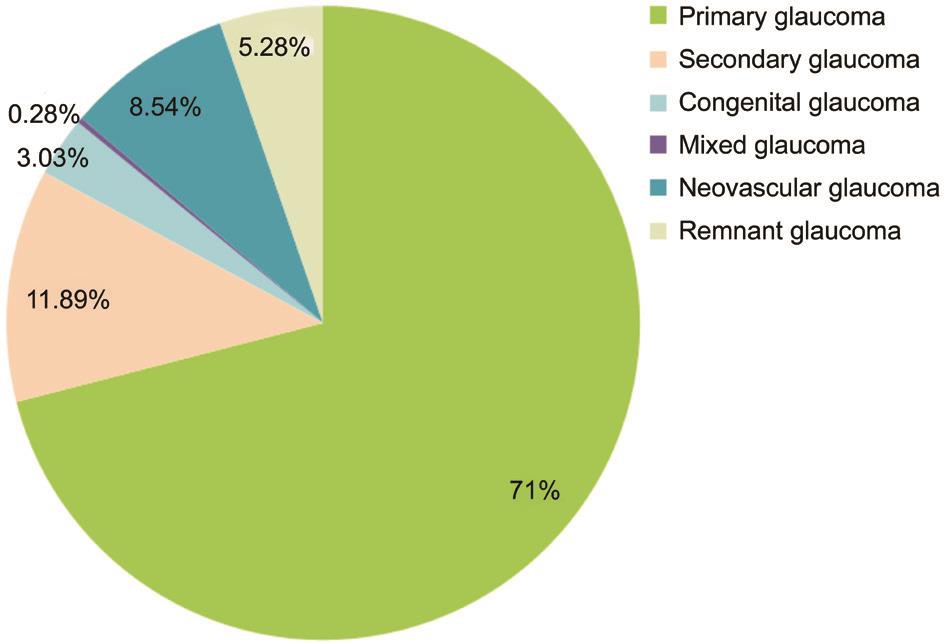
Figure 1 Proportions of different types of glaucoma.
Xiang-Ji Li1,2, Richard Filek3,4, Xiang-Ge He5, Wei Wang5, Hong Liu4, Lian He1, Yu-Rong Tang6, Lin Xie1
1Department of Ophthalmology, the Third Affiliated Hospital,Chongqing Medical University, Chongqing 400016, China
2Department of Ophthalmology, Institute of Surgery Research,Daping Hospital, Third Military Medical University,Chongqing 400042, China
3Department of Pathology and Laboratory Medicine, Western University, London ON N6A 3K7, Canada
4Ivey Eye Institute, St. Joseph's Hospital, London ON N6A 4V2, Canada
5Chongqing Aier Eye Hospital of Aier Eye Hospital Group,Chongqing 400020, China
6Department of Ophthalmology, People's Hospital Zhongshan Branch, Chongqing 400013, China
Surgery is an effective treatment for glaucoma[1]. Although there are a variety of surgical approaches, their basic principle is to create a new aqueous humor outflow pathway to decrease the intraocular pressure (IOP) back to the normal range, and thereby prevent further optic nerve damage. Despite continuous improvements in filtration surgery, a shallow or flat anterior chamber (FAC) still remains a common postoperative complication, which may result in anterior chamber disappearance and irido-corneal touch (grade III FAC). If not treated in time, there is an increased risk for corneal edema, endothelial cell loss[2], lens opacity and peripheral anterior synechia[3],eventually leading to IOP elevation and loss of visual functions[4-5]. In addition, postoperative FAC is often associated with prolonged hospital stay and a demand for re-operation in some cases, which may contribute to patients’ dissatisfaction or even medical disputes.
It remains unknown whether and how preoperative clinical conditions, type of glaucoma, and surgical approach affect the risk of FAC after glaucoma filtration surgery. In clinical settings, multiple risk factors may jointly contribute to the occurrence of FAC following glaucoma filtration surgery, thus making it difficult to prevent such a complication.
Although novel devices such as Ex-PRESS glaucoma mini shunt are increasingly being used in glaucoma drainage surgery, Ahmed glaucoma valve implantation, which provides a different pathway for aqueous drainage from that of trabeculectomy or Ex-PRESS mini shunt, remains an indispensable surgical approach for patients with refractory glaucoma (e.g. remnant glaucoma and neovacular glaucoma)who have undergone multiple failed surgeries with extensive conjunctival scarring. It has been shown in prior studies however that FAC is likely to occur after Ahmed valve implantation; some ophthalmologists have even reported a demand for partial ligation of the drainage tube of Ahmed valve during surgery[6-7]to prevent the occurrence of shallow anterior chamber. The Ahmed valve is designed to automatically open or close depending on the level of IOP, and a partial ligation of the drainage tube may affect the postoperative IOP and even lead to surgical failure. Moreover, Ahmed valve is typically used in patients with refractory glaucoma, who are more prone to choroidal detachment and FAC after surgery.Therefore, it is important to identify the risk factors and assess the extent of each factor’s influence on the incidence of grade III postoperative FAC, which may provide valuable insights into our clinical practice. This study aimed to investigate the incidence rate and risk factors for grade III FAC after glaucoma filtration surgery based on 5-year data.
Study Design and Data CollectionA retrospective chart review of patients who underwent trabeculectomy or Ahmed glaucoma valve implantation in Daping Hospital from January 1st, 2009 to December 31st, 2013 was performed. The study was approved by the Ethics Committee of the Third Affiliated Hospital of Third Military Medical University Human Research Protection Program. After obtaining written informed consent, eyes undergoing trabeculectomy or glaucoma valve implantation alone or in combination with other surgical approaches or antimetabolites were included for analysis. Those eyes treated by Ex-PRESS glaucoma mini shunt implantation, nonpenetrating trabeculectomy,cyclophotocoagulation alone, cyclocryotherapy alone, laser trabeculoplasty, or laser iridotomy were excluded from analysis.
Based on discharge diagnosis, glaucoma was classified into primary glaucoma, secondary glaucoma, congenital glaucoma,mixed glaucoma, neovacular glaucoma, and remnant glaucoma. Primary glaucoma includes primary angle-closure glaucoma (PACG) and primary open angle glaucoma (POAG);and PACG is subclassified into acute PACG (aPACG) and chronic PACG (cPACG). Secondary glaucoma included Posner-Schlossman syndrome, iridocorneal endothelial syndrome, traumatic glaucoma, pigmentary glaucoma,exfoliation syndrome, surgically induced glaucoma, steroidinduced glaucoma, and etc. Neovacular glaucoma was listed separately from secondary glaucoma in this study. Congenital glaucoma included juvenile glaucoma and infantile glaucoma.Patients whose IOP went up again after anti-glaucoma surgery were classified as remnant glaucoma.
The surgical approach used to treat glaucoma was categorized into trabeculectomy alone, trabeculectomy+mitomycin C(MMC), trabeculectomy+lens extraction, trabeculectomy+vitrectomy, trabeculectomy+lens extraction+vitrectomy,trabeculectomy+trabeculotomy, trabeculectomy+cyclocryotherapy; Ahmed glaucoma valve implantation alone,Ahmed valve implantation+MMC, Ahmed valve implantation+lens extraction, Ahmed valve implantation+vitrectomy,Ahmed valve implantation+lens extraction+vitrectomy,Ahmed valve implantation+lens extraction, and Ahmed valve implantation+cyclophotocoagulation. Lens extraction used in glaucoma filtration surgery included phacoemulsification lens extraction (PHACO), extracapsular cataract extraction(ECCE), intracapsular cataract extraction (ICCE), lensectomy,or ultrasonication; while vitrectomy used in filtration surgery included vitrectomy or anterior vitrectomy.
Based on the Spaeth grading system[8], FAC can be classified anatomically into 3 stages. A grade II FAC denotes contact between the entire iris and the corneal endothelium. This is in contrast to grade I, in which iris/corneal touch is limited to the periphery of the iris, and grade III, in which there is both total iris apposition and also contact between the lens (or vitreous)and the cornea[9].
As anterior chamber disappearance may lead to serious consequences, our study focused on grade III FAC after glaucoma filtration surgery, which also reduced the potential bias caused by inaccurate description in medical record as well as clinician’s subjective judgment. Since immediate operation is often required when grade III postoperative FAC occurs,bias resulting from a clinician’s subjective judgment could be avoided. Using grade III FAC as the dependent variable, this retrospective analysis investigated the influence of various types of glaucoma, various surgical approaches, and various risk factors on the incidence of grade III FAC after surgery.
Variable SelectionIn this retrospective analysis, grade III FAC was used as the dependent variable, while type of glaucoma, surgical approach, as well as other risk factors (IOP at admission ˃50 mm Hg, preoperative IOP˃30 mm Hg, age ˃60y, hypertension, coronary heart disease, and diabetes) were used as independent variables[10-11].
Statistical AnalysisAll data analysis was performed by using SPSS 17.0. The Chi-square test was used to compare the incidence rates of grade III postoperative FAC among patients with various types of glaucoma, between use versus non-use of MMC during surgery, as well as trabeculectomy versus Ahmed glaucoma valve implantation. The Fisher’s exact test was conducted to compare the incidence rates of grade III postoperative FAC between trabeculectomy plus lens extraction and/or vitrectomy versus Ahmed valve implantation plus lens extraction and/or vitrectomy. Logistic regression analysis was performed to identify the risk factors for grade III FAC. A P˂0.05 was considered statistically significant.
A total of 2179 eyes receiving anti-glaucoma surgery for the first-listed diagnosis of “glaucoma” were included in this study. Ninety-one eyes suffered from grade III FAC after surgery, with an overall incidence rate of 4.18%. Of these, 77 eyes received re-operation, 12 were relieved after bandaging,mydriasis, anti-inflammation and other conservative treatment.The remaining 2 refused further treatment and were discharged from hospital.
Incidence Rate of Grade III Flat Anterior Chamber by Type of GlaucomaAs shown in Figure 1, a majority of eyes were treated for primary glaucoma (1547/2179 eyes, 71%),including POAG, aPACG, and cPACG (Figure 2). Other types of glaucoma included secondary glaucoma (259 eyes, 11.89%),neovascular glaucoma (186 eyes, 8.54%), remnant glaucoma(115 eyes, 5.28%), congenital glaucoma (66 eyes, 3.03%), and mixed glaucoma (6 eyes, 0.28%).
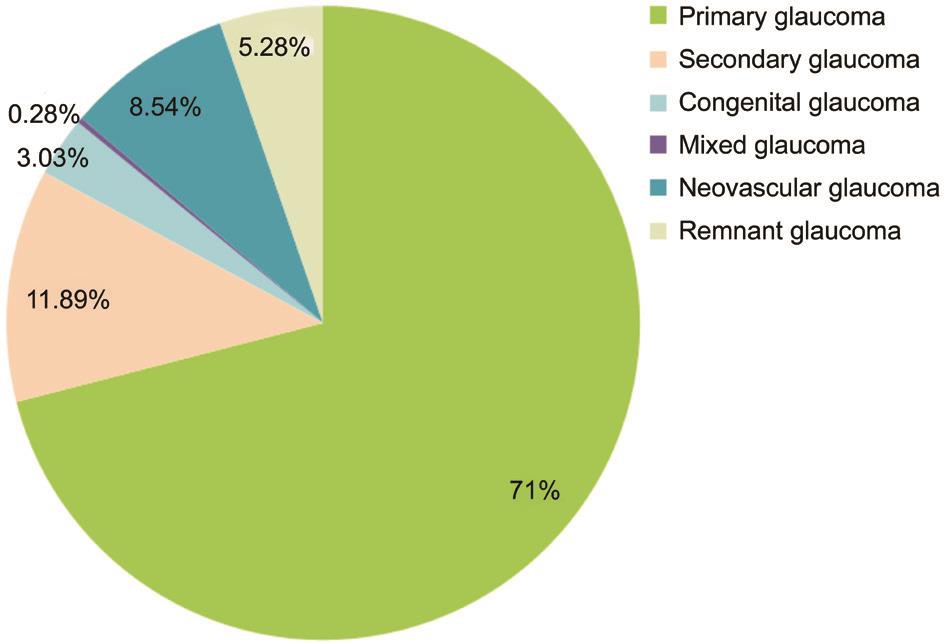
Figure 1 Proportions of different types of glaucoma.

Figure 2 Proportions of different types of primary glaucoma.
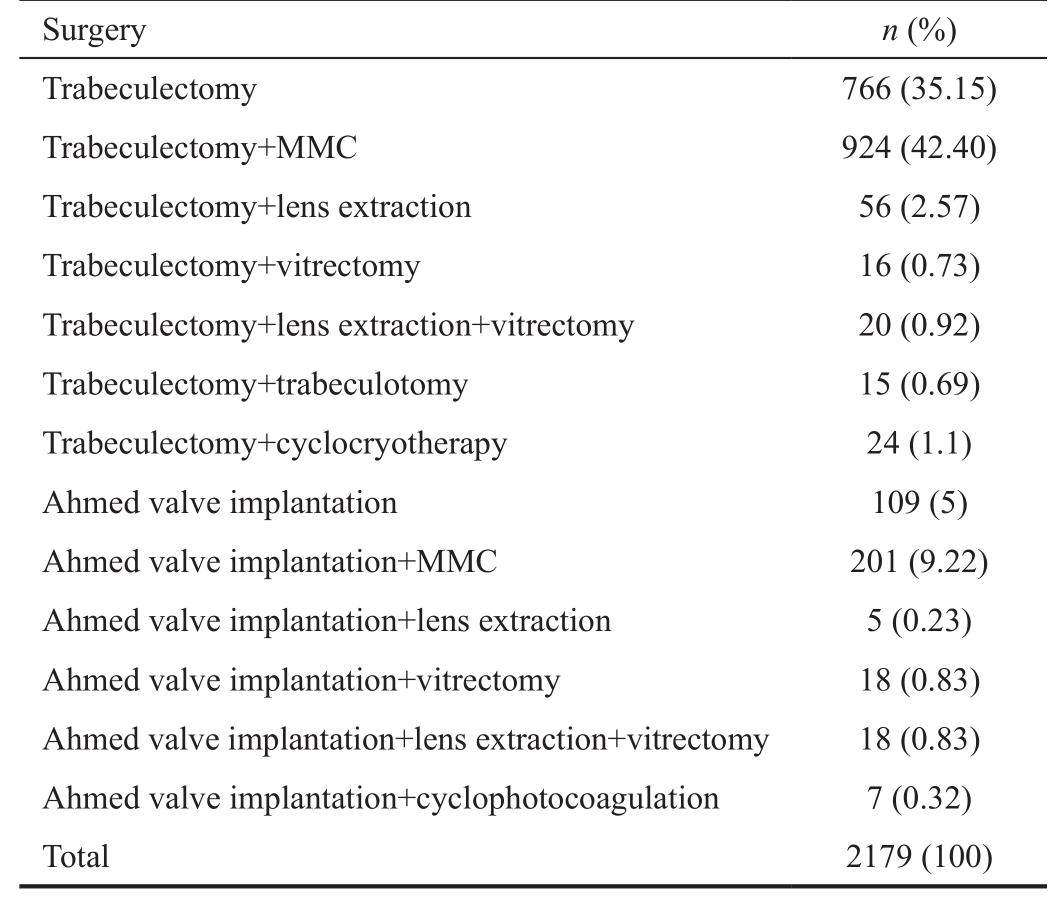
Table 1 Incidence rate of grade III FAC by type of glaucoma n (%)
FAC: Flat anterior chamber; POAG: Primary open angle glaucoma;aPACG: Acute primary angle-closure glaucoma; cPACG: Chronic primary angle-closure glaucoma. According to Chi-square test,χ2=92.751, two-tailed P˂0.0001.
The incidence rate of grade III FAC by type of glaucoma is shown in Table 1. Of 471 eyes with POAG, grade III FAC occurred in only 3 eyes (0.64%). PACG was diagnosed in 1076 eyes, 39 (3.62%) of which developed grade III FAC, including 12 eyes (12/300, 4%) with aPACG and 27 eyes (27/776,3.48%) with cPACG. Six of 259 eyes (2.32%) with secondary glaucoma, 28 of 186 eyes (15.05%) with neovasular glaucoma,1 of 66 eyes (1.52%) with congenital glaucoma, and 14 of 115 eyes (12.17%) with remnant glaucoma suffered from grade III FAC. Of 6 eyes with mixed glaucoma, none developed grade III FAC after surgery. The Chi-square test revealed that type of glaucoma had a significant effect on the incidence rate of grade III postoperative FAC (χ2=92.751, P˂0.0001); neovascular glaucoma and remnant glaucoma were associated with a significantly higher risk of grade III FAC.
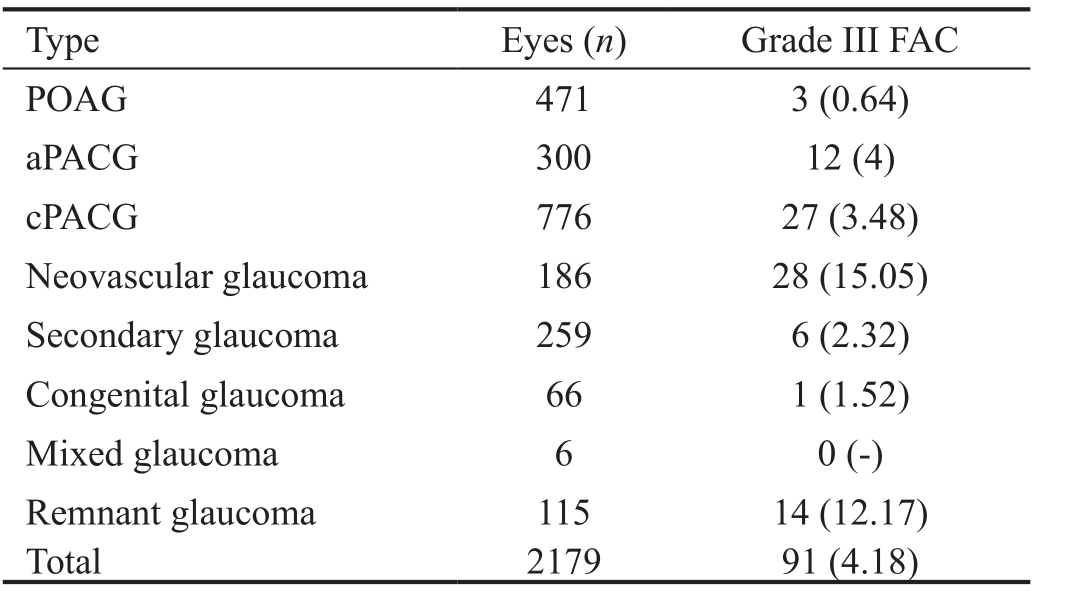
Incidence Rate of Grade III Flat Anterior Chamber by Surgical Approach and Use of AntimetabolitesThe proportions of different approaches for glaucoma filtration surgery are listed in Table 2. Trabeculectomy plus MMC(924/2179 eyes, 42.4%) and trabeculectomy alone (766,35.15%) were the most commonly used surgical approaches for patients with glaucoma.
We compared the incidence rates of grade III postoperative FAC between use versus non-use of MMC during trabeculectomy or Ahmed glaucoma valve implantation using the Chi-square test. Results indicated that the incidence rates of grade III FAC were similar in eyes receiving trabeculectomy with or without MMC (χ2=1.196, P=0.274); the incidence rates of grade III FAC were also comparable in eyes receiving Ahmed valve implantation with or without MMC (χ2=1.584, P=0.208; Table 3).According to Chi-square test, trabeculectomy with versus without MMC: χ2=1.196, two-tailed P=0.274; Ahmed valve implantation with versus without MMC: χ2=1.584, two-tailed P=0.208.
As the use of MMC did not affect the incidence of grade III FAC,eyes treated with or without MMC during trabeculectomy or Ahmed glaucoma valve implantation were pooled for analysis.The Chi-square test revealed that eyes receiving Ahmed valve implantation had a significantly higher risk of developing grade III FAC compared with those receiving trabeculectomy(χ2=71.026, P˂0.001; Table 4).
In eyes undergoing trabeculectomy+lens extraction or Ahmed valve implantation+lens extraction, either with or without primary intraocular lens implantation, none developed grade III FAC after surgery (Table 5).
When vitrectomy was performed in combination with trabeculectomy, no case of grade III FAC was reported;whereas when vitrectomy was done in combination with Ahmed valve implantation, 3 of 18 eyes (16.67%) developed grade III FAC (Table 6). According to the Fisher’s exact test,the difference was not statistically significant (P=0.230).
One eye (1/19, 5%) treated by trabeculectomy+lens extraction+vitrectomy and another eye (1/17, 5.56%) treated by Ahmed valve implantation+lens extraction+vitrectomy suffered from grade III FAC after surgery (Table 7). The Fisher’s exact test showed that the difference was not statistically significant (P=1).
Incidence Rate of Grade III Flat Anterior Chamber by Other Potential Risk FactorsAmong the 2179 eyes, 1186(54.43%) were aged over 60 years old at the time of surgery,68 (5.73%) of whom developed grade III FAC after surgery,accounting for 74.72% of all cases with grade III FAC.Twenty-seven of 385 patients (7.01%) with an IOP higher than 50 mm Hg at admission, 44 of 619 patients (7.11%) with a preoperative IOP higher than 30 mm Hg, 18 of 289 patients(6.22%) accompanied with hypertension, 2 of 289 patients(3.03%) with a history of coronary heart disease, and 18 of 166 patients (5.42%) with a history of diabetes developed grade III FAC after surgery (Table 8).
Table 2 Proportions of different approaches for glaucoma filtration surgery
MMC: Mitomycin C.
Table 3 Incidence rate of grade III FAC by use of MMC n (%)
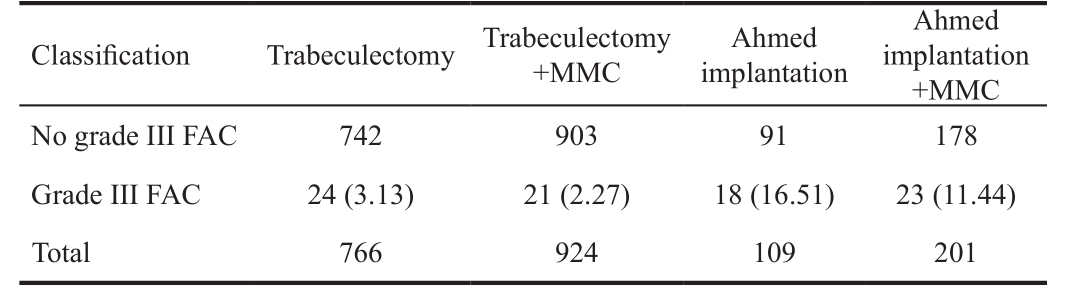
MMC: Mitomycin C; FAC: Flat anterior chamber.
Table 4 Incidence rate of grade III FAC after trabeculectomy versus Ahmed valve implantation n (%)
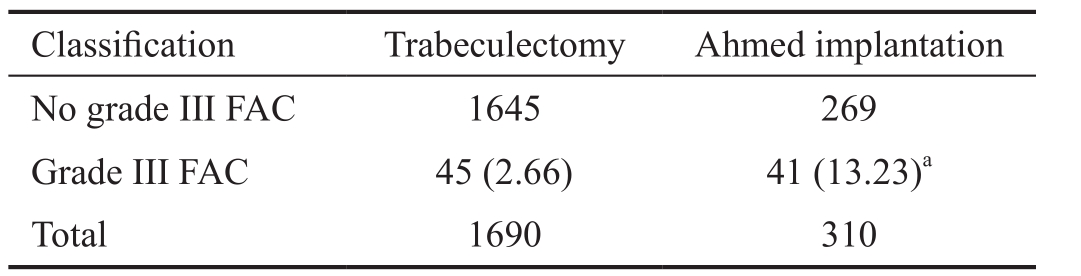
FAC: Flat anterior chamber.aChi-square test, χ2=71.026, two-tailed P˂0.001.
Table 5 Incidence rate of grade III FAC after trabeculectomy or Ahmed valve implantation combined with lens extraction n (%)

FAC: Flat anterior chamber.
Table 6 Incidence rate of grade III FAC after trabeculectomy or Ahmed valve implantation combined with vitrectomy n (%)

FAC: Flat anterior chamber. According to Fisher’s exact test, twotailed P=0.230.
Table 7 Incidence rate of grade III FAC after trabeculectomy or Ahmed valve implantation combined with both lens extraction and vitrectomy n (%)
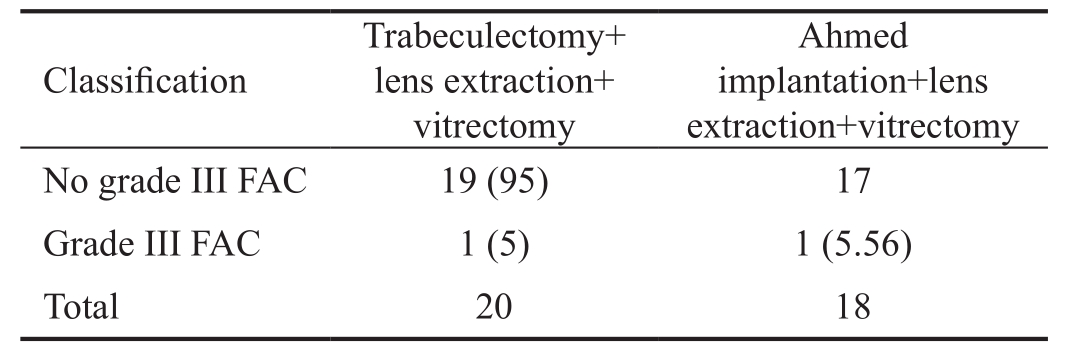
FAC: Flat anterior chamber. According to Fisher’s exact test, twotailed P=1.
Regression Analysis of Risk Factors for Grade III Flat Anterior ChamberThe logistic regression analysis, which used grade III FAC as the dependent variable and potential risk factors as the independent variables, showed that POAG had a negative correlation with the incidence of grade III FAC,while neovascular glaucoma, remnant glaucoma, Ahmed valve implantation, Ahmed valve implantation+MMC, Ahmed valve implantation+vitrectomy, age˃60y, and IOP at admission ˃50 mm Hg were positively correlated with the incidence of grade III FAC (all P˂0.05). No significant correlation was observed between the risk of grade III FAC and other factors(P˃0.05; Table 9).
FAC is a common complication after anti-glaucoma surgery.If not treated properly, grade III FAC may lead to treatment failure. The overall incidence rate of grade III postoperative FAC was up to 4.18% in this study. Thus, it is important to identify subsets of patients who are more susceptible to FAC and surgical approaches that are more likely to induce FAC after surgery. This may aid in the selection of surgical approaches,improve surgical techniques to reduce the risk of FAC, help patients understand the potential risks of surgical treatment and also aid in them making their own treatment decisions.
Type of GlaucomaIn this study, the incidence rates of grade III FAC reached as high as 15.05% and 12.17% in patients with neovascular glaucoma and remnant glaucoma, respectively,both of which were much higher than the overall rate of 4.18%.Often caused by retinal ischemia and vascular dysfunction,neovascular glaucoma is usually associated with a very high preoperative IOP and neovascular leakage. There is also an increased risk for choroidal detachment and even expulsive choroidal hemorrhage during or after surgery, leading to flattening or even disappearance of the anterior chamber[12].Typically seen in patients who have undergone multiple surgeries, remnant glaucoma may be associated with abnormal anterior chamber structure, goniosynechia, posterior synechia,intumescent lens, and occlusion peripheral fistula due to postoperative inflammation. When patients receive glaucoma filtration surgery again, a lower pressure in the anteriorchamber as compared to the posterior chamber and inadequate aqueous drainage may create a pressure gradient that pushes the lens and iris forward, resulting in FAC. In our study, most cases of malignant glaucoma with grade III postoperative FAC and IOP elevation were observed in patients diagnosed as one of these two types of glaucoma. By contrast, during the 5-year span, only 3 of 471 eyes with POAG developed grade III FAC after surgery, probably because POAG is often seen in young and middle-aged males with adequate depth and volume of the anterior chamber, good choroidal vascular elasticity and thus a lower risk of leakage.
Table 8 Incidence rate of grade III FAC by other risk factors n (%)
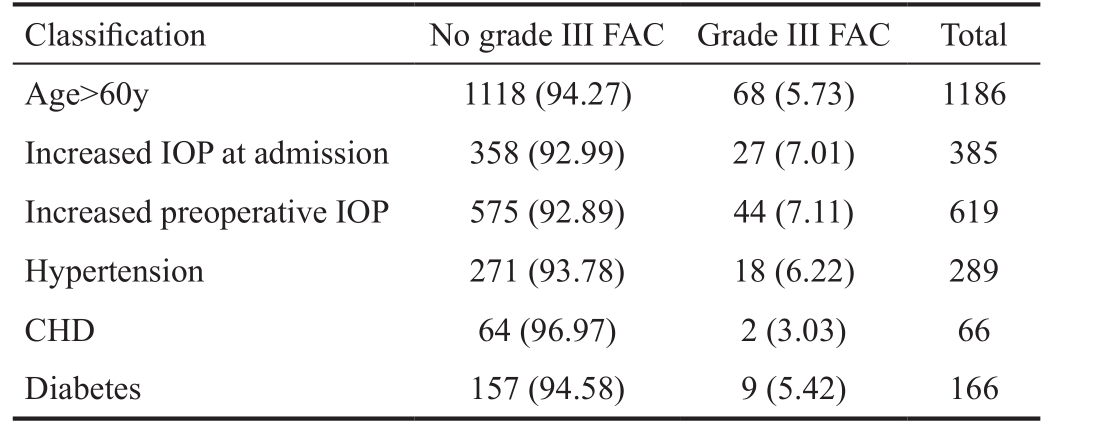
FAC: Flat anterior chamber; CHD: Coronary heart disease; IOP:Intraocular pressure.
Table 9 Logistic regression analysis of risk factors for grade III FAC
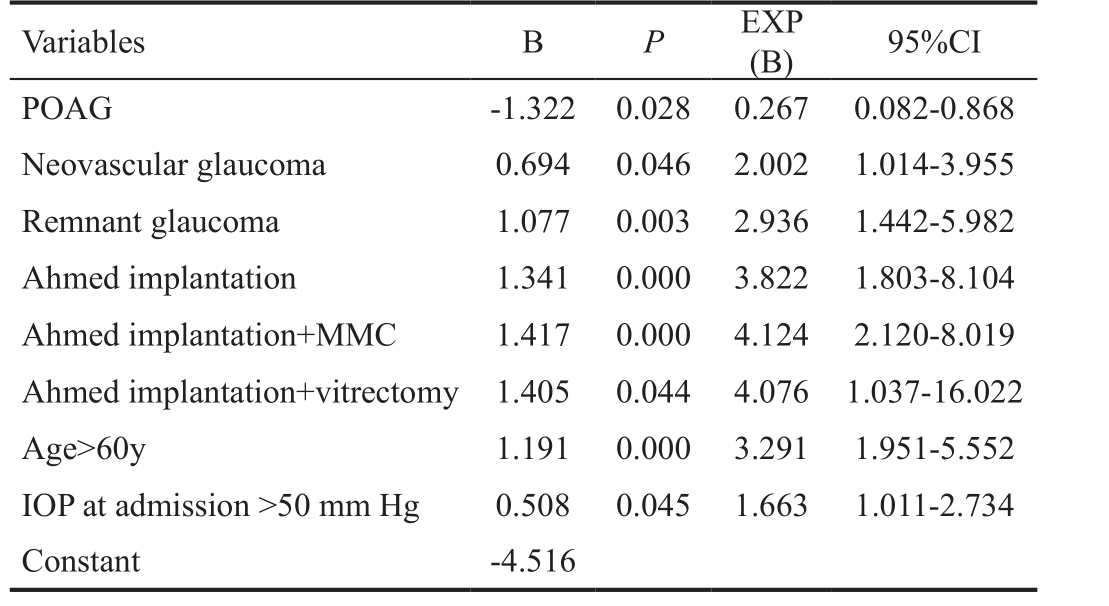
POAG: Primary open angle glaucoma; MMC: Mitomycin C; IOP:Intraocular pressure; CI: Confidence interval.
Type of ProcedureTrabeculectomy remains the main surgical approach for glaucoma patients in our ophthalmic center, accounting for 80% of all anti-glaucoma surgeries.In this study, 45 of 1690 eyes receiving trabeculectomy with or without the use of MMC developed grade III FAC after surgery, with an incidence of 2.66%; while 41 of 310 eyes receiving Ahmed valve implantation with or without MMC suffered from grade III FAC, with an incidence of 13.23%.Both of these incidence rates are lower than those reported in published literatures[13]. Notably, we found that Ahmed valve implantation was much more likely to induce grade III FAC after surgery as compared to trabeculectomy. The Logistic regression analysis also confirmed that glaucoma valve implantation, glaucoma valve implantation+MMC,glaucoma valve implantation+vitrectomy were associated with a significantly higher risk for grade III FAC.
Here are several reasons that may explain why Ahmed glaucoma valve implantation is associated with a higher risk for grade III FAC than trabeculectomy. Firstly, Ahmed valve is typically used to treat refractory glaucoma including neovascular glaucoma, traumatic glaucoma, or complex cases that have previously undergone multiple surgeries. Secondly,unlike trabeculectomy, peripheral iridotomy hole is often not made during Ahmed valve implantation, and postoperative pupillary block may create a pressure gradient between the anterior and posterior chambers, resulting in a higher risk for FAC or even disappearance of the anterior chamber.Thirdly, due to its unfavorable switching performance[14-16], the Ahmed valve may not produce moderate resistance against aqueous outflow at the early stage after implantation, leading to excessive drainage of the aqueous humor. Meanwhile,choroidal detachment and ciliary body edema may cause an increased pressure in the posterior chamber, which also contributes to a high risk for grade III FAC after surgery.
Influence of AntimetabolitesSince its use in glaucoma filtration surgery in the early 1990s[17], MMC, which inhibits the proliferation of fibroblasts, has effectively prevented bleb scarring after surgery and improved the success rate of anti-glaucoma surgery[18-19]. Some surgeons argue however that the use of MMC during surgery results in a higher risk for excessive filtration, non-healing wound or even wound leakage, which might contribute to flattening or disappearance of the anterior chamber after surgery[20]. Our study showed that the incidence rate of grade III FAC after trabeculectomy alone was 3.13%, while that after trabeculectomy+MMC was 2.27%;the rate after glaucoma valve implantation alone was 16.51%,while that after valve implantation+MMC was 11.44%. The incidence rates were slightly lower when MMC was used;however, the differences were not statistically significant for both comparisons.
Although MMC is able to prevent postoperative scarring,excessive filtration at the early stage after surgery may lead to FAC. In our ophthalmic center, limbus-based conjunctival flap is routinely made when trabeculectomy is combined with the use of MMC, which helps to prevent non-healing wound or wound leakage, and thus reduce the risk of FAC. Moreover,the decision as to whether or not to use MMC should also be individualized. For some elderly patients who are more prone to excessive filtration due to the thin fascia, the use of MMC is not recommended; whereas for younger patients who are less likely to develop grade III FAC after surgery, MMC is commonly used to improve the success rate of anti-glaucoma surgery[21].
Other Risk FactorsIn our study, the Logistic regression analysis revealed that old age (˃60y) and higher IOP at admission (˃50 mm Hg) were significantly correlated with the incidence of grade III postoperative FAC, while other factors such as preoperative IOP˃30 mm Hg, hypertension,coronary heart disease (CHD), and diabetes had no significant correlation with the incidence of grade III FAC. We found that the incidence of grade III FAC among patients aged over 60y was 5.73%, and that among patients whose IOP at admission exceeded 50 mm Hg was 7.01%, both of which were much higher than the overall incidence of 4.18% in this study.
Old age (˃60y) is a risk factor for postoperative FAC, probably related to the reduced elasticity and contractility of choroidal vessels in elderly patients, leading to an increased risk for choroidal effusion and detachment. However, the regression analysis did not find a significant correlation between factors like hypertension, CHD, and diabetes and the incidence of grade III FAC. We speculate that other factors may also contribute to the occurrence of grade III FAC after glaucoma filtration surgery, including intumescent lens, zonular laxity,and reduced depth of the anterior chamber[22-23]; forward movement of the lens and significant pupillary block; vitreous liquefaction and posterior detachment, resulting in loss of plasticity and poor resistance against choroidal effusion; as well as subconjunctival atrophy, which may be associated with excessive filtration and excessive IOP reduction, leading to ciliary body or choroidal detachment. If the ciliary body is affected, reduced aqueous humor production may further aggravate flattening or disappearance of the anterior chamber after surgery.
A higher preoperative IOP is often associated with serious ocular circulatory disturbance. Elevated IOP induces tissue hypoxia and ischemia, or even necrosis, uveal serofibrinous and bloody effusion in serious cases. The huge fluctuations of IOP before and after surgery may cause choroidal vascular dilation and effusion - an abnormal accumulation of fluid in the suprachoroidal space- and hence the formation of choroidal detachment[24], resulting in the occurrence of postoperative FAC. Increased IOP before surgery as well as decreased IOP after surgery may also induce ciliary body edema, leading to anterior dislocation of the lens and ciliary block. According to the regression analysis, preoperative IOP˃30 mm Hg was not found to be correlated with the incidence of FAC. IOP at admission ˃50 mm Hg, commonly seen in patients with aPACG or neovascular glaucoma, was significantly correlated with the risk of grade III FAC, possibly because of the higher degree of ocular pathological damages and limited mechanism for compensation.
Predictive Value of Risk FactorsThe occurrence of grade III FAC is attributed to multiple factors. Based on the findings of our Logistic regression analysis, it is suggested that several factors including patient’s clinical conditions, type of glaucoma, and surgical approach be taken into consideration to inform clinical decision-making. Risk prediction for postoperative FAC can be performed for each individual patient based on the type of glaucoma, age, IOP at admission,and the planned surgical approach. For high-risk patients,alternative techniques such as laser iridotomy, lens extraction,or cyclophotocoagulation may be considered[25-26]. If filtration surgery is still required, the potential risks must be fully explained to patients before surgery.
Limitations of This StudyWe acknowledge that our study has some limitations. Although a large sample consisting of 2179 patients receiving trabeculectomy or Ahmed glaucoma valve implantation during the 5-year period was enrolled in this retrospective analysis, some potential risk factors, such as the anterior chamber depth and lens thickness, were not be assessed due to data unavailability or incompleteness.Additional studies are required to identify and validate all the risk factors for grade III FAC after glaucoma filtration surgery.
Thank you to the secretaries and staff of Daping Hospital where this research was conducted.
Authors’ contributions:All authors made substantial contributions to conception and design. Li XJ and Wang W collected the data. Li XJ, Filek R, He XG, He L, Tang YR and Xie L made substantial contributions to analysis and interpretation of data. Li XJ and Filek R wrote the first draft of the manuscript. All authors were involved in revising the manuscript critically for important intellectual content. He XG and Xie L gave final approval of the version to be published.All authors read and approved final manuscript.
Conflicts of Interest:Li XJ, None; Filek R, None; He XG,None; Wang W, None; Liu H, None; He L, None; Tang YR,None; Xie L, None.
REFERENCES
1 Vladyka V, Liscak R, Simonova G, Pilbauer J, Hejdukova I, Novacek L. Progress in glaucoma treatment research: a nonrandomized prospective study of 102 patients with advanced refractory glaucoma treated by Leksell gamma knife irradiation. J Neurosurg 2005;102 Suppl:214-219.
2 Fiore PM, Richter CU, Arzeno G, Arrigg CA, Shingleton BJ, Bellows AR, Hutchinson BT. The effect of anterior chamber depth on endothelial cell count after filtration surgery. Arch Ophthalmol 1989;107(11):1609-1611.
3 Phillips CI, Clark CV, Levy AM. Posterior synechiae after glaucoma operations: aggravation by shallow anterior chamber and pilocarpine. Br J Ophthalmol 1987;71(6):428-432.
4 Schwenn O, Kersten I, Dick HB, Muller H, Pfeiffer N. Effects of early postfiltration ocular hypotony on visual acuity, long-term intraocular pressure control, and posterior segment morphology. J Glaucoma 2001;10(2):85-88.
5 Benson SE, Mandal K, Bunce CV, Fraser SG. Is post-trabeculectomy hypotony a risk factor for subsequent failure? A case control study. BMC Ophthalmol 2005;5:7.
6 Yang JW, Kim YI, Gi CW. The effect of a 5-0 prolene ligation around the Ahmed glaucoma valve tube on the postoperative hypotony. J Korean Ophthalmol Soc 2001;42(8):1172-1177.
7 HaiBo T, Xin K, ShiHeng L, Lin L. Comparison of Ahmed glaucoma valve implantation and trabeculectomy for glaucoma: a systematic review and meta-analysis. PLoS One 2015;10(2):e0118142.
8 Alemu B. Trabeculectomy: complications and success in IOP control.Ethiop Med J 1997;35(1):1-11.
9 de Barros DS, Navarro JB, Mantravadi AV, Siam GA, Gheith ME,Tittler EH, Baez KA, Martinez SM, Spaeth GL. The early FAC after trabeculectomy: a randomized, prospective study of 3 methods of management. J Glaucoma 2009;18(1):13-20.
10 Brubaker RF, Pederson JE. Ciliochoroidal detachment. Surv Ophthalmol 1983;27(5):281-289.
11 Huang J, Lin J, Wu Z, Xu H, Zuo C, Ge J. Outcomes of Ahmed glaucoma valve implantation in advanced primary congenital glaucoma with previous surgical failure. Clin Ophthalmol 2015;9:977-983.
12 Foreman-Larkin J, Netland PA, Salim S. Clinical management of malignant glaucoma. J Ophthalmol 2015;2015:283707.
13 Al-Haddad CE, Abdulaal M, Al-Moujahed A, Ervin AM, Ismail K.Fornix-based versus limbal-based conjunctival trabeculectomy flaps for glaucoma: findings from a cochrane systematic review. Am J Ophthalmol 2017;174:33-41.
14 Prata JA Jr, Mermoud A, LaBree L, Minckler DS. In vitro and in vivo flow characteristics of glaucoma drainage implants. Ophthalmology 1995;102(6):894-904.
15 Porter JM, Krawczyk CH, Carey RF. In vitro flow testing of glaucoma drainage devices. Ophthalmology 1997;104(10):1701-1707.
16 Eisenberg DL, Koo EY, Hafner G, Schuman JS. In vitro flow properties of glaucoma implant devices. Ophthalmic Surg Lasers 1999;30(8):662-667.
17 Chen CW, Huang HT, Bair JS, Lee CC. Trabeculectomy with simultaneous topical application of mitomycin-C in refractory glaucoma.J Ocular pharmacol 1990;6(3):175-182.
18 De Fendi LI, Arruda GV, Scott IU, Paula JS. Mitomycin C versus 5-fluorouracil as an adjunctive treatment for trabeculectomy: a metaanalysis of randomized clinical trials. Clin Exp Ophthalmol 2013;41(8):798-806.
19 Na JH, Sung KR, Shin JA, Moon JI. Antifibrotic effects of pirfenidone on Tenon's fibroblasts in glaucomatous eyes: comparison with mitomycin C and 5-fluorouracil. Graefes Arch Clin Exp Ophthalmol 2015;253(9):1537-1545.
20 Tsai JC, Chang HW, Kao CN, Lai IC, Teng MC. Trabeculectomy with mitomycin C versus trabeculectomy alone for juvenile primary openangle glaucoma. Ophthalmologica 2003;217(1):24-30.
21 Okimoto S, Kiuchi Y, Akita T, Tanaka J. Using the early postoperative intraocular pressure to predict pressure control after a trabeculectomy. J Glaucoma 2014;23(6):410-414.
22 Kashiwagi K, Chiba T, Mabuchi F, Furuya T, Tsukahara S. Fiveyear incidence of angle closure among glaucoma health examination participants. Graefes Arch Clin Exp Ophthalmol 2013;251(4):1219-1228.
23 Sawaguchi S, Sakai H, Iwase A, Yamamoto T, Abe H, Tomita G,Tomidokoro A, Araie M. Prevalence of primary angle closure and primary angle-closure glaucoma in a southwestern rural population of Japan: the Kumejima Study. Ophthalmology 2012;119(6):1134-1142.
24 Bellows AR, Chylack LT Jr, Hutchinson BT. Choroidal detachment.Clinical manifestation, therapy and mechanism of formation. Ophthalmology 1981;88(11):1107-1115.
25 Murthy GJ, Murthy PR, Murthy KR, Kulkarni VV, Murthy KR. A study of the efficacy of endoscopic cyclophotocoagulation for the treatment of refractory glaucomas. Indian J Ophthalmol 2009;57(2):127-132.
26 Lin SC. Endoscopic and transscleral cyclophotocoagulation for the treatment of refractory glaucoma. J Glaucoma 2008;17(3):238-247.
Co-first authors:Xiang-Ji Li and Richard Filek
Correspondenceto:Lin Xie. Department of Ophthalmology,Institute of Surgery Research, Daping Hospital, Third Military Medical University, Chongqing 400042, China.xielin_66@163.com
Received:2018-04-18 Accepted: 2018-05-31
Abstract● AlM: To investigate the incidence rate and risk factors for grade lll flat anterior chamber (FAC) after glaucoma filtration surgery based on 5-year data.● METHODS: Patients who underwent glaucoma filtration surgery in Daping hospital from January 2009 to December 2013 were enrolled in this retrospective study. The incidence of grade lll FAC following glaucoma filtration surgery was determined. Regression analysis was performed to investigate the influence of glaucoma type, surgical approach, age, and preoperative intraocular pressure (lOP)on the risk of postoperative FAC.● RESULTS: A total of 2179 eyes receiving anti-glaucoma surgery were included. Ninety-one eyes suffered from postoperative FAC, with an overall incidence rate of 4.18%.Of 471 eyes with primary open angle glaucoma (POAG),grade lll FAC occurred in only 3 eyes (0.64%). Primary angleclosure glaucoma (PACG) was diagnosed in 1076 eyes,39 (3.62%) of which developed grade lll FAC, including 12 eyes (12/300, 4%) with acute PACG (aPACG) and 27 eyes(27/776, 3.48%) with chronic PACG (cPACG). Six of 259 eyes (2.32%) with secondary glaucoma, 28 of 186 eyes(15.05%) with neovasular glaucoma, 1 of 66 eyes (1.52%)with congenital glaucoma, and 14 of 115 eyes (12.17%)with remnant glaucoma suffered from grade lll FAC. Of 6 eyes with mixed glaucoma, none developed grade lll FAC after surgery. When stratified by surgical approach, 24 of 766 eyes (3.13%) undergoing trabeculectomy, 21 of 924 eyes (2.27%) treated by trabeculectomy plus mitomycin C (MMC), 18 of 109 eyes (16.51%) undergoing Ahmed glaucoma valve implantation, 23 of 201 eyes (11.44%)managed by Ahmed implantation plus MMC, and 5 of 133 eyes (3.76%) treated by Ahmed implantation plus lens extraction or vitrectomy developed grade lll FAC. Logistic regression analysis revealed that factors including neovasular glaucoma, remnant glaucoma, glaucoma valve implantation, glaucoma valve implantation+MMC,glaucoma valve implantation+vitrectomy, age>60y, and lOP at admission >50 mm Hg were significantly associated with an increased risk for grade lll FAC.● CONCLUSlON: The overall incidence of grade lll FAC after glaucoma filtration surgery is 4.18%. Patients with neovasular glaucoma and remnant glaucoma are at a higher risk of developing FAC. Ahmed glaucoma valve implantation is associated with a higher risk for grade lll FAC compared with trabeculectomy. No significant correlation was observed between the use of MMC in glaucoma filtration surgery and the risk of postoperative FAC. Higher lOP at admission (>50 mm Hg) and old age(>60y) are risk factors for grade lll FAC.
● KEYWORDS:glaucoma; filtration surgery; grade III flat anterior chamber; trabeculectomy; glaucoma valve implantation; mitomycin C
DOl:10.18240/ijo.2018.08.12
Citation:Li XJ, Filek R, He XG, Wang W, Liu H, He L, Tang YR,Xie L. Risk factors for flat anterior chamber after glaucoma filtration surgery. Int J Ophthalmol 2018;11(8):1322-1329