Effect of intracorneal ring segment implantation on corneal asphericity
Canan A. Utine1,2, Ziya Ayhan1, Ceren Durmaz Engin1
1Department of Ophthalmology, Faculty of Medicine, Dokuz Eylul University, Izmir 35340, Turkey
2Izmir International Biomedicine and Genome Center, Dokuz Eylul University, Izmir 35340, Turkey
INTRODUCTION
Intracorneal ring segments (ICRS) have long been used for the optical rehabilitation of corneal ectasia[1-2].Experience in the ophthalmology literature has shown that ICRS implantation leads to unexpectedly high visual gain in select eyes, even though the amount of refractive correction is not significant. However, in other eyes even getting close to emmetropia does not guarantee visual satisfaction[3].
This unpredictability is due to insufficiency of lower order aberrations of the eye in exploring visual quality of the patient;whilst ICRS implantation decision and selection is currently based on them.
Corneal shape is not a perfect sphere but its central part has a stronger curvature than its periphery. Thus, corneal asphericity is the main source of spherical aberration of the eye. The corneal asphericity coefficient (i.e., Q value) has a mean value of -0.26±0.18 in human cornea (range: -0.88 to +0.50)[4]. The Q value that would decrease primary spherical aberration to nil is calculated as -0.46[5]. However same Q value, with different curvatures will result in different amount of spherical aberration and adverse effects on visual quality. Therefore,Q value changes should be evaluated in association with the keratometric values[6].
A previous study has shown that ICRS can effectively reduce the excess of prolateness in keratoconus in relation to the thickness of the ring segment, modifying the corneal shape to a more physiologic, aspheric shape[7]. Herein, we aimed to analyze the effects of ICRS implantation on corneal curvatures,corneal asphericity values and visual acuity.
SUBJECTS AND METHODS
Patients with keratoconus, pellucid marginal degeneration and high corneal astigmatism ineligible for keratorefractive surgery who admitted for optical and visual rehabilitation were assessed for possible means of visual gain. Main indication for ICRS implantation in all patients was contact lens intolerance and/or insufficient visual gain by contact lens fit. After a complete ophthalmic examination and a thorough discussion of the risks and benefits of the surgery, ICRS implantation was planned. Detailed signed informed consent was obtained from each subject before the surgery.
The preoperative and postoperative data of patients with keratoconus were analysed in this study. For the sake of patient homogeneity, patients with other indications were not included into the analysis. The study adhered to the tenets of the Declaration of Helsinki.
Surgical TechniqueThe intrastromal channels for ICRS implantation were created with the femtosecond laser device(iFS, Advanced Femtosecond laser, Abbott Laboratories Inc.Abbott Park, Illinois, USA) with a ring energy and side cut energy of 1.30 µJ. As per the KeraRing[8]2009 nomogram based on visual, refractive and topographic parameters, 1 or 2 ring segments were implanted at 75%-80% depth of the thinnest stromal thickness at the implantation site. Inner diameter of implanted ICRS was 5 mm, thicknesses were 150-300 µm and arc lengths were 90°-210°. Selection of the ICRS and implantation parameters, as well as ICRS implantation (KeraRing;Mediphacos, Belo Horizonte, Brazil) was performed by the same surgeon at Dokuz Eylul University, Department of Ophthalmology, Cornea Division (Utine CA).
The postoperative regimen included moxifloxacin 0.5%(Vigamox®, Alcon, USA) and dexamethasone 0.1% (Maxidex®,Alcon, USA) eye drops four times daily for one week.Patients were instructed to avoid rubbing the eye and to use preservative-free artificial tears frequently-sodium hyaluronate 15% (Eyestil®; SIFI, Rome, Italy).
A complete ophthalmologic examination was performed preoperatively and postoperatively at 1stweek, 1st, 3rdmonths.Changes in uncorrected and corrected distance visual acuities(UDVA and CDVA, respectively) in Snellen lines, refractive errors, mean simulated keratometry readings (i.e., SimKavg),anterior and posterior corneal asphericity coefficients (i.e.,Qantand Qpost, respectively) measured with Scheimpflug tomography (Pentacam, Oculus®, Germany) at the postoperative 3rdmonth were evaluated. Postoperative data of 1stweek and 1stmonth were not included into the analysis as final refractive and visual results are expected to be achieved after 3mo. Relationship between these parameters and number/thicknesses of implanted ICRS were analyzed retrospectively.An Excel 2016 spreadsheet was used to analyze the data.A paired t-test was used to evaluate the postoperative data in relation to the preoperative data of the patients. The relationship between the selected parameters were analyzed by Pearsons’ correlation analysis (correlation coefficient r value for the strength of the linear relationship between two variables, coefficient of determination r2value for the proportion of the variance in the dependent variable that can be explained by variation in the independent variable and related P values for statistical significance). A P value ˂0.05 was deemed statistically significant.
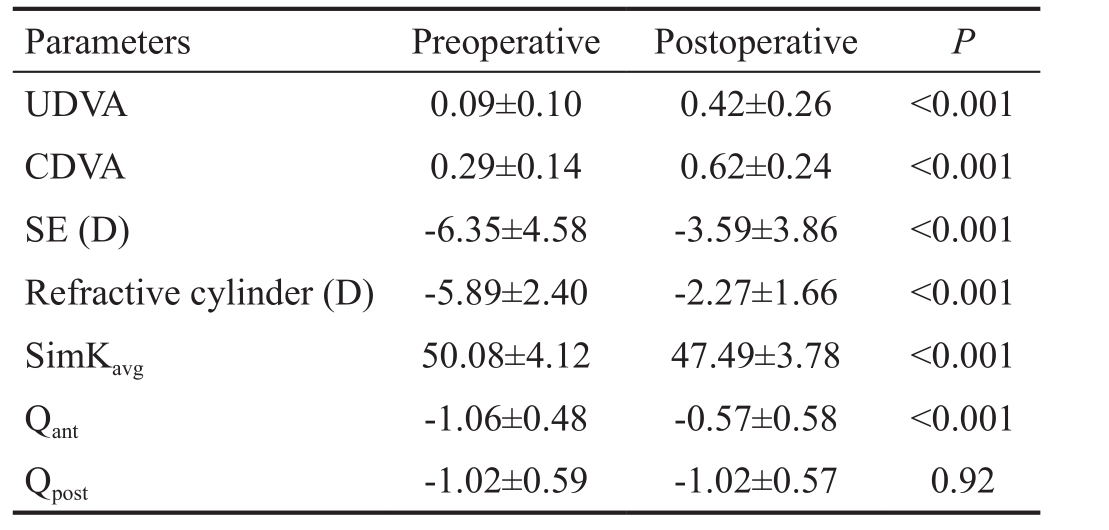
Table 1 The preoperative and postoperative visual and refractive parameters of the patients
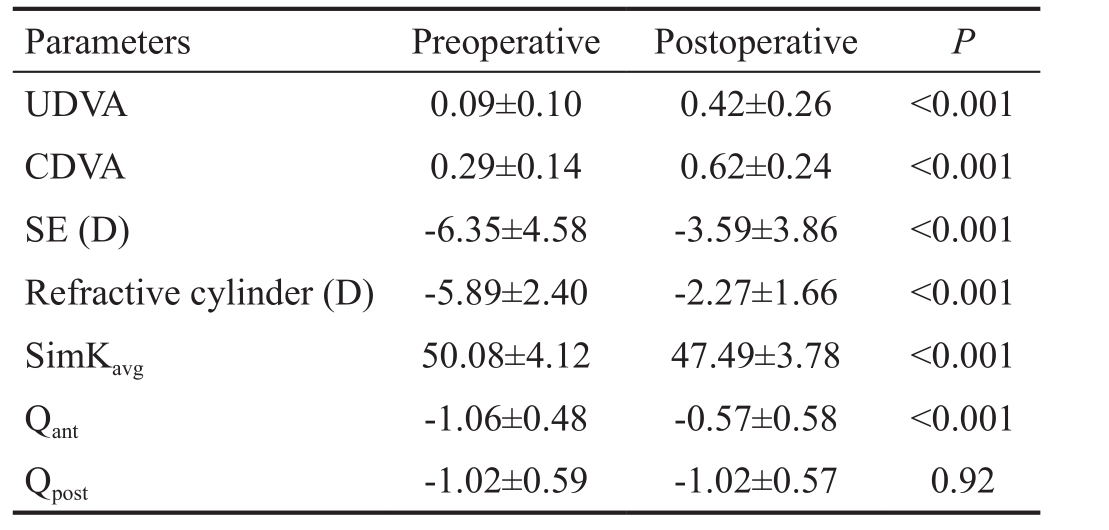
UDVA: Uncorrected distance visual acuity; CDVA: Corrected distance visual acuity; SE: Spherical equivalent; SimKavg: Average simulated keratometry reading; Qant: Q value of the anterior corneal surface; Qpost: Q value of the posterior corneal surface.
Parameters Preoperative Postoperative P UDVA 0.09±0.10 0.42±0.26 ˂0.001 CDVA 0.29±0.14 0.62±0.24 ˂0.001 SE (D) -6.35±4.58 -3.59±3.86 ˂0.001 Refractive cylinder (D) -5.89±2.40 -2.27±1.66 ˂0.001 SimKavg50.08±4.12 47.49±3.78 ˂0.001 Qant-1.06±0.48 -0.57±0.58 ˂0.001 Qpost-1.02±0.59 -1.02±0.57 0.92
RESULTS
Data of 42 eyes of 32 patients with keratoconus was retrospectively reviewed. The age of patients at the time of surgery ranged 6-51y (median: 27, mean: 28.5±9.74).There were 20 right, 22 left eyes in this cohort. The intrastromal channels were created with the following parameters:5.01±0.03 mm inner diameter, 5.71±0.03 mm outer diameter and 384.21±34.12 µm depth.
There was a significant improvement in UDVA and CDVA,along with a significant decrease in refractive spherical equivalent (SE), cylinder and SimKavgpostoperatively(P˂0.001 for all; Table 1). There was a significant increase in mean Qantfrom -1.06±0.48 towards a more physiological Q value of -0.57±0.58 postoperatively (P˂0.001) but there was no significant change in mean Qpost(P=0.92).
Postoperative values of Qantand SimKavgwere strongly dependent on their preoperative values (r=0.74, r2=0.56, P˂0.001; r=0.86,r2=0.74, P˂0.001, respectively). There was a strong negative correlation between the postoperative change in Qantand the postoperative change in SimKavg(r=-0.70, r2=0.49, P˂0.01).
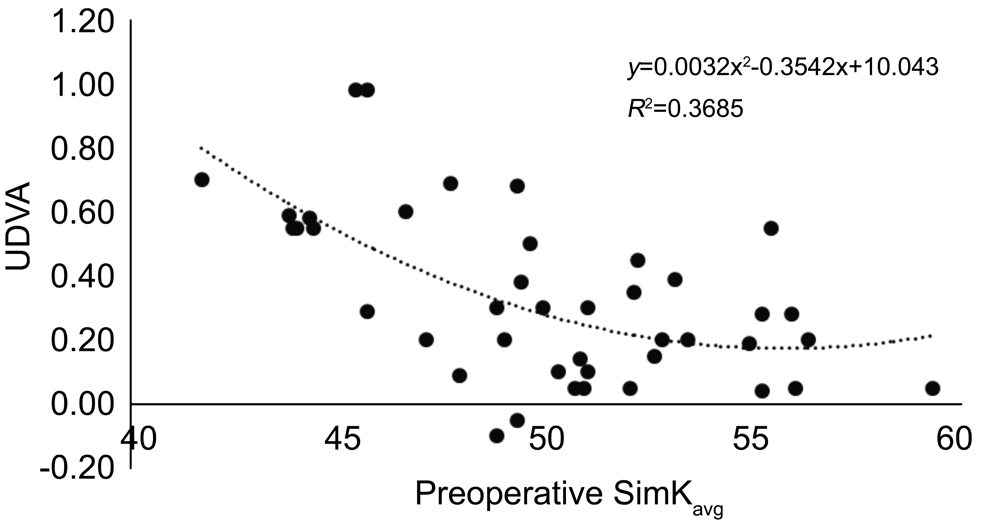
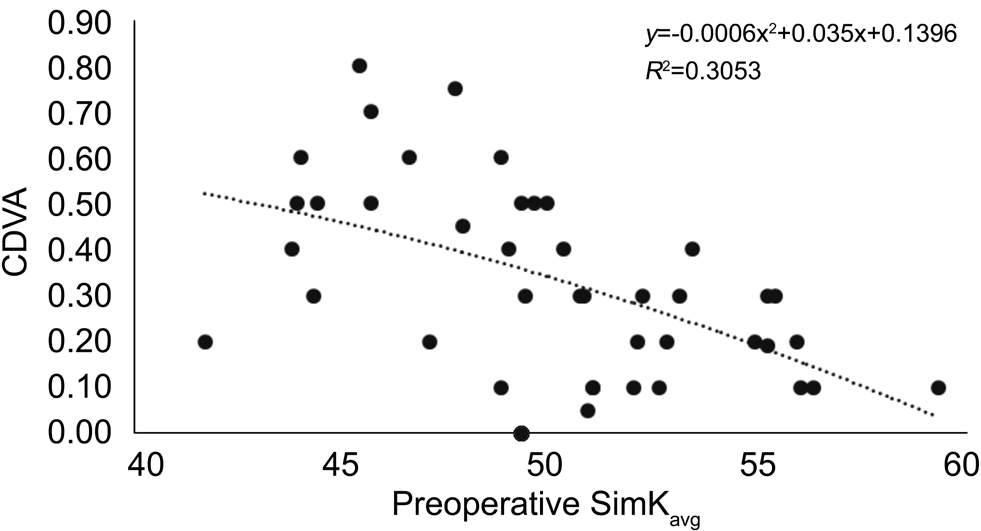
The postoperative changes in neither UDVA nor CDVA were correlated with the postoperative changes in SE and cylinder(P˃0.05 for all). There was a strong negative correlation between the postoperative changes in UDVA, CDVA and the preoperative SimKavg(r=-0.56, r2=0.31, P˂0.001; r=-0.55,r2=0.30, P˂0.001, respectively). When a polynomial regression analysis is performed, the r2values improved to 0.36 and 0.31,respectively (Figures 1, 2).
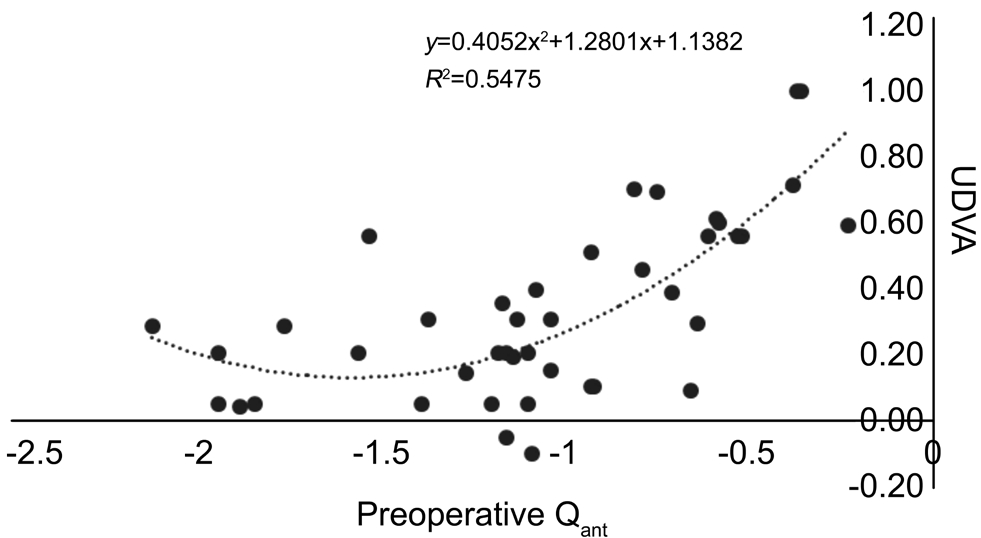
Similarly, there was a strong positive correlation between the postoperative changes in UDVA, CDVA and the preoperative Qant(r=0.62, r2=0.38, P˂0.001; r=0.54, r2=0.29, P˂0.001,respectively). When a polynomial regression analysis is performed, the r2values improved to 0.55 and 0.35,respectively (Figures 3, 4).
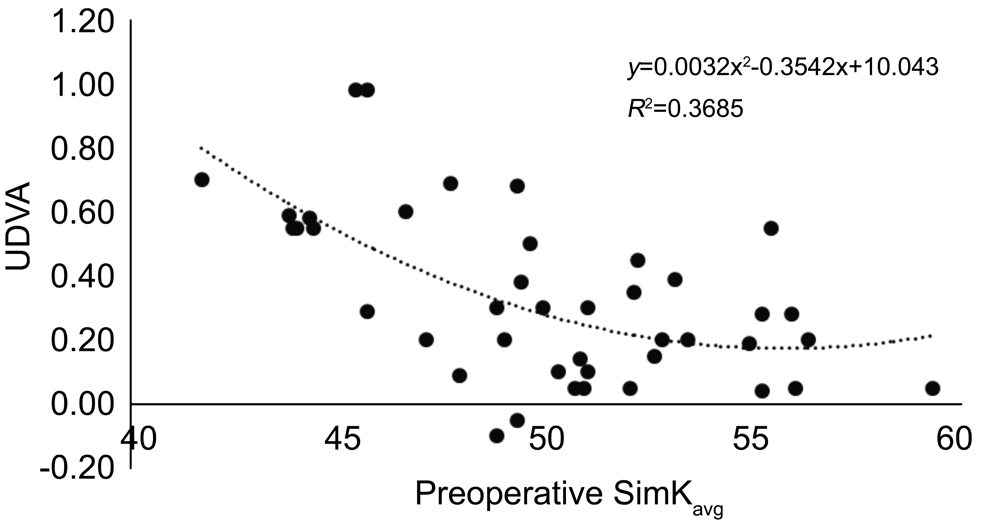
Figure 1 The correlation between preoperative SimKavgand change in UDVA.
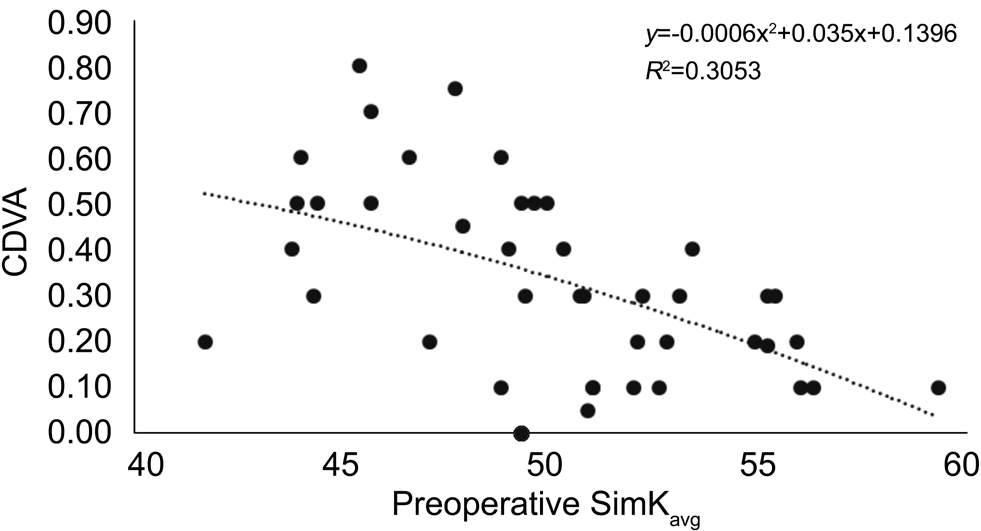
Figure 2 The correlation between preoperative SimKavgand change in CDVA.
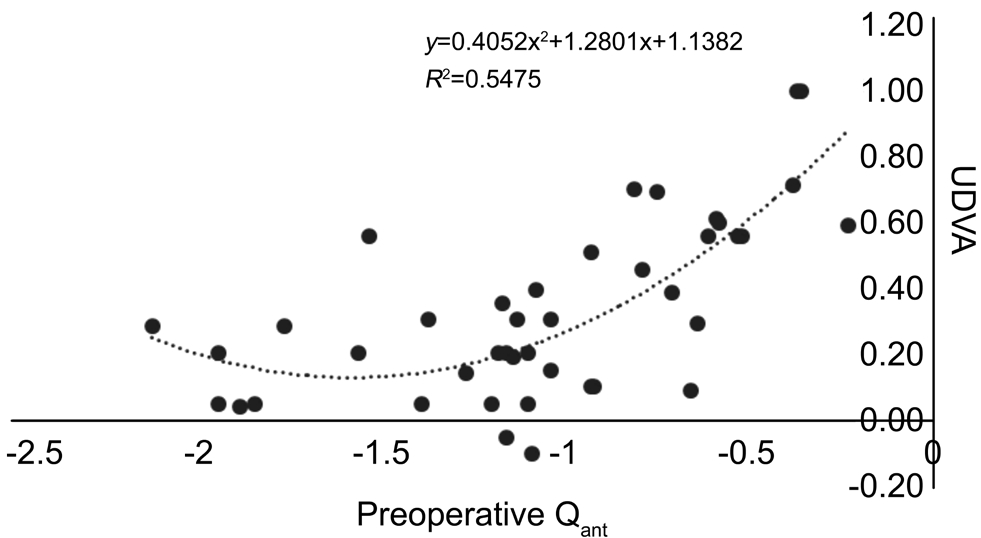
Figure 3 The correlation between preoperative Qantand change in UDVA.

Figure 4 The correlation between preoperative Qantand change in CDVA.
A negative correlation was also present between postoperative SimKavgand changes in UDVA/CDVA (r=-0.56, r2=0.31,P˂0.001; r=-0.50, r2=0.25, P˂0.001, respectively). Similarly,a positive correlation was detected between postoperative Qantand changes in UDVA/CDVA (r=0.59, r2=0.35, P˂0.001;r=0.50, r2=0.25, P˂0.01, respectively).
A significant correlation was detected neither between postoperative changes in Qantor SimKavgand average thickness of implanted ICRS; nor between postoperative changes in Qantor SimKavgand number of implanted ICRS (P˃0.05, for all).
DISCUSSION
The normal human anterior corneal surface is not spherical but rather like a conoid. The typical corneal section is a prolate ellipse, with a more curved central apex and progressive flattening towards the periphery. In the inverse profile, i.e.when the cornea is flattened in its center and becomes steeper towards the periphery, corneal shape is said to be oblate. The physiologic asphericity of the cornea shows a significant individual variation ranging from mild oblate to moderate prolate[4,9]. Q value is the unitless best fit ellipsoid (conic constant) to describe apical ratio of change and is a measure of deviation of any surface from sphere. In other words, it defines the conical shape that best fits the cone shape. Q value of an ideal spherical surface is 0.00. A prolate surface has negative,an oblate surface has positive Q value.
The shape of a surface does affect spherical aberration. The Q value that will decrease the primary spherical aberration of the eye to nil is calculated as -0.46[5]. A parabola is, on the other hand, a prolate surface that eliminates all spherical aberration and has a Q value of -0.52. The mean Q value of human cornea is known to be -0.26±0.18 (range: -0.88 to +0.50) which reduces spherical aberration by half[4,10]. For a particular Q value, increase in radius at the apex (flattening of the surface)decreases the distance to the best-fit-sphere. On the other hand,for fixed keratometric readings, as the Q value is more negative(hyperprolate cornea), the distance to the best-fit-sphere increases. As an example with an apical radius of 7.75 mm, when corneal asphericity decreases from -0.1 to -0.5, the distance to best-fit-sphere increases by 4-fold. Keratometry and Q value could be used to calculate the spherical aberration of a single refracting surface. For a corneal Q value of -0.26 and SimKavgof 44.00 D, the calculated spherical aberration is 0.18 μm[11].With equal curvature, the longitudinal spherical aberration becomes negative if the surface is more prolate than perfect Cartesian oval[9]. A hyper-prolate cornea, where peripheral rays are focused behind central rays, creates a larger depth of field; but a negative spherical aberration causes hyperopic shift in refraction. Therefore, not only the SimK readings but also the Q value determines severity of the cone and affects visual acuity.
ICRS implantation surgery has long been used for the treatment of ectatic diseases of the cornea and complies with Barraquer and Blavatskaya postulates, according to which the thickness of the addition in peripheral cornea determines the amount of flattening, and the diameter of the added ring determines how much the cornea will be flattened[12]. Postoperative outcome is a central flattening of the cornea while the periphery is displaced forward[13]. The resultant cornea is flattened at the areas corresponding to the segments extremities and making it curve at the ring’s body area[3]. Current nomograms for ICRS selection use preoperative subjective refraction, topographical keratometry and cone location data. However, postoperative surprises are not rare in terms of visual gain. The lack of correspondence between postoperative visual acuity and residual ametropia has also been observed before[3]. Similarly in this study, the postoperative changes in UDVA or CDVA were not correlated with the postoperative changes in refractive SE or cylinder (P˃0.05 for all). Thus, decrease in refractive error may not necessarily indicate visual improvement; and success of the surgery should not be evaluated by postoperative refraction, only. Indeed, basic requirements for visual gain after ICRS implantation surgery are yet to be clarified.
Given the fact that postoperative values or the amount of changes in refractive errors are not indicative of improvement in visual acuity, attention has already been turned on corneal asphericity which serves as a marker of visual quality and turning it “normal” can be a predictor of visual gain.Ferrara and Torquetti[14]have argued that in patients with significant corneal flattening after ICRS implantation without considerable improvement of UDVA and CDVA, oblate corneal shape (positive Q values) could explain the lack of visual improvement. They found a direct correlation between ring thickness and reduction of Q values, on which they built their fourth generation nomogram[14]. However, integration of this nomogram and previous one that takes cone distribution and subjective/topographic astigmatism into account, is not clear.This observation seems to be correct both for primary ectasias and for iatrogenic ectasias. Torquetti and Ferrara[15]have shown that in patients with corneal ectasia after refractive surgery,whose ablated oblate corneas have turned into prolate with the development of ectasia, mean asphericity decreased from -0.95 preoperatively to -0.23 after ICRS implantation.
In this study, the change in Qantwas correlated with the change in SimKavg(P˂0.01). Indeed, not only the preoperative values of Qantand SimKavg, but also their resultant values seem to be determinants of improvement in visual acuity.Maximum increase in UDVA and CDVA were seen in eyes with postoperative Qantof ˃-0.50. Therefore, getting close to the ideal prolate structure from a hyperprolate one seems to be beneficial for sound improvement in the visual acuity. Thus,it would be wise if one could choose ICRS parameters to aim a target Q value postoperatively. However, this approach is not merely unrealistic, but also requires development of new nomograms. Simply, as postoperative Qantand SimKavgare strongly dependent on their respective preoperative values,these parameters may be used as predictors of visual gain and aid in patient selection (Figures 1-4). It has been shown that corneal curvature and asphericity indices were the parameters best positioned to detect keratoconus progression in mild to moderate disease[16]. This is particularly important as measurement error in keratoconic eyes is significantly greater than healthy eyes, and reliable preoperative patient selection criteria are needed for surgery planning. The results of this study were in agreement with that of Torquetti et al[17]and Lyra et al[18]although they reported best correlation of visual outcomes with anterior corneal astigmatism.
Interestingly, postoperative changes in Qantor SimKavgwere correlated with neither the number nor the thicknesses of implanted segments in this study. A previous study on postlaser-assisted in situ keratomileusis ectasia patients revealed better correction of SE with two segments compared to single segment implantation; nonetheless, the level of astigmatism in the single-segment group was significantly better than that in the double-segment group[19]. In this study, we could detect no correlation with the number or thickness of implanted rings with the visually predictive topographic parameters. All implanted ICRS had the same 5.0 mm diameter, therefore a correlation with the ring diameter could not be examined. A significant correlation was only detected between the change in Qantand the change in SimKavg, each of which were strongly dependent on their preoperative values.
In a multicenter, retrospective, nonrandomized study of 611 keratoconic eyes, Vega-Estrada et al[20]have found that ICRS implantation provides significantly better results in patients with a severe form of the disease. However in that study, keratoconus grading was performed according to the degree of visual limitation, not the keratometric data.There were overlapping keratometry readings in different keratoconus severity groups. Furthermore, patients with most severe keratoconus grades had a wide range of preoperative SimKavgvalues between 38.48 D and 82.62 D. Thus, the study population was not accurately grouped in terms of corneal curvatures, which is the main parameter for ICRS segment selection. In our practice we also note that the lesser preoperative visual acuity, the greater visual gain patient achieves; but the expected visual gain decreases significantly when preoperative SimKavgvalue is greater than 55 D.
Limitations of this study include small sample size and not being able to measure corneal aberrations other than spherical aberration, as the study was conducted with the Scheimpflug tomography device Pentacam which does not provide other corneal aberrometric data.
In conclusion, ICRS implantation seem to approximate the anterior corneal asphericity of “advanced prolate” shape to “the optimal prolate” Q value of -0.52 and “spherical aberrationfree” human corneal Q value of -0.46. This improvement in corneal asphericity may have a role in improvement in UDVA and CDVA, in addition to the effect of decreased refractive cylinder. It should be kept in mind that ICRS implantation serves as the last resort for optical and visual rehabilitation before corneal transplantation surgeries, in ectatic diseases[21].If planned and performed properly, it offers a minimally invasive method for improvement in corneal asphericity and visual acuity. For this reason, further improvements on the nomograms and patient selection criteria are mandatory.
ACKNOWLEDGEMENTS
Conflicts of Interest:Utine CA, None; Ayhan Z, None;Durmaz Engin C, None.
REFERENCES
1 Kaya V, Utine CA, Karakus SH, Kavadarli I, Yilmaz OF. Refractive and visual outcomes after Intacs vs ferrara intrastromal corneal ring segment implantation for keratoconus: a comparative study. J Refract Surg 2011;27(12):907-912.
2 Cakir H, Utine CA. Combined Kerarings and Artisan/Artiflex IOLs in keratectasia. J Refract Surg 2010:1-8.
3 Guarnieri FA, Ferrara P, Torquetti L. Chapter 5: Biomechanics of Additive Surgery: Intracorneal Rings. Corneal Biomechanics and Refractive Surgery 2015:pp 73-107.
4 Kiely PM, Smith G, Carney LG. The mean shape of the human cornea.Opt Acta (Lond) 1982;29:1027-1040.
5 Manns F, Ho A, Parel JM, Culbertson W. Ablation profiles for wavefront-guided correction of myopia and primary spherical aberration.J Cataract Refract Surg 2002;28(5):766-774.
6 McDonald M. Q value or spherical aberration: Which is more important to correct? Wavefront Congress, Visual Optics Institute, 22-25 Feb 2007, Santa Fe, USA. Available at: http://voi.opt.uh.edu/VOI/WavefrontCongress/2007/presentations/42Q-factor_McDonald.pdf.
7 Torquetti L, Ferrara P. Corneal asphericity changes after implantation of intrastromal corneal ring segments in keratoconus. Emmetropia 2010;1:178-181.
8 Jorge L Alió, Alfredo Vega-Estrada, Pablo Sanz-Diez, et al. KeraRing Calculation Guidelines. 2009 version 5.2 Mediphacos Ophthalmic Professionals Inc. Available at: http://www.jaypeejournals.com/ejournals/ShowText.aspx?ID=7644&Type=FREE&TYP=TOP&IN=_eJournals/images/JPLOGO.gif&IID=583&isPDF=YES.
9 Calossi A. Corneal asphericity and spherical aberration. J Refract Surg 2007;23(5):505-514.
10 Gatinel D, Haouat M, Hoang-Xuan T. A review of mathematical descriptors of corneal asphericity. J Fr Ophtalmol 2002;25(1):81-90.
11 Beiko GHH. The fundamentals of spherical aberration. Cataract& Refractive Surgery Today Europe (CRST Europe) Bryn Mawr Communications, LLC, USA. 2012;pp 61-63. Available at: https://crstodayeurope.com/articles/2012-jul/the-fundamentals-of-sphericalaberration/.
12 Barraquer JI. Modification of refraction by means of intracorneal inclusions. Int Ophthalmol Clin 1966;6(1):53-78.
13 Piñero DP, Alio JL. Intracorneal ring segments in ectatic corneal disease-a review. Clin Exp Ophthalmol 2010;38(2):154-167.
14 Ferrara P, Torquetti L. The new Ferrara ring nomogram: The importance of corneal asphericity in ring selection. Vision Panamerica September 2010:92-95. Available at: http://www.paao.org/pdf/vpa/9.3_vpa.pdf.
15 Torquetti L, Ferrara P. Intrastromal corneal ring segment implantation for ectasia after refractive surgery. J Cataract Refract Surg 2010;36(6):986-990.
16 Guber I, McAlinden C, Majo F, Bergin C. Identifying more reliable parameters for the detection of change during the follow-up of mild to moderate keratoconus patients. Eye Vis (Lond) 2017;25:24.
17 Torquetti L, Arce C, Merayo-Lloves J, Ferrara G, Ferrara P, Signorelli B, Signorelli A. Evaluation of anterior and posterior surfaces of the cornea using a dual Scheimpflug analyzer in keratoconus patients implanted with intrastromal corneal ring segments. Int J Ophthalmol 2016;9(9):1283-1288.
18 Lyra JM, Lyra D, Ribeiro G, Torquetti L, Ferrara P, Machado A.Tomographic findings after implantation of ferrara intrastromal corneal ring segments in keratoconus. J Refract Surg 2017;33(2):110-115.
19 Hashemi H, Gholaminejad A, Amanzadeh K, Hashemi M,Khabazkhoob M. Single-segment and double-segment INTACS for post-LASIK ectasia. Acta Med Iran 2014;52(9):681-686.
20 Vega-Estrada A, Alio JL, Brenner LF, Javaloy J, Plaza Puche AB,Barraquer RI, Teus MA, Murta J, Henriques J, Uceda-Montanes A.Outcome analysis of intracorneal ring segments for the treatment of keratoconus based on visual, refractive, and aberrometric impairment. Am J Ophthalmol 2013;155(3):575-584.e1.
21 Vega-Estrada A, Alio JL. The use of intracorneal ring segments in keratoconus. Eye Vis (Lond) 2016;3:8.
Correspondenceto:Canan A. Utine. Department of Ophthalmology, Faculty of Medicine, Dokuz Eylül University,Mithatpasa cad. No:1606 Inciraltı Kampusu, Balcova 35340,Izmir, Turkey. cananutine@gmail.com
Received:2017-12-31 Accepted: 2018-04-17
Abstract● AlM: To evaluate the visual, refractive and corneal asphericity changes after intrastromal corneal ring segment (lCRS)implantation for visual rehabilitation of keratoconus.● METHODS: A total of 42 eyes of 32 patients were included.After creation of intrastromal tunnels of 5.01±0.03 mm inner diameter, 5.71±0.03 mm outer diameter and at 384.21±34.12 µm depth, 1 or 2 lCRS of 150-300 µm thickness and 90°-210° arc length were implanted. Changes in uncorrected distance visual acuity (UDVA), corrected distance visual acuity(CDVA), refractive errors, mean simulated keratometry readings (SimKavg), anterior and posterior corneal asphericity values (Qantand Qpost, respectively) measured with Scheimpflug topography were evaluated retrospectively.● RESULTS: There was a significant improvement in UDVA and CDVA, along with a significant decrease in refractive spherical equivalent (SE), cylinder and SimKavgpostoperatively (P<0.001 for all). Mean Qantincreased from-1.06±0.48 to -0.57±0.58 postoperatively (P<0.001). Change in mean Qpostwas insignificant (P=0.92). Postoperative changes in UDVA and CDVA were not correlated with the postoperative changes in SE and cylinder (P>0.05 for all);but were correlated with the preoperative SimKavgand Qantvalues (P<0.001 for all).● CONCLUSlON: lCRS implantation seems to approximate the anterior corneal asphericity of “advanced prolate”shape to “optimal prolate” shape and an “ideal Q value” of-0.46; which may have a role in improved UDVA and CDVA postoperatively, besides decreased refractive cylinder values.
● KEYWORDS:cornea ectasia; corneal asphericity; intracorneal ring segments; keratoconus; Q value
DOl:10.18240/ijo.2018.08.09
Citation:Utine CA, Ayhan Z, Durmaz Engin C. Effect of intracorneal ring segment implantation on corneal asphericity. Int J Ophthalmol 2018;11(8):1303-1307