
Figure 1 The development of the Knapp procedure A: Traditional Knapp procedure; B, C: Standard Knapp procedure (modified); D:Augmented Knapp procedure[9]. MR: Medial rectus muscle; SR:Superior rectus muscle; LR: Lateral rectus muscle.
Wen-Ting Luo, Tong Qiao, Hai-Yun Ye, Si-Hong Li, Quan-Li Chen
Shanghai Children’s Hospital Affiliated to Shanghai Jiao Tong University, Shanghai 200062, China
M onocular elevation deficiency (MED) is defined as the inability to elevate one eye equally in abduction,adduction, and primary gaze. MED was originally termed double elevator palsy (DEP) when the disorder was thought to be caused by paresis of the two eye elevators, the superior rectus(SR) and inferior oblique (IO)[1]. When the sound eye is fixed,the paralyzed eye appears to be hypotropic and pseudoptotic.When the paralyzed eye is fixed, the ptosis disappears, and the sound eye appears to be hypertropic. Pseudoptosis may cover the true vertical deviation, leading clinicians to misdiagnose it as congenital ptosis and then to perform a ptosis correction surgery. In the same way, Von Noorden[2]attributed DEP to long-term palsy of the SR in the presence of a normally functioning IO muscle, suggesting that the motor signs may be attributed to SR paralysis alone. Jampel and Fells[3]suggested a unilateral supranuclear lesion in the pretectal area near or inside the third cranial nerve nucleus in some cases. Scott and Jackson[4]stressed the importance of concomitant restriction caused by a tight inferior rectus (IR) muscle as the cause or sequel of DEP. Using a scleral search coil technique for evaluating saccadic velocities, Ziffer et al[5]classified DEP into three subgroups of IR restriction: complete or incomplete SR palsy and supranuclear palsy. MED is a congenital disease that requires surgical treatment. Knapp[6]created the traditional Knapp procedure. The medial and lateral rectus muscles are placed across the corners of the insertion of the SR as depicted in Figure 1A. Because of eye rotation caused by the traditional Knapp procedure, we adopted the standard Knapp procedure:we fix the upper ends of the medial and lateral rectus muscle to the nasal and temporal insertion sides of the SR muscle and then fix the bottom ends to the corresponding shallow sclera along Tenon’s capsule (Figure 1B, 1C). In addition to enhancing the elevation of the transposition, by closing the gap of interrelation between the medial rectus or lateral rectus and SR muscle, Snir[7]created and named the augmented Knapp procedure (Figure 1D). The purpose of this study was to evaluate various surgical outcomes between the standard and augmented Knapp procedures based on improvements in the vertical deviation and ocular motility in young children.
The study was approved by the Institutional Review Board of Shanghai Children’s Hospital (approval No.2016R032-F01)and was performed in accordance with the tenets of the Declaration of Helsinki. Written informed consent was obtained from the patients.
We reviewed 22 MED patients undergoing surgery at Shanghai Children’s hospital from July 2014 to January 2018, including 17 males and 5 females. One patient with positive forced duction test (FDT) was excluded. In 21 cases, the FDT was negative. The patients were aged 8mo to 12y (mean 5.4y).Twenty-one patients were classified into 2 groups as follows:group A (n=16) underwent the standard Knapp procedure;group B (n=5) underwent the augmented Knapp procedure(Foster procedure). The cases of limited supraduction due to Brown syndrome, thyroid ophthalmopathy, orbital fractures and malignancies, as well as cases with previous SR weakening, were excluded. Preoperative evaluation included the assessment of visual acuity (VA), pupillary function, cycloplegic refraction, eye movements, slit lamp examination and ophthalmoscopy. The children were assessed for VA using the E letter matching test if the child was cooperative and by the fixation reflex of “central, steady, and maintained” if they were not cooperative. Alignment was measured by the alternative prism cover test in patients with good VA and cooperation and by the modified Krimsky test in preverbal children looking at a distant accommodative target. Neutralizing prisms were held in front of the eye with DEP to measure the primary deviation. The degree of motility restriction was recorded using a conventional method from -1 to -4, each grade representing a 25% upward limitation from the horizontal midline. FDT was performed in the operating room after general anesthesia using non-depolarizing muscle relaxants in all cases.

Figure 1 The development of the Knapp procedure A: Traditional Knapp procedure; B, C: Standard Knapp procedure (modified); D:Augmented Knapp procedure[9]. MR: Medial rectus muscle; SR:Superior rectus muscle; LR: Lateral rectus muscle.
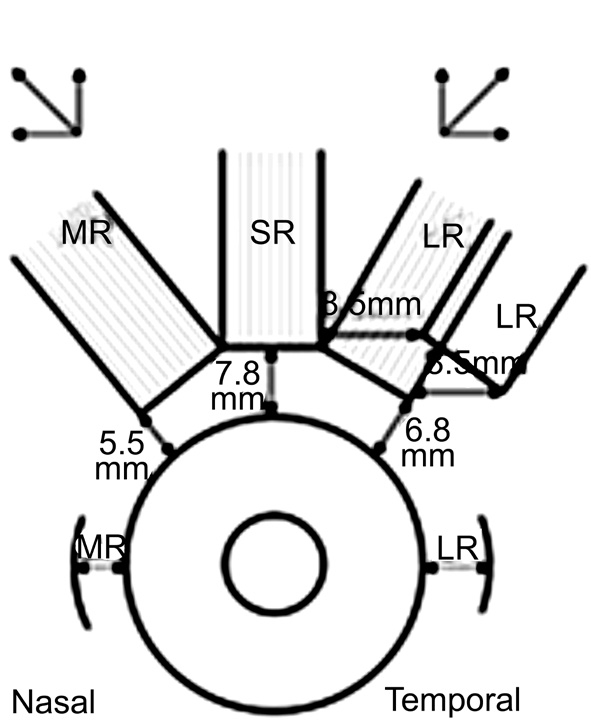
Figure 2 Standard Knapp and lateral rectus recession procedure.
If the FDT was positive, it meant that elevation was restricted.The choice of the IR recession in the paralyzed eye combined with the SR recession in the sound eye (R&R) is common. The amount of surgery is primarily based on the first squint angle.If the FDT was negative, it meant that elevation was paralyzed.The choice of undergoing the standard Knapp procedure (full medial and lateral rectus transposition towards SR) (Figure 1B, 1C) or augmented Knapp procedure[7]depended on various vertical deviations and ocular motility disorders. Snir[7]designed the augmented Knapp procedure (Figure 1D). The procedure was similar to the Foster[8]procedure, only the SR muscle replaced the lateral rectus muscle. In the augmented transposition procedure, a non-absorbable 5-0 polyester(Dacron) suture (Ethicon, Somerville, NJ, USA) was placed in the sclera, 8.0 mm posterior to the insertion of the paralyzed extraocular muscle (EOM), near the upper and lower borders,thereby fixing 25% of the belly of each transposed muscle adjacent to the paralyzed SR muscle. This procedure closed the gap between the transposed rectus muscle and the paralyzed SR muscle. If there was monocular elevation deficiency with horizontal squint, we always adopted combination surgery according to the normal procedure dose (Figure 2) to ensure that there was no anterior segment ischemia in the case of surgery with simultaneous recession and resection of the medial and lateral rectus.In this study, we analyzed long-term alignment and elevation improvement. The cure standard was defined as a final vertical residual deviation ≤10 prism diopter (PD) and ≥25% elevation improvement after operation. The follow-up for group A ranged from 6 to 36mo (mean 21mo), and that of group B ranged from 6 to 35mo (mean 18mo).
Table 1 Pre- and postoperative evaluations of group A
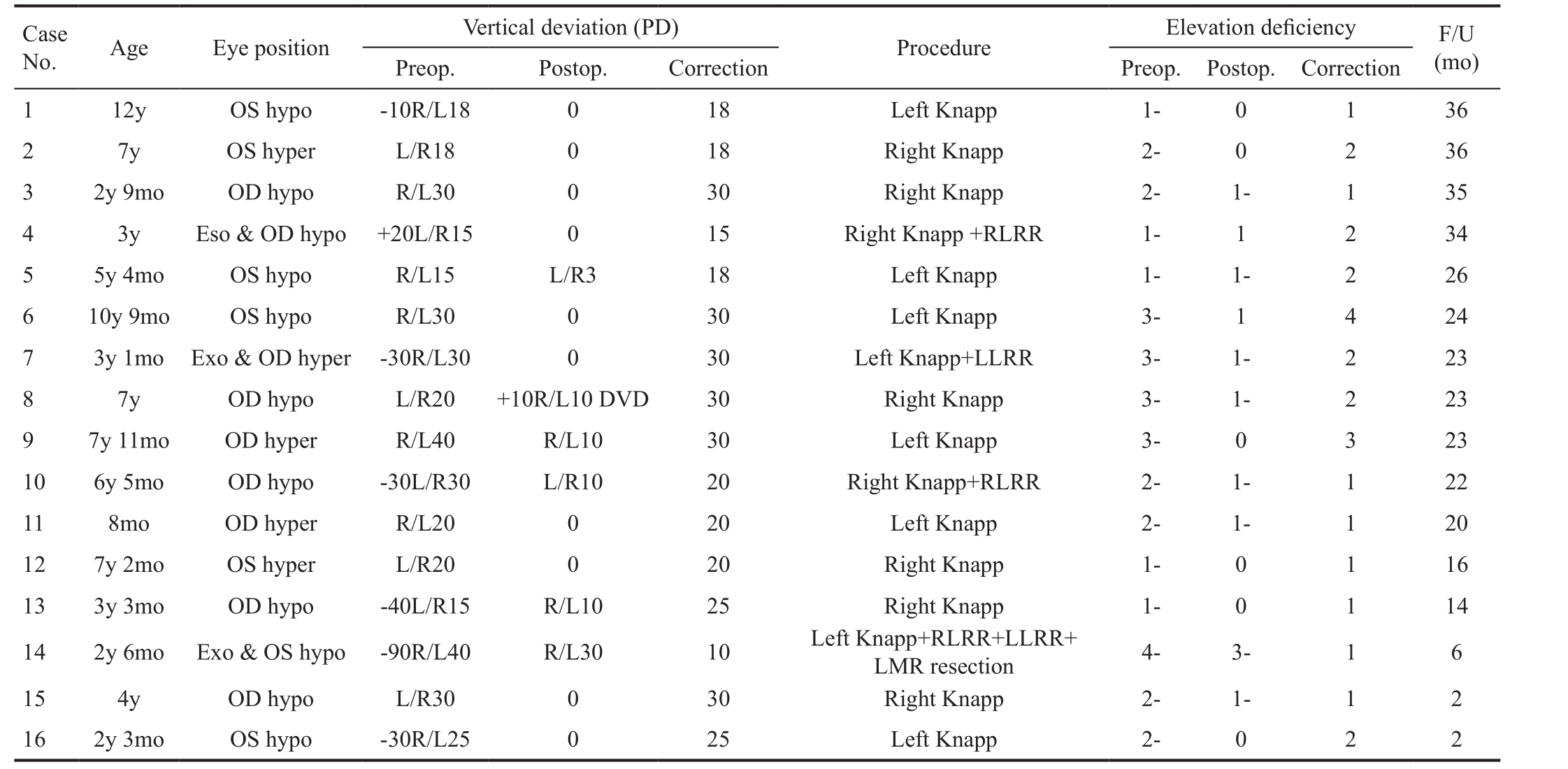
PD: Prism diopter; Hypo: Hypotropia; Hyper: Hypertropia; RLRR: Right lateral rectus recession; LLRR: Left lateral rectus recession; LMR:Left medium rectus; Exo: Exotropia; Eso: Esotropia; F/U: Follow-up.
Table 2 Pre- and postoperative evaluations of group B
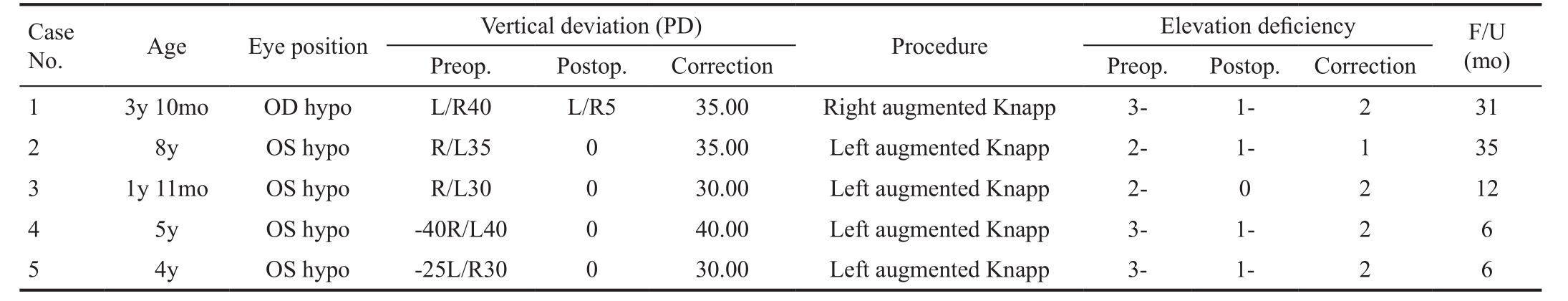
PD: Prism diopter; Hypo: Hypotropia.
Statistical AnalysisStatistical analysis was performed using IBM SPSS Statistics version 21. The results, where appropriate, were reported as the mean and standard deviations. A pairwise comparison between the preoperative and postoperative values was performed by applying the nonparametric Wilcoxon signed-rank test. Differences observed in corrected vertical deviation and elevation deficiency among the two groups were analyzed by the non-parametric Mann-Whitney U test. P˂0.05 was considered significant.
Among the 21 patients, preoperatively, the best corrected VA of the paralyzed eyes was 1.0, while the worst was 0.1. Six cases of patients could not cooperate to measure VA. Nine cases were affected in the right eye, 12 cases were affected in the left eye, and only 3 cases had stereo vision before the procedure; the other patients had no stereo vision. Eight patients had horizontal strabismus, including 7 with exotropia and 1 with esotropia.
The vertical deviation and elevation deficiency were comparable pre- and postoperatively in group A. We also observed age, eye position, surgical procedure and follow-up periods (Table 1). Group B is also shown in Table 2.
The average corrected vertical deviation in group B(augmented Knapp) was statistically better than that of group A (standard Knapp) (Z=-2.897, P=0.003). For group A, the vertical deviation in the primary position decreased from 24.75Δ±8.35Δ (range, 15Δ-40Δ) to 4.56Δ±8.07Δ after surgery(range, 0Δ-30Δ), for an improvement of 23.06Δ±6.51Δ(Z=-3.532 P˂0.05). In group B, the vertical deviation in the primary position decreased from 35.00Δ±5.00Δ (range,30Δ-40Δ) to 1.00Δ±2.24Δ (range, 0Δ-5Δ), for an improvement of 34.00Δ±4.18Δ (Z=-2.041 P=0.041). There were significant differences between the pre- and postoperative elevations in each group (group A, P˂0.05; group B, P˂0.05). The average scale of improved elevation in group B (1.80±0.45) was notstatistically significantly better than that of group A (1.69±0.87;Z=-0.732 P=0.548; Table 3).
Table 3 Pre- and postoperative evaluations of the two study groups mean±SD
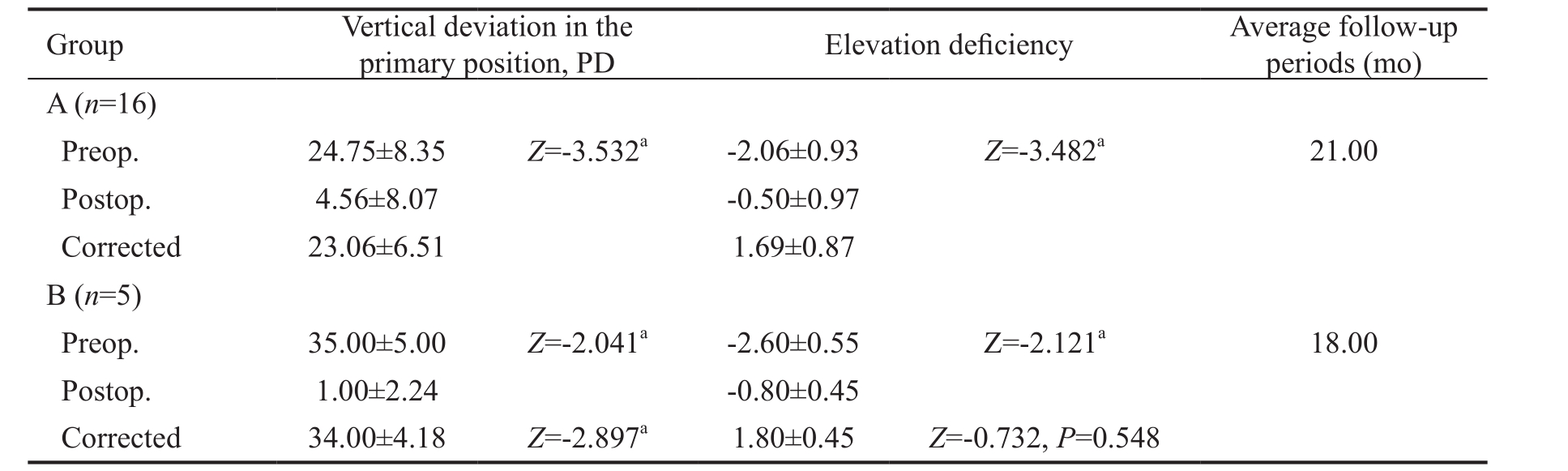
PD: Prism diopter; SD: Standard deviation.aP˂0.05.
The details of the vertical deviation change pre- and postoperatively were provided in each case: group A, 1-16;group B, 17-21 (Figure 3). The detailed vertical deviations changed pre- and postoperatively in each case: group A, 1-16;group B, 17-21 (Figure 4).
In 1 case, the FDT was positive, so IR recession was performed. After 1.5y of follow-up, we found another eye with elevation deficiency, and FDT was positive before surgery; we performed the same procedure in the second eye. All patients were positive for Bell’s sign, in which 2 patients had true ptosis and 1 patient had Marcus-Gunn syndrome. In 15 cases,the sound eyes were dominant, and in 6 cases, the paralyzed eye was fixed. Only 3 patients maintained binocular vision in the downgaze position before surgery. Most patients have no stereo acuity. At follow-up visit after surgery, 21 cases (95%)were within 10 PD of orthotropia, and all patients (100%)reached ≥25% elevation improvement after surgery.
One 7-year-old patient was found to have bilateral dissociated vertical deviation (DVD) with small esotropia after the surgery.We used 1% atropine cycloplegic refraction, and moderate hypermetropia showed. We prescribed adequate hypermetropia spectacles and esotropia disappeared with glasses.
There was one MED case with unilateral coronal synostosis, a 3-year-old girl. Six months after craniofacial reconstruction, we adopted the Knapp procedure in the left eye to correct MED and lateral rectus recession in right eye to correct exotropia,obtaining a good outcome after 2mo follow-up. Before surgery,the child with unilateral coronal synostosis had compensatory head posture; the Knapp procedure in the left eye and lateral rectus recession in the right eye were performed. After surgery, the compensatory head posture disappeared. From Figure 5A and Figure 5B, we can observe the malformation of the child’s skull, especially left coronal synostosis. The craniofacial deformity was caused by premature closure of the coronal synostosis. After the craniotomy, the frontal bone shifted anteriorly, and the child’s skull was restored to ideal appearance (Figure 5C, 5D).
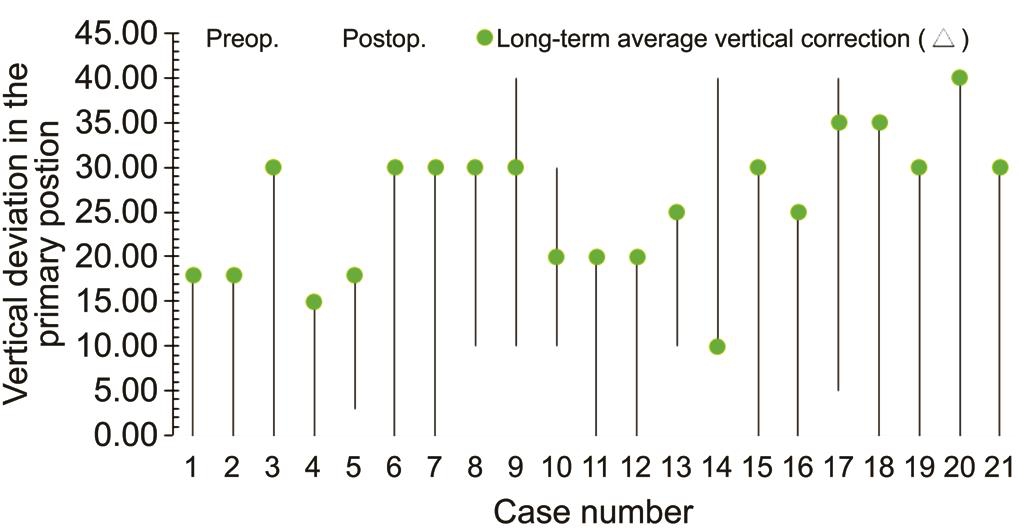
Figure 3 The vertical deviation change (Δ) preoperative and postoperatively in the primary position Δ: Prism diopter (PD).
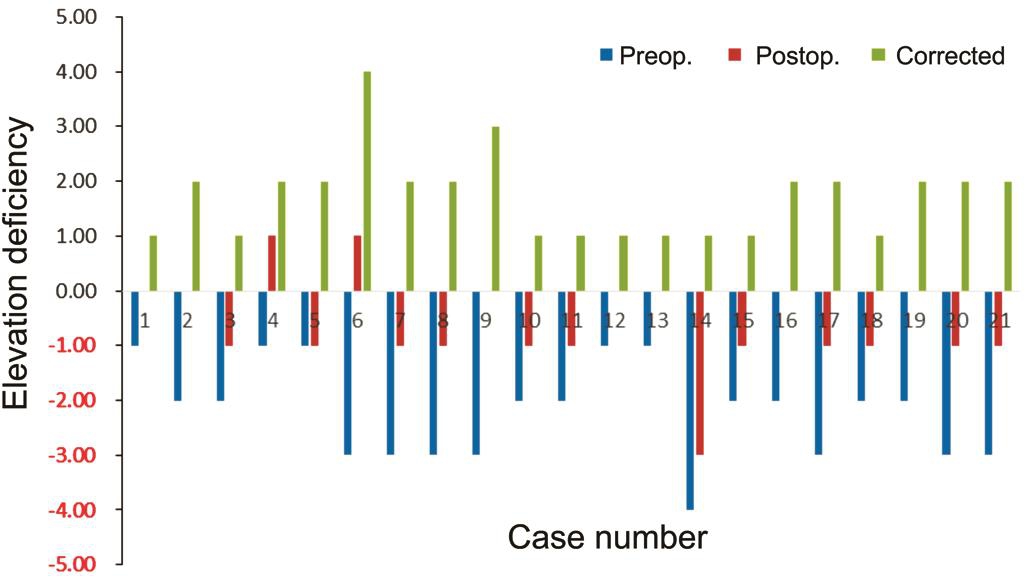
Figure 4 The corrected elevation deficiency change pre- and postoperatively.
The nine-gaze positions of a patient showed deficient elevation of the left eye both in adduction and abduction preoperatively(Figure 6A). Two months follow-up after the Knapp procedure,the elevation deficiency had recovered (Figure 6B). The average follow-up periods lasted 21mo in group A and 18mo in group B. No obvious complications occurred in any patients.
In our study, the augmented Knapp procedure corrected more vertical deviation than did the standard Knapp procedure. The standard Knapp procedure corrected average vertical deviation was 23.06Δ±6.51Δ, while that of the augmented Knapp procedure was 34.00Δ±4.18Δ (Table 3). This result was similar to that of recent studies.
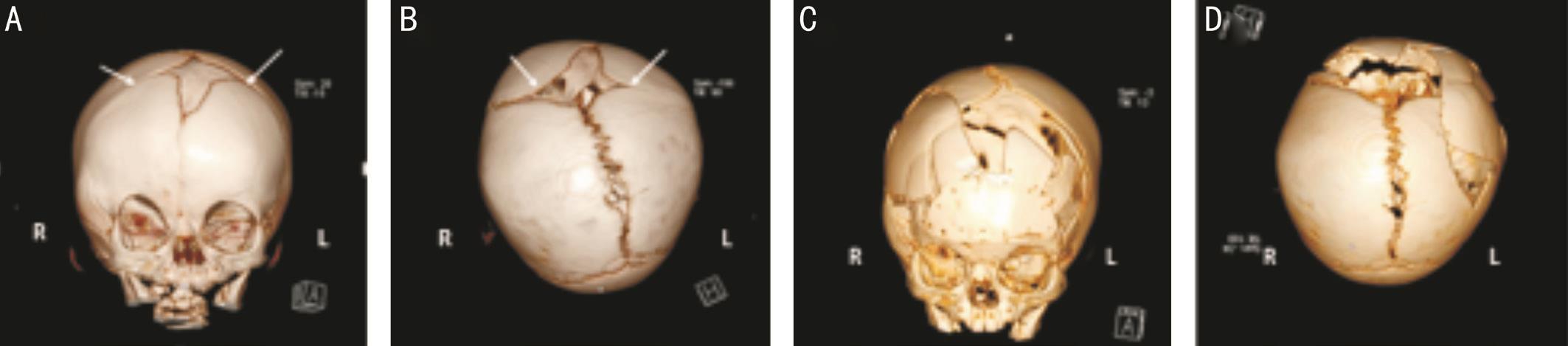
Figure 5 The 3D reconstruction of computer tomography (CT) scan of the child with unilateral coronal synostosis, pre- and postoperative craniotomy The white arrowhead refers to the coronal seams. A, B: Images were taken one week before craniotomy, when the child was 6mo old; C, D: Images were taken one week after craniotomy surgery; A, C: Coronal position; B, D: Horizontal position.
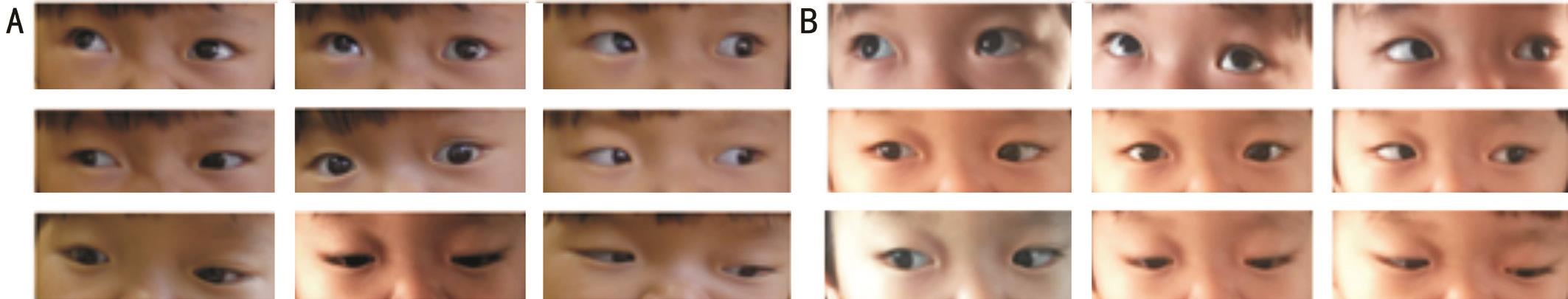
Figure 6 Alignment before and after surgery in this case A: Nine-gaze positions of the patient showing deficient elevation of the left eye both in adduction and abduction; B: Two months after surgery, the eye elevation improved significantly pre- versus postoperatively.
Knapp[6]created and reported 15 MED undergoing the Knapp procedure. The range 21Δ-55Δ (mean 38Δ) was corrected.Watson[10]corrected an average of 30.5Δ. Barsoum-Homsy[11]corrected an average of 31.7Δ in 4 patients. All of the above studies were performed with the traditional Knapp procedure.We found that the standard Knapp procedure could correct ˂30Δ vertical deviation. Zafar et al[12]reported 12 FDT-negative cases and performed the Knapp procedure. Zhuang et al[13]operated on 2 cases and corrected them 29Δ and 32Δ.Talebnejad et al[14]operated on 4 cases, and corrected an average of 20Δ. In our study, the augmented Knapp corrected 30-40Δ. Snir et al[7]compared the outcome of the augmented procedure with that of the standard Knapp procedures and found: 1) a greater decrease in the hypotropia deviation; 2) a greater improvement in the elevation deficiency and 3) a lower rate of reoperation. After 15.4mo of observation, no surgical complications or abnormal changes occurred. Li et al[9,15]performed 7 augmented Knapp procedures with a corrected average 32.8Δ±5.7Δ.
However, the results in this study indicated that the augmented Knapp procedure (1.80±0.45) did not show a substantially different improved elevation compared with the postoperative results of the standard Knapp procedure (1.69±0.87). The Knapp procedure corrected primary position deviation much more than it recovered ocular motility; the right eye alignment benefitted for binocular vision and head position; perhaps in this condition, we will sacrifice up-gaze eye movement. In recent studies, Snir et al[7]and Li et al[9,15]found that Foster transposition demonstrated the strongest effect in improving up-gaze.
In this study, only 1 out of 22 patients had IR restriction, which is different from recent studies. Metz et al[16]reported 80%patients to be PDT (+). Wright and Spigel[17]thought that the factor of IR restriction occupied 70% of the causes of MED.Scott and Jackson[4]reported that IR restriction occupied 73.3%. This incidence was similar to that found in the Awadein and El-Fayoumi’s[18]study (76%). In our study, patients were young: children from 8mo to 12y were included (mean 5.44y).Because of our early interference, the IR muscle had not shown mechanical restriction. MED needs early diagnosis and early treatment for complication to be reduced and easy and for surgery to be easier for the surgeon. In our study, only 3 patients had binocular vison, and the remaining cases had no binocular function; abnormal head position might compensate the balance of both eyes, and the other cases without binocular function may be due to MED causing early monocular suppression and amblyopia in early childhood, affecting the formation and development of binocular vision. Large-angle hypotropia often accompanied by ptosis is also an important factor that destroys binocular vision. Meanwhile, when suffering from large hypotropia, most congenital MED patients often have no binocular vision. Small-angle hypotropia by elevating the chin overcomes diplopia, thereby preserving binocular vision. There have been a few cases reported studying the stability of eye position after transposition; Buck et al[19]assessed the effect of the Knapp procedure increasing with time. In the primary position, the presence of vertical deviation, diplopia, amblyopia and binocular visual field range restriction meant the need for surgery[9]. By improving the primary position, we can increase the binocular visual field.
If FDT is negative, the patients have MED or supranuclear palsy, and they need to undergo the Knapp procedure. For more than 30Δ vertical deviation, the Foster procedure should be adopted. In contrast, Kamlesh et al[20]performed R&R surgery even if FDT was negative, showing a success rate of 92.31% with a mean correction of 47.30 PD and improvement in elevation as well as Bell’s sign. For MED with horizontal squint, we always adopted combination surgery according to normal procedure dose (Figure 2); we believed that the Knapp procedure would not influence the horizontal alignment. Zafar performed 12 Knapp procedures combined with the horizontal procedure and achieved the ideal effect[11].
One 7-year-old patient exposed bilateral DVD with small esotropia after the surgery. We diagnosed her as having accommodative esotropia; with follow-up, the DVD was controlled.We believe the right alignment will help to control the DVD.One MED case had unilateral coronal synostosis (a type of craniosynostosis syndrome); it was the first time to report MED in craniosynostosis syndrome; strabismus surgery must be done after craniofacial reconstruction, because decreasing intracranial pressure is the most important choice.Craniosynostosis (or craniostenosis) is the premature fusion of one or more cranial sutures. This condition can occur in association with more than 130 different syndromes, and V-pattern strabismus is common in craniostenosis[21].
The choice of a reasonable surgical method can not only correct primary deviation but can also improve ocular motility.If FDT is positive, one needs to recess the IR. For our early interference, the IR muscle has not shown mechanical restriction, and recession surgery could be avoided. If PDT is negative, the Knapp procedure could be considered, using either the standard or augmented Knapp procedure. For a vertical deviation of ˂30Δ, we can choose the standard Knapp procedure. For a greater deviation of 30Δ-40Δ, the Foster procedure should be adopted. In conclusion, although the etiology is complicated, if the proper operation is selected,most cases with monocular elevation deficiency can achieve good therapeutic outcomes.
The authors thank all of the patients and their families.
Conflicts of Interest: Luo WT, None; Qiao T, None; Ye HY,None; Li SH, None; Chen QL, None.
REFERENCES
1 White J. Paralysis of the superior rectus and the inferior oblique muscle of the same eye. Arch Ophthalmol 1942;27(2):366-371.
2 Von Noorden GK. Binocular vision and ocularmotility. 6th ed. ST Louis: Mosby; 2002.
3 Jampel RS, Fells P. Monocular elevation paresis caused by a central nervous system lesion. Arch Ophthalmol 1968;80(1):45-57.
4 Scott WE, Jackson OB. Double elevator palsy: the significance of inferior rectus restriction. Am Orthopt J 1977;27:5-10.
5 Ziffer AJ, Rosenbaum AL, Demer JL, Yee RD. Congenital double elevator palsy: vertical saccadic velocity utilizing the scleral search coil technique. J Pediatr Ophthalmol Strabismus 1992;29(3):142-149.
6 Knapp P. The surgical treatment of double-elevator paralysis. Trans Am Ophthalmol Soc 1969;67:304-323.
7 Snir M, Friling R, Kalish-Stiebel H, Bourla D, Weinberger D, Axer-Siegel R. Combined rectus muscle transposition with posterior fixation sutures for the treatment of double-elevator palsy. Ophthalmology 2005;112(5):933-938.
8 Foster RS. Vertical muscle transposition augmented with lateral fixation.J AAPOS 1997;1(1):20-30.
9 Li YP, Zhang W, Ding J, Ma HZ, Zhao KX. Knapp procedure and modified knapp procedure with foster suture for the treatment of double elevator palsy. Zhonghua Yan Ke Za Zhi 2017;53(12):903-907.
10 Watson A. A new operation for double elevator paresis. Trans Can Ophthalmology Soc 1962;25:182.
11 Barsoum-Homsy M. Congenital double elevator palsy. J Pediatr Ophthalmol Strabismus 1983;20(5):185-191.
12 Zafar SN, Azad N, Khan A. Outcome of surgical treatment of monocular elevation deficiency. J Pak Med Assoc 2012;62(4):355-357.
13 Zhuang J, Pan M, Ren X, Xiu Y, Xie R. Clinical features and surgical treatment in congenital double elevator paralysis. Chinese Journal of Ophthalmologic Medicine (Electronic Edition) 2012;2(1):17-21.
14 Talebnejad MR, Roustaei GA, Khalili MR. Monocular elevation deficiency: a case series of surgical outcome. Iran J Med Sci 2014;39(2):102-106.
15 Li Y, Sun L, Zhang W, Zhao K. Comparison of augmented and nonaugmented modified knapp procedure for the treatment of nonrestrictive double elevator palsies. J AAPOS 2016;20(5):401-404.
16 Metz HS. Double elevator palsy. Arch Ophthalmol 1979;97(5):901-903.
17 Wright K, Spigel P. Pediatric ophthalmology and strabismus. 2nd ed.New York: Springer;2003.
18 Awadein A, El-Fayoumi D. Surgical management of monocular elevation deficiency combined with inferior rectus restriction. J AAPOS 2015;19(4):316-321.
19 Burke JP, Ruben JB, Scott WE. Vertical transposition of the horizontal recti (Knapp procedure) for the treatment of double elevator palsy:effectiveness and long-term stability. Br J Ophthalmol 1992;76(12):734-737.
20 Kamlesh, Dhiman S, Thacker P, Karothiya B, Goel Y, Rastogi A,Chaudhary R. To assess the efficacy of vertical muscle surgery for management of hypotropia in monocular elevation deficiency type II. Int Ophthalmol 2017;37(4):1009-1016.
21 Qiao T, Wang G, Xiong J, Luo W, Chen J. Surgical treatment of V-pattern exotropia in crouzon syndrome. J Pediatr Ophthalmol Strabismus 2015;52(5):299-304.
Correspondenceto:Tong Qiao. Shanghai Children’s Hospital Affiliated to Shanghai Jiao Tong University, 355 Luding Road,Shanghai 200062, China. Qiaojoel@163.com
Received:2018-03-14 Accepted: 2018-06-26
Abstract● AlM: To describe the clinical features of congenital double elevator palsy (CDEP) and to evaluate various surgical outcomes between the standard Knapp and augmented Knapp procedures, based on improvements in primary eye position and ocular motility.● METHODS: Twenty-two patients with CDEP at Shanghai Children’s Hospital were enrolled from July 2014 to January 2018. The forced duction test (FDT) was negative in 21 patients, aged 8mo to 12y (mean 5.4y). Patients were divided into two treatment groups: 16 patients underwent the standard Knapp procedure (group A), with or without horizontal squint procedure; and 5 patients underwent the augmented Knapp procedure (Foster procedure; group B). One patient underwent inferior rectus recession in the affected eye and superior rectus recession in the sound eye because of a positive FDT. The pre- and postoperative vertical deviations in the primary position and ocular motility were compared in the two groups.● RESULTS: Twenty-one eyes of the 22 patients (95%)were aligned within 10 prism diopters (PD), and all patients(100%) reached ≥25% elevation improvement after surgery.The average corrected vertical deviation in group B was statistically better than that of group A. For group A,the vertical deviation in the primary position decreased from 24.75Δ±8.35Δ to 4.56Δ±8.07Δ after surgery, for an improvement of 23.06Δ±6.51Δ (P<0.05). ln group B, the decrease was from 35.00Δ±5.00Δ (range 30Δ-40Δ) to 1.00Δ±2.24Δ, for an improvement of 34.00Δ±4.18Δ (P<0.05).There were significant differences between the pre- and postoperative elevation in each group (group A, P<0.05;group B, P<0.05). The average scale of improved elevation in group B (1.80±0.45) was not significantly better than that of group A (1.69±0.87; Z=-0.732, P=0.548). The average follow-up periods lasted 21mo in group A and 18mo in group B.● CONCLUSlON: For vertical deviations <30Δ, the standard Knapp procedure can be chosen. For deviations greater than 30Δ-40Δ, the Foster procedure should be chosen.Because of our early interference, the inferior rectus (lR)muscle did not show mechanical restriction. Monocular elevation deficiency (MED) should be diagnosed early so that complications will be reduced and the procedure will be easier for the surgeon.
● KEYWORDS:monocular elevator deficiency; double elevator palsy; forced duction test; inferior rectus recession;standard Knapp procedure; augmented Knapp procedure
DOl:10.18240/ijo.2018.08.16
Citation:Luo WT, Qiao T, Ye HY, Li SH, Chen QL. Clinical features and surgical treatment of double elevator palsy in young children. Int J Ophthalmol 2018;11(8): 1352-1357