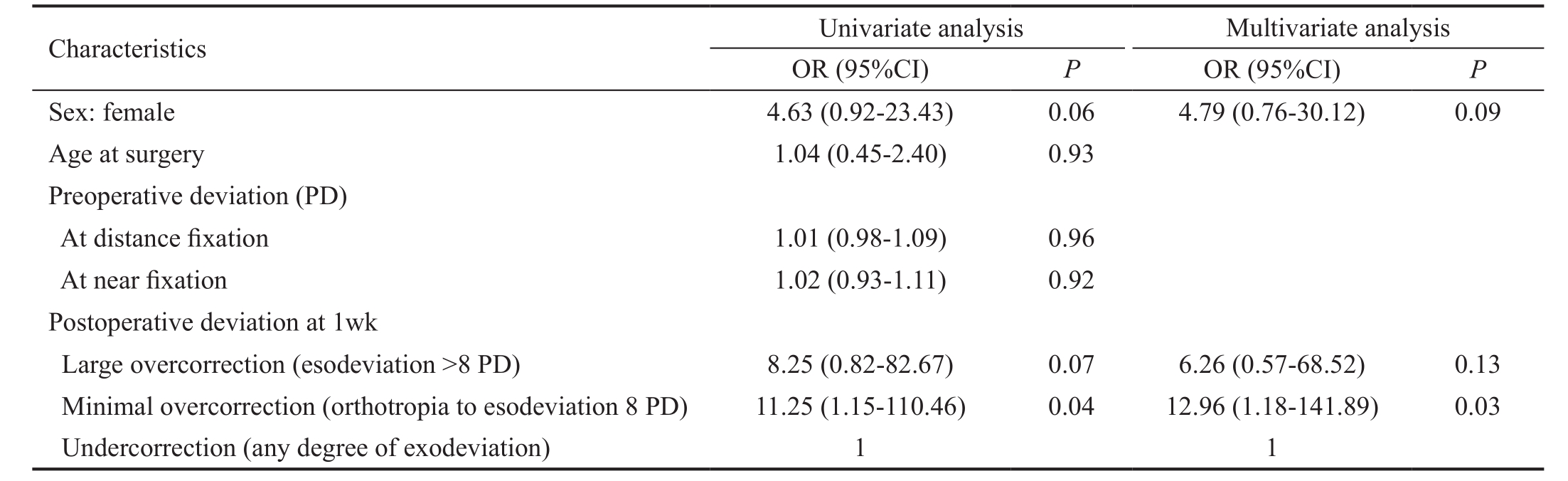
Table 1 Comparison of preoperative characters of patients in each outcome group at 2y
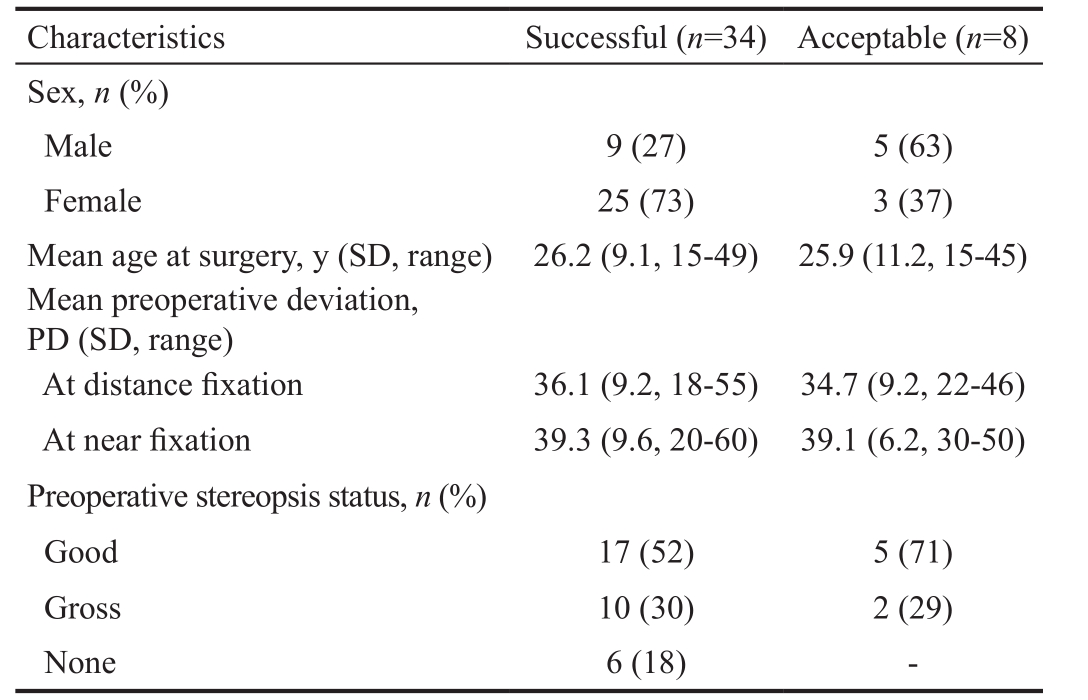
SD: Standard deviation; PD: Prism diopter.
Ponnarun Kanjanawasee1,2, Pokpong Praneeprachachon1,3, Parnchat Pukrushpan1
1Department of Ophthalmology, Faculty of Medicine,Chulalongkorn University, Bangkok 10330, Thailand
2Department of Ophthalmology, Faculty of Medicine, Burapha University, Chonburi 20131, Thailand
3Rutnin Eye Hospital, Bangkok 10110, Thailand
Exodeviation affects approximately 0.5%-1% of the population and is more common in the Asian population[1-4].Untreated patients may have progression of deviation to manifest tropia and loss of their binocular vision. Moreover,exodeviation may cause uncomfortable symptoms, such as asthenopia and diplopia, and may also affect their appearance.Several surgical procedures are used for correction of exotropia. Unilateral recession and resection surgery is one of the preferred choices, especially for the basic type of intermittent exotropia[5]. Many studies have reported that unilateral recession and resection surgery has a satisfactory outcome[6-11]and a lower recurrent rate[10-13]. The factors associated with a successful outcome have also been studied.Many previous studies have recommended that overcorrection in the early postoperative period is required for a satisfactory outcome[14-20]. However, the appropriate amount of initial deviation remains unclear. Furthermore, most previous studies investigated in all age groups, mainly children, and few reports on just adult exodeviation are available[20-21].
This study aimed to evaluate the relationship between early postoperative deviation and long-term outcome after unilateral recession and resection surgery for adult exotropia, and to evaluate exotropic shift after unilateral recession and resection surgery.
This study was approved by the institutional review board of King Chulalongkorn Memorial Hospital (IRB number 001/57)and Rutnin Eye Hospital. The study followed the tenet of Declaration of Helsinki and is registered in the Thai Clinical Trial Registry (TCTR20141023001).
Medical records of patients with exotropia who underwent unilateral lateral rectus recession with medial rectus resection at King Chulalongkorn Memorial Hospital or Rutnin Eye Hospital between April 2005 and October 2012 were reviewed.Patients who had surgery at the age of 15y or older and had a postoperative follow-up period of at least 2y were included.The surgery was performed by 1 of 2 surgeons (Pukrushpan P and Praneeprachachon P) using the same surgical technique.An adjustable suture technique was used in co-operative patients.Exclusion criteria were paretic or restrictive strabismus,sensory exotropia, a history of previous strabismus surgery,additional oblique or vertical muscle surgery, amblyopia with best corrected visual acuity worse than 20/40, and coexisting ocular disease apart from refractive error.
We contacted every patient who was lost to follow-up or who had a postoperative follow-up of less than 2y. Patients were provided necessary information regarding the study and were asked to visit the hospital for a follow-up. On the follow-up day, informed consent was obtained.
Data collection included age at surgery, sex, best corrected Snellen visual acuity, types of exotropia, preoperative and postoperative sensory status, preoperative and postoperative distance (6 m) and near (0.3 m) deviation at 1wk, 1, 6mo, 1,2y, and longer until their final visit.
The deviation was measured by the alternate prism cover test. Types of exotropia were classified preoperatively as basic, divergence excess, or convergence insufficiency, based on distance-near disparity after 1h of monocular patching.Initial postoperative deviation was the distance deviation at 1wk. We categorized initial postoperative deviation into large overcorrection [esodeviation˃8 prism diopters (PD)],minimal overcorrection (orthotropia to esodeviation 8 PD), and undercorrection (any degree of exodeviation).
Motor outcome, the distance deviation at the 2-year followup and the last follow-up were categorized into 3 groups:successful, acceptable, and poor. A successful motor outcome was defined as orthotropia or esodeviation ≤8 PD or exodeviation ≤10 PD. An acceptable outcome was defined as exodeviation of 11-20 PD. A poor outcome was defined as esodeviation ˃8 PD or exodeviation ˃20 PD.
Sensory status was evaluated by the Titmus stereo test and was divided into 3 groups: good, gross, and none. A good status was defined as stereopsis ˂70 seconds of arc, gross as stereopsis of 70-3000 seconds of arc, and none as stereopsis ˃3000 seconds of arc.
Statistical AnalysisUnivariable and multivariable binary logistic regression analysis were used to identify factors associated with a successful outcome. Mean postoperative deviation at the subsequent follow-up was compared usingthe generalized estimating equation. Kaplan-Meier survival analysis was used for assessing surgical outcome with time. P values ˂0.05 were considered statistically significant. All data analyses were performed using the Statistical Package for the Social Sciences for Windows (SPSS, Version 22.0, Chicago,IL, USA).
Table 1 Comparison of preoperative characters of patients in each outcome group at 2y
SD: Standard deviation; PD: Prism diopter.
Initially, 72 patients were eligible for the study. Among these patients, 30 were excluded because of missing medical records, wrong contact information, and patients refused to come for follow-up because of transportation problems.Finally, a total of 42 patients were included in this study. There were 14 men (33%) and 28 women (67%). Most patients had intermittent exotropia (33 patients, 79%) of whom 32 (97%)of them had the basic type. Only 1 patient had the convergence insufficiency type. The mean age at surgery was 26y [standard deviation (SD), 9.4; range, 15-49y]. The median postoperative follow-up period was 30mo (interquartile range, 24-48mo;range, 24-108mo). All patients underwent surgery under general anesthesia. Suture adjustment under topical anesthesia was performed in 32 (76%) patients.
Mean preoperative exodeviation was 36 PD at distance fixation(SD, 9.1; range, 18-55 PD) and 39 PD at near fixation (SD,9.0; range, 20-60 PD). For preoperative stereopsis status,22 (55%), 12 (30%), and 6 (15%) patients had good, gross, and no stereopsis, respectively. Two patients had missing data for stereopsis.
A successful outcome was found in 81% (34/42) of patients at 2y and 71% (30/42) at the final visit. At 2y of follow-up, no patients had a poor outcome. Preoperative characteristics of patients in each outcome group at 2y are shown in Table 1. Of the 8 patients who had an acceptable outcome at 2y, 2 patients had increased exotropic deviation. Of these 2 patients, 1 had exotropia of 25 PD at 4y of follow-up and the other patient had exotropia of 22 PD at 9y of follow-up, and were classified into the poor outcome group at the final visit.
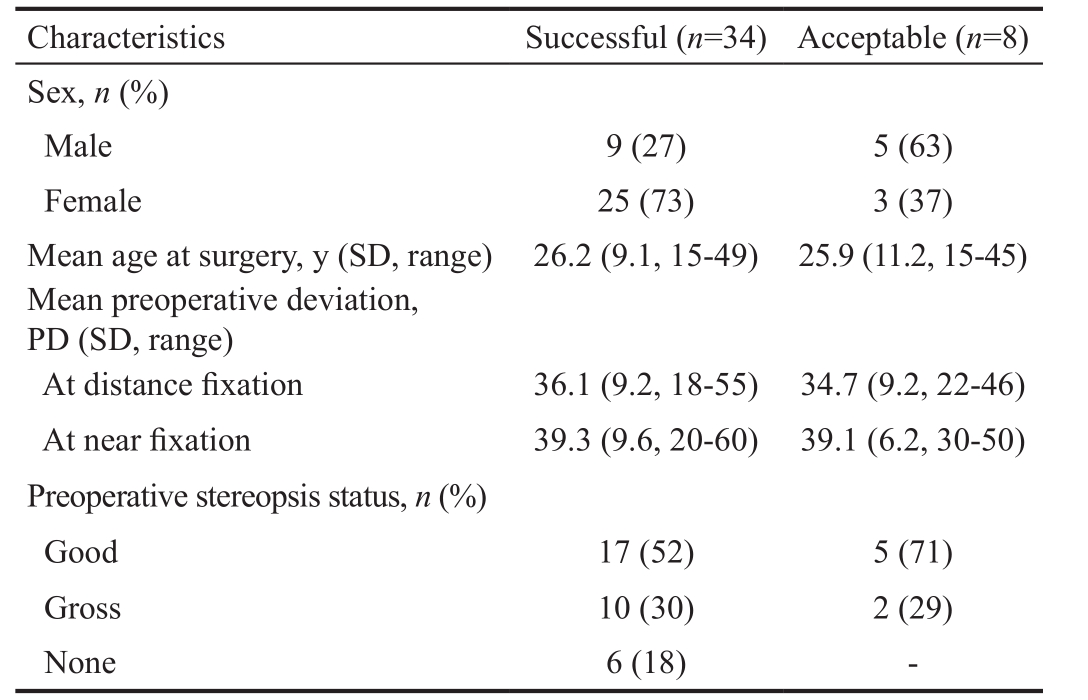
Table 2 Univariate and multivariate analysis of factors associated with a successful outcome at 2y
PD: Prism diopters; OR: Odds ratio; CI: Confidence interval.
For initial postoperative alignment, 12, 16, and 14 patients had large overcorrection, minimal overcorrection, and undercorrection,respectively. The mean deviation was esodeviation 10.4 PD(SD, 1.3; range, 9-14 PD), esodeviation 3.1 PD (SD, 3.3;range, 0-8 PD), and exodeviation 4.1 PD (SD, 2.3; range, 2-10 PD),respectively.
For factors associated with a successful outcome, univariate and multivariate analysis showed that initial postoperative minimal overcorrection (orthotropia to esodeviation 8 PD) was the only significant factor associated with a successful outcome at 2y (Table 2) and at the final visit.
The chance of a successful outcome was 2.2-fold higher in patients with initial minimal overcorrection (RR=2.2, 95%CI,1.18-4.06) and 2.1-fold higher in patients with initial large overcorrection (RR=2.14, 95%CI, 0.14-4.09) compared with those with initial undercorrection.
Kaplan-Meier Survival analysis showed that a successful outcome decreased with time (Figure 1). Among the groups, the probability of success was higher in the initial overcorrection group and lower in the initial undercorrection group (Figure 2). At the end of the observational period,less than half of the patients were in the non-success group.Therefore, we were unable to determine the median survival time.
Most patients showed exotropic drift at the subsequent followup visit, especially in the first month after surgery (Figure 3).The mean exotropic drift was 4.7 PD within the first month(SD, 4.6; range, esotropic drift 2 PD to exotropic drift 18 PD).The overall 2-year exotropic drift was 9.3 PD (SD, 5.2; range,0-21 PD).
For postoperative sensory status, 5 patients in the successful outcome group and 2 patients in the acceptable outcome group had improved sensory status. None of the patients had decreased sensory status after surgery.
Our study represents the largest series of adult patients (≥15 years old) who underwent unilateral recession and resection surgery for correction of exotropia. The minimal followup time was 2y. After surgery, 80.9% and 71.4% of patients had a successful outcome at 2y and at the final follow-up,respectively.
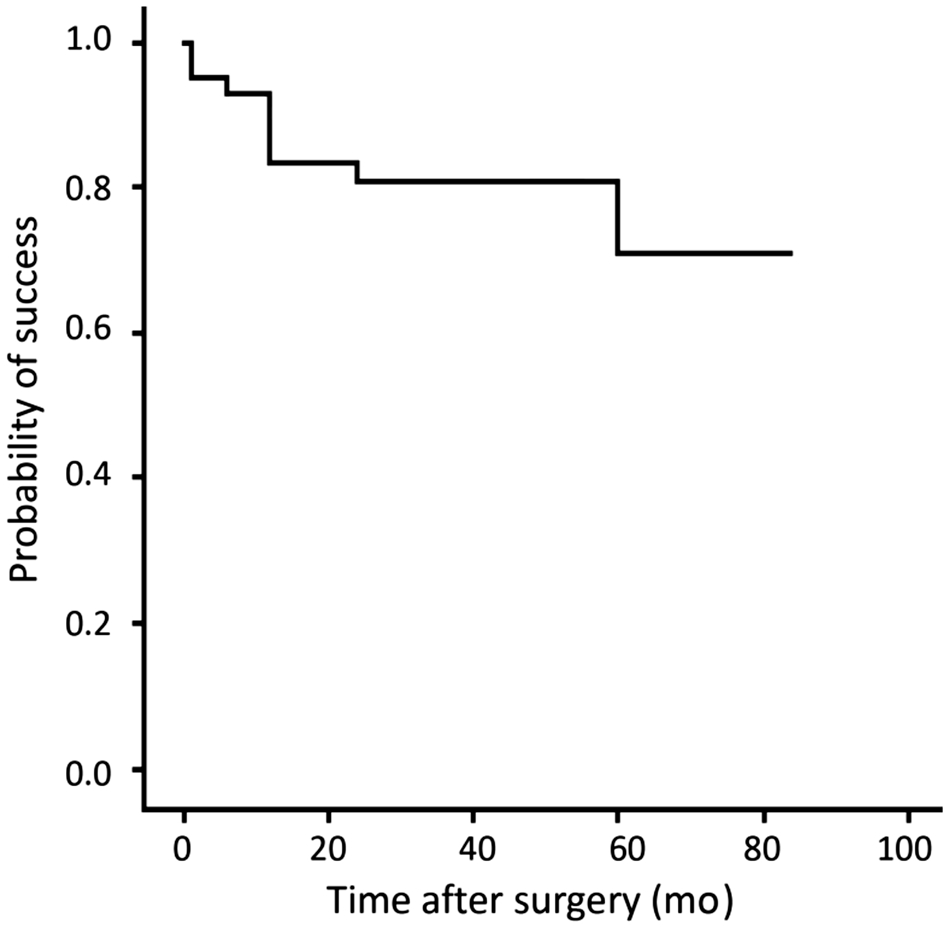
Figure 1 Survival curves with time after surgery.

Figure 2 Survival curves for each initial postoperative group with time after surgery.
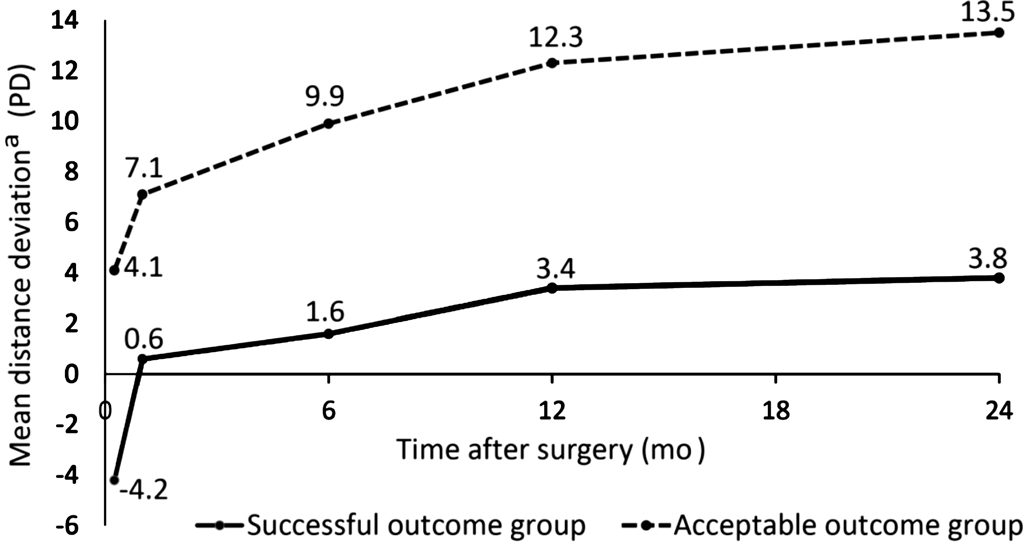
Figure 3 Exotropic drift in each outcome group within the first 2y after surgerya+: Exodeviation, −: Esodeviation.
Many studies have investigated factors that might related to successful outcome after exotropic surgery. In our study,we assessed initial postoperative factors at 1wk because, at this time, patients are more comfortable and cooperative.Therefore, measurements should be more accurate. We found that the chance of successful outcome was high in both initial minimal overcorrection group (orthotropia to esodeviation 8 PD) and initial overcorrection group (esodeviation ˃8 PD).However, univariate and multivariate analysis showed that initial minimal overcorrection was the only factor associated with a successful outcome at 2y and the final visit.
Several previous studies also found this relationship, but there was no consensus on the appropriate amount of initial deviation[14-20]. Scott et al[15]suggested esodeviation of 4-14 PD, Oh and Hwang[17]suggested esodeviation ˃10 PD, Raab and Parks[18]suggested esodeviation of 10-20 PD, Lee et al[19]suggested esodeviation of 1-10 PD and Jung et al[20]suggested esodeviation ˂10 PD. In our study, we found that initial postoperative deviation between orthotropia and esodeviation of 8 PD at 1wk postoperatively achieved the highest chance of successful outcome. However, other studies found no significant relationship between initial postoperative deviation and a successful outcome[13,22-24].
Additionally, some previous studies found that age at surgery,preoperative deviation and myopic refractive error were associated with a successful outcome[1,4,25-27]. In our study,neither of these factors had a good correlation with outcome.The difference in results between studies might be due to a difference in choice of surgery, assessment time postoperatively, definition for a successful outcome, and the follow-up period.
For survival analysis, Oh and Hwang[17]also studied the recurrent time after surgery. They found that the median recurrent time was 48.3mo. In our study, although we combined acceptable and poor outcomes together as a nonsuccess group owing to the small number of patients, we still could not determine the median survival time because less than half of the patients were in the non-success group.
This study found that exotropic drift was greatest within the first month after surgery. Park and Kim[28]and Choi et al[29]also reported that the amount of exotropic drift was the greatest during the first month after surgery, with a mean drift of 8.2 PD[28]. A new 7-year-follow-up study also found that more than 50% of exotropic drift was observed within the first year after surgery and there was no significant change after 18mo in patients who underwent unilateral recession and resection surgery[30].
Limitations of the study are as follows. First, this was a retroprospective study. Therefore, we had missing data.Second, although an attempt was made to contact all patients who met the criteria, only 42 out of 72 patients were included.Third, our study mainly emphasized on motor outcome. We did not combine motor and sensory evaluation for a successful outcome. A prospective study that assesses both outcomes may yield different results.
In conclusion, unilateral recession and resection surgery in adult patients with exotropia has a satisfactory outcome. For a successful outcome, initial overcorrection is recommended because of the tendency of exotropic drift, which occurs postoperatively.
Foundation:Supported by the Ratchadapiseksompoch Fund(No.RA57/046).
Conflicts of Interest: Kanjanawasee P, None; Praneeprachachon P, None; Pukrushpan P, None.
REFERENCES
1 Chia A, Roy L, Seenyen L. Comitant horizontal strabismus: an Asian perspective. Br J Ophthalmol 2007;91(10):1337-1340.
2 Matsuo T, Matsuo C. The prevalence of strabismus and amblyopia in Japanese elementary school children. Ophthalmic Epidemiol 2005;12(1):31-36.
3 Yu CB, Fan DS, Wong VW, Wong CY, Lam DS. Changing patterns of strabismus: a decade of experience in Hong Kong. Br J Ophthalmol 2002;86(8):854-856.
4 Saleem QA, Cheema AM, Tahir MA, Dahri AR, Sabir TM, Niazi JH.Outcome of unilateral lateral rectus recession and medial rectus resection in primary exotropia. BMC Res Notes 2013;6:257.
5 Burian HM, Spivey BE. The surgical management of exodeviations.Trans Am Ophthalmol Soc 1964;62:276-306.
6 Wang L, Wu Q, Kong X, Li Z. Comparison of bilateral lateral rectus recession and unilateral recession resection for basic type intermittent exotropia in children. Br J Ophthalmol 2013;97(7):870-873.
7 Kushner BJ. Selective surgery for intermittent exotropia based on distance/near differences. Arch Ophthalmol 1998;116(3):324-328.
8 Chia A, Seenyen L, Long QB. Surgical experiences with two-muscle surgery for the treatment of intermittent exotropia. J AAPOS 2006;10(3):206-211.
9 Jeoung JW, Lee MJ, Hwang JM. Bilateral lateral rectus recession versus unilateral recess-resect procedure for exotropia with a dominant eye. Am J Ophthalmol 2006;141(4):683-688.
10 Kim H, Yang HK, Hwang JM. Comparison of long-term surgical outcomes between unilateral recession and unilateral recession-resection in small-angle exotropia. Am J Ophthalmol 2016;166:141-148.
11 Kimura Y, Kimura T. Comparative study of plication-recession versus resection-recession in unilateral surgery for intermittent exotropia. Jpn J Ophthalmol 2017;61(3):286-291.
12 Cho YA, Kim SH. Postoperative minimal overcorrection in the surgical management of intermittent exotropia. Br J Ophthalmol 2013;97(7):866-869.
13 Choi J, Kim SJ, Yu YS. Initial postoperative deviation as a predictor of long-term outcome after surgery for intermittent exotropia. J AAPOS 2011;15(3):224-229.
14 Clarke WN, Noel LP. Surgical results in intermittent exotropia. Can J Ophthalmol 1981;16(2):66-69.
15 Scott WE, Keech R, Mash AJ. The postoperative results and stability of exodeviations. Arch Ophthalmol 1981;99(10):1814-1818.
16 Beneish R, Flanders M. The role of stereopsis and early postoperative alignment in long-term surgical results of intermittent exotropia. Can J Ophthalmol 1994;29(3):119-124.
17 Oh JY, Hwang JM. Survival analysis of 365 patients with exotropia after surgery. Eye (Lond) 2006;20(11):1268-1272.
18 Raab EL, Parks MM. Recession of the lateral recti. Early and late postoperative alignments. Arch Ophthalmol 1969;82(2):203-208.
19 Lee S, Lee YC. Relationship between motor alignment at postoperative day 1 and at year 1 after symmetric and asymmetric surgery in intermittent exotropia. Jpn J Ophthalmol 2001;45(2):167-171.
20 Jung EH, Kim SJ, Yu YS. Factors associated with surgical success in adult patients with exotropia. J AAPOS 2016;20(6):511-514.
21 Chalifoux E, Alkharashi M, Superstein R, Louis M, Blais C, Sabzevari S, Flanders M. Adjustable surgical treatment of adult exotropia:postoperative target angles and surgical success. Can J Ophthalmol 2016;51(4):254-257.
22 Ruttum MS. Initial versus subsequent postoperative motor alignment in intermittent exotropia. J AAPOS 1997;1(2):88-91.
23 Leow PL, Ko ST, Wu PK, Chan CW. Exotropic drift and ocular alignment after surgical correction for intermittent exotropia. J Pediatr Ophthalmol Strabismus 2010;47(1):12-16.
24 Pineles SL, Deitz LW, Velez FG. Postoperative outcomes of patients initially overcorrected for intermittent exotropia. J AAPOS 2011;15(6):527-531.
25 Gezer A, Sezen F, Nasri N, Gözüm N. Factors influencing the outcome of strabismus surgery in patients with exotropia. J AAPOS 2004;8(1):56-60.
26 Zou D, Casafina C, Whiteman A, Jain S. Predictors of surgical success in patients with intermittent exotropia. J AAPOS 2017;21(1):15-18.
27 Kim WJ, Kim MM. Variability of preoperative measurements in intermittent exotropia and its effect on surgical outcome. J AAPOS 2017;21(3):210-214.
28 Park KH, Kim SY. Clinical characteristics of patients that experience different rates of exodrift after strabismus surgery for intermittent exotropia and the effect of the rate of exodrift on final ocular alignment. J AAPOS 2013;17(1):54-58.
29 Choi MY, Hyung SM, Hwang JM. Unilateral recession-resection in children with exotropia of the convergence insufficiency type. Eye (Lond)2007;21(3):344-347.
30 Park H, Kim WJ, Kim MM. The stabilization of postoperative exo-drift in intermittent exotropia after surgical treatment. Korean J Ophthalmol 2016;30(1):60-65.
Correspondenceto:Parnchat Pukrushpan. Pediatric Ophthalmology and Strabismus Division, Department of Ophthalmology, Faculty of Medicine, Chulalongkorn University, Bangkok 10330, Thailand. parnchat@gmail.com
Received:2017-08-21 Accepted: 2018-01-03
Abstract● AlM: To evaluate the relationship between early postoperative deviation and long-term outcome after unilateral recession and resection surgery for adult exotropia, and to evaluate exotropic shift after surgery.● METHODS: This was a retroprospective study involving adult patients with exotropia who underwent unilateral recession and resection surgery and were followed up for at least 2y. The results were evaluated at 2y and the final visit. Factors influencing a successful outcome were analyzed. Early postoperative deviation at 1wk was used to evaluate relationship with long-term outcome. The longterm outcome was classified into 3 groups: successful,acceptable, and poor. Successful outcome was defined as a distance deviation between esodeviation 8 prism diopters (PD) and exodeviation 10 PD.● RESULTS: Forty-two patients were enrolled. The mean age at surgery was 26y (range, 15-49y). The median follow-up period was 30mo (range, 24-108mo). Successful outcome was found in 81% of patients at 2y and in 71%at the final visit. Overcorrection at 1wk postoperatively was associated with a successful outcome at 2y. lnitial postoperative alignment between orthotropia and esodeviation of 8 PD had the highest chance of a successful outcome (RR=2.2). The mean postoperative exotropic drift was 4.7 PD at the first month and 9.3 PD at 2y.● CONCLUSlON: lnitial postoperative deviation can predict long-term outcome after unilateral recession and resection surgery for adult exotropia. The most desirable outcome at 1wk post-operatively was orthotropia to small esodeviation. Most patients have exotropic drift at a subsequent follow-up, especially in the first month after surgery.
● KEYWORDS:exotropia; unilateral surgery; recession and resection; strabismus
DOl:10.18240/ijo.2018.08.17
Citation:Kanjanawasee P, Praneeprachachon P, Pukrushpan P.Relation between early postoperative deviation and long-term outcome after unilateral lateral rectus recession and medial rectus resection for adult exotropia. Int J Ophthalmol 2018;11(8):1358-1362