Jin Zy, Zhang ZH, Xu DD, Meng W, Jiang B, Fang HY, Sun ZY, Chen Y, Sun HY, Feng F. Quantitative evaluation of extraocular muscle with high-field magnetic resonance in patients with Graves’ophthalmopathy with upper-lid retraction. Zhongguo Yi Xue Ke Xue Yuan Xue Bao 2012;34(5):461-467.
17 Hu H, Xu XQ, Wu FY, Chen HH, Su GY, Shen J, Hong XN, Shi HB.Diagnosis and stage of Graves’ ophthalmopathy: efficacy of quantitative measurements of the lacrimal gland based on 3-T magnetic resonance imaging. Exp Ther Med 2016;12(2):725-729.
18 Song A, Carter KD, Nerad JA, Boldt C, Folk J. Steroid-induced ptosis:case studies and histopathologic analysis. Eye (Lond) 2008;22(4):491-495.
19 Singleton JR, Baker BL, Thorburn A. Dexamethasone inhibits insulin-like growth factor signaling and potentiates myoblast apoptosis.Endocrinology 2000;141(8):2945-2950.
20 Patel P, Khandji J, Kazim M. Recurrent thyroid eye disease. Ophthalmic Plast Reconstr Surg 2015;31(6):445-448.
21 Shen L, You Y, Sun S, Chen Y, Qu J, Cheng L. Intraocular and systemic pharmacokinetics of triamcinolone acetonide after a single 40-mg posterior subtenon application. Ophthalmology 2010;117(12):2365-2371.22 Mens JM, Nico de Wolf A, Berkhout BJ, Stam HJ. Disturbance of the menstrual pattern after local injection with triamcinolone acetonide. Ann Rheum Dis 1998;57(11):700.
23 Kim JE, Pollack JS, Miller DG, Mittra RA, Spaide RF, ISIS Study Group. ISIS-DME: a prospective, randomized, dose-escalation intravitreal steroid injection study for refractory diabetic macular edema. Retina 2008;28(5):735-740.
24 Yuksel-Elgin C, Elgin C. Intraocular pressure elevation after intravitreal triamcinolone acetonide injection: a Meta-analysis. Int J Ophthalmol 2016;9(1):139-144.
25 Kalina PH, Erie JC, Rosenbaum L. Biochemical quantification of triamcinolone in subconjunctival depots. Arch Ophthalmol 1995;113(7):867-869.
Co-first authors:Dong-Dong Xu and Yu Chen
Correspondenceto:Hui Li. Department of Ophthalmology,Peking Union Medical College Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing 100730, China. lihuipumch@163.com
Received:2017-11-29 Accepted: 2018-05-17
Abstract● AlM: To report the long-term outcomes of a large cohort of upper lid retraction patients treated with subconjunctival triamcinolone acetonide injections.● METHODS: This retrospective clinical study was conducted from 2009 to 2016. The documents of 97 patients (126 eyes) were reviewed. The patients were treated with subconjunctival triamcinolone acetonide injections monthly and evaluated pre- and post-treatment by taking measurements of the upper margin reflex distance (MRD1,the distance between the upper-lid margin and the pupil center), lid aperture, lagophthalmos and proptosis. The patients were divided into the cured group, the improved group and the ineffective group based on the final treatment effectiveness. The improved group and the ineffective group were combined into non-cured group.● RESULTS: The follow-up time was 23.45±14.86mo. Of the patients, 63 (64.9%) were assigned to the cured group, 22 (22.7%) in the improved group, 12 (12.4%) in the ineffective group. lnjection times for cured group was 4.66±1.74, and for non-cured group was 5.17±2.08(P≤0.05). The MRD1 was significantly reduced between baseline and 1mo after the initiation of treatment in the cured and improved groups (P<0.001). The values did not change significantly after 4mo for the improved group,while they continued to decrease in the cured group. ln the ineffective group, the MRD1 did not significantly change after treatment. A statistically significant difference was observed between the baseline and post-treatment values of the mean muscle thickness (2.95±0.99 mm vs 2.04±0.63 mm,P<0.05) and surface area (27.27±10.5 mm2vs 18.3±7.04 mm2,P<0.05) of the levator superioris with magnetic resonance imaging examination. Twelve patients (12.4%) relapsed after treatment and required additional subconjunctival injections. The main side effects included menstrual cycle disturbances (32%) and elevations of intra-ocular pressure(18.6%).● CONCLUSlON: A repeated subconjunctival injection of triamcinolone is an effective and relatively safe treatment for upper lid retraction due to thyroid-associated ophthalmopathy.This is related to the anti-inflammation effect of the medicine and the levator thickness can become thinner. Patients must be monitored regularly for recurrences and side effects.
● KEYWORDS:triamcinolone acetonide; thyroid associated ophthalmopathy; eyelid retraction; magnetic resonance imaging
DOl:10.18240/ijo.2018.08.07
Citation:Xu DD, Chen Y, Xu HY, Li H, Zhang ZH, Liu YH. Longterm effect of triamcinolone acetonide in the treatment of upper lid retraction with thyroid associated ophthalmopathy. Int J Ophthalmol 2018;11(8):1290-1295