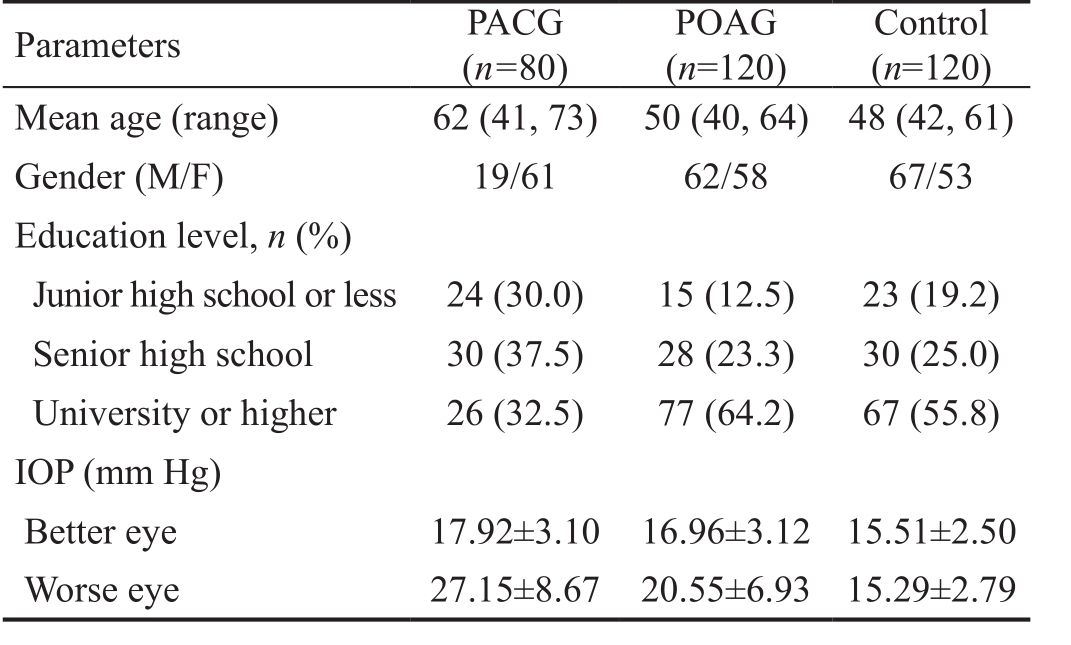
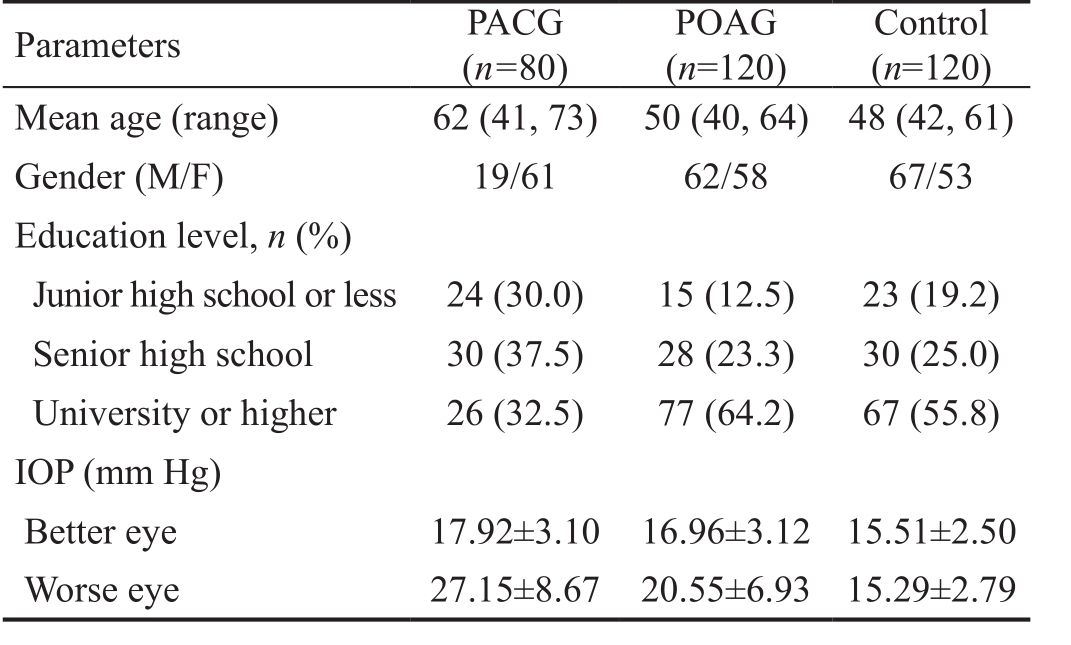
Table 1 Demographic and clinical characteristics of all participants
Xiao-Ping Ma1, Man-Yi Shen1, Guang-Lin Shen1, Qiao-Ran Qi1, Xing-Huai Sun2
1Department of Ophthalmology, Zhongshan Hospital, Fudan University, Shanghai 200032, China
2Department of Ophthalmology, Eye & Ent Hospital of Fudan University, Shanghai 200031, China
M elatonin (5-methoxy N-acetyltryptamine) is a neurohormone secreted from the pineal gland in human beings, which has a circadian rhythm in its secretion to the blood flow. It has been reported that melatonin and some of its derivatives produce a marked reduction in intraocular pressure(IOP) in normotensive and hypertensive conditions through melatonin receptors[1-3]. In addition, melatonin protects ocular tissue against free radicals which always lead to an extensive loss of the retinal ganglion cells[4-5].
Glaucoma is a common, pathophysiologically heterogeneous,progressive optic neuropathy. Elevated IOP together with excessive retinal oxidative stress (ROS) are considered as the main risk factors in the developing of glaucoma, leading to glaucomatous alterations and neurodegeneration[6]. Taking into account the benefits melatonin have to the human eye, we may propose a hypothesis that dysfunctional melatonin signaling may be considered a possible risk factor in the pathogenesis of glaucoma[2]. Rosen et al[7]reported that age-related macular degeneration (AMD), in which cumulative oxidative stress plays an important role, interfered in the production of melatonin. But the changes of circulatory melatonin level in glaucoma have not been reported previously.
Furthermore, it has been reported that patients with different degrees of blindness resulting from glaucoma show abnormal circadian rhythms, along with sleep disturbances and depressed moods[5]. Recently, there has been evidence that alterations in the secretory pattern of melatonin is present in various psychiatric disorders. Rahman et al[8]demonstrated a significant sleep-wake cycle disruption in low melatonin secretors. In the study by Crasson et al[9], the patients with major depression showed a 77min peak time delay of serum melatonin secretion.Considering the possible pathophysiological connection glaucoma has to sleep disorders, anxiety and depression, this may indicate that the nature of melatonin secretion rhythm in glaucoma be disturbed.
In the present study, we tested the hypothesis individuals with primary glaucoma show higher rates of sleep disturbance,anxiety and depression, as compared with a non-glaucoma control group. Serum melatonin was measured to determine whether alterations in the secretory pattern of melatonin are present in glaucoma patients with various psychiatric disorders.
SubjectsThis was a perspective case-control study conducted from March 2014 to February 2015. In this study, 80 patients with primary angle-closure glaucoma (PACG) and 120 patients with primary open angle glaucoma (POAG) were recruited consecutively in the Eye and Ent Hospital of Fudan University,which is one of the largest eye care hospitals in China. All participants underwent a comprehensive ophthalmologic examination including review of medical history, visual acuity, IOP measurement, gonioscopy, dilated fundoscopy examination. PACG is a chronic progressive optic neuropathy with an occludable drainage angle and features indicating that trabecular obstruction by the peripheral iris has occurred,while the anterior chamber angle of POAG shown to be open on gonioscopy. A control group of 120 healthy subjects without family history of glaucoma or high IOP were recruited from the same area. Participants exclusion criteria included:1) any kind of intraocular surgery or laser treatment within the last three months; 2) personal history of any other ocular disease such as retinitis pigmentosa; 3) systemic diseases including psychiatric illness; 4) drug or alcohol abuse; 5)pregnancy or lactation; 6) night work or transmeridian travel in the previous three months, that might affect the results. All patients and control participants gave informed consent prior to participation. The study was conducted under Human Research Ethics Committee approval and conformed to the tenets of the Declaration of Helsinki.
Methods
Psychometric measuresParticipants were asked to complete a battery of questionnaires independently which included measures of subjective levels of sleepiness, anxiety and depression. Sleep quality of each subject in the three groups(POAG group, PACG group and control group) was measured with the Pittsburgh sleep quality index (PSQI), self-rating anxiety scale (SAS) and self-rating depression scale (SDS)were applied to assess anxiety and depression consecutively.The time required to finish each questionnaire was strictly limited ˂10min for PSQI, SAS and SDS, respectively. Sleep was considered to be disturbed if the global PSQI score was higher than 7. SAS total score ˃45 was predefined as cut-off score for anxiety and SDS total score ˃50 was predefined as cut-off score for depression, as suggested in earlier literature.Scores of PSQI, SAS and SDS were compared between the three groups.
Table 1 Demographic and clinical characteristics of all participants
Melatonin assessmentAfter psychometric measures, we chose 58 patients with primary glaucoma and 20 non-glaucoma control patients to collect their serum samples at 7-10 a.m.(background light intensity ˂2 lx, participants were allowed to sleep from 23:00 to 06:00). For measure of serum melatonin,blood samples of 5 mL were drawn from forearm vein and centrifuged immediately. Serum samples (2 mL) were frozen at -70℃ until enzyme linked immunosorbent assay (ELISA).This is a competitive immunoassay that determined the melatonin levels by use of a melatonin ELISA kit (LSBioTM Melatonin EIA Competition ELISA Kit America) and an ELISA reader (thermo multiskan FC). Serum melatonin levels are given in pg/mL. We compared melatonin levels in POAG,PACG and control groups and analyzed the disturbance of melatonin levels in glaucoma patients with sleep disorders,anxiety and depression.
Statistical AnalysisStatistical analyses were performed by using SPSS 20.0 software. Continuous variables were expressed as means±standard deviation and analyzed by using the non-parametric Wilcoxon ranked test and one-way ANOVA.While categorical variables were presented as percentage, they were assessed by mean of the Pearson’s Chi-squared test (χ2).P˂0.05 considered statistically significant.
Eventually, 80 PACG patients, 120 POAG patients and 120 controls with a complete questionnaire were included.Demographic details of recruited patients were shown in Table 1.The scores of PSQI, SAS and SDS were higher in glaucoma patients than in controls, whereas the PACG group had a higher score for all scales (9.38±0.40; 46.08±8.99; 51.11±10.72)than the POAG group (7.43±0.35; 45.42±9.87; 49.04±12.24)and control group (4.16±0.28; 35.49±9.18; 40.31±13.08)(Table 2). Taking PSQI score ˃7, SAS score ˃45 and SDS score ˃50 as cut-off, the prevalence of sleep disorder, anxiety and depression in the PACG group (80.0%, 56.2%, 51.2%)was significantly higher than in the POAG group (54.2%,P=0.000; 50.0%, P=0.000; 53.3%, P=0.000) and control group (17.5%, P=0.000; 21.7%, P=0.000; 25.8%, P=0.000)(Table 2). There were 58 patients in the glaucoma group and20 control participants as shown in Table 3, and the mean age was significant high in primary glaucoma as compared with non-glaucoma (P=0.000). The serum melatonin levels in PACG (37.29±2.99 pg/mL) and POAG (35.97±3.64 pg/mL)were significantly higher than the controls (29.96±3.94 pg/mL)(P˂0.001), but no significant difference was found between the PACG and POAG (P=0.216˃0.05). Comparisons were done separately for glaucoma patients with and without sleep disturbance, for patients with and without anxiety disorder, and for patients with and without depression. From Table 4, we could see that depression was significantly associated with sex and the IOP of the worse eye. Glaucoma patients with sleep disorders, anxiety and depression were more likely resulting in the increase of melatonin levels compared with simple glaucoma patients during the daytime.
Table 2 Comparison of sleep disturbance, anxiety and depression and using self-rating scales between the three groups
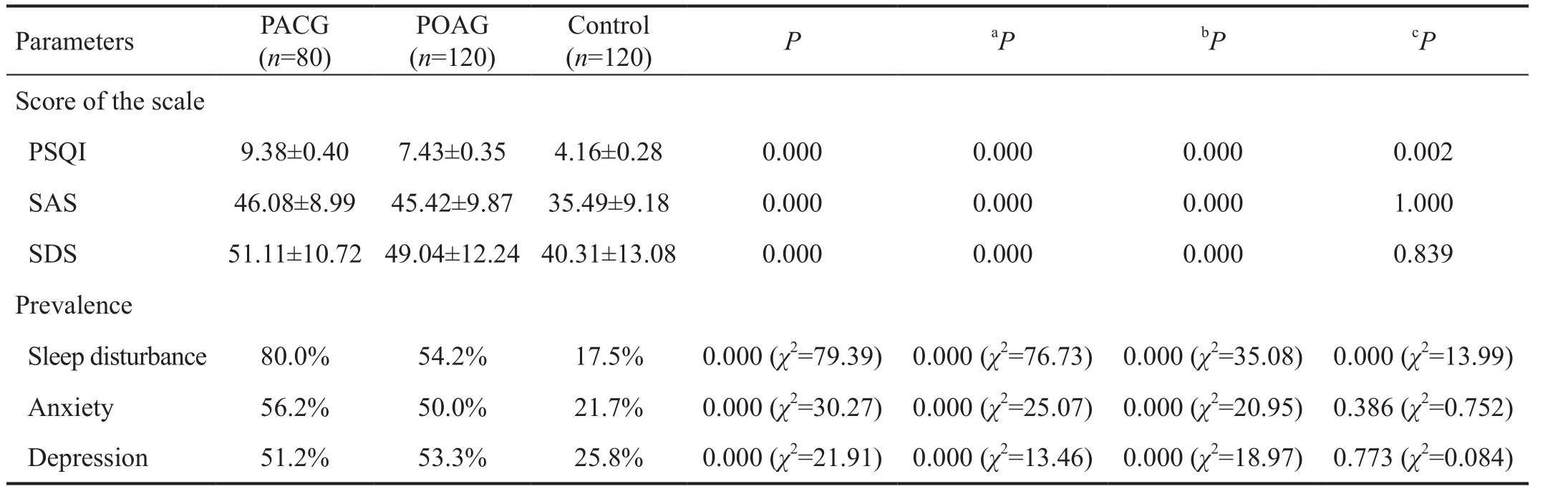
PACG: Primary angle-closure glaucoma; POAG: Primary open angle glaucoma; PSQI: Pittsburgh sleep quality index; SAS: Self-rating anxiety scale; SDS: Self-rating depression scale.aPACG versus control;bPOAG versus control;cPACG versus POAG. Kruskal-Wallis test followed by all pairwise multiple comparisons.
Table 3 Demographic data and melatonin levels in patients with glaucoma and normal controls
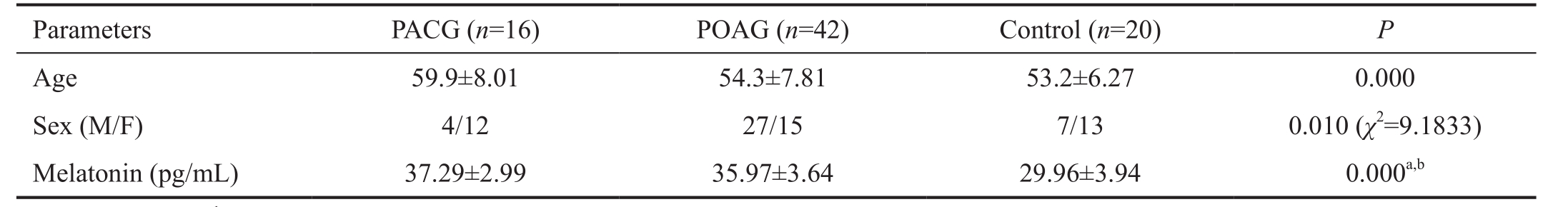
aP OAG vs control;bPACG vs control.
Table 4 Comparison of melatonin levels in glaucoma patients with psychiatric disorders and the control group
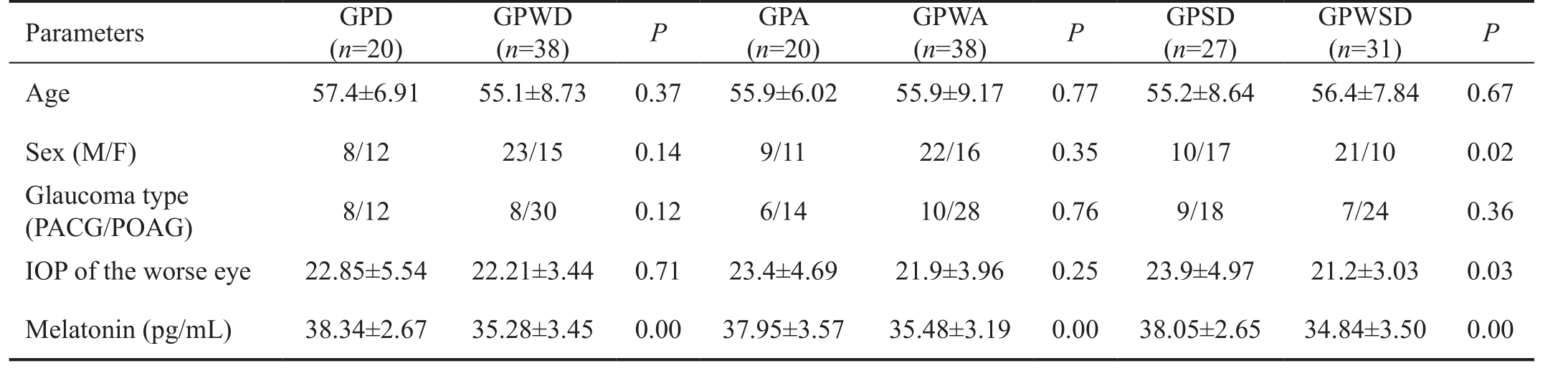
GPD: Glaucoma patients with depression; GPWD: Glaucoma patients without depression; GPA: Glaucoma patients with anxiety; GPWA:Glaucoma patients without anxiety; GPSD: Glaucoma patients with sleep disturbance; GPWSD: Glaucoma patients without sleep disturbance;PACG: Primary angle-closure glaucoma; POAG: Primary open angle glaucoma.
The rhythm of melatonin secretion from the pineal gland,increasing during the evening and returning to its baseline levels at about 10 a.m., is driven by a “biological clock” in the suprachiasmatic nucleus (SCN) of the hypothalamus[10]. According to the circadian disruption hypothesis, light intensity and certain critical wave lengths might disrupt the endogenous circadian rhythm and specifically suppress production of the pineal hormone melatonin and its secretion into the blood via a specific pathway[11]. Retinal stimulation by light sends a stimulatory signal to the SCN which in turn transmits the signal indirectly to pinealocytes regulating the pineal melatonin secretion[12]. It has been reported that daily illumination, ophthalmic factors,sleep duration, and race each had independent associations with acrophases of melatonin excretion[13].
In our study, results showed melatonin concentrations of glaucoma patients especially those with psychiatric disorders increased at 7-10 a.m., and suggested that the effects of glaucoma on the rhythm of melatonin secretion can be twofold: 1) affecting the photic input to the circadian system;2) a direct impact of sleep disorders, anxiety and depression relating to glaucoma.
Glaucoma is an ocular degenerative disease with a progressive death of the retinal ganglion cells and eventually causes optic nerve atrophy by way of axonal loss. Intrinsically photosensitive retinal ganglion cells (IpRGC), a specialized subset of retinal ganglion cells, play a major role in photo transduction through the retinohypothalamic tract to the SCN and herewith also in the regulation of the pineal melatonin secretion[6]. IpRGC death leads to direct and adverse effects on the circadian timing system as well as disruption of melatonin secretion. Furthermore, reduced axonal number would have a relative diminution of transmitted stimuli and reduced axonal stimulation to the central visual pathways likely diminishes light input to the circadian system, affecting the rhythm of pineal melatonin production[12].
In addition, melatonin levels in patients with PACG are higher than that in POAG. Acute IOP elevation in some of the PACG patients leads to ischemic-reperfusion damage to the whole retina, including not only the ganglion cells, but also other neurons like rods and cons[14]. Therefore, in PACG, the residual IpRGCs may get less input from the residual rods and cons, resulting in less photic input to circadian system and increase of melatonin concentrations. However, there’s not much distance of melatonin level between 37.29±2.99 and 35.97±3.64 pg/mL, which might be attributed to no statistically significant IOP and statistically speaking, more studies are needed.
The patients in glaucoma group were older as compared to control group which might relate to the increase of serum melatonin level as well. The effects of age on the melatonin secretion rhythm might be wide-ranging, as 1) ophthalmic factors associated with increasing age such as senile miosis and opacification of the ocular lens reduce light transmission to the retina, eventually affect retinal stimulation to SCN and melatonin secretion; 2) age-related reduction in light responsivity leads to that it might be inadequate to prevent circadian misalignment with an average amount of illumination for the elderly, resulting in a disturbance of melatonin secretion; 3) normal individuals losing ganglion cells in an age-dependent manner at an estimated rate as high as 5000 axons per year[15], together with neurodegenerative changes with age in the SCN may cause decreased regulation function of pineal melatonin secretion.
On the basis of aforementioned analysis, glaucoma is an ophthalmological disease affecting the photic input to the circadian system and leading to circadian rhythm alteration and melatonin production impairment. On the other hand,there has been evidence that glaucoma leads to a high incidence of sleep disorders, anxiety and depression as well as a dysregulation of circadian rhythms[15]. In the present study, we used self-reporting questionnaires to investigate the prevalence of disturbed sleep, anxiety, and depression among glaucoma patients. As compared with 17.5% of the control patients, 80% of PACG patients and 54.2% of POAG patients had a PSQI total score indicating clinically relevant sleep disturbance. Our study showed significant differences concerning different PSQI scores which could partly be caused by a circadian misalignment. Regarding anxiety in glaucoma patients, this study showed higher SAS scores among patients with glaucoma, as compared with the control group. In the whole sample, 21.7% of the control patients reached SDS scores above the predefined cut-off, whereas this percentage was 51.2% for PACG and 53.3% for POAG. Our results are in concordance with those of Mabuchi et al[16]who found a higher prevalence of anxiety and depression among glaucoma patients. Wang and colleagues have found that the ratio of POAG patients with sleep disorders grew with the aggravation of the impairment of visual field, but the differences were not statistically significant[14].
Considering the melatonin secretion are altered in patients suffering from both disturbed sleep as well as in patients suffering from major depressive disorder, the disturbances of melatonin rhythm could be related to the comorbid depression and sleep disorder in glaucoma patients[17-18]. We measured serum melatonin levels in glaucoma patients with or without psychiatric diseases and found that in patients with sleep disorders, anxiety or depression, the mean serum melatonin level was significantly higher. We evidently determined that the increase of melatonin secretion in glaucoma patients related to the sleep disorders, anxiety and depression.Increased melatonin level of patients with psychiatric problem might be explained by the reduction of the photic input to the circadian system as a result of less opportunity for exposure to bright light exposure. Furthermore, stress reaction caused by psychiatric disorders may lead to oxidative damage in retinal which also resulted in the death of IpRGCs and abnormal melatonin secretion[19].
LimitationsOur study has some limitations that deserve comment. First, we did not limit the social factors such as profession which may affect the circadian rhythm. The second limitation is the use of self-rating scales to assess sleep symptoms, anxiety and depression. Although all scales used in the current study are widely employed in research and have been chosen because of their clinical validity and reliability, a more objective index may be warranted to test the psychiatric disorders of glaucoma patients and a psychiatrist is needed to make the right diagnosis. The third limitation is that we did not analyze cup disc ratio and visual field defects in glaucoma patients and perform the glaucoma grading. Correlation analysis may help reveal association between glaucoma severity and psychiatric disorders and give further assessment of the influence of glaucoma on melatonin secretion.
There is a relatively high prevalence of sleep disturbance,anxiety and depression among glaucoma patients. At present,standard ophthalmological care for glaucoma consists mainly of the management of IOP. Considering higher comorbid levels of sleep disorders, anxiety and depression can be assumed for glaucoma patients, an additional psychiatric assessment and treatment are needed in glaucoma patients. Nevertheless,further studies are needed in order to discover a better solution for treating psychiatric disorders which in turn, have positive results in relieving the progression of glaucoma.
ACKNOWLEDGEMENTS
Conflicts of Interest:Ma XP, None; Shen MY, None; Shen GL, None; Qi QR, None; Sun XH, None.
REFERENCES
1 Chesnokova NB, Beznos OV, Lozinskaya NA, Volkova MS, Zaryanova EV, Zefirov NA, Grigoryev AV. Novel agonists of melatonin receptors as promising hypotensive and neuroprotective agents for therapy of glaucoma. Biomed Khim 2017;63(1):75-80.
2 Tosini G, Iuvone M, Boatright JH. Is the melatonin receptor type 1 involved in the pathogenesis of glaucoma? J Glaucoma 2013;22 Suppl 5:S49-S50.
3 Alkozi H, Sanchez-Naves J, de Lara MJ, Carracedo G, Fonseca B, Martinez-Aguila A, Pintor J. Elevated intraocular pressure increases melatonin levels in the aqueous humour. Acta Ophthalmol 2017;95(3):e185-e189.
4 Siu AW, Maldonado M, Sanchez-Hidalgo M, Tan DX, Reiter RJ.Protective effects of melatonin in experimental free radical-related ocular diseases. J Pineal Res 2006;40(2):101-109.
5 Agorastos A, Huber CG. The role of melatonin in glaucoma implications concerning pathophysiological relevance and therapeutic potential. J Pineal Res 2011;50(1):1-7.
6 Agorastos A, Skevas C, Matthaei M, Otte C, Klemm M, Richard G,Huber CG. Depression, anxiety, and disturbed sleep in glaucoma. J Neuropsychiatry Clin Neurosci 2013;25(3):205-213.
7 Rosen R, Hu DN, Perez V, Tai K, Yu GP, Chen M, Tone P, McCormick SA, Walsh J. Urinary 6-sulfatoxymelatonin level in age-related macular degeneration patients. Mol Vis 2009;15:1673-1679.
8 Rahman SA, Marcu S, Kayumov L, Shapiro CM. Altered sleep architecture and higher incidence of subsyndromal depression in low endogenous melatonin secretors. Eur Arch Psychiatry Clin Neurosci 2010;260(4):327-335.
9 Crasson M, Kjiri S, Colin A, Kjiri K, L’Hermite-Baleriaux M, Ansseau M, Leqros JJ. Serum melatonin and urinary 6-sulfatoxymelatonin in major depression. Psychoneuroendocrinology 2004;29(1):1-12.
10 Iuvone PM, Tosini G, Pozdeyev N, Haque R, Klein DC, Chaurasia SS.Circadian clocks, clock networks, arylalkylamine N-acetyltransferase, and melatonin in the retina. Prog Retin Eye Res 2005;24(4):433-456.
11 Anisimov VN, Vinogradova IA, Panchenko AV, Popovich IG,Zabezhinski MA. Light-at-night-induced circadian disruption, cancer and aging. Curr Aging Sci 2012;5(3):170-177.
12 Jean-Louis G, Zizi F, Lazzaro DR, Wolintz AH. Circadian rhythm dysfunction in glaucoma: a hypothesis. J Circadian Rhythms 2008;6:1.
13 Jean-Louis G, Kripke DF, Elliott JA, Zizi F, Wolintz AH, Lazzaro DR. Daily illumination exposure and melatonin: influence of ophthalmic dysfunction and sleep duration. J Circadian Rhythms 2005;3:13.
14 Wang H, Zhang Y, Ding J, Wang N. Changes in the circadian rhythm in patients with primary glaucoma. PLoS One 2013;8(4):e62841.
15 Lim NC, Fan CH, Yong MK, Wong EP, Yip LW. Assessment of depression, anxiety, and quality of life in singaporean patients with glaucoma. J Glaucoma 2016;25(7):605-612.
16 Mabuchi F, Yoshimura K, Kashiwagi K, Shioe K, Yamagata Z, Kanba S, Iijima H, Tsukahara S. High prevalence of anxiety and depression in patients with primary open-angle glaucoma. J Glaucoma 2008;17(7):552-557.
17 Khaleghipour S, Masjedi M, Ahade H, Enayate M, Pasha G, Nadery F,Ahmadzade G. Morning and nocturnal serum melatonin rhythm levels in patients with major depressive disorder an analytical cross sectional study.Sao Paulo Med J 2012;130(3):167-172.
18 Bay E, Donders J. Risk factors for depressive symptoms after mild-tomoderate traumatic brain injury. Brain Inj 2008;22(3):233-241.
19 Brotto LA, Gorzalka BB, LaMarre AK. Melatonin protects against the effects of chronic stress on sexual behaviour in male rats. Neuroreport 2001;12(16):3465-3469.
Co-first authors:Xiao-Ping Ma and Man-Yi Shen
Correspondenceto:Xing-Huai Sun. Department of Ophthalmology, Eye & Ent Hospital of Fudan University, No. 83 Fenyang Road, Xuhui District, Shanghai 200031, China.xhsun@shmu.edu.cn
Received:2017-03-25 Accepted: 2018-06-07
Abstract● AlM: To determine whether glaucoma patients exhibit an abnormal melatonin concentration in serum and the effects of psychiatric disorders caused by glaucoma in melatonin secretion.● METHODS: A sample of 80 primary angle-closure glaucoma(PACG) patients, 120 primary open angle glaucoma (POAG)patients, and 120 normal controls were enrolled in this study. All the participants were asked to complete the following questionnaires: Pittsburgh sleep quality index(PSQl), self-rating anxiety scale (SAS), and self-rating depression scale (SDS). Variance analysis was used to compare the subscores between the groups. After that,we chose 58 patients with primary glaucoma and 20 nonglaucoma control patients to collect their serum samples at 7-10 a.m. Serum melatonin levels were measured using enzyme linked immunosorbent assay (ELlSA).● RESULTS: Of all participants, the scores of PSQl, SAS, and SDS in PACG and POAG group were 9.38±0.40, 46.08±8.99,51.11±10.72 and 7.43±0.35, 45.42±9.87, 49.04±12.24 respectively,significantly higher than those in control group (4.16±0.28,35.49±9.18, 40.31±13.08). The serum melatonin levels in PACG (37.29±2.99 pg/mL) and POAG (35.97±3.64 pg/mL) were significantly higher than the controls (29.96±3.94 pg/mL)(P<0.001). But no difference was found between the PACG and POAG (P=0.216). Glaucoma patients with sleep disorders, anxiety and depression were more likely resulting in the increase of melatonin levels.● CONCLUSlON: There is a significant increase in serum melatonin levels in glaucoma patients compared to the controls especially in glaucoma patients with psychiatric disorders such as sleep disorders, anxiety and depression.
● KEYWORDS:glaucoma; melatonin; circadian rhythm; sleep disorder; anxiety; depression
DOl:10.18240/ijo.2018.08.14
Citation:Ma XP, Shen MY, Shen GL, Qi QR, Sun XH. Melatonin concentrations in serum of primary glaucoma patients. Int J Ophthalmol 2018;11(8):1337-1341