Differences in energy and corneal endothelium between femtosecond laser-assisted and conventional cataract surgeries: prospective, intraindividual, randomized controlled trial
Lucia Bascaran1, Txomin Alberdi1, Itziar Martinez-Soroa1, Cristina Sarasqueta2, Javier Mendicute1
1Ophthalmology Department, Donostia University Hospital,San Sebastián 20014, Spain
2Biodonostia Institute, Donostia University Hospital, San Sebastián 20014, Spain
INTRODUCTION
The social, physical and economic impact of cataract is important in the industrialized world, where the highest cataract surgery rates are found and patients seek surgery at earlier stages. As patients search for higher expections of surgical experience and postoperative visual and refractive results,the pressure on the surgeon is significantly increased[1]. The latest improvements in cataract surgery have aimed to reduce iatrogenic effects on the eye, minimize complication rates and improve refractive outcomes. Femtosecond lasers have been introduced to assist cataract surgery providing increased precision and reproducibility of anterior capsulotomy[2-3], better wound architecture[4], reduced ultrasound power[2,4], mean effective phacoemulsification time (EPT) and mean phaco energy[1]. Decreased collateral tissue damage[5]and anterior chamber manipulation[6], as well as better corrected distance visual acuity (CDVA) 6mo after surgery[1]have also been related to during femtosecond laser-assisted cataract surgery (FLACS).Despite a growing number of publications, conclusions of recent Meta-analysis on the effect of FLACS on endothelial cell density and cumulative dissipated energy (CDE) are not consistent. Early Meta-analysis[1]found conflicting results regarding endothelial cell count depending on the follow-up periods at which the results were analyzed. More recently,Popovic et al[7]concluded there were no significant differences in endothelial cell count between techniques. However,these authors[1,7]also found that FLACS allowed for lower endothelial cell loss. The most recent Meta-analysis on endothelial cell loss has shown there is no significant difference between both techniques[8]. Similarly, while Popovic et al[7]conclude there are no differences in CDE between techniques,Chen et al[9]have found FLACS to decrease the need of CDE.To our knowledge, despite cell morphology is a reliable indicator of endothelial damage, there are no publications regarding the effect of FLACS on endothelial cell morphology.Similarly, little has been reported on torsional energy and fluid requirements during conventional phacoemulsification (CP)when using fracture techniques and FLACS. The contribution of this research aims to provide further evidence with regards to controversial issues such as endothelial cell loss and CDE. It is also the only endothelial morphologic analysis published to date.The objective of this paper was to prospectively compare endothelial cell density after FLACS and CP in an intraindividual study. Secondary objectives of this study aimed to evaluate the effect of FLACS in surgical efficiency and endothelium morphology.
SUBJECTS AND METHODS
A prospective single-centre intraindividual non-blinded,randomized, controlled trial was designed and approved by the Local Ethics Committee. The study conformed to the Declaration of of Helsinki and all patients signed an informed consent prior to participation. Surgeries took place between November 2013 and January 2015 in the Ophthalmology Department of the Hospital Universitario Donostia (San Sebastián, Spain). Registry number: ISRCTN24007865.
SubjectsOne hundred patients with visually significant bilateral cataract were recruited. Inclusion and exlusion criteria were the following. Inclusion criteria: patients over 50y of age with bilateral cataract. Exclusion criteria included previous ophthalmic surgery or ophthalmic pathology such as glaucoma, irregular astigmatism, keratoconus,corneal scarring, any type of ocular inflammatory disease,amblyopia, age-related macular disease (ARMD), intraocular tumours, pseudoexfoliation syndrome, any condition which contraindicated intraocular lens implantation in the capsular bag or intraoperative complications. Patients with poorly dilating pupils (pupil size in midriasis ≤6 mm) were not considered.For sample size calculation we estimated a preoperative cell count of 2300 cells/mm2[10]. We assumed a 5% difference between groups with mean postoperative cell counts of 2200 in FLACS and 2100 in CP and a standard deviation (SD) of 200.For a power of 90% and expected loss of 5%, the sample size required was 90 experimental units per group.
After signature of the informed consent, epidemiologic data were recorded and a complete ophthalmological examination including optic biometry (IOL Master 500, Carl Zeiss Meditec, Germany), noncontact computer-assisted specular microscope (SP-3000, Topcon Europe), pachymetry (TMS-5,Tomey, Nagoya, Japan), uncorrected and best corrected visual acuity (UCVA and BCVA; EDTRS Charts) and refraction was performed. Cataract was graded according to the Lens Opacities Classification System III (LOCS III). Grading was performed by a certified ophthalmologist (Bascaran L) using a BQ 900 slit lamp (Haag Streit) at maximum illumination without light filtering.
Within one month of the preoperative visit, cataract surgery was performed on the first eye. Surgical technique (FLACS or CP) was randomized using computer randomization[11]and one week later the fellow eye was operated with the technique that had not been performed on the first eye.
Standard dilation protocol was applied as follows: phenylephrine 10%, diclofenac 1 mg/mL and cyclopentolate 1%, 2 eyedrops each at 30min and 20min before surgery. All surgeries were performed under topical anesthesia (2 drops of 5% lidocaine in conjunctival sac each 5min for 15min previous to surgery)and patients underwent systemic sedation (midazolam 0.02-0.04 mg/kg and lorazepam 1 mg 30min before surgery) in all cases. Preoperative disinfection of eyelids and periorbital skin was performed with 10% povidone and 1 drop of 5% povidone was instiled into conjuntival sac before and after surgery. BSS Plus™ (Alcon, Fortworth, Texas, USA) was used as irrigating solution in all cases. All surgeries were performed by the same experienced surgeon (Mendicute J).
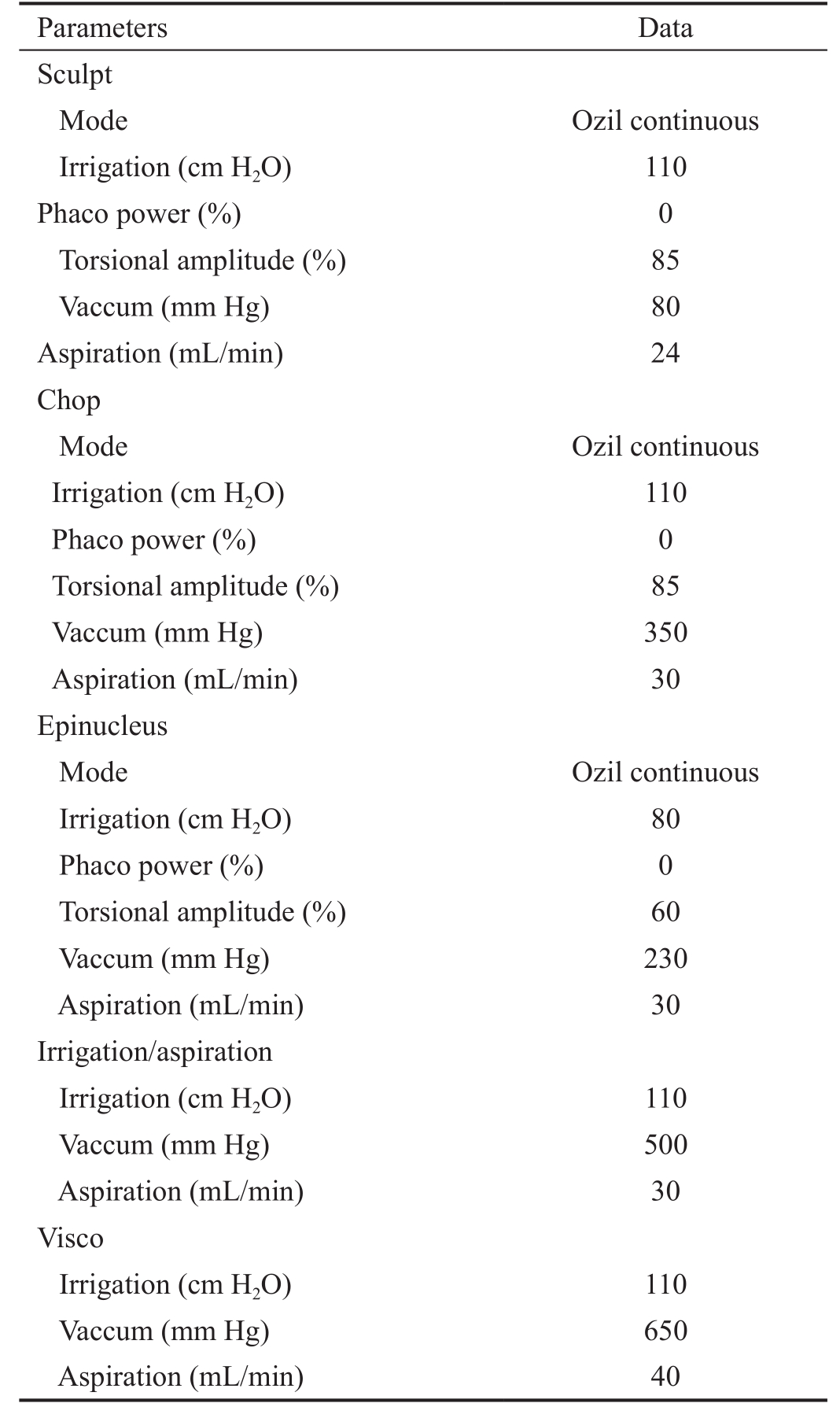
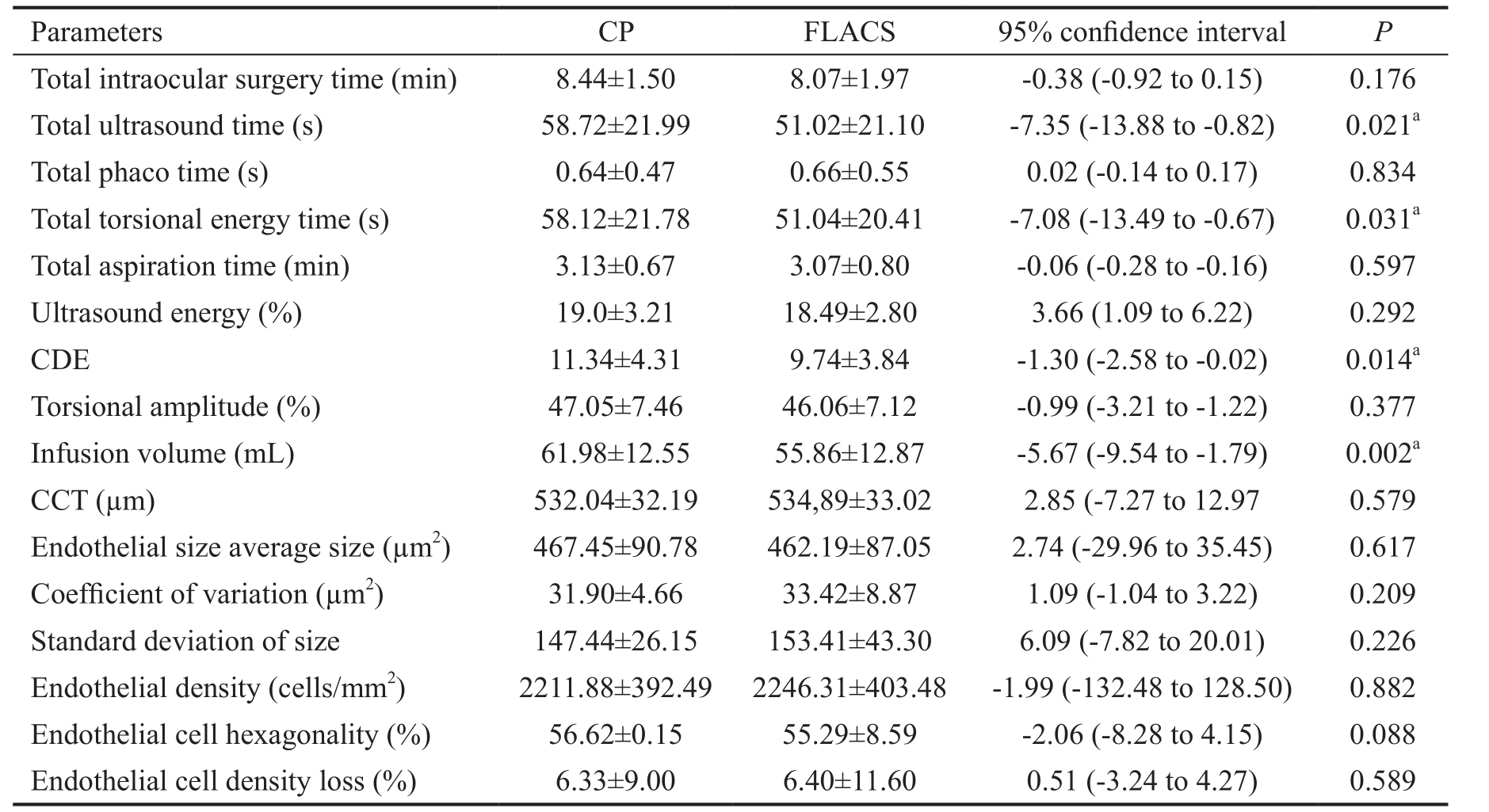
Conventional PhacoemulsificationPhacoemulsification was performed using the Infinity®Vision System (Alcon, Fortworth,Texas, USA). Phacoemulsification settings (Table 1) were the same at all times. After opening a 2.2 mm temporal clear corneal incision, 0.1 mL of intracameral 1% lidocaine was injected. The anterior chamber was then occupied with 1.2%sodium hyaluronate (Amvisc, Bausch+Lomb, Rochester, NY,USA). Ophthalmic viscosurgical device (OVD) and a continuous curvilinear capsulorhexis was created with a cystotome needle and forceps. After slight removal of OVD, hydrodissection and hydrodelineation followed. Phacoemulsification was performed with a Kelman 45º angled tip using phaco-stop and chop technique.
Femtosecond Laser Assisted Cataract SurgeryFLACS was performed using the Victus®Femtosecond Laser Platform(software version: Victus SW V2.7 SP 03) (Bausch+Lomb Technolas, Rochester, New York, USA), located in the same operating room where phacoemulsification took place. After the 5.0 mm femtosecond laser capsulotomy and nuclear fragmentation had been completed, the patient was moved from the femtosecond laser platform bed into the operative bed. Thesame laser settings for capsulotomy and nuclear fragmentation were used in all cases (Table 2). Nuclear fragmentation pattern had been optimized by the surgeon (Mendicute J) before the beginning of this trial. The two central rings with 4 radial cuts fragmentation pattern can be seen in Figure 1. The anterior chamber was filled with the same OVD and the capsulorexis removed with forceps. Phacoemulsification of the central cylinder was performed first and nuclear quadrant separation followed. These quadrants were then phacoemulsified (same parameters shown in Table 1) in and aspirated.
Table 1 Infinity®vision system settings
Parameters Data Sculpt Mode Ozil continuous Irrigation (cm H2O) 110 Phaco power (%) 0 Torsional amplitude (%) 85 Vaccum (mm Hg) 80 Aspiration (mL/min) 24 Chop Mode Ozil continuous Irrigation (cm H2O) 110 Phaco power (%) 0 Torsional amplitude (%) 85 Vaccum (mm Hg) 350 Aspiration (mL/min) 30 Epinucleus Mode Ozil continuous Irrigation (cm H2O) 80 Phaco power (%) 0 Torsional amplitude (%) 60 Vaccum (mm Hg) 230 Aspiration (mL/min) 30 Irrigation/aspiration Irrigation (cm H2O) 110 Vaccum (mm Hg) 500 Aspiration (mL/min) 30 Visco Irrigation (cm H2O) 110 Vaccum (mm Hg) 650 Aspiration (mL/min) 40
In both groups, after nuclear fragments had been phacoemulsified,cortex was aspirated with a coaxial tip. The capsular bag was then inflated with OVD and a foldable hydrophobic acrylic monofocal intraocular lens (enVista, Bausch+Lomb, Rochester,NY, USA) was implanted into the capsular bag. OVD was completely removed and prophylactic 0.1 mL of intracameral cefuroxime (1 mg/0.1 mL) injected into the anterior chamber.

Figure 1 Femtosecond laser nuclear fragmentation pattern.
Table 2 Capsulotomy and lens fragmentation femtosecond laser settings

Parameters Data Capsulotomy Energy 7200 nJ Spot spacing 6 µm Line spacing 4 µm Lens fragmentation Data Combination Radials and circulars Energy 8200 nJ Spot spacing 10 µm Line spacing 10 µm Radial cuts No. of radials 4 Radial outer diameter 6000 µm Circular cuts No. of circulars 2 Circular outer diameter 2000 µm
The 6-month Postoperative VisitFor endothelium evaluation three images of the endothelium were taken at each visit.The one with the highest quality was selected for analysis.Endothelial analysis in an area of 0.25×0.5-mm2of the central corneal endothelium was performed automatically by a noncontact computer-assisted specular microscope (SP-3000,Topcon Europe), after cell border identification was supervised and corrected, if necessary, by an experience operator(Bascaran L). Central corneal thickness (CCT) measurements were obtained with Scheimpflug imaging of the anterior segment (TMS-5, Tomey, Nagoya, Japan). Endothelial cell loss percentage was calculated using the following formula:loss of endothelial cells (%)= (endothelial cell count preopendothelial cell count postop)/endothelial cell count preop.
Outcome MeasuresIntraoperative measurements included total intraocular surgery time, total ultrasound time, total phacoemulsification time, total torsional energy time, total aspiration time, ultrasound energy, CDE, torsional amplitude and volume of fluid used during surgery. Total intraocular surgery time was timed by an observer. It accounts for the time lapse between the first paracentesis was performed and the hydration of the last corneal wound. All other parameters are provided by the Infinity phacoemulsification device as part of its final parameter summary.
Postoperative recorded parameters for analysis included:endothelial cell density (cells/mm2), average cell area (μm2),SD of size, polymegetism [coefficient of variation (CV)],plemorphism (% of hexagonal cells), cell size distribution and CCT.
Statistical AnalysisStatistical analysis was performed with the SPSS version 21 (SPSS, Inc., Chicago, IL, USA). A t-test is used to compare sample means. Pearson’s Chi-squared test was used to analyze the difference in cataract nucleus hardness. A P value of less than 0.05 was considered statistically significant.
RESULTS
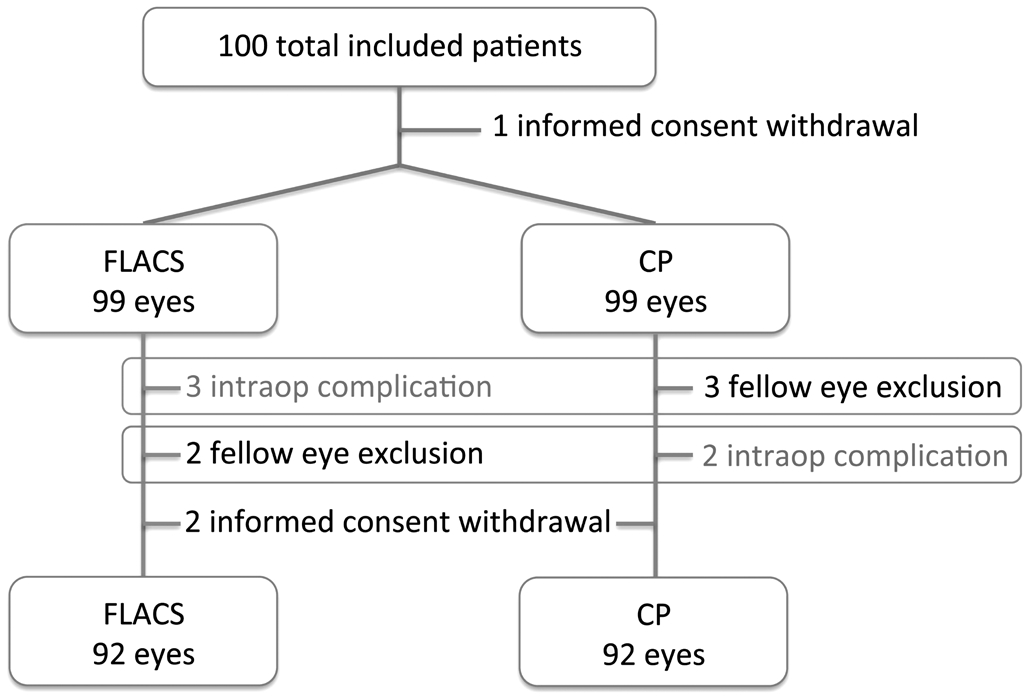
From the one hundred included patients (200 eyes), the following issues arised (Figure 2). Three patients withdrew informed consent: one patient withdrew consent before surgery and two inmediately after second eye surgery.Five intraoperative complications were registered and five postoperative adverse events were reported.
The five intraoperative complications occurred in five different patients: three posterior capsular rupture without vitreous loss were registered (2 CP and 1 FLACS), an anterior capsular tear with posterior expansion and nucleus drop that required pars plana vitrectomy (FLACS) and one eye in which FLACS could not be performed because of docking problems(femtosecond laser platform bed calibration incidence). Both eyes of these patients were excluded from analysis. From the five complications described, there were no permanent vision loss or serious ocular complications. The three posterior capsular ruptures achieved BCVA of 0.00 logMAR one month after surgery. The patient with anterior radial tear and nuclear drop required pars plana vitrectomy which was performed the same day. This patient achieved UCVA of 0.00 logMAR one month after surgery and routine cataract surgery on the fellow eye followed. The patient in which docking could not be performed underwent uneventful CP surgery.
The five postoperative adverse events (three patients) were reported 3mo after surgery. One patient presented with bilateral Irvine-Gass syndrome, the second patient presented with bilateral adenoviral conjunctivitis and the third presented central vein occlusion in one eye (CP group). All of these patients exited the study at the time of presentation of the adverse events and were treated to the best of our knowledge by sub-specialists of the department. Data from these 3 patients was analyzed until the presentation of the adverse event.
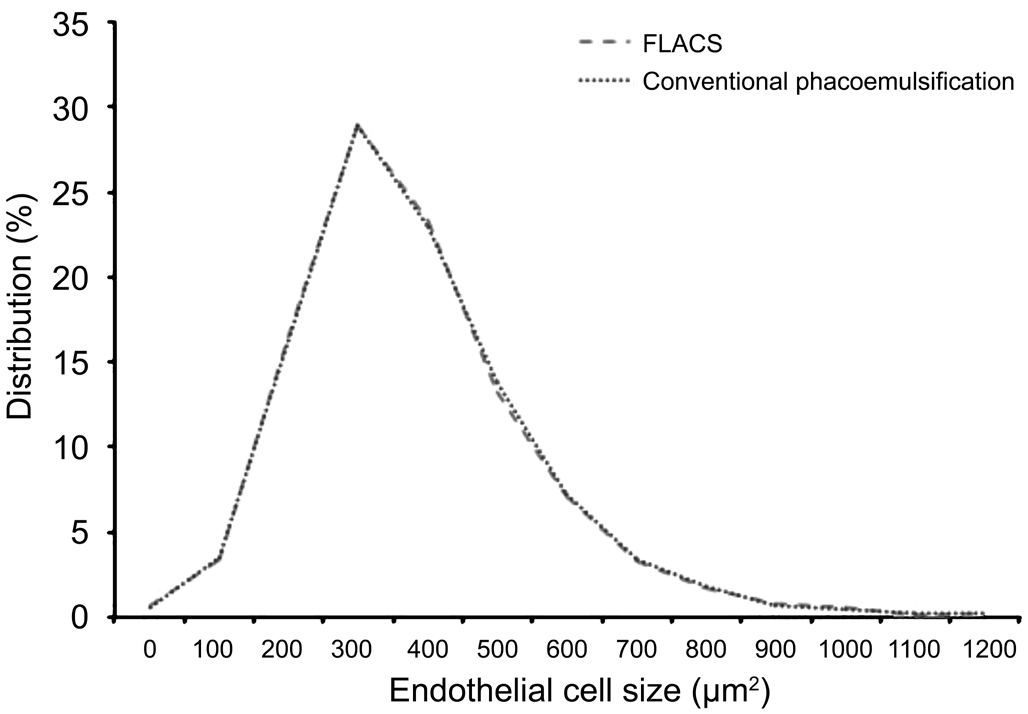
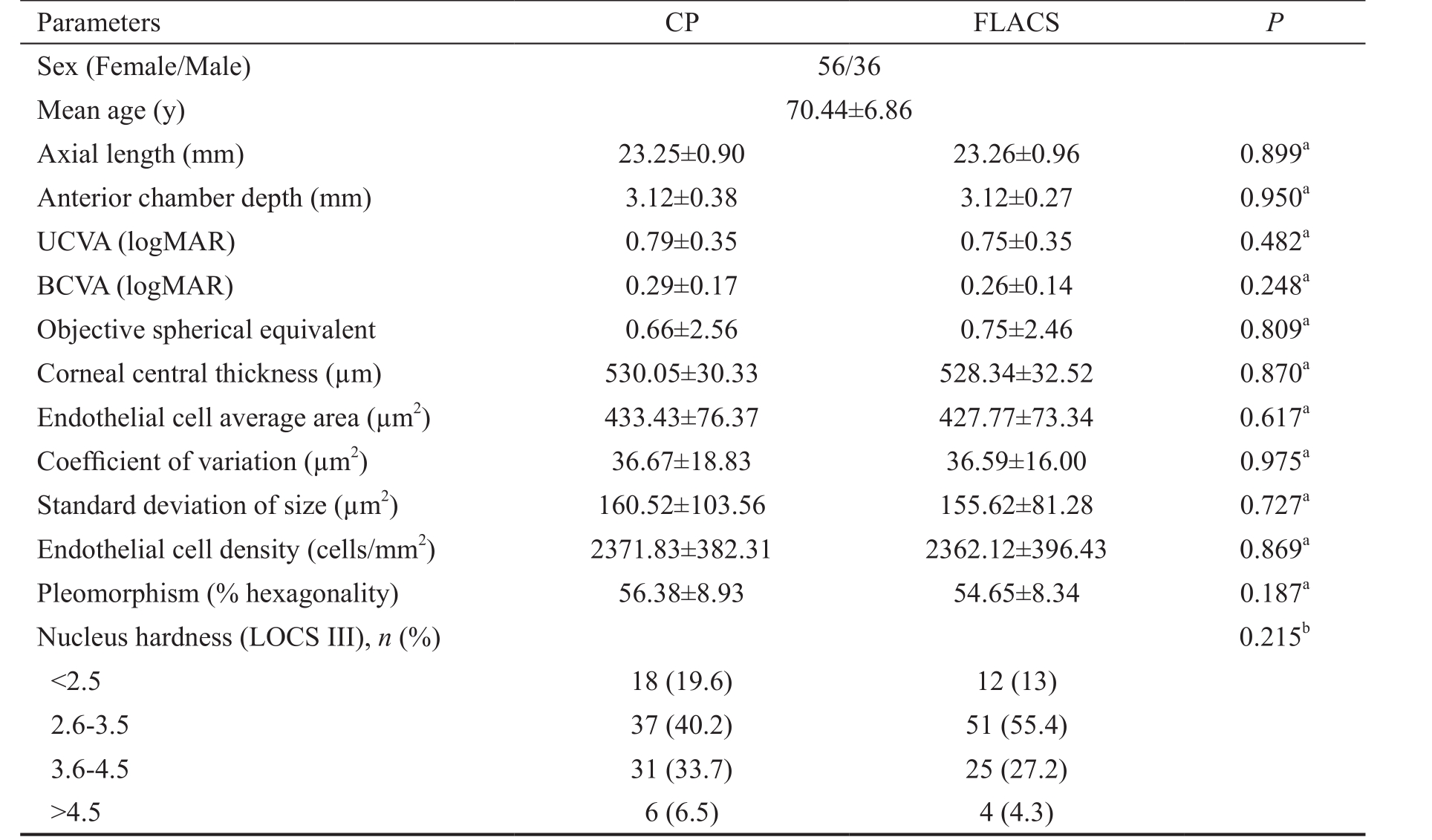
Fifty-six of the included patients were female and 36 were male. Mean age was 70.44±6.86y. There were no preoperative significant differences between groups in biometric characteristics, endothelial condition or nuclear hardness (P˃0.05; Table 3). Preoperative endothelial cell size distribution between groups was not statistically significant(Figure 3).
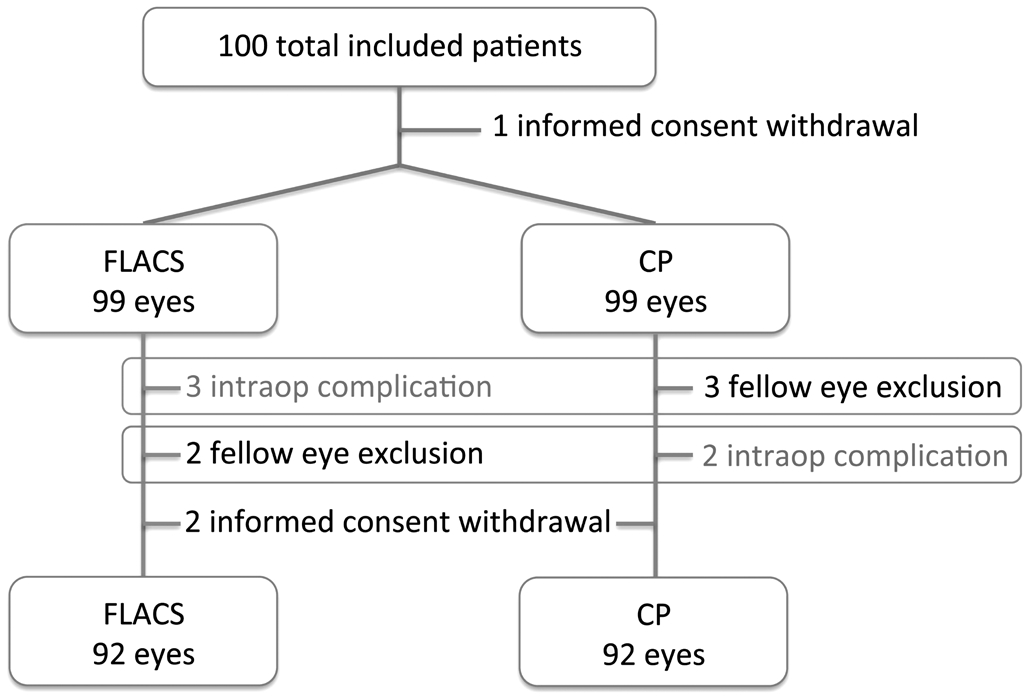
Figure 2 Flow chart showing the selection and inclusion of study subjects.
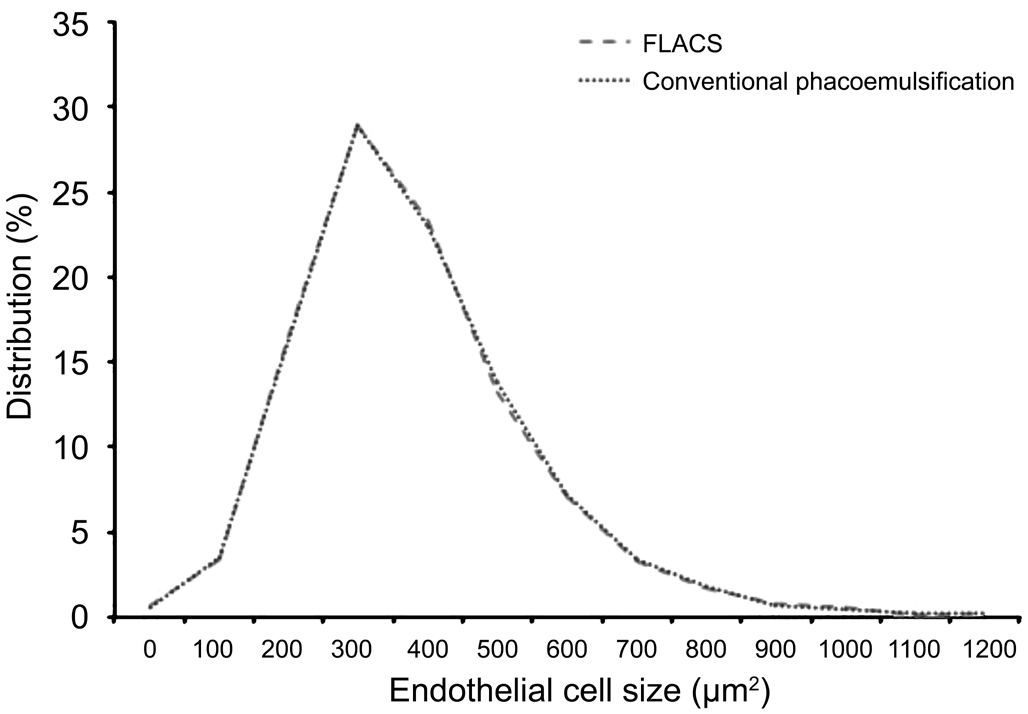
Figure 3 Preoperative endothelial cell distribution.
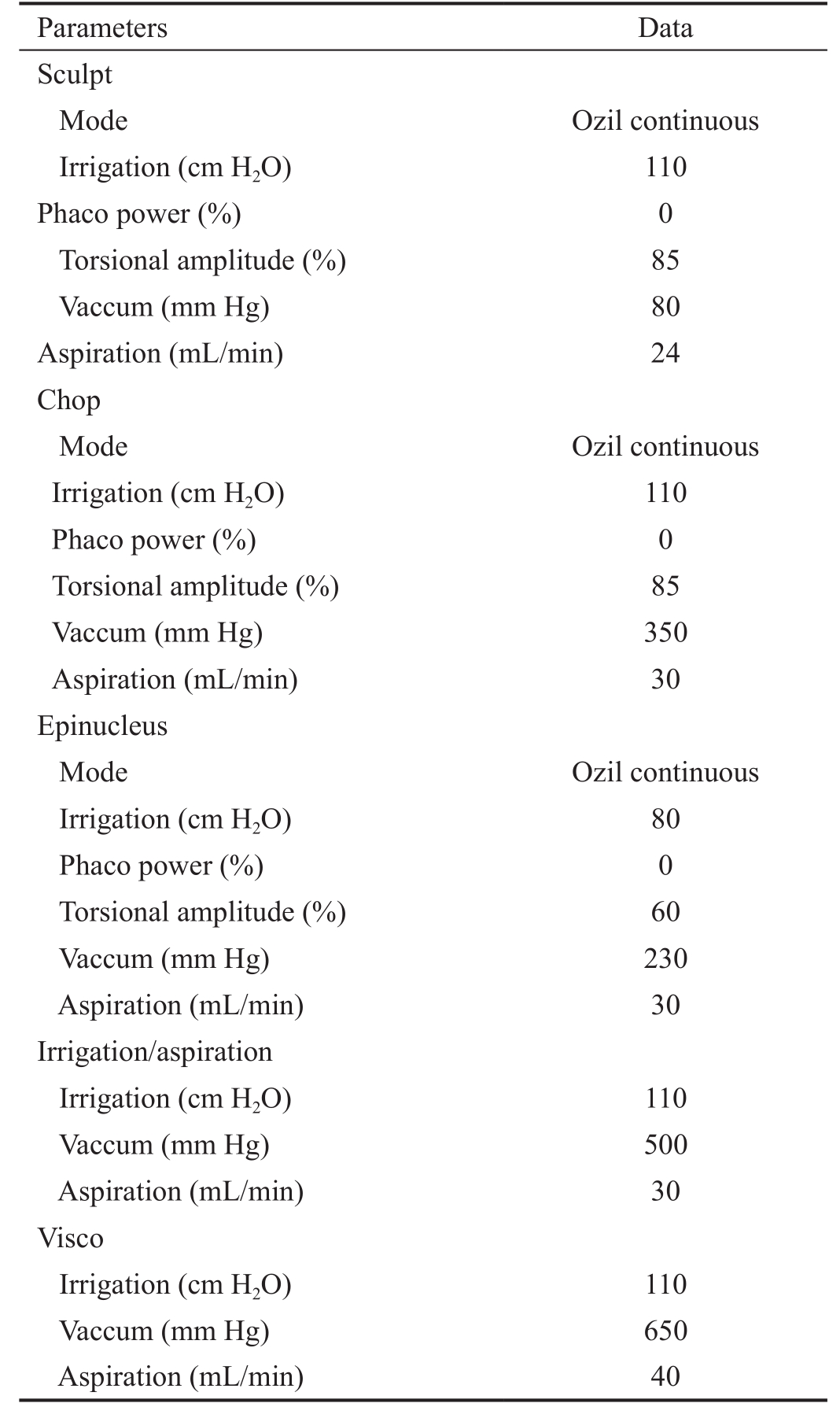
Table 4 shows the results (mean±SD, estimated effect size and confidence interval) for the recorded parameters. FLACS required statistically significant lower total ultrasound time,total torsional energy time, CDE and infusion volumes(P˂0.05). There were no significant differences between techniques in intraocular surgery time. Differences in endothelial analysis parameters were not statistically significant(P˃0.05). No differences were noted in CCT, endothelial cell average size, endothelial cell SD in size, CV, hexagonality,endothelial cell density or endothelial cell density loss between groups at this visit.
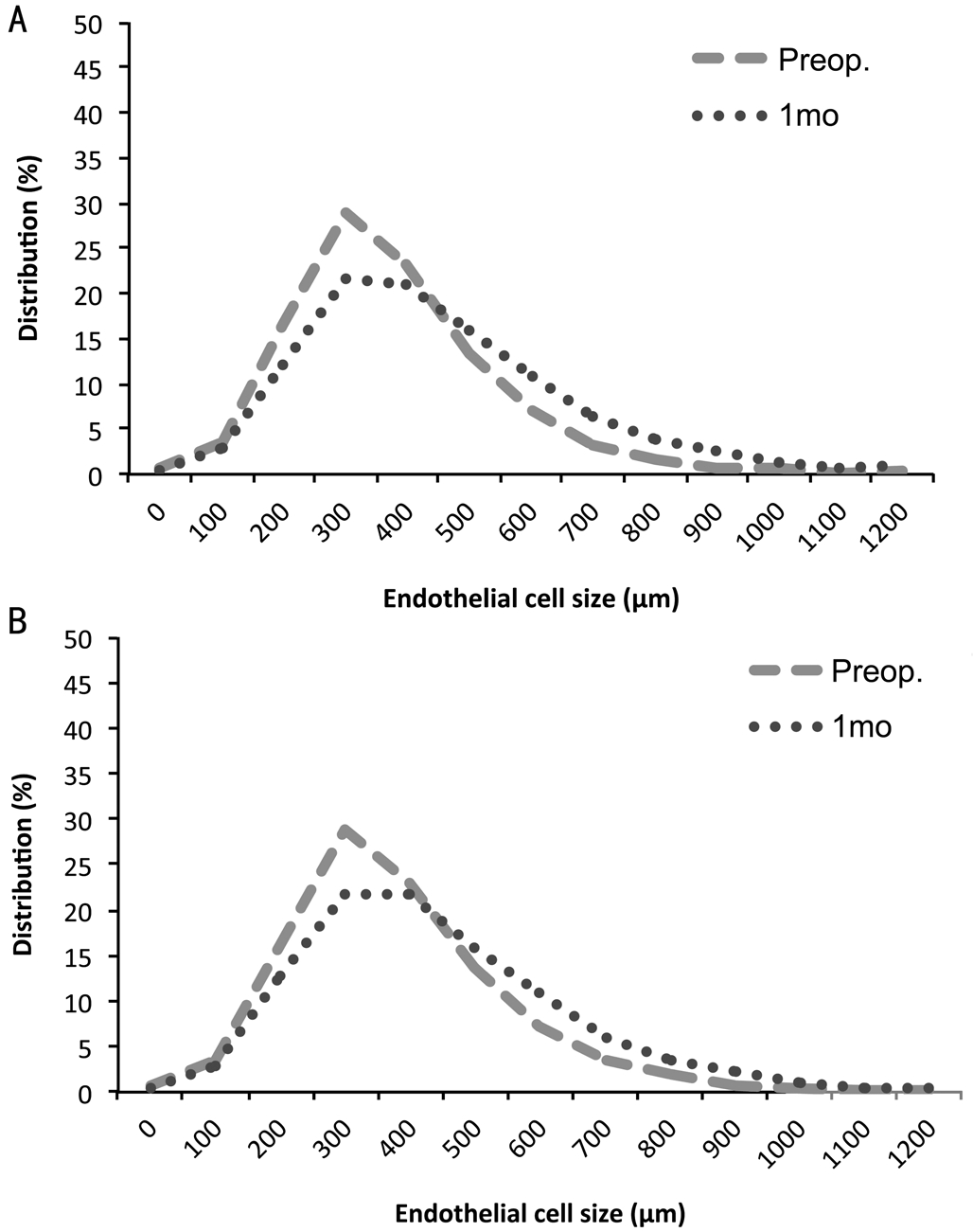
Figure 4 represents pre and postoperative endothelial cell distribution in both groups. Differences in endothelial cell size distribution between the pre and postoperative visits were statistically significant in both groups (P˂0.05) but there was no significant difference in the change of cell size distribution between groups (P˃0.10).
DISCUSSION
Our results showed FLACS significantly reduced CDE,torsional energy time and mean total ultrasound (P˂0.05).Mean total longitudinal ultrasound time was less than 1s in both groups and differences were not statistically significant.We also found that in this series, FLACS significantly reduced(P˂0.05) in about 9% the mean irrigating solution volume needed to perform cataract surgery. However, although mean intraocular surgery time is shorter in FLACS than in CP, the difference between groups is not statistically significant. In this study, the endothelial analysis did not reflect the energy savings reported. There were no significant differenes between groups in endothelial cell density. We did not find significant differences between the two groups in CCT or endothelial cell density loss either. There was no difference in endothelial cell morphologic analysis between groups in cell area, SD of cell area, CV and cell hexagonality. Similarly, the change in cell size distribution after surgery in both groups was not statistically significant.
Table 3 Preoperative group data n=92, mean±SD
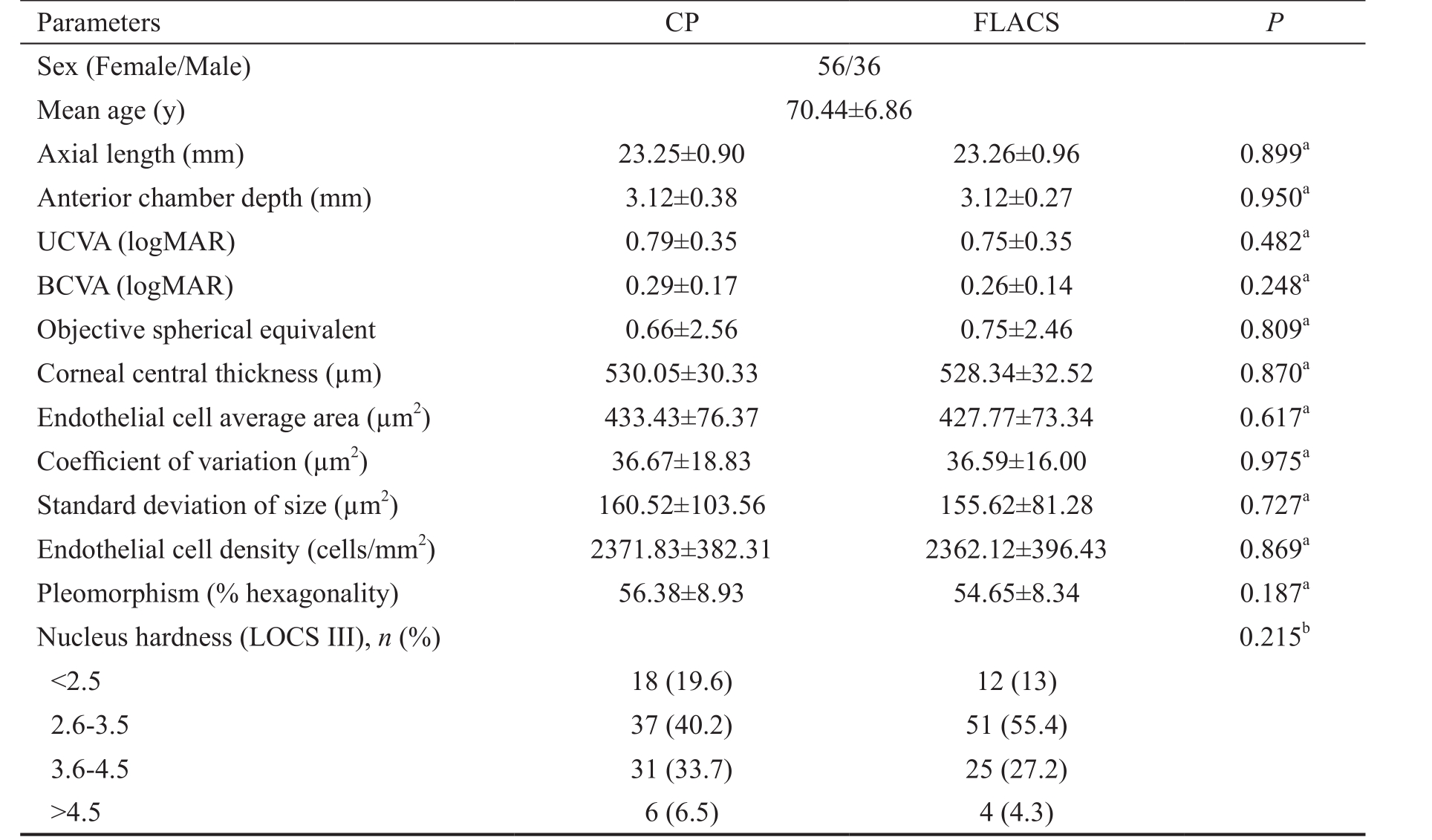
UCVA: Uncorrected visual acuity; BCVA: Best corrected visual acuity; CP: Conventional phacoemulsification; FLACS:Femtosecond laser-assisted cataract surgery.aThe t-test;bChi-squared test.
Parameters CP FLACS P Sex (Female/Male) 56/36 Mean age (y) 70.44±6.86 Axial length (mm) 23.25±0.90 23.26±0.96 0.899aAnterior chamber depth (mm) 3.12±0.38 3.12±0.27 0.950aUCVA (logMAR) 0.79±0.35 0.75±0.35 0.482aBCVA (logMAR) 0.29±0.17 0.26±0.14 0.248aObjective spherical equivalent 0.66±2.56 0.75±2.46 0.809aCorneal central thickness (µm) 530.05±30.33 528.34±32.52 0.870aEndothelial cell average area (µm2) 433.43±76.37 427.77±73.34 0.617aCoefficient of variation (µm2) 36.67±18.83 36.59±16.00 0.975aStandard deviation of size (µm2) 160.52±103.56 155.62±81.28 0.727aEndothelial cell density (cells/mm2) 2371.83±382.31 2362.12±396.43 0.869aPleomorphism (% hexagonality) 56.38±8.93 54.65±8.34 0.187aNucleus hardness (LOCS III), n (%) 0.215b<2.5 18 (19.6) 12 (13)2.6-3.5 37 (40.2) 51 (55.4)3.6-4.5 31 (33.7) 25 (27.2)>4.5 6 (6.5) 4 (4.3)
Table 4 Results for the recorded parameters mean±SD
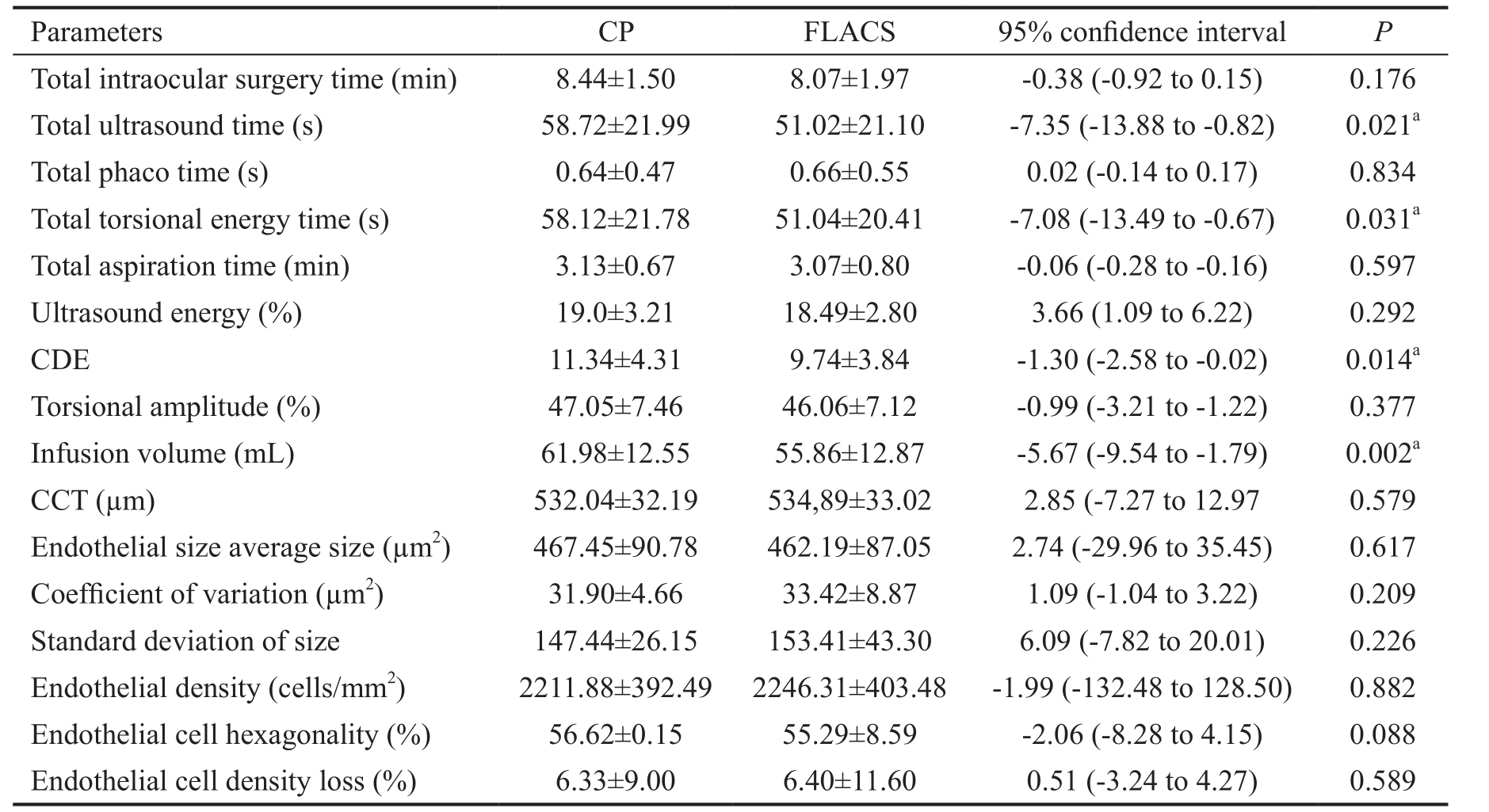
CDE: Cumulative dissipated energy; CCT: Central corneal thickness; CP: Conventional phacoemulsification; FLACS:Femtosecond laser-assisted cataract surgery.aStatistically significant.
Parameters CP FLACS 95% confidence interval P Total intraocular surgery time (min) 8.44±1.50 8.07±1.97 -0.38 (-0.92 to 0.15) 0.176 Total ultrasound time (s) 58.72±21.99 51.02±21.10 -7.35 (-13.88 to -0.82) 0.021aTotal phaco time (s) 0.64±0.47 0.66±0.55 0.02 (-0.14 to 0.17) 0.834 Total torsional energy time (s) 58.12±21.78 51.04±20.41 -7.08 (-13.49 to -0.67) 0.031aTotal aspiration time (min) 3.13±0.67 3.07±0.80 -0.06 (-0.28 to -0.16) 0.597 Ultrasound energy (%) 19.0±3.21 18.49±2.80 3.66 (1.09 to 6.22) 0.292 CDE 11.34±4.31 9.74±3.84 -1.30 (-2.58 to -0.02) 0.014aTorsional amplitude (%) 47.05±7.46 46.06±7.12 -0.99 (-3.21 to -1.22) 0.377 Infusion volume (mL) 61.98±12.55 55.86±12.87 -5.67 (-9.54 to -1.79) 0.002aCCT (µm) 532.04±32.19 534,89±33.02 2.85 (-7.27 to 12.97 0.579 Endothelial size average size (µm2) 467.45±90.78 462.19±87.05 2.74 (-29.96 to 35.45) 0.617 Coefficient of variation (µm2) 31.90±4.66 33.42±8.87 1.09 (-1.04 to 3.22) 0.209 Standard deviation of size 147.44±26.15 153.41±43.30 6.09 (-7.82 to 20.01) 0.226 Endothelial density (cells/mm2) 2211.88±392.49 2246.31±403.48 -1.99 (-132.48 to 128.50) 0.882 Endothelial cell hexagonality (%) 56.62±0.15 55.29±8.59 -2.06 (-8.28 to 4.15) 0.088 Endothelial cell density loss (%) 6.33±9.00 6.40±11.60 0.51 (-3.24 to 4.27) 0.589
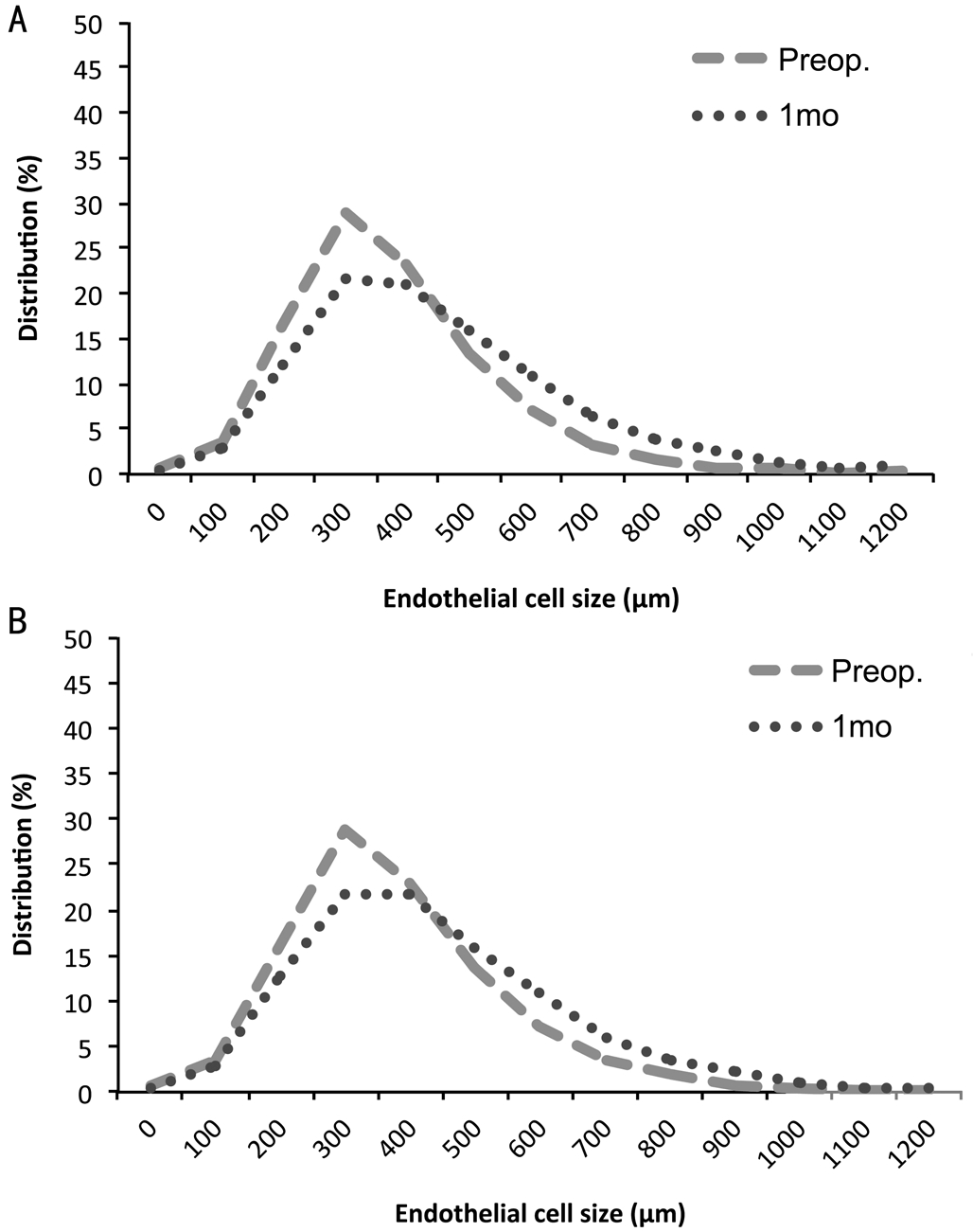
Figure 4 Endothelial cell distribution change A: FLACS; B: CP.
FLACS avoids the need for capsulorhexis and fragmentation and the development of this technology has been aimed to increase surgical efficiency. Higher values of CDE are related with longer surgical and recovery times while lower CDE values may correlate with more efficient surgery[12]. Despite comparing this FLACS to an experienced surgeon in fracture techniques, FLACS would still be expected to improve efficiency and the reduction we observed in CDE, torsional energy time and mean total ultrasound add further evidence to the already available. On a broader analysis, we recorded the irrigation solution volume used, since an excessive volume of intraoperative irrigation solution could increase of hydrodynamic flow and turbulence in the anterior chamber potentially damaging endothelial cells[13]. We believe this reduction in the volume of irrigation solution required can be explained by the pre-fragmentation of the nucleus, that avoids the need of manipulation (with associated wound leakage)and ineffective phacoemulsification of the nucleus fragments.Despite shorter intraocular surgery times that have been observed with FLACS, the difference between groups has not been statistically significant. We found that the femtosecond cuts through the anterior cortex fibres when performing the capsulorhexis made the aspiration of cortex more laborious and time consuming in FLACS. We cannot rule out, however, that the small sample size of our study might hinder hypothetical statistical significance if larger samples were considered.
Ultrasound and fluid dynamic energy have been found to have the worst effect on ocular structures[14]. Ultrasound time has been related to the pathogenesis of endothelial cell loss[15]and different groups have implicated greater infusion volumes as an independent predictors of endothelial cell loss during cataract surgery[16-17]. Since our results showed a significant improvement in surgical efficiency, we would have expected decreased endothelial damage signs in the FLACS group.However, no differences in endothelial cell count or any other endothelial evaluation parameter were found. Various hypothesis may be put forward: fracture phacoemulsification techniques are very evolved and are difficult to beat in standard cataract surgeries, endothelial reponse to surgical aggresion during the first 6mo covers for small undetected differences in the early postoperative period or the relatively low sample on which this paper bases its conclusions might not show differences that could potentially be significant with an increase in sample size.
With regards to surgical parameters, our results are in line with previous publications. Our results support the findings of the only other publication we have found in which torsional energy time was specifically analysed[18], where a reduction of torsional energy in FLACS is found, and previous publications[19-20]in which significant reductions in mean ultrasound times when pretreating cataract with femtosecond laser were reported. Reddy et al[21]were the only to conclude there were no significant differences in mean ultrasound time between groups. Theirs, however, was a multisurgeon trial in which femtosecond laser fragmentation patterns, phacoemulsification settings, surgeon technique and experience were not controlled and depended on each surgeon.
In terms of surgical efficiency, EPT or CDE are usually considered. EPT comparison between different platforms is difficult and controversial[22]because of differences in calculating algorithms, but most publications have found a significant decrease in EPT when performing FLACS compared to CP[19-21,23-25]. Despite some authors not having found statistical differences between techniques[26-28], available Meta-analysis agree that FLACS is related with a lower EPT[1,7,9]. However, Meta-analysis conclusions with regards to CDE are dissent. While Popovic et al[7]found no evidence of lower CDE in FLACS, Chen et al[9]concluded there is lower CDE in FLACS. This inconsistency shows the need for more studies in order to draw consistent conclusions. Our results add further evidence, supporting those papers who found FLACS is related to a significant CDE reduction when compared to CP[18,29-30]. Recently, Yesilirmak et al[31]demonstrated CDE could be further reduced by using an active-fluidics phacoemulsification torsional platform.
Only two authors have analysed the use of fluids during cataract surgery and they have not found significant differences between groups[21,32]. We believe that although sample sizes and study designs differ, the difference in our results with those from previous authors might be related to surgical technique and nuclear fragmentation patterns. The posible effect of intracameral cefuroxime on the corneal endothelium has also been raised[33]. In this study, both groups received 0.1 mL; of intracameral cefuroxime (1 mg/0.1 mL) at the end of surgery, eliminating hypothetical bias. Most publications on this matter, however, conclude its use is safe for the corneal endothelium[34-35], even in vulnerable tissues[36].
Some authors have reported longer intraocular surgery time in FLACS[37]but other groups report similar times between groups[30]. Like us, none of them have found the differences between groups in intraocular surgery times to be statistically significant. Available results are not enough to draw evidencebased conclusions on this matter. Larger series of experienced FLACS surgeons are still needed.
The most commonly considered parameters to analyze effect of FLACS on endothelium include CCT, endothelial cell density and endothelial cell density loss. In our series, we did not find significant differences between groups in any of these three parameters. The effect FLACS may have in endothelial cell loss remains uncertain, as publications show controversial results in the early-mid postoperative period. Endothelial cell loss in FLACS in the early postoperative period (up until 1mo postop) seems to be significantly lower than CP[18,38-39], but some groups failed to demonstrate statistical significance[27-28,40].Long term effect of FLACS on endothelial cell loss is still under discussion. Some authors find a significant reduction in endothelial cell loss three months after FLACS[14], while other groups[28,30,41]did not find significant differences in their series.According to the few available publications with 6mo followup periods, there are no significant differences in endothelial cell loss between techniques[18,28,38]. Meta-analysis conclusions on the effect of FLACS on CCT vary. Some relate FLACS with lower CCT[7,9], others do not find significant differences other than one day after surgery[1].
Morphologic analysis of endothelial cells has been considered a better indicator of endothelial damage[42]. Endothelial cells have been described to enlarge when endothelial damage occurs. If this happens, an increase in cell area and a decrease in endothelial cell density, as well as an increase in the coefficient of variation and a loss in hexagonality are expected. This is, to our knowledge, the only paper to perform a complete morphologic analysis of the corneal endothelium after FLACS and compare to CP. There is only one other publication[30]that considers hexagonality in their analysis when comparing FLACS and CP. The authors did not find any difference between groups one day and three months after surgery in hexagonality cell loss. The importance of morphologic analysis of the endothelium is that the sole consideration of CCT and endothelial density excludes other important aspects of endothelial condition. According to our results, we cannot conclude FLACS made a significant difference, the long-term effect of FLACS on the corneal endothelium being comparable to that after CP. Larger sample sized studies and improvements in imaging techniques and analysis software would be interesting in order to determine the effect of FLACS on endothelium.
There are some limitations in this study. With regards to study design, it is a non-blinded study with a low sample size.Follow-up has been set 6mo after surgery, but longer followups with early postoperative study points (1mo, 3mo) would give us a more detailed picture of what is happening with the endothelial cells. Also, there has been a recent update in the Victus®femtosecond laser platform. For this clinical trial,the same fragmentation pattern was used in all cases with independence of cataract grading because of limitations in the femtosecond laser software available at that time. As newer software updates appear, different fragmentation patterns become available and therefore higher optimization may be obtained. Since ultrasound requirements not only depend on nuclear grading results on the LOCS III scale[43], but also on the grid pattern used for lens fragmentation[19], more intensive fragmentation patterns in denser cataracts would probably help lower ultrasound requirements. Reliability on specular microscopes for endothelial cell analysis has also been questioned. It is true that available analysis systems have technical limitations that might bias and distort results, but continuous improvements in software analysis allow for higher precision analysis. Finally, it has been recently published that changes in intraocular pressure have transient effects on the endothelial cell structure and function in animals[44]. Although we have not found papers showing evidence of something similar happening in human endothelium, the potential effect of intraocular pressure changes during and after surgery on the endothelial cell analysis during the postoperative period has not been considered in this study.
In conclusion, this paper provides evidence on a controversial topic: the effect of FLACS on endothelial cell density.Although theory suggests FLACS should be less harmful to endothelial cells, available publications up until now fail to show consistent evidence. We hope our paper will help to define the real effect of FLACS on the endothelium. It is also the only series to perform a complete morphologic analysis on endothelium damage comparing FLACS and CP. Its analysis of torsional energy and CDE support limited previous evidence and it is the largest to consider the effect of FLACS on infusion volume. Debate might arise on where the perfect equilibria might stand. Smaller grid sizes will reduce ultrasound requirements but may be related to higher femtosecond laser exposures and higher irrigation solution volume necessities.On the other hand, prefragmentation of the nucleus into larger pieces reduces femtosecond laser exposure and the irrigating fluid volume but will compromise CDE reduction. Further analysis with larger samples, longer follow-up periods and controlled designs of the effect of each parameter on the eye's tissues, with special attention to their clinical relevance, are still necessary.
ACKNOWLEDGEMENTS
Authors’ contributions:Bascaran L: Concept and design,data collection, analysis and interpretation of data, writing the manuscript, administrative, technical or material support;Alberdi T: Concept and design, critical revision of the manuscript, statistical expertise, supervision; Martinez-Soroa I: Analysis and interpretation of data, critical revision of the manuscript; Sarasqueta C: Analysis and interpretation of data, critical revision of the manuscript, statistical expertise;Mendicute J: Concept and design, analysis and interpretation of data, critical revision of the manuscript, statistical expertise,administrative, technical or material support, supervision.
Conflicts of Interest:Bascaran L, None; Alberdi T, None;Martinez-Soroa I, None; Sarasqueta C, None; Mendicute J is consultant for Alcon, provides research support for Alcon,Acufocus, Bausch+Lomb, Medicem, Novagali, Zeiss and is part of the speakers bureau for Alcon and Bausch+Lomb.
REFERENCES
1 Chen X, Xiao W, Ye S, Chen W, Liu Y. Efficacy and safety of femtosecond laser-assisted cataract surgery versus conventional phacoemulsification for cataract: a meta-analysis of randomized controlled trials. Sci Rep Aug 2013;5:13123.
2 Nagy ZZ, Kranitz K, Takacs AI, Mihaltz K, Kovacs I, Knorz MC.Comparison of intraocular lens decentration parameters after femtosecond and manual capsulotomies. J Refract Surg 2011;27(8):564-569.
3 Mastropasqua L, Toto L, Calienno R, Mattei PA, Mastropasqua A,Vecchiarino L, Di Iorio D. Scanning electron microscopy evaluation of capsulorhexis in femtosecond laser-assisted cataract surgery. J Cataract Refract Surg 2013;39(10):1581-1586.
4 Palanker DV, Blumenkranz MS, Andersen D, Wiltberger M, Marcellino G, Gooding P, Angeley D, Schuele G, Woodley B, Simoneau M, Friedman NJ, Seibel B, Batlle J, Feliz R, Talamo J, Culbertson W. Femtosecond laser-assisted cataract surgery with integrated optical coherence tomography. Sci Transl Med 2010;2(58):58ra85.
5 Sugar A. Ultrafast femtosecond laser refractive surgery. Curr Opin Ophthalmol 2002;13(4):246-249.
6 Hatch KM, Talamo JH. Laser-assisted cataract surgery: benefits and barriers. Curr Opin Ophthalmol 2014;25(1):54-61.
7 Popovic M, Campos-Möller X, Schlenker MB, Ahmed II. Efficacy and safety of femtosecond laser-assisted cataract surgery compared with manual cataract surgery: a meta-analysis of 14 567 eyes. Ophthalmology 2016;123(10):2113-2126.
8 Ye Z, Li Z, He S. A meta-analysis comparing postoperative complications and outcomes of femtosecond laser-assisted cataract surgery versus conventional phacoemulsification for cataract. J Ophthalmol 2017;2017:3849152.
9 Chen X, Chen K, He J, Yao K. Comparing the curative effects between femtosecond laser-assisted cataract surgery and conventional phacoemulsification surgery: a meta-analysis. PLoS One 2016;11(3): e0152088.
10 Galgauskas S, Norvydaitė D, Krasauskaitė D, Stech S, Ašoklis RS.Age-related changes in corneal thickness and endothelial characteristics.Clin Interv Aging 2013;8:1445-1450.
11 Urbaniak GC, Plous S. (2007) Research Randomizer (Version 3.0).Computer Software. http://www.randomizer.org/.
12 Chen M, Chen M. Comparison of CDE data in phacoemulsification between an open hospital-based ambulatory surgical center and a freestanding ambulatory surgical center. Clin Ophthalmol 2010;4:1287-1289.
13 Millá E, Vergés C, Ciprés M. Corneal endothelium evaluation after phacoemulsification with continuous anterior chamber infusion. Cornea 2005;24(3):278-282.
14 Fishkind W, Bakewell B, Donnenfeld ED, Rose AD, Watkins LA,Olson RJ. Comparative clinical trial of ultrasound phacoemulsification with and without the WhiteStar system. J Cataract Refract Surg 2006;32(1):45-49.
15 Dick HB, Kohen T, Jacobi FK, Jacobi KW. Long-term endothelial cell loss following phacoemulsification through a temporal clear corneal incision. J Cataract Refract Surg 1996;22(1):63-67.
16 Hayashi K, Hayashi H, Nakao F, Hayashi F. Risk factors for corneal endothelial injury during phacoemulsification. J Cataract Refract Surg 1996;22(8):1079-1084.
17 Mahdy MA, Eid MZ, Mohammed MA, Hafez A, Bhatia J. Relationship between endothelial cell loss and microcoaxial phacoemulsification parameters in noncomplicated cataract surgery. Clin Ophthalmol 2012;6:503-510.
18 Mastropasqua L, Toto L, Mastropasqua A, Vecchiarino L, Mastropasqua R, Pedrotti E, Di Nicola M. Femtosecond laser versus manual clear corneal incision in cataract surgery. J Refract Surg 2014;30(1):27-33.
19 Conrad-Hengerer I, Hengerer FH, Schultz T, Dick HB. Effect of femtosecond laser fragmentation of the nucleus with different softening grid sizes on effective phaco time in cataract surgery. J Cataract Refract Surg 2012;38(11):1888-1894.
20 Daya SM, Nanavaty MA, Espinosa-Lagana MM. Translenticular hydrodissection, lens fragmentation, and influence on ultrasound power in femtosecond laser-assisted cataract surgery and refractive lens exchange.J Cataract Refract Surg 2014;40(1):37-43.
21 Reddy KP, Kandulla J, Auffarth GU. Effectiveness and safety of femtosecond laser-asssited lens fragmentation and anterior capsulotomy versus the manual technique in cataract surgery. J Cataract Refract Surg 2013;39(9):1297-1306.
22 Packer M, Solomon JD. Letters to the editor: impact of crystalline lens opacification on effective phacoemulsification time in femtosecond laserassisted cataract surgery. Am J Ophthalmol 2014;157(2):426-432.e1.
23 Abell RG, Kerr NM, Vote BJ. Femtosecond laser-assisted cataract surgery compared with conventional cataract surgery. Clin Exp Ophthalmol 2013;41(5):455-462.
24 Abell RG, Kerr NM, Vote BJ. Toward zero effective phacoemulsification time using femtosecond laser pretreatment. Ophthalmology 2013;120(5):942-948.
25 Conrad-Hengerer I, Hengerer FH, Schultz T, Dick HB. Effect of femtosecond laser fragmentation on effective phacoemulsification time in cataract surgery. J Refract Surg 2012;28(12):879-883.
26 Ecsedy M, Mihaltz K, Kovacs I, Takacs A, Filkorn T, Nagy ZZ. Effect of femtosecond laser cataract surgery on the macula. J Refract Surg 2011;27(10):717-722.
27 Takacs AI, Kovacs I, Mihaltz K, Filkorn T, Knorz MC, Nagy ZZ.Central corneal volume and endothelial cell count following femtosecond laser-assisted refractive cataract surgery compared to conventional phacoemulsification. J Refract Surg 2012;28(6):387-391.
28 Mursch-Edlmayr AS, Bolz M, Luft N, Ring M, Kreutzer T, Ortner C, Rohleder M, Priglinger SG. Intraindividual comparison between femtosecond laser-assisted and conventional cataract surgery. J Cataract Refract Surg 2017;43(2):215-222.
29 Chen H, Lin H, Chen W, Zhang B, Xiang W, Li J, Chen W, Liu Y.Femtosecond laser combined with non-chopping rotation phacoemulsification technique for soft-nucleus cataract surgery: a prospective study. Sci Rep 2016;6:18684.
30 Krarup T, Holm LM, La Cour M, Kjaerbo H. Endothelial cell loss and refractive predictability in femtosecond laser-assisted cataract surgery compared with conventional cataract surgery. Acta Ophthalmol 2014:92(7):617-622.
31 Yesilirmak N, Diakonis VF, Sise A, Waren DP, Yoo SH, Donaldson KE. Differences in energy expenditure for conventional and femtosecondassisted cataract surgery using 2 different phacoemulsification systems. J Cataract Refract Surg 2017;43(1):16-21.
32 Conrad-Hengerer I, Al Juburi M, Schultz T, Hengerer FH, Dick HB. Corneal endothelial cell loss and corneal thickness in conventional compared with femtosecond laser-assistedc ataract surgery: three-month follow-up. J Cataract Refract Surg 2013;39(9):1307-1313.
33 Ozlem TY, Necati DM, Fatma YM, Gülsen Y, Ayşe NB, Firdevs O. Are cefuroxime and vancomycin really safe on the corneal endothelial cells?Graefes Arch Clin Exp Ophthalmol 2010;248(3):415-420.
34 Montan PG, Wejde G, Setterquist H, Rylander M, Zetterström C.Prophylactic intracameral cefuroxime. Evaluation of safety and kinetics in cataract surgery. J Cataract Refract Surg 2002;28(6):982-987.
35 Shahraki K, Fard MNA, Shahri F, Pourmatin R, Mohammadi T,Boroumand PG, Shahraki K. Effects of intracameral cefuroxime on corneal endothelial cell counts and its morphology after cataract surgery.Interv Med Appl Sci 2017;9(2):100-104.
36 Cicik ME, Doğan C, Arslan OŞ. Effect of intracameral ophthalmic cefuroxime solution (aprokam®) in the prophylaxis of cataract surgery in patients with keratoplasty. Balkan Med J 2018;35(2):181-185.
37 Yu AY, Ni LY, Wang QM, Huang F, Zhu SQ, Zheng LY, Su YF.Preliminary clinical investigation of cataract surgery with a noncontact femtosecond laser system. Lasers Surg Med 2015;47(9):698-703.
38 Abell RG, Kerr NM, Howie AR, Mustaffa Kamal MA, Allen PL, Vote BJ. Effect of femtosecond laser-assisted cataract surgery on the corneal endothelium. J Cataract Refract Surg 2014;40(11):1777-1783.
39 Mayer WJ, Klaproth OK, Hengerer FH, Kohnen T. Impact of crystalline lens opacification on effective phacoemulsificaition time in femtosecond laser assisted cataract surgery. Am J Ophthalmol 2014;157(2):426-432.
40 Gros-Otero J, Contreras-Martin I, Blazquez-Sanchez V. Induced changes in macula and endothelium after femtosecond laer-assisted cataract surgery: comparison with standard phacoemulsification. J Emmetropia 2013;4:185-189.
41 Yu Y, Chen X, Hua H, Wu M, Lai K, Yao K. Comparative outcomes of femtosecond laser-assisted cataract surgery and manual phacoemulsification:a six-month follow-up. Clin Exp Ophthalmol 2016;44(6):472-480.
42 Matsuda M, Suda T, Manabe R. Serial alterations in endothelial cell shape and pattern after intraocular surgery. Am J Ophthalmol 1984;98(3):313-319.
43 Bencić G, Zorić-Geber M, Sarić D, Corak M, Mandić Z. Clinical importance of the Lens Opacities Classification System III (LOCS III) in phacoemulsification. Coll Antropol 2005;29(Suppl 1):91-94.
44 Li X, Zhang Z, Ye L, Meng J, Zhao Z, Liu Z, Hu J. Acute ocular hypertension disrupts barrier integrity and pump function in rat corneal endothelial cells. Sci Rep 2017;7(1):6951.
Correspondenceto:Lucia Bascaran. Ophthalmology Department, Donostia University Hospital, Paseo del Dr.Beguiristain s/n, San Sebastián 20014, Spain. luciabascaran@gmail.com
Received:2017-09-20 Accepted: 2018-05-17
Abstract● AlM: To compare intraoperative phacoemulsification parameters and its effect on the corneal endothelium of eyes undergoing femtosecond laser-assisted cataract surgery (FLACS) versus conventional phacoemulsification(CP) cataract surgery.● METHODS: Two hundred eyes from one hundred patients were included in a prospective, non-blinded, randomized,controlled, intraindividual clinical study. One hundred eyes underwent FLACS while their one hundred fellow eyes underwent CP. All surgeries were performed using the Victus®femtosecond laser platform and lnfinity®Vision System phacoemulsification machine. Primary outcome measure was endothelial cell density 6mo after surgery.Secondary outcome measures included central corneal thickness (CCT), average cell area, standard deviation,coefficient of variation and hexagonality before surgery and 6mo after surgery and endothelial cell density loss during this period were also evaluated. lntraoperative efficiency parameters [cumulative dissipated energy (CDE),total intraocular surgery time, total ultrasound time, total phacoemulsification time, total torsional energy time, total aspiration time, ultrasound energy, torsional amplitude and fluid required during surgery] were also collated.● RESULTS: Data from these patients was not considered for analysis. Data from 92 patients were analysed.Postoperative endothelial cell density (cells/mm2) between groups (2211.88±392.49 CP; 2246.31±403.48 FLACS) was not statistically significant (P=0.869). Total ultrasound time, torsional energy time, CDE and fluid requirements were significantly lower the FLACS group (P<0.05). Other parameters did not show statistically significant difference between FLACS and CP.● CONCLUSlON: FLACS displays significant improvements in phacoemulsification parameters in comparison to CP.There are no significant differences in corneal endothelium measures between FLACS and CP.
● KEYWORDS:cataract; femtosecond laser assisted cataract surgery; phacoemulsification parameters; corneal endothelium;endothelial cell morphology
DOl:10.18240/ijo.2018.08.10
Citation:Bascaran L, Alberdi T, Martinez-Soroa I, Sarasqueta C,Mendicute J. Differences in energy and corneal endothelium between femtosecond laser-assisted and conventional cataract surgeries:prospective, intraindividual, randomized controlled trial. Int J Ophthalmol 2018;11(8):1308-1316