Evaluation of traumatic retinopathy with ultra-wide field imaging under corneal scar or fixed small pupil
Min Tang1, Yan-Nian Hui2, You-Yi Li1, Yue He1, Yang Cao1, Xiao-Hong Xiang1, Hong-Bin Lyu1
1Department of Ophthalmology, Affiliated Hospital of Southwest Medical University, Luzhou 646000, Sichuan Province, China
2Department of Ophthalmology, Xijing Hospital of the Fourth Military Medical University, Xi’an 710023, Shaanxi Province,China
INTRODUCTION
Complicated ocular trauma often compromises the anterior segment involving the cornea and the iris. After primary wound repair of the cornea and secondary vitreous surgery, serious complications such as corneal scar formation,iris defect and adhesions, and pupil displacement remained,which may shadow the optic axis and make the evaluation for the traumatic retinopathy more difficulty. Various traumatic retinopathies are the main reasons for poor visual outcomes in patients with complicated ocular injury, and poor evaluation of the retinal status will seriously interfere to the decisionmaking for management in such conditions. Ultra-wide field(UWF) imaging technology uses red (633 nm) and green(532 nm) lasers reflected off a large concave elliptical mirror,enabling large scan angles of up to the ora serrata under a small pupil, which provides a new method for solving this problem. Therefore, we used this technique to observe a series of patients with complicated ocular trauma, and compared with the conventional 45-degree fundus photography and direct ophthalmoscopy. Up to now we did not find similar study reported in the literature.
SUBJECTS AND METHODS
PatientsTwenty-eight patients with complicated ocular injury who were treated in our hospital from June 2016 to May 2017 enrolled in the retrospective analyses. The study was carried out with the approval of the Ethics Committee of Southwest Medical University. Due to the study’s nature of fundus examination, the requirement of informed consent was waived.All patients underwent secondary vitrectomy after emergencyoperation for corneal or sclera laceration repair, and had regularly follow up afterwards.
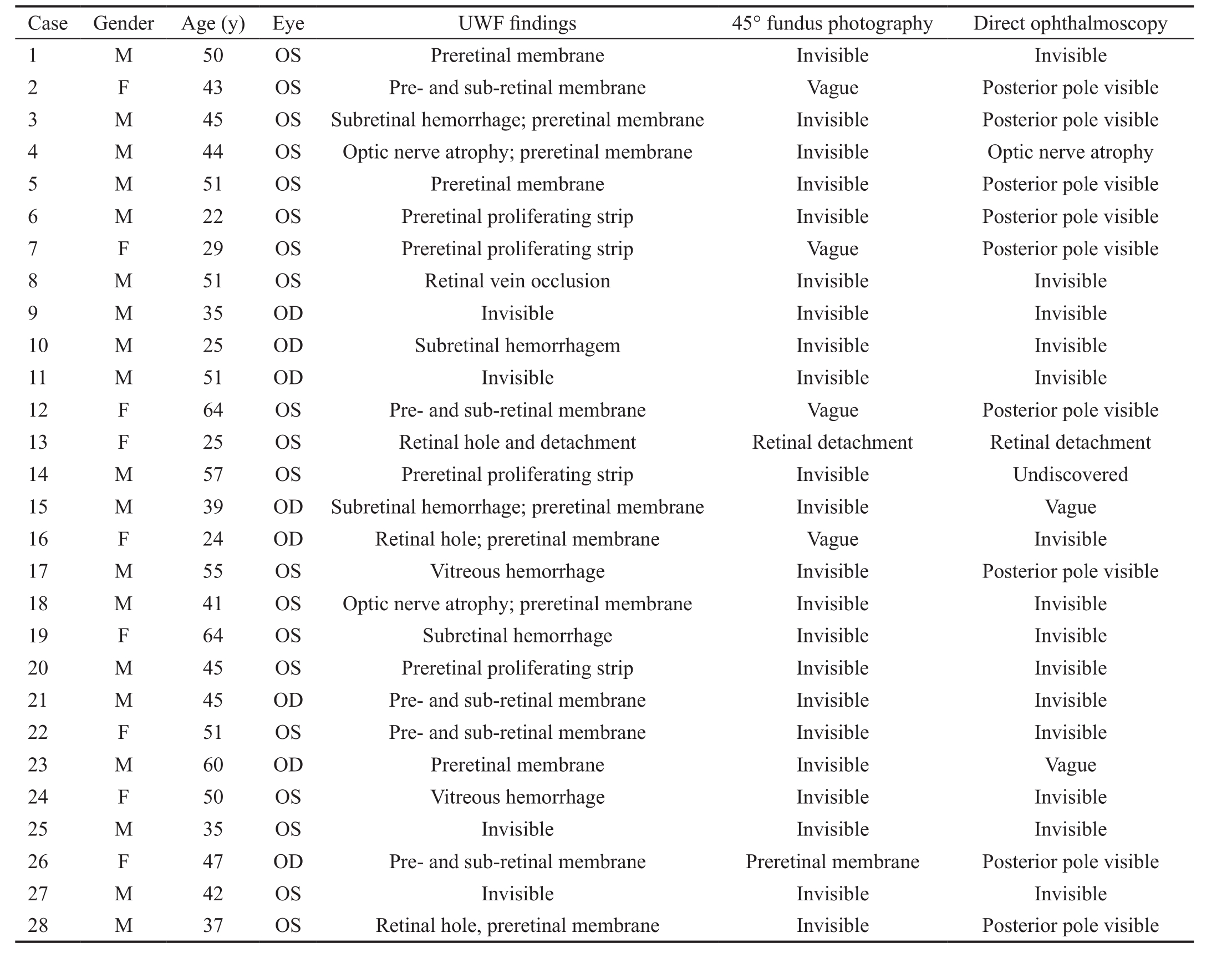
Table 1 In 28 eyes, 5 cases had simple pupil changes, and 23 cases had corneal scar or fixed small pupil simultaneously
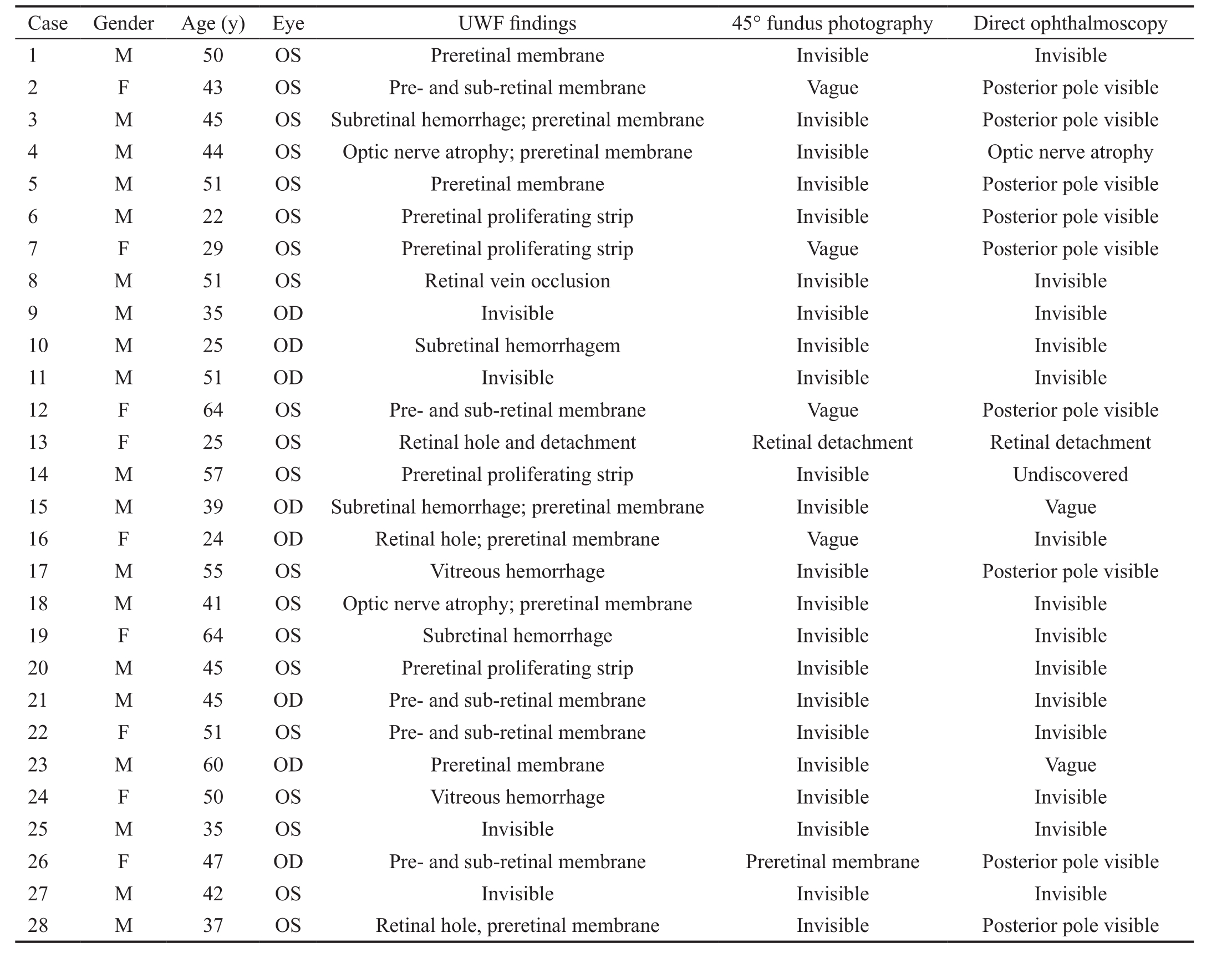
Case Gender Age (y) Eye UWF findings 45° fundus photography Direct ophthalmoscopy 1 M 50 OS Preretinal membrane Invisible Invisible 2 F 43 OS Pre- and sub-retinal membrane Vague Posterior pole visible 3 M 45 OS Subretinal hemorrhage; preretinal membrane Invisible Posterior pole visible 4 M 44 OS Optic nerve atrophy; preretinal membrane Invisible Optic nerve atrophy 5 M 51 OS Preretinal membrane Invisible Posterior pole visible 6 M 22 OS Preretinal proliferating strip Invisible Posterior pole visible 7 F 29 OS Preretinal proliferating strip Vague Posterior pole visible 8 M 51 OS Retinal vein occlusion Invisible Invisible 9 M 35 OD Invisible Invisible Invisible 10 M 25 OD Subretinal hemorrhagem Invisible Invisible 11 M 51 OD Invisible Invisible Invisible 12 F 64 OS Pre- and sub-retinal membrane Vague Posterior pole visible 13 F 25 OS Retinal hole and detachment Retinal detachment Retinal detachment 14 M 57 OS Preretinal proliferating strip Invisible Undiscovered 15 M 39 OD Subretinal hemorrhage; preretinal membrane Invisible Vague 16 F 24 OD Retinal hole; preretinal membrane Vague Invisible 17 M 55 OS Vitreous hemorrhage Invisible Posterior pole visible 18 M 41 OS Optic nerve atrophy; preretinal membrane Invisible Invisible 19 F 64 OS Subretinal hemorrhage Invisible Invisible 20 M 45 OS Preretinal proliferating strip Invisible Invisible 21 M 45 OD Pre- and sub-retinal membrane Invisible Invisible 22 F 51 OS Pre- and sub-retinal membrane Invisible Invisible 23 M 60 OD Preretinal membrane Invisible Vague 24 F 50 OS Vitreous hemorrhage Invisible Invisible 25 M 35 OS Invisible Invisible Invisible 26 F 47 OD Pre- and sub-retinal membrane Preretinal membrane Posterior pole visible 27 M 42 OS Invisible Invisible Invisible 28 M 37 OS Retinal hole, preretinal membrane Invisible Posterior pole visible
All patients were followed up routinely for visual acuity,intraocular pressure and slit lamp examinations. For fundus examination and comparison of positive findings of traumatic retinopathies, three qualified doctors performed the exam with only one method each separately in a blind way. Doctor A performed direct ophthalmoscopy using a YZ6E direct ophthalmoscope (Suzhou, China). Doctor B did conventional 45-degree fundus photography with a KOWA fundus camera(KOWA, Japan), and Doctor C applied UWF imaging with an Optomap panoramic 200Tx laser scanning ophthalmoscope(Optos 200TX, Optos PLC, Dunfermline, Scotland, UK).If the corneal scar in the pupil area or pupil had a severe shift, the eye position was adjusted to change the location and angle of the laser into the eye. If necessary, eye position guidance was given so as to achieve fundus scanning. The three doctors did not know the patient’s condition and other test results. And finally, these examination results were confirmed by the chief doctor (Lyu HB) and analyzed.
Statistical AnalysisSPSS17.0 software was used to perform 2 tests, and Bonferroni correction method was used to compare the positive finding rate. Statistical significance was defined as P˂0.05.
RESULTS
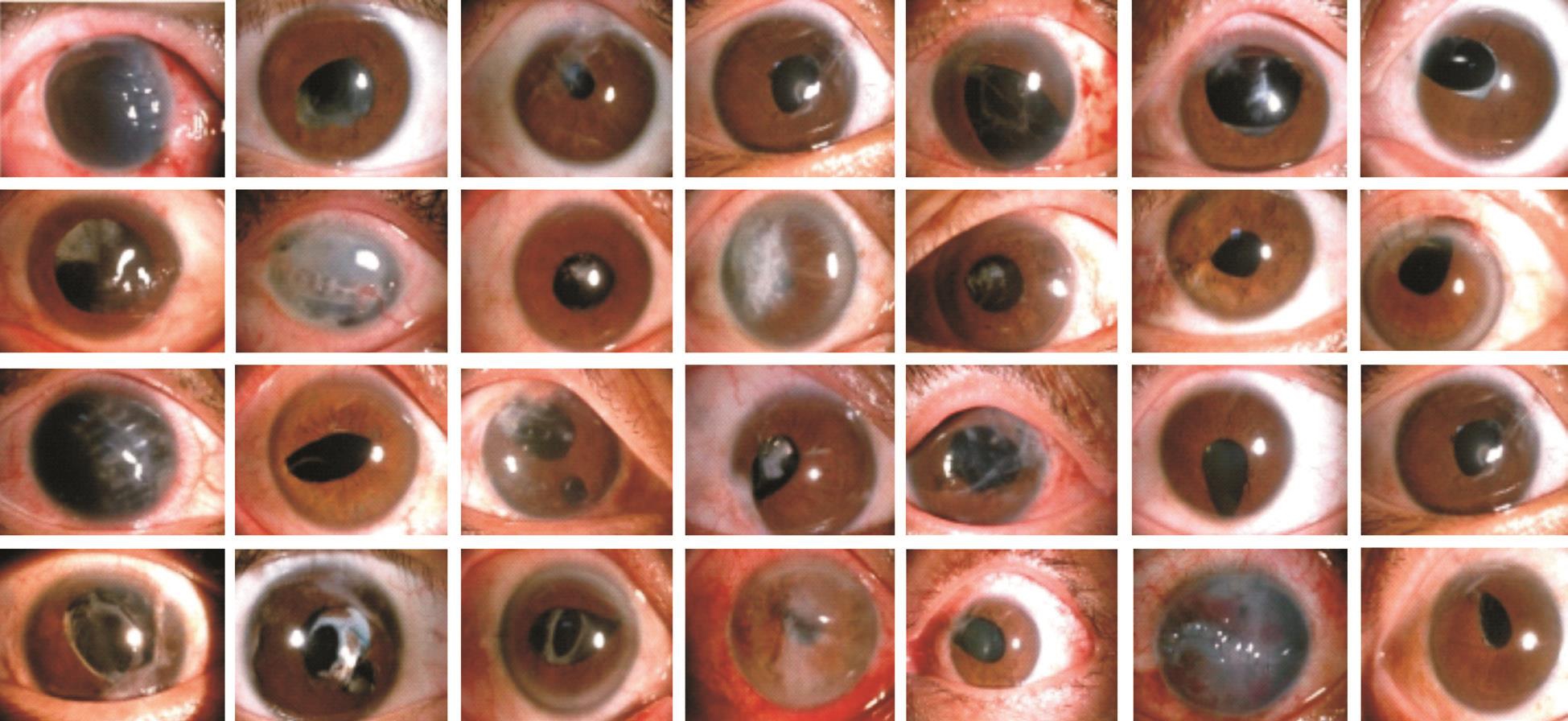
Patient CharacteristicsTwenty-eight patients with complicated ocular trauma were enrolled in this study, including 19 males and 9 females, with an average age of 43.42±12.62 (11 to 64)y.Causes of trauma included injury by nails, blades, emery wheels, stones, etc; while some other eyes mergered injury of physical damages such as car accident and high fall injury.Blast injury was also included. All of the 28 cases had eye penetrating injuries or globe rupture, and/or intraocular foreign bodies accompanied with corneal and scleral injury, varying degrees of iridodiastasis, lens dislocation, vitreous hemorrhage,retinal detachment and other serious injuries. The time interval between emergency operation for wound closure and elective vitrectomy was about 1-8wk, while the follow up time points was about 1 to 3mo after secondary vitrectomy. The patient characteristics are summarized in Table 1. The anterior segment photographs of 28 cases are shown in Figure 1. Representative cases are shown in Figures 2-5.
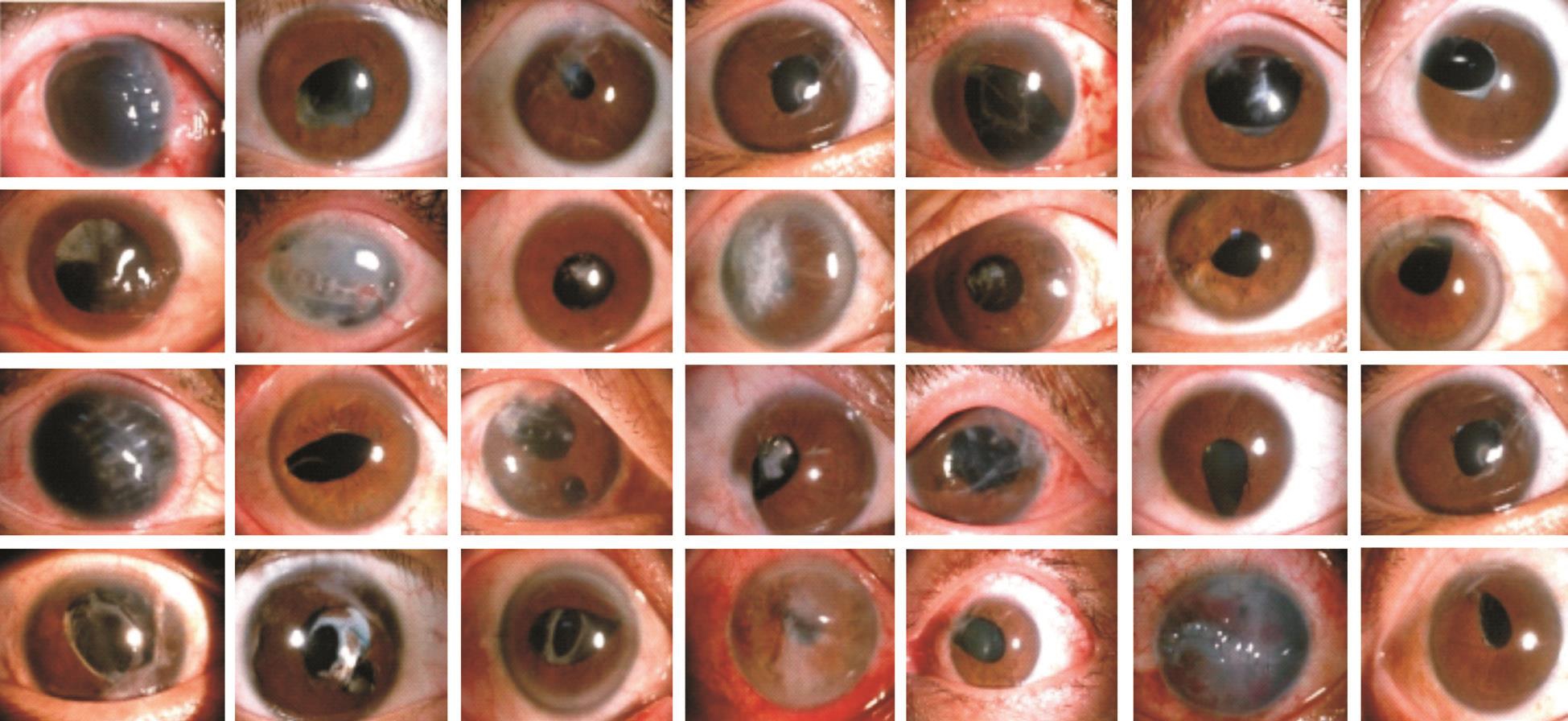
Figure 1 Anterior segment photographs of 28 traumatized eyes with corneal scar and/or fixed small pupil Each photo is corresponding to the case number in Table 1 from left to right and then up to down.

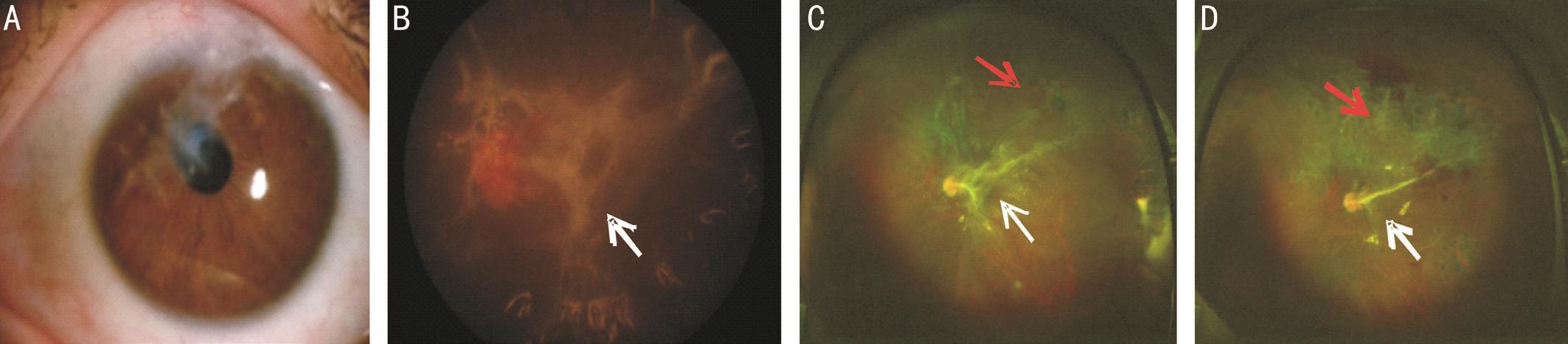
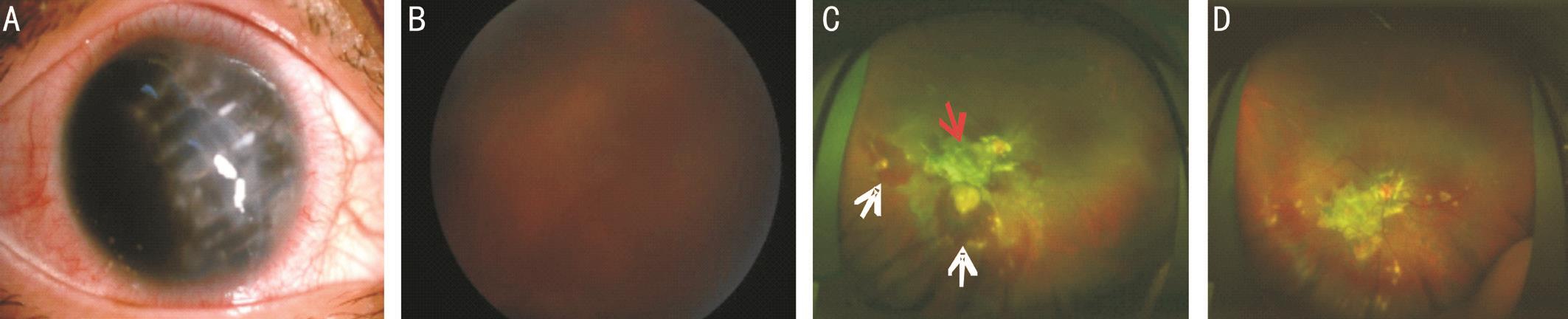
Figure 2 The left injured eye of Case 7 with pupil displacement The pupil superonasal shift after primary wound repair of left eye, and posterior synechia appears (A) and 45° fundus photograph shows the dis and a vague retinal vasculature (B). UWF image shows clear laser spots(white arrowheads) and retinal proliferating strips in the peripheral area (red arrows) (C).
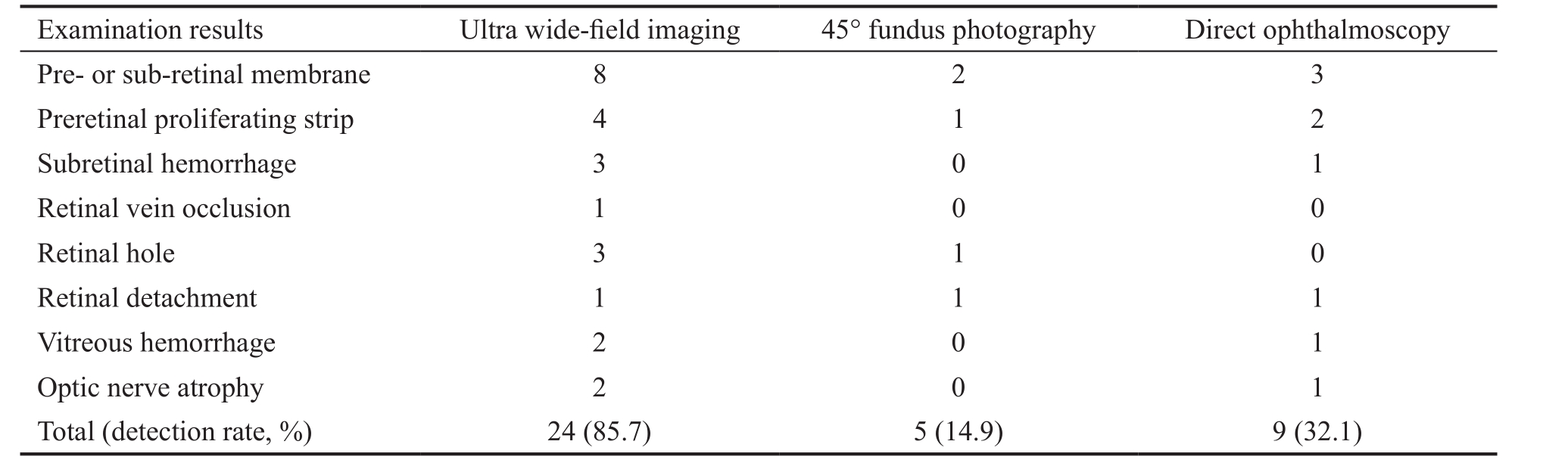
Table 2 Findings of 3 fundus examinations of 28 traumatized eyes with corneal scar or fixed small pupil
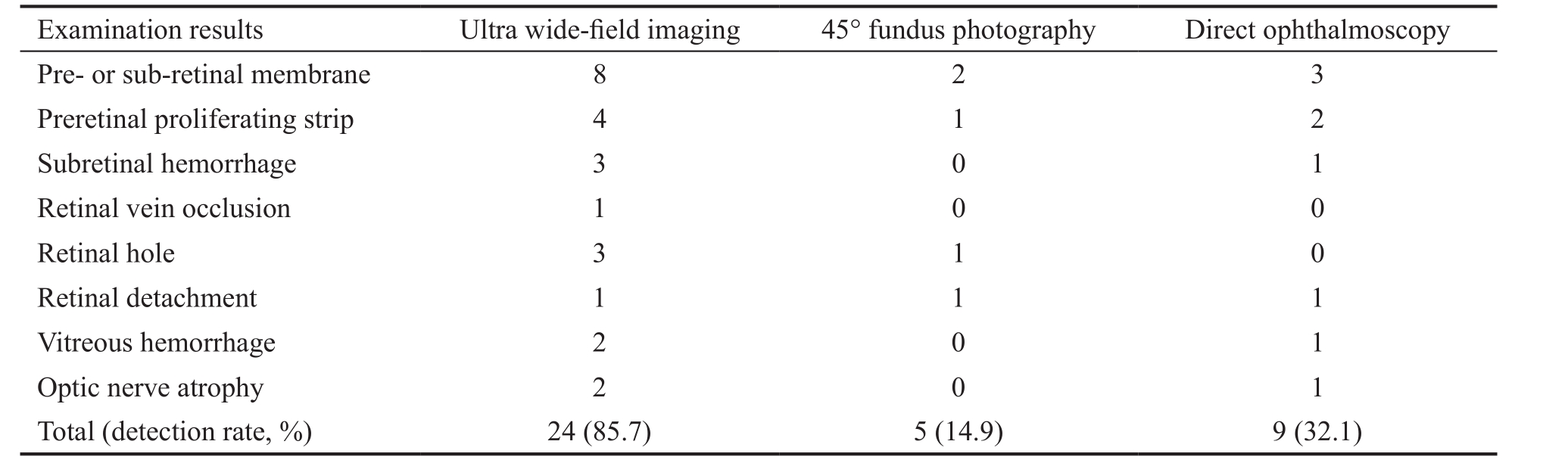
Examination results Ultra wide-field imaging 45° fundus photography Direct ophthalmoscopy Pre- or sub-retinal membrane 8 2 3 Preretinal proliferating strip 4 1 2 Subretinal hemorrhage 3 0 1 Retinal vein occlusion 1 0 0 Retinal hole 3 1 0 Retinal detachment 1 1 1 Vitreous hemorrhage 2 0 1 Optic nerve atrophy 2 0 1 Total (detection rate, %) 24 (85.7) 5 (14.9) 9 (32.1)
Three Fundus ExaminationsThe results of direct ophthalmoscopy, traditional 45-degree fundus examination and UWF imaging showed positive traumatic fundus changes in 9 cases (32.1%), 5 cases (14.9 %), and 24 cases (85.7%),respectively (Table 2).
The difference was statistically significant (Bonferroni correction, P˂0.001) while there was no statistical difference between the conventional 45-degree fundus photography and direct ophthalmoscopy (Bonferroni correction, P˃0.017).Among the 28 patients, 24 injured eyes were detected fundus lesions by UWF imaging. Among them, 8 eyes (28.6%, Cases 1, 2, 5, 12, 21, 22, 23 and 26) had periretinal membranes,which received no special treatment and/or were treated when silicone oil was removed. Four eyes (14.3%, Cases 6, 7, 14 and 20) appeared proliferating band before optic disk, of whom 2 eyes had no light perception; subretinal hemorrhage occurred in 3 eyes and spontaneously absorbed in 2 eyes (Figure 5).One eye (3.6%, Case 8) had retinal vein occlusion, diagnosed as ischemic type by fluorescence fundus angiography, and was given retinal laser photocoagulation. Three eyes (10.7%,Cases 13, 16 and 28) were complicated with retinal breaks,of which one eye received laser photocoagulation while one eye had retinal detachment and was treated with an additional vitrectomy. Two eyes (7.1%, Cases 17 and 24) were complicated with vitreous hemorrhage, of which one case had a second vitrectomy and the other received conservative treatment. Two eyes (7.1%, Cases 4 and 18) appeared optic nerve atrophy without special treatment.

Figure 3 The left penetrating injured eye of Case 1 with corneoscleral laceration A: Linear corneal scar from 1 to 4:30 o’clock,accompanying corneal opacities; B: The fundus is invisible through the 45° fundus photography; C: UWF image shows silicone oil filling in vitreous cavity, laser spots and pre-retinal membranes.
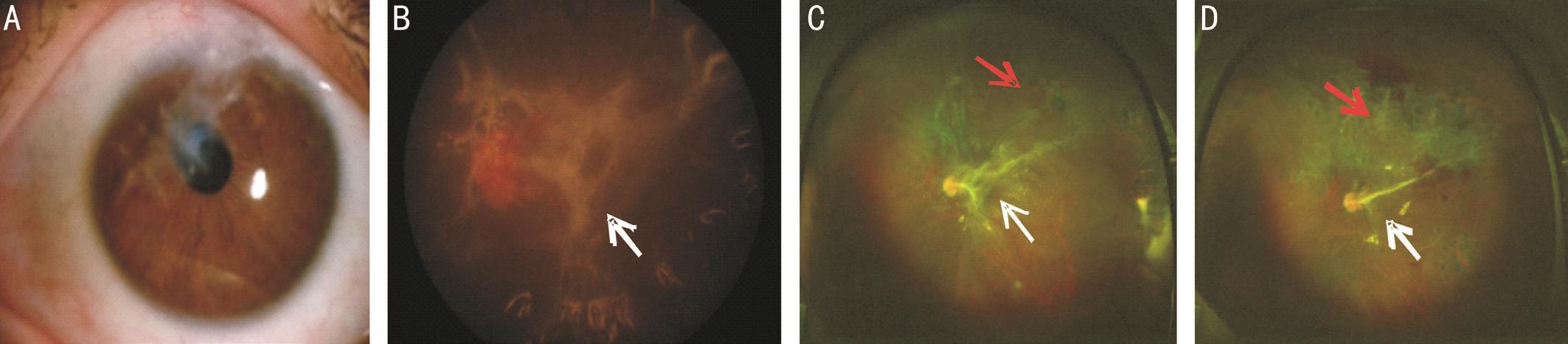
Figure 4 The left penetrating injured eye of of Case 4 with limbus laceration A: Linear corneal scar from 1 to 9 o’clock, beyond the edge of pupil; B: The 45° fundus photograph shows the disc and pre-retinal membrane; C: UWF image shows silicone oil filling in vitreous cavity, laser spot, retinal proliferating strips (white arrow) and retinal hole (red arrow); D: One week after the removal of silicone oil, retinal hole has been closed, with laser spots surrounding (red arrow). A small number of retinal proliferative membranes are still visible (white arrow).
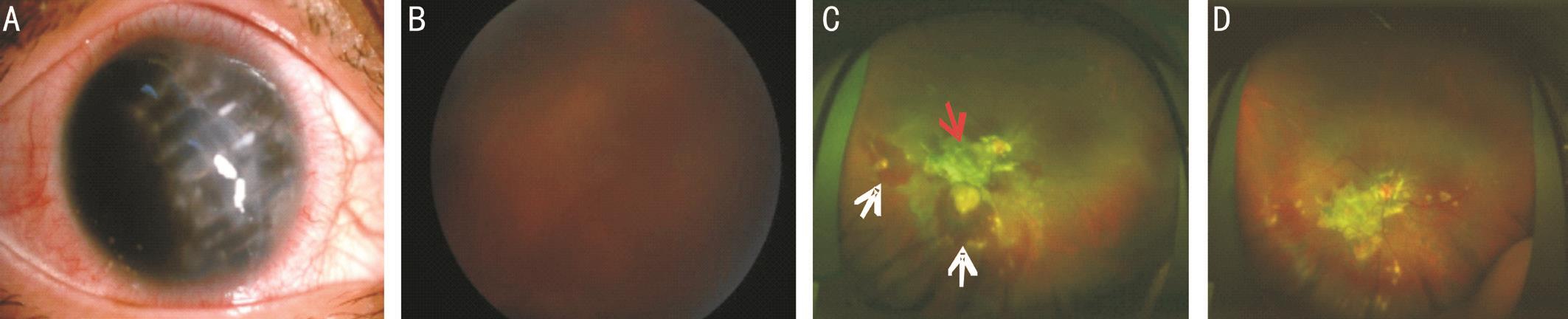
Figure 5 The right penetrating injured eye of of Case 15 with limbus laceration A: Linear corneal scar from 11 to 5 o’clock, accompanying corneal opacities; B: Fundus is invisible through the 45° fundus photography; C: UWF image shows pre-retinal membrane (red arrow) near the optic disc, and mass subretinal hemorrhage (white arrows); D: A large proliferated membrane is observed at the temporal side of optic disc, and subretinal hemorrhage has been absorbed 3mo after surgery.
DISCUSSION
We believe our study compares favorably with other contemporary studies in terms of its meaningful results. It is generally known that ocular trauma is a major visionthreatening disease and responsible for monocular blindness and low vision worldwide, according to the report that about 1.6 million of the world’s monocular blindness is caused by trauma[1]. In China, ocular trauma is the primary cause of monocular blindness, and mechanical ocular trauma,especially open ocular trauma accounts for the majority[2].Traumatic retinopathy is the main cause of eye injury-induced irreversible damage. In recent years, introduction of the advanced ophthalmic examination equipment, such as optical coherence tomography (OCT)[3], adaptive optics scanning ophthalmoscope (AOSO)[4]and fundus autofluorescence(FAF)[5]made the evaluation of traumatic retinopathy more effective. However, complicated ocular trauma often associated with the anterior segment involving the cornea and the iris.After primary wound repair of the cornea and secondary vitrectomy, serious complications such as corneal scar formation, iris defect and adhesions, and pupil displacement remained, which may shadow the optic axis and make the evaluation for the traumatic retinopathy more difficulty.
In our study, UWF imaging technology was used to observe a series of patients with complicated ocular trauma postoperatively. Surprisingly to us, the fundus photos could not be obtained using conventional photography but did well with UWF imaging. Among the 28 eyes, 24 ocular fundus images could be clearly shown, and those findings served as an indicator for further treatment, which is of great significance to guide the management of such complicated cases.
UWF Imaging Technology for Fundus Images Under the Fixed Small PupilIn the UWF imaging system, a concave dual-focus elliptical mirror device was used. The laser scanning head and the tested eye are placed on the two focal points of the elliptical mirror respectively, which can form a virtual scanning center behind the iris, just like the scanning device was placed in the eye, and rotated to complete the imaging of the retina at 200°[6]. UWF imaging system achieving 200°range of retina scan needs to ensure at least 140° range of incident light into the pupil according to its design principle.In the premise of accurate focus, the lowest imit of pupil diameter is 2 mm that allowed to ensure 140° range of incident light into it. As we know the normal pupils diameter range from 2.5 to 4.0 mm, therefore, the UWF imaging system can achieve 200° retinal imaging under the condition of nonmydriatic pupil[7]. The effective pupil diameter of patients with complicated ocular trauma that allow the laser to enter may be less than the normal due to factors such as pupil displacement,iris adhesion, pupil deformation, or occlusion of corneal scars,we can adjust the position of incident light to make the angle reach or be close to 140° before laser reaches real focus, and thus achieving ultra-wide field of the eye laser scanning. In our study, 8 patients would not be obtained the fundus imaging totally by conventional fundus examination due to pupil shift or iris adhesions, while they were detected by UWF imaging(Figures 2 and 4).
UWF Imaging Technology for Fundus Images Under Corneal ScarIn our study, all patients were associated with various extent and transparency of corneal scar. The relationship of corneal scar and UWF imaging can be summarized as follows: when the corneal scar is close to but not beyond the pupil edge (having 2-3 mm transparent area in the visual axis), a clear fundus imaging with about 200°range can be achieved; when the scar is beyond the edge of the pupil, a clear fundus imaging with a certain range can also be achieved by adjusting the location and angle of laser scanning, no matter whether it is accompanied with changes in pupil morphology (Figure 4). When the corneal scar covers the pupil area, a certain range of clear fundus imaging can also be achieved, as the UWF imaging system has a strong penetration because a red and green laser for scanning are simultaneously applied (Figures 3 and 5). In this study, 3 patients (Cases 9,11 and 27) with severe corneal leukoplakia did not obtain the fundus imaging.
Evaluating Traumatic Retinopathy For the Management of Complicated Ocular TraumaDue to the factors such as corneal scar and pupil deformation which block visual axis,the fundus could be difficult to be viewed after operations. The fundus lesions, such as proliferative periretinal membrane,subretinal hemorrhage (Figure 5), retinal vascular occlusion,and optic nerve atrophy could seriously affect prognosis.Traumatic proliferative vitreoretinopathy (tPVR) is observed in more than 70% of patients with open globe injuries involving the posterior segment, and usually progresses to traction retinal detachment[8]. tPVR and traction retinal detachment have been confirmed as major risk factors for poor anatomical and functional outcomes after injury[9-11]. In our study, we found that complicated injured eyes after vitrectomy was associated with obvious proliferation, characterized by membranes or strands, which caused by trauma-induced inflammatory response, retinal gliosis and fibrosis[12-13]. Studies have also shown that silicone oil is closely related to recurrent PVR[14-15]and timely detection of traumatic retinopathy may help to prevent further visual loss in silicone oil-filled eye.
Subretinal hemorrhage can result from trauma or vitreoretinal surgery and affect visual function due to separation of the neural retina and pigment epithelium, and photoreceptor cell death[16]. In this study, 3 cases of subretinal hemorrhage were found, and some of them was absorpted.
In our study, 12 patients (50%) had distinct extent of proliferative membranes on the macular area, optic disc and other structures, resulting in light perception vision. Other retinopathies found in our study, such as retinal breaks,retinal vein occlusion[17], if not timely found and interfered,may induce retinal detachment, vitreous hemorrhage and other serious complications, which need repeat treatment and operation.
The limitations of this study include insufficient sample due to the poor patient compliance. Secondly, the time of follow up was limited, so some long-term outcomes did not effectively present. We would include more cases and follow longer in future study.
Moreover, UWF imaging technology still has some limitations.Because of the “Greenland effect”, a spherical surface greater than a 180° was presented in the form of a plane, causing the deformation of the peripheral image. And the fundus pseudocolor images scanned by UWF imaging still has a certain degree of distortion[18]. Laser scanning with the present wave lengths can still not penetrate the full-thickness cornea scar to achieve fundus imaging. If corneal scar is too large and opaque, the pupil is seriously deformed, or the eye can’t move due to extraocular muscle injury, the imaging taken and adjustment of patient’s eye position would be very difficult and time-consuming. Mackenze et al[19]reported low diagnosis sensitivity before the equatorial lesions. However, even if the imaging range is less than 200° due to the above factors, or imaging quality is relatively low, it still holds a very significant advantage compared to traditional fundus examinations.
ACKNOWLEDGEMENTS
The authors thank the students for their participation.
Foundation:Supported by Sichuan Province Scientific Research Project of Institutions of Higher Education (No.2017-ZRQN-108).
Conflicts of Interest:Tang M, None; Hui YN, None; Li YY,None; He Y, None; Cao Y, None; Xiang XH, None; Lyu HB,None.
REFERENCES
1 Patel D. Eye injuries: improving our practice. Community Eye Health 2015;28(91):41-43.
2 Wagne PJ, Lan GK. Mechanical ocular trauma. Curr Opin Ophthalmol 1996;7(4):57-64.
3 Yu W, Zheng L, Zhang Z, Dai R, Dong F. Spectral-domain optical coherence tomography characteristics of macular contusion trauma.Ophthalmic Res 2012;47(4):220-224.
4 Stepien KE, Martinez WM, Dubis AM, Cooper RF, Dubra A, Carroll J.Subclinical photoreceptor disruption in response to severe head trauma.Arch Ophthalmol 2012;130(3):400-402.
5 Lavinsky D, Martins EN, Cardillo JA, Farah ME. Fundus autofluorescence in patients with blunt ocular trauma. Acta Ophthalmologica 2011;89(1):e89-e94.
6 Friberg TR, Pandya A, Eller AW. Non-mydriatic panoramic fundus imaging using a non-contact scanning laser-based system. Ophthalmic Surg Lasers Imaging 2003;34(6):488-497.
7 Kato Y, Oguchi M, Tamaoki A, Yoshida N, Kaga T, Ichikawa K.Performance of fundus photography using the ultra-widefield scanning laser ophthalmoscope Optos 200Tx™. Journal of Japanese Association of Certified Orthoptist 2012;41(0):207-212.
8 Winthrop SR, Cleary PE, Minckler DS, Ryan SJ. Penetrating eye injuries: a histopathological review. Br J Ophthalmol 1980;64(11):809-817.
9 Cardillo JA, Stout JT, LaBree L, Azen SP, Omphroy L, Cui JZ, Kimura H, Hinton DR, Ryan SJ. Post-traumatic proliferative vitreoretinopathy.The epidemiologic profile, onset, risk factors, and visual outcome.Ophthalmology 1997;104(7):1166-1173.
10 El-Asrar AM, Al-Amro SA, Khan NM, Kangave D. Visual outcome and prognostic factors after vitrectomy for posterior segment foreign bodies. Eur J Ophthalmol 2000;10(4):304-311.
11 Andreoli MT, Andreoli CM. Surgical rehabilitation of the open globe injury patient. Am J Ophthalmol 2012;153(5):856-860.
12 Jin Y, Chen H, Xu X, Hu Y, Wang C, Ma Z. Traumatic proliferative vitreoretinopathy: clinical and histopathological observations. Retina 2017;37(7):1236-1245.
13 Hui YN, Liang HC, Cai YS, Kirchhof B, Heimann K. Corticosteroids and daunomycin in the prevention of experimental proliferative vitreoretionopathy induced by macrophages. Graefes Arch Clin Exp Ophthalmol 1993;231(2):109-114.
14 Halberstadt M, Domig D, Kodjikian L, Koerner F, Garweg JG. PVR recurrence and the timing of silicon oil removal. Klin Monbl Augenheilkd 2006;223(5):361-366.
15 Berrod J P, Sellier A, Rozot P, Raspiller A. Treatment of vitreoretinal proliferation in rhegmatogenous detachment and silicone oil tamponade. J Fr Ophtalmol 1996;19(2):97-105.
16 Lee OT, Bhisitkul R, Dunaief J. Neuroprotection, the role of iron in photoreceptor toxicity induced by subretinal hemorrhage. Invest Ophthalmol Vis Sci 2007;48(13):3034-3034.
17 Tanaka M, Ninomiya H, Kobayashi Y, Qiu H. Studies on vitrectomy cases associated with complicated branch retinal vein occlusion. Nippon Ganka Gakkai Zasshi 2000;104(2):103-109.
18 Chou B. Limitations of the Panoramic 200 Optomap. Optom Vis Sci 2003;80(10):671-672.
19 Mackenzie PJ, Russell M, Ma PE, Isbister CM, Maberley DA.Sensitivity and specificity of the optos optomap for detecting peripheral retinal lesions. Retina 2007;27(8):1119-1124.
Correspondenceto:Hong-Bin Lyu. Department of Ophthalmology, Affiliated Hospital of Southwest Medical University, Luzhou 646000, Sichuan Province, China.oculistlvhongbin@163.com
Received:2018-03-05 Accepted: 2018-04-11
Abstract● AlM: To evaluate the value of ultra-wide field (UWF)imaging in the management of traumatic retinopathy under the condition of corneal scar or fixed small pupil after complicated ocular trauma.● METHODS: Twenty-eight patients (28 eyes) with complicated ocular trauma were enrolled in the study from June 2016 to May 2017, including 19 males and 9 females with age ranged from 11 to 64 (43.42±12.62)y. All patients were treated with secondary vitrectomy after emergency operation for wound repair of open ocular trauma. Direct ophthalmoscopy and 45-degree fundus photography were taken at each time point of follow up for comparison of findings with UWF images. Routine eye examination including visual acuity, intraocular pressure, slit lamp examination were performed and analyzed as well.● RESULTS: Among the 28 traumatized eyes, the positive rate for identification of traumatic retinopathed was 32.1%(9 cases), 14.9% (5 cases), and 85.7% (24 cases) with direct ophthalmoscopy, 45-degree fundus photography, and UWF imaging, respectively. The detective rate of UWF imaging under the condition of corneal scar or fixed small pupil was statistically greater than that of 45-degree fundus photography and direct ophthalmoscopy (Bonferroni correction, P<0.001). UWF image was obtained in 19 eyes with opaque corneal scar, otherwise their fundus could not be seen by conventional methods. The additional findings of traumatic retinopathies by UWF imaging included periretinal membranes or pre-retinal proliferating strip,retinal holes, hemorrhage in the vitreous or sub-retinal space.● CONCLUSlON: UWF imaging is superior to traditional fundus photography in the evaluation of traumatic retinopathies under the condition of corneal scar or fixed small pupil after complicated ocular trauma.
● KEYWORDS:ultra-wide field imaging; complicated ocular trauma; corneal scar; fixed small pupil; fundus photography;traumatic retinopathy
DOl:10.18240/ijo.2018.08.19
Citation:Tang M, Hui YN, Li YY, He Y, Cao Y, Xiang XH, Lyu HB. Evaluation of traumatic retinopathy with ultra-wide field imaging under corneal scar or fixed small pupil. Int J Ophthalmol 2018;11(8):1371-1376