lnfluence of severity and types of astigmatism on visual acuity in school-aged children in southern China
Li-Li Wang, Wei Wang, Xiao-Tong Han, Ming-Guang He
Zhongshan Ophthalmic Center, State Key Laboratory of Ophthalmology, Sun Yat-Sen University, Guangzhou 510060,Guangdong Province, China
INTRODUCTION
Astigmatism is one of the most common refractive errors. Severe astigmatism without effective correction leads to visual impairment, amblyopia, and myopia during emmetropization[1-3]. Visual impairment due to astigmatism may also cause insufficient educational performance and affect working potential[4-6]. The prevalence of astigmatism in Chinese children ranges from 2% to 42.7%[7-11]. Previous studies also have documented that children of Hispanic and African-American ethnicities had higher risk of astigmatism than non-Hispanic white children[12]. Asian ethnicity was also related with higher risk of astigmatism[13-14]. However, these findings are considerably different and not directly comparable due to the differences in disease definition.
Knowledge of the influence of severity and subtypes of astigmatism on visual performance is essential for a better understanding of the impact of astigmatism on visual function and probably amblyopia. It is well established that astigmatism lead to visual reduction for both distant and near distance.However, the cutoff of clinical significant astigmatism has not been established currently. For example, the definition of astigmatism varied across population-based studies.Hashemi et al[15]used the cylinder of 0.5 D as the cutoff in the population survey in Iran. The Sydney Myopia Study (SMS)and Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error Study (CLEERS) adopted a cylinder of 1.0 D as the cutoff for astigmatism definition[12,16-17]. The Baltimore Pediatric Eye Disease Study (BPEDS), Strabismus, Amblyopia and Refractive Error in Singaporean Children Study (STARS)and Multi-Ethnic Pediatric Eye Disease Study (MEPEDS)used a relatively high cutoff (cylinder ≥1.50 D) to examine the prevalence of astigmatism in preschool children[13,18-20].
The Refractive Error Study in Children (RESC) is a multicountry large-scale population-based, cross-sectional survey of refractive error and visual impairment in school-aged children, which has used standard methodology and common definition[7,21]. Using Guangzhou RESC data, we found that the overall prevalence of astigmatism (cylinder≥0.75 D) was 42.7% in Chinese children[7]. The objective of this study was to further explore the association of astigmatism with visual impairment and to identify the cutoff of astigmatism for functional visual impairment.
SUBJECTS AND METHODS
Study PopulationThe RESC surveys were conducted using a standardized protocol with randomized cluster sampling of the targeted study population, which was detailed in previous reports[7,21-22]. The RESC survey was reviewed and approved by human experimentation committees or Institutional Review Boards (IRB) of World Health Organization. Approval for the studies at specific sites was obtained from local health authorities. Written informed consent for each examined child was obtained from a parent or other responsible adult during the household enumeration. The research followed the tenets of the Declaration of Helsinki.
Ocular ExaminationsClinical examination of participants including external eye, anterior segment, media and fundus were performed by trained RESC optometrists or ophthalmologist using standardized protocols. Ocular alignment was assessed using the cover and uncover test at near (0.5 m) and distance (4 m). Hirschberg corneal light reflex was used to measure the degree of tropia.
Visual Acuity and Cycloplegic RefractionUncorrected monocular distance visual acuity was measured at 4 m with a retro-illuminated logMAR chart (Precision Vision, La Salle,IL, USA), in a monocular fashion with the right eye followed by the left eye, using five tumbling “E” optotypes on each line and recorded as the smallest line read with one or no errors. If uncorrected visual acuity (UCVA) in either eye was 20/40 (0.5)or worse, best-corrected visual acuity (BCVA) was measured after cycloplegic refraction.
Autorefraction was performed after cycloplegia. Cycloplegia was induced with two drops of 1% cyclopentolate administered to each eye 5min apart and a third drop administered if a pupillary light reflex was still present after 20min. Successful cycloplegia and pupil dilation were evaluated after an additional 15min and was defined as a pupil dilution of more than 6 mm and without light reflex. Refractive error was determined by cycloplegic streak retinoscopy followed by measurement with a handheld auto-refractor (Retinomax K-plus, Nikon, Tokyo, Japan) after visual acuity measurement.For the current paper, auto-refraction data with complete cycloplegia were used.
Definitions of Refractive Error and Visual ImpairmentMinimum meridian is the meridian with the smallest refractive error, the one closest to 0.0 D. Absolute minimum meridian is the absolute value of minimum meridian. Myopia was defined as a minimum meridian ≤-0.75 D. Hyperopia was defined as minimum meridian ≥1.00 D. Emmetropia was defined as a minimum meridian refraction from -0.5 D to +0.75 D.Spherical degree was defined as the angle of the minimum meridian power. Cylindrical refractive error was expressed in negative cylinder form. Types of astigmatism were defined based on the minus astigmatism axis of the right eye: with the rule (WTR; cylinder axis 0° to 30° or 150° to 180°),against the rule (ATR; cylinder axis 60° to 120°) and oblique(OBL; cylinder axis 31° to 59° or 121° to 149°). The visual impairment was defined based on UCVA and on BCVA. Three cut-offs were used for visual impairment: UCVA≤20/40 (0.5)or UCVA≤20/32 (0.7) or BCVA≤20/32 (0.7).
Statistical AnalysisStatistical analysis was performed using Stata Version 11.0 (Stata Corporation, College Station, Texas,USA). The data on the right eyes was used for analysis. The prevalence of astigmatism was categorized into 10 subgroups based on cylinder severity: 0 D, 0.25 D, 0.50 D, 0.75 D, 1.00 D,1.25 D, 1.50 D, 1.75-2.00 D, 2.25-3.00 D and ˃3.00 D. Multivariate logistic regression analysis was used to explore the association of visual impairment and astigmatism severity after controlling for age, sex, and spherical error. Confidence intervals (CI) and P values (significant at the ˂0.05 level) for prevalence estimates and regression models were calculated with adjustment for cluster effects associated with the sampling design. Wald binomial confidence intervals for odds ratios(OR) were calculated. Multivariate linear regression analysis was performed to investigate the association of astigmatism and logMAR visual acuity. A P-value less than 0.05 was considered statistically significant.
RESULTS
Study PopulationA total of 5053 children age 5-15y were enumerated in Guangzhou, of whom 4364 (86.4%) children were examined. Among of them 4312 (85.3%) children received successful cycloplegic auto-refraction (1%cyclopentolate) and a reliable visual acuity measurement. After excluding 51 children with visual impairment due to nonrefractory causes (amblyopia, cataract, retinal disorder and other causes), 4261 children underwent further evaluation.Visual acuity testing is challenging in children age 5-6y because visual and cognitive function is still developing.After excluding 532 (12.49%) children age 5-6y, a total of 3729 children age 7-15y were included in the current analysis finally.
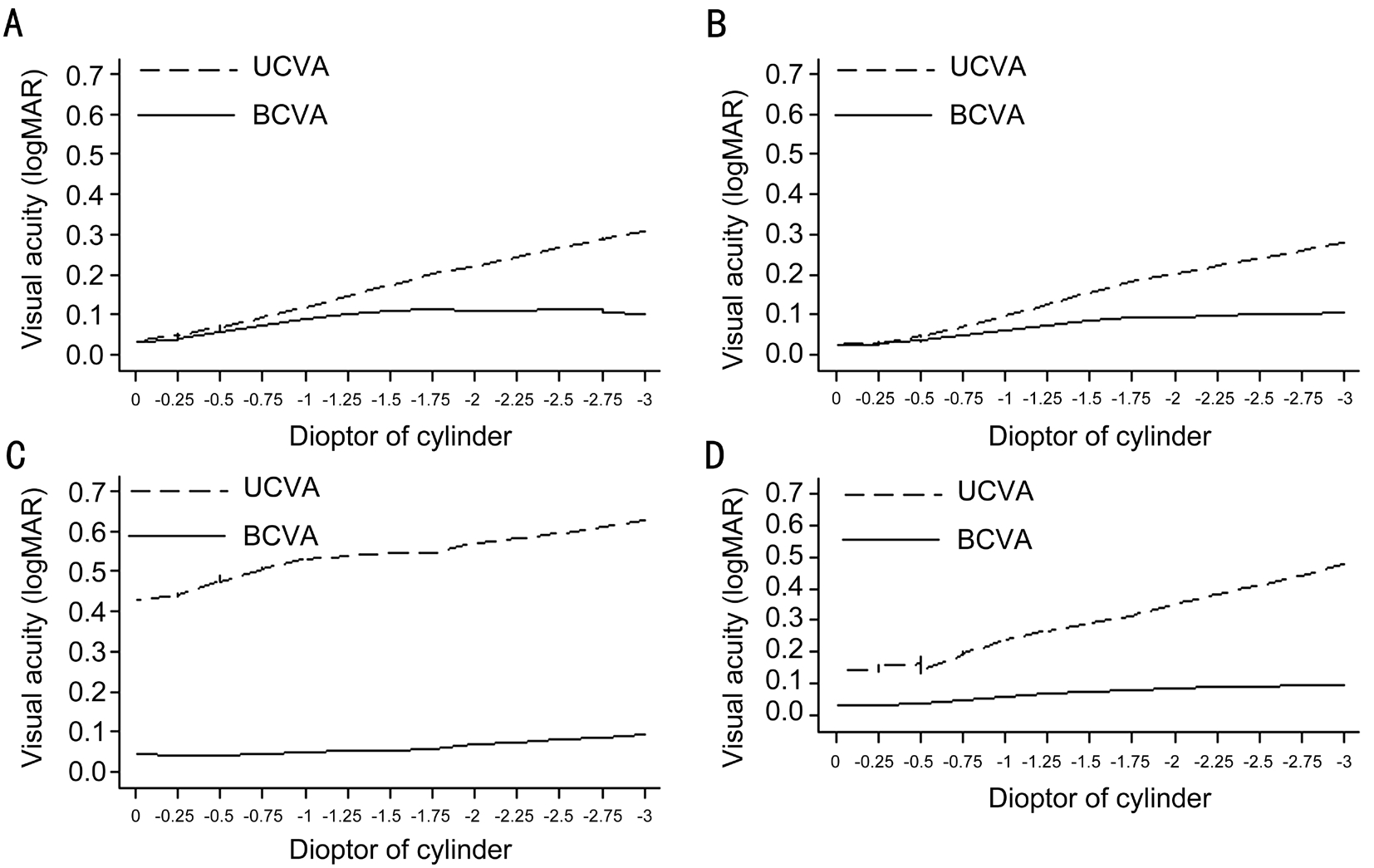
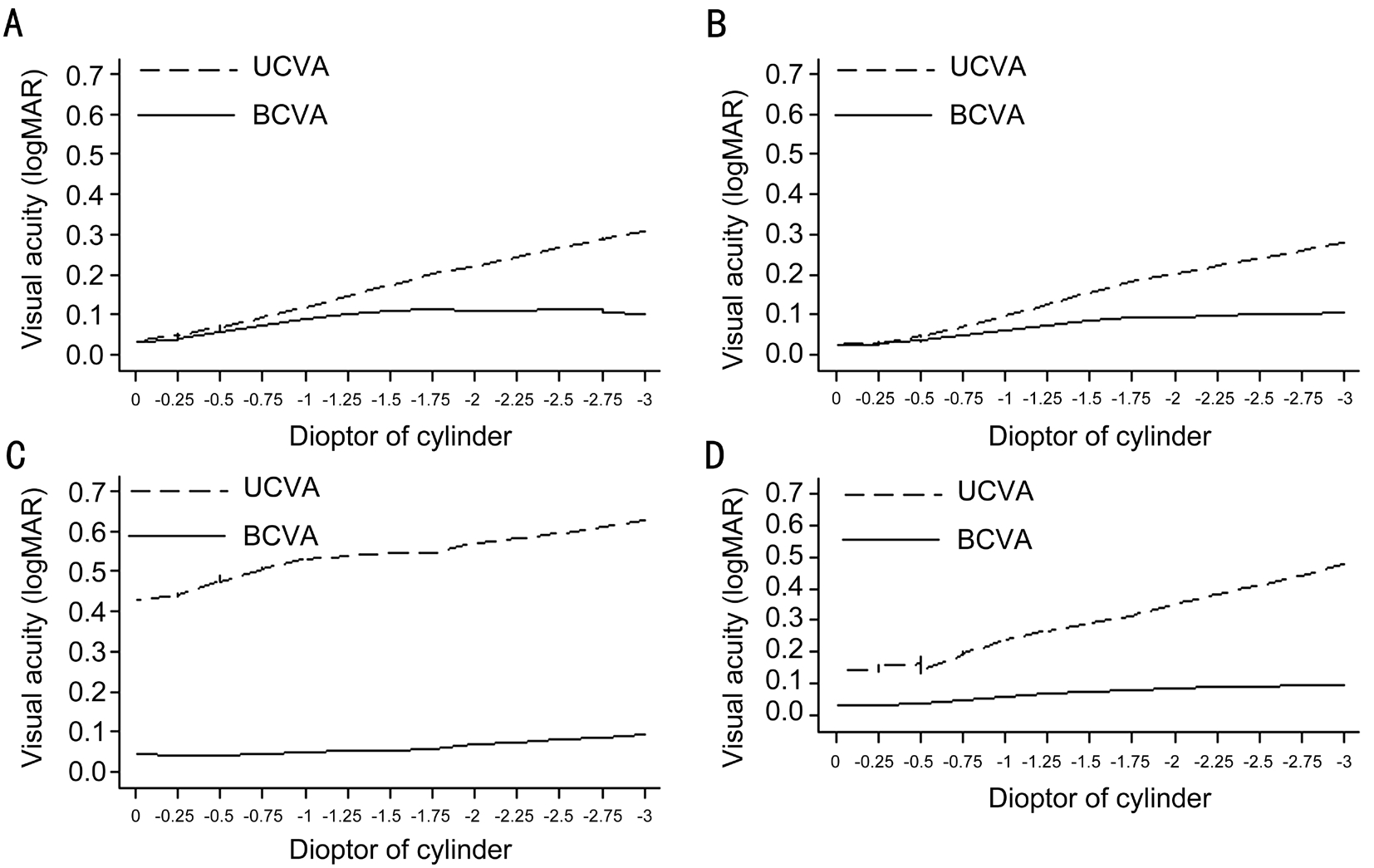
Figure 1 Lowess smoothed cylinder-specific distribution of BCVA and UCVA of children aged 7-15y of hyperopia, emmetropia, myopia and all children A: Hyperopia is defined as sphere power (minimum meridian) +1.00 D or more; B: Emmetropia is defined as sphere power(minimum meridian) more or equal to -0.50 D and less or equal to +0.75 D; C: Myopia is defined as sphere power (minimum meridian) -0.75 D or less; D: All children.
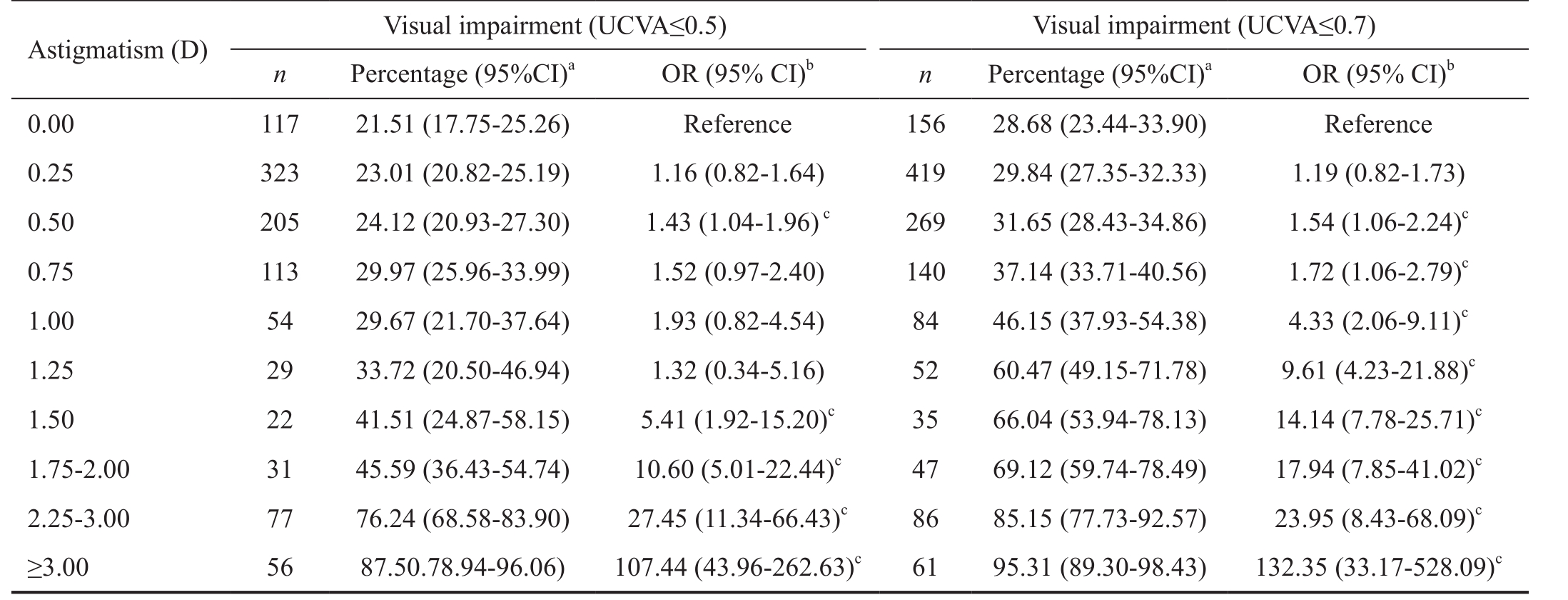
Table 1 Prevalence of uncorrected visual impairment by severity of astigmatism
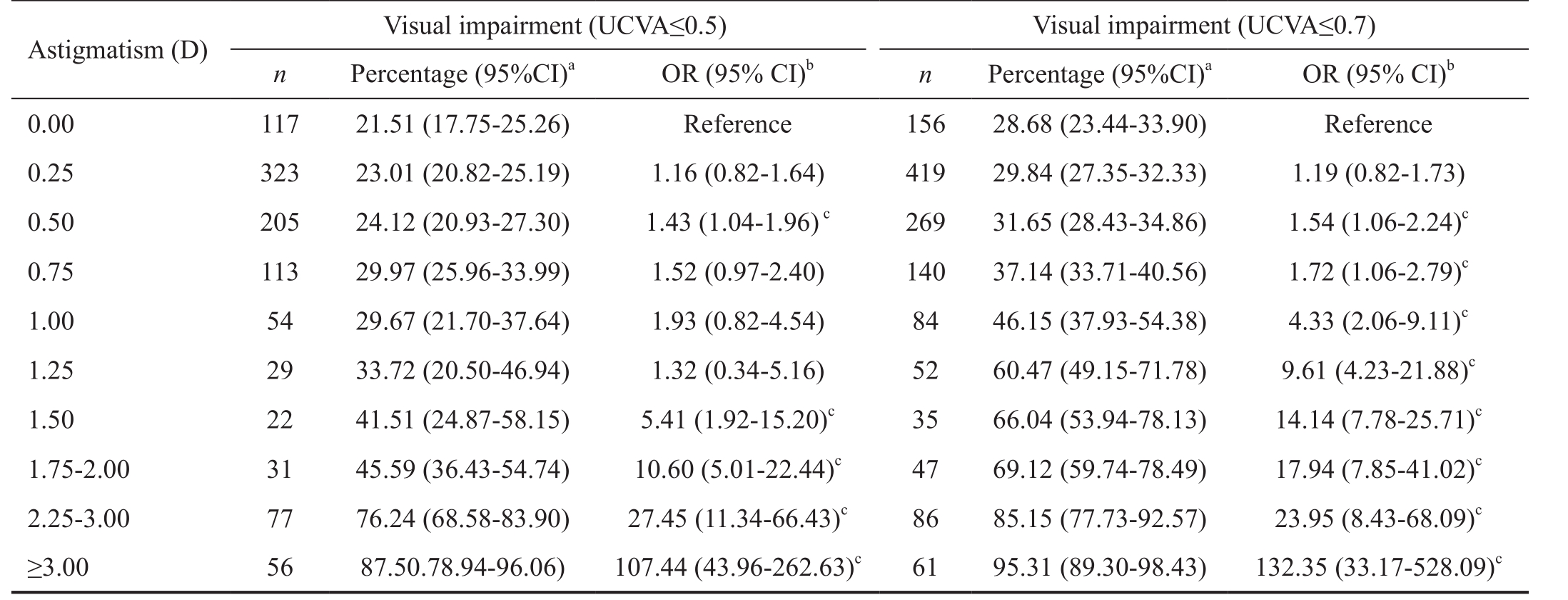
95%CI: 95% confidence interval; D: Diopter; UCVA: Uncorrected visual acuity; OR: Odds ratio.aVisual impairment is defined as UCVA ≤0.5 or 0.7 in the right eye.bAdjusted for age, gender, and absolute minimum meridian. Binomial Wald 95%CIs were calculated.cIndicated statistical significance.
Astigmatism (D) Visual impairment (UCVA≤0.5) Visual impairment (UCVA≤0.7)n Percentage (95%CI)aOR (95% CI)bn Percentage (95%CI)aOR (95% CI)b0.00 117 21.51 (17.75-25.26) Reference 156 28.68 (23.44-33.90) Reference 0.25 323 23.01 (20.82-25.19) 1.16 (0.82-1.64) 419 29.84 (27.35-32.33) 1.19 (0.82-1.73)0.50 205 24.12 (20.93-27.30) 1.43 (1.04-1.96)c269 31.65 (28.43-34.86) 1.54 (1.06-2.24)c0.75 113 29.97 (25.96-33.99) 1.52 (0.97-2.40) 140 37.14 (33.71-40.56) 1.72 (1.06-2.79)c1.00 54 29.67 (21.70-37.64) 1.93 (0.82-4.54) 84 46.15 (37.93-54.38) 4.33 (2.06-9.11)c1.25 29 33.72 (20.50-46.94) 1.32 (0.34-5.16) 52 60.47 (49.15-71.78) 9.61 (4.23-21.88)c1.50 22 41.51 (24.87-58.15) 5.41 (1.92-15.20)c35 66.04 (53.94-78.13) 14.14 (7.78-25.71)c1.75-2.00 31 45.59 (36.43-54.74) 10.60 (5.01-22.44)c47 69.12 (59.74-78.49) 17.94 (7.85-41.02)c2.25-3.00 77 76.24 (68.58-83.90) 27.45 (11.34-66.43)c86 85.15 (77.73-92.57) 23.95 (8.43-68.09)c≥3.00 56 87.50.78.94-96.06) 107.44 (43.96-262.63)c61 95.31 (89.30-98.43) 132.35 (33.17-528.09)c
Association of Astigmatism and Visual ImpairmentFigure 1 shows the distribution of logMAR BCVA and UCVA stratified by astigmatism severity of hyperopic, emmetropic and myopic spherical categories. As expected, BCVA and UCVA decreased with a higher degree of cylinder. UCVA was more affected by astigmatism and sphere than BCVA. In children without significant spherical error, mean logMAR BCVA reduced from 0.03±0.05 to 0.06±0.07, 0.12±0.08 from no astigmatism to one diopter astigmatism and astigmatism ≥3.00 D; mean UCVA was reduced to less than 0.03±0.06 to 0.09±0.12 and 0.38±0.13. In children with hyperopia, Mean BCVA reduced from 0.03±0.06 to 0.11±0.07, 0.12±0.02 from no astigmatism to one diopter astigmatism and astigmatism ˃3.00 D; mean UCVA was reduced to less than 0.32±0.06 to 0.13±0.08 and 0.41±0.16. In children with myopia, mean BCVA reduced from 0.04±0.07 to 0.06±0.08, 0.13±0.08 from no astigmatism to one diopter astigmatism and astigmatism ˃3.00 D; mean UCVA was reduced to less than 0.43±0.26 to 0.55±0.27 and 0.47±0.21.
In the multivariate linear regression model that included logMAR visual acuity, astigmatism (per diopter), age, gender,absolute minimum meridian (per diopter), statistically significant correlation was found between astigmatism magnitude and BCVA (standardized coefficient β=0.025,P˂0.001), astigmatism magnitude and UCVA (standardized coefficient β=0.051, P˂0.001).

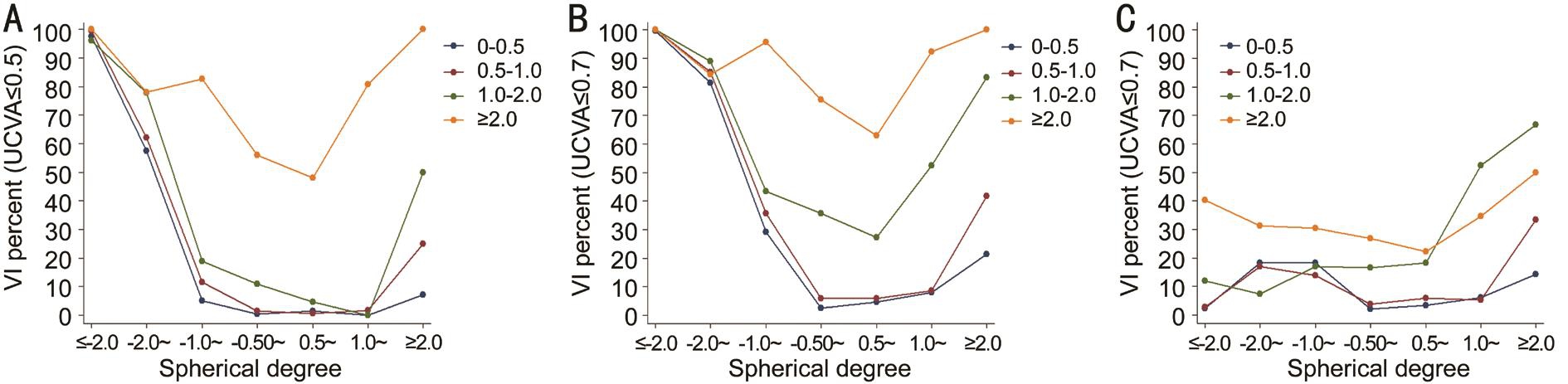
Figure 2 Proportion of visual impairment by cylinder severity in children aged 7-15y A: Proportion of UCVI (UCVA≤0.5) by cylinder; B:Proportion of UCVI (UCVA≤0.7) by cylinder; C: Proportion of BCVI (BCVA≤0.7) by cylinder.
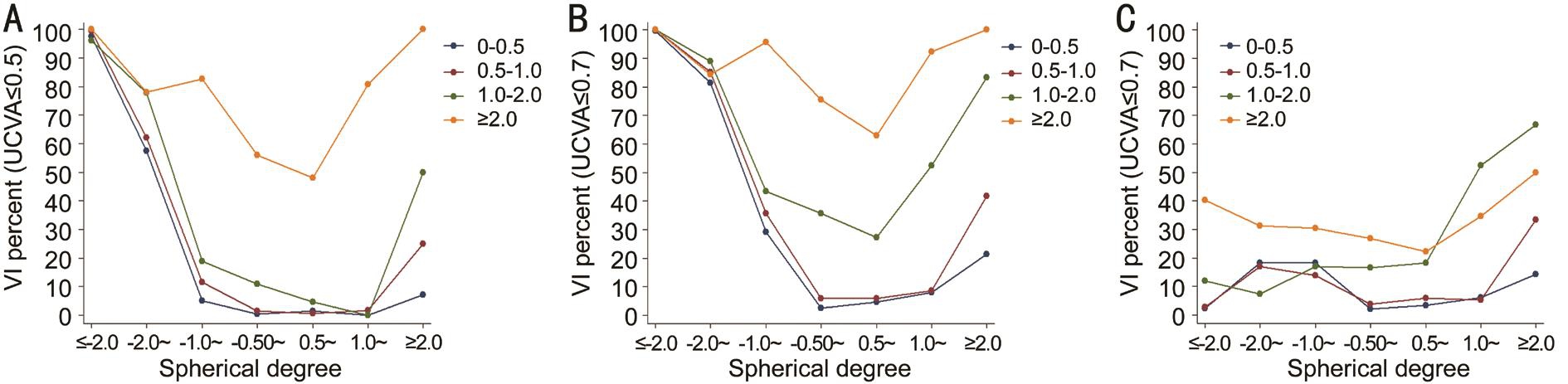
Figure 3 Relationship between visual impairment and cylinder severity after controlling for spherical degree in children aged 7-15y A:Visual impairment (UCVA≤0.5); B: Visual impairment (UCVA≤0.7); C: Visual impairment (BCVA≤0.7).
Distribution of uncorrected visual impairment (UCVI)stratified by astigmatism was shown in Table 1 & Figure 2.UCVI (UCVA≤0.5) increased from 21.51% in children without astigmatism to 87.5% of children with astigmatism ≥3.00 D and UCVI (UCVA≤0.7) increased from 28.68% of children without astigmatism to 95.31% of children with astigmatism≥3.00 D in the multivariate logistic regression model that included age (per year), gender, absolute minimum meridian(per diopter), astigmatism (per diopter) as covariates. Children with astigmatism 0.50 D, 1.00 D, more or equal to 3.00 D have 1.54, 4.33, 132.35 folds odds ratios for UCVI (UCVA≤0.7)than children without astigmatism.
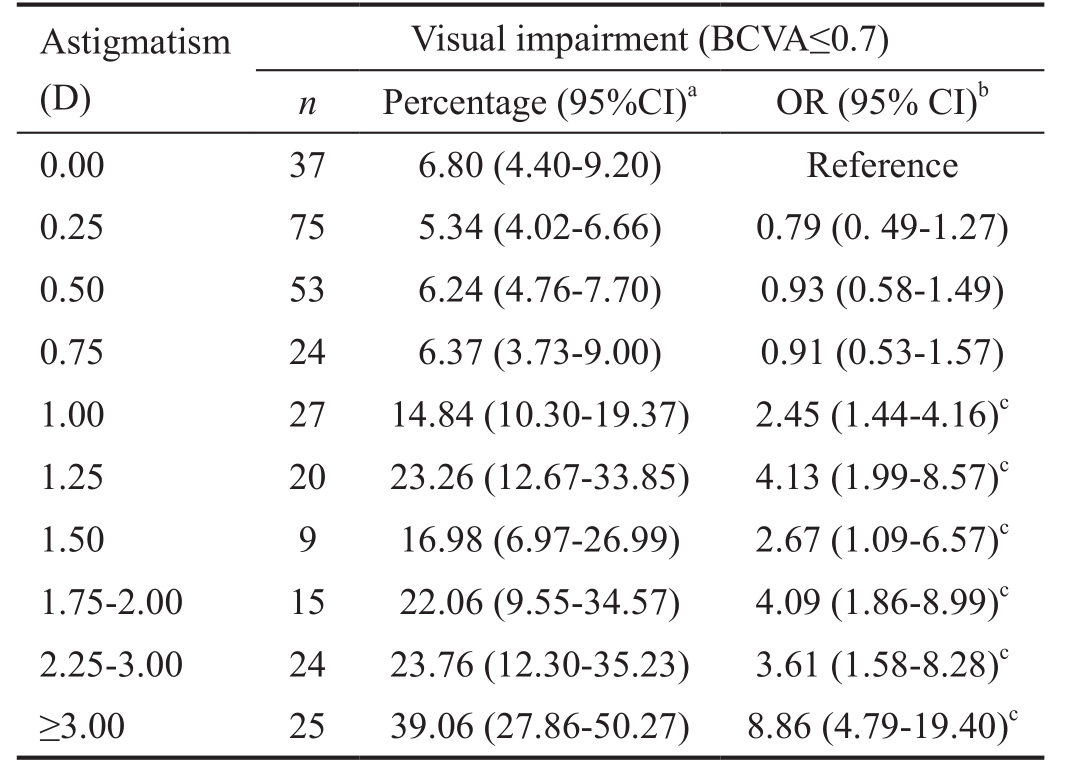
Distribution of best-corrected visual impairment (BCVI;BCVA≤0.7) stratified by astigmatism severity categories was shown in Figure 2. A substantially increase of BCVI was found in astigmatism of 1.00 D. BCVI raised from 6.80% of children without astigmatism to 39.06% of children with astigmatism more or equal to 3.00 D (Table 2). In the multivariate logistic regression model that included age (per year), gender, absolute minimum meridian (per diopter), astigmatism groups as covariates. Children with astigmatism 1.00 D, 1.75-2.00 D,more or equal to 3.00 D have 2.45, 4.09, 8.86 folds times risk of BCVI separately than children without astigmatism.
After controlling for spherical degree, astigmatism severity has considerable effect on visual impairment (Figure 3). Within the same spherical group, the prevalence of visual impairment increases considerably with astigmatism increased to more than 1.00 diopter. The proportion of UCVI was mainly driven by the sphere in myopic children but among the children with mild sphere diopters (-1 to +1 D), severe astigmatism (cylinder greater than 1 D) would lead to substantial UCVI (Figure 3A and 3B). Similarly, children with astigmatism ≥1.00 D hadgreater BCVI prevalence than the children with cylinder power less than 1.00 D (21.66%, 95%CI: 18.15%-25.17% vs 5.95%,95%CI: 4.96%-6.94%). In the multivariate logistic regression model that included age, gender, astigmatism≥1.00 D, absolute minimum meridian as covariates within hyperopic, emmetropic and myopic refraction categories. Proportions of BCVI were higher when the astigmatism ≥1.00 D and this was consistently found in every refraction category. (OR=10.87, 95%CI: 6.18-19.06 for hyperopic refraction category; OR=7.11, 95%CI:4.46-11.34 for emmetropic refraction category; OR=2.17,95%CI: 1.52-3.08 for myopic refraction category; OR=4.20,95%CI: 3.08-5.74 of all children aged 7-15y).
Table 2 Prevalence of best-corrected visual impairment by severity of astigmatism
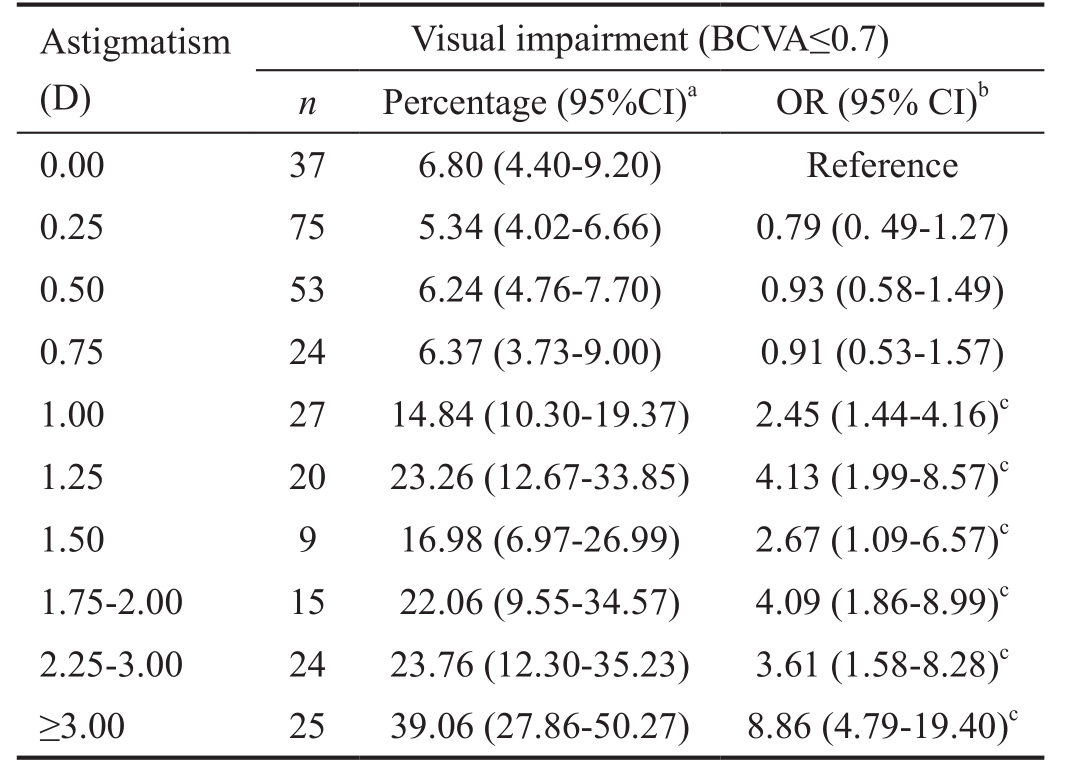
95%CI: 95% confidence interval; D: Diopter; BCVA: Best-corrected visual acuity; OR: Odds ratio.aVisual impairment is defined as BCVA≤0.7 in the right eye.bAdjusted for age, gender, and absolute minimum meridian. Binomial Wald 95%CIs were calculated.cIndicated statistical significance.
Visual impairment (BCVA≤0.7)n Percentage (95%CI)aOR (95% CI)b0.00 37 6.80 (4.40-9.20) Reference 0.25 75 5.34 (4.02-6.66) 0.79 (0. 49-1.27)0.50 53 6.24 (4.76-7.70) 0.93 (0.58-1.49)0.75 24 6.37 (3.73-9.00) 0.91 (0.53-1.57)1.00 27 14.84 (10.30-19.37) 2.45 (1.44-4.16)c1.25 20 23.26 (12.67-33.85) 4.13 (1.99-8.57)c1.50 9 16.98 (6.97-26.99) 2.67 (1.09-6.57)c1.75-2.00 15 22.06 (9.55-34.57) 4.09 (1.86-8.99)c2.25-3.00 24 23.76 (12.30-35.23) 3.61 (1.58-8.28)c≥3.00 25 39.06 (27.86-50.27) 8.86 (4.79-19.40)cAstigmatism(D)
Effect of Astigmatism Subtypes on Visual ImpairmentFigure 4 shows the distribution of BCVI stratified by astigmatism severity and astigmatism subtypes. Proportions of BCVI were higher in OBL than WTR and ATR astigmatism when the astigmatism ≥1.00 D in emmetropic refractive category. In the multivariate logistic regression model that included age,gender, astigmatism severity, astigmatism subtypes, absolute minimum meridian as covariates within clinically significant astigmatism (astigmatism ≥1.00 D) and hyperopic, emmetropic and myopic refraction categories, OBL astigmatism were associated with a higher risk of BCVI relative to WTR astigmatism in myopic refractive category (OR=12.87, 95%CI:2.20-75.38). No significant difference was found in UCVI among astigmatism subtypes.
DISCUSSION
Using Guangzhou RESC data, we firstly explored the influence of severity and type of astigmatism on visual acuity in the urban school children in southern China. The results showed that the prevalence of visual impairment was significantly associated with both the magnitude and subtypes of astigmatism after controlling for age, sex, and spherical powers. When the astigmatism ≥1.00 D, nearly 22% children had BCVA≤0.7. The OR of BCVI was 10.87 times higher than non-astigmatism, indicating a cylinder power ≥1.00 D may be an appropriate cutoff for clinical significant astigmatism. In addition, the OBL astigmatism was associated with higher risk for visual impairment than WTR at the same cylindrical levels of refractive error.
We found that the visual acuity was nearly linear declined in distance visual acuity with increasing severity of astigmatism(Figure 1). Furthermore, both the prevalence of UCVA and BCVA were increased with an increased cylinder power.Only few studies have reported the association between severity of astigmatism and visual performance. Villegas et al[23]reported astigmatism less than 0.5 D did not affect visual acuity. Guo and Atchison[24]reported that a reduction of 0.1 logMAR line of letters was associated with an average 0.28 D of induced cylindrical power. Another 2 studies reported that distance visual acuity declined linearly with increasing imposed astigmatism, with 1-2 lines of logMAR visual acuity per one diopter[25-26]. Other studies also have documented that astigmatism resulted in reduction of near visual acuity, functional visual impacts, and visual developments[27]. Astigmatism of 0.50 D had clinical significant more risk of UCVI (UCVA≤0.7) than children without astigmatism. The current study found that every diopter increases of cylinder were correlated with decreases in BCVA(β=0.025, P˂0.001) and UCVA (β=0.051, P˂0.001), which is corroborated with the aforementioned findings and underscores its clinical importance and highlights the need for astigmatism correction. The uncorrectable astigmatism demonstrated by substantially number of people with severe astigmatism was not corrected to normal vision may indicate the association of severe astigmatism and amblyopia.

Figure 4 Influence of severity and types of astigmatism on the prevalence of best-corrected visual acuity impairment(BCVA≤0.7) in children aged 7-15y W: With the rule; O: Oblique;A: Against the rule.
The lack of definition of clinical significant astigmatism contributes to the substantial discrepancies in astigmatism prevalence across studies, which often makes it impossible to analyze and compare the results directly. Various cutoffs of cylinder power were used for defining astigmatism. For example, 0.5 D in population-based studies in Iran and Brazil,0.75 D in Guangzhou RESC study, 1.0 D in CLEERS and SMS, 1.5 D in BPEDS, STARS and MEPEDS. There is a clear need for an agreed definition of clinically significant astigmatism, which requires more studies on how cylindrical errors affect visual acuity. Our results based on large-scale population showed that the prevalence of visual impairment increased substantially when cylinder power of ≥1.00 D,indicating that this value may be an appropriate astigmatism cutoff. Astigmatism ≥1.00 D bring in a decrease in BCVA and an increase in BCVI in hyperopic, emmetropic and myopic eyes, suggesting that higher levels of cylinder produce optical distortions that are not completely correctable by the usual correction of both sphere and cylinder.
The influence of stigmatism axis on visual acuity remains controversial. Some studies reported that reduction in distance visual acuity with induced astigmatism was greatest in ATR or OBL astigmatism, and least in WTR astigmatism[28-29].However, other studies did not observe significant correlations between cylinder axis and visual impairment[30-31]. The discrepancy between studies may be associated with the differences in methodology, accommodation and pupil size. Previous study reported that OBL astigmatism related amblyopia require longer treatment[32]. This study observed more visual impairment due to OBL astigmatism than WTR astigmatism in the myopic refractive category, indicating that children with clinically significant OBL astigmatism should be corrected. Further studies with large sample size and various ethnic origins are warranted to confirm or refute our findings.Astigmatism is associated with substantial social and financial burden worldwide. Though the exact cost for astigmatism correction was unavailable, the WHO estimated that the global cost of uncorrected refractory errors was 20 000 million US dollars and led to annually 202 000 million US dollar loss of gross domestic product in 2007. Additional 47 000 fulltime functional clinical refractionists and 18 000 ophthalmic dispensers were needed[33]. For Singapore school children,it was reported that and annual direct cost of myopia was$221.68 (US$148) per subject[34]. Another study estimated that at least $3.8 billion annually were needed for correcting distance vision impairment, and the majority of them were myopia, hyperopia, and astigmatism[35]. Our results showed that compulsory correction of astigmatism ˂1.0 D may be unnecessary because it causes low proportion of visual impairment.
The strength of this study lies in the population-based design and use of standardized recruitment strategy and methodology.This study has limitations. Firstly, the nature of cross-sectional design prevents the cause-effect inference, thus the definitive evidence is needed by longitudinal data. Secondly, no near visual acuity or functional impact of astigmatism was included in the current study. Thirdly, the influence of astigmatism on visual acuity was also related to other factors, including the higher-order aberrations, pupil size, the accommodative status,cortex adaptation to astigmatism. Further studies adjusting these factors were warranted.
In conclusion, the severity and types of astigmatism significantly affected both the UCVA and BCVA. Astigmatism≥1.00 D causes significantly more BCVI, suggesting that cylinder power ≥1.00 D is an appropriate cutoff, for defining clinically significant astigmatism. OBL astigmatism causes more visual acuity loss than WTR at the same level of cylindrical error. Further studies with large sample size and multiple ethnicities are needed to confirm or refute our findings.
ACKNOWLEDGEMENTS
Authors’ contributions:He MG designed the experimental protocol and collected the data. All authors were involved in the analysis. Wang LL wrote the first draft of the manuscript.He MG, Wang W and Han XT reviewed and revised the manuscript and produced the final version. All authors read and approved the final manuscript.
Foundations:Supported by the World Health Organization under National Institute of Health contract N01-EY-2103;Fundamental Research Funds of the State Key Laboratory in Ophthalmology; National Natural Science Foundation of China (No.81125007); The Research Accelerator Program was at University of Melbourne and the CERA Foundation.The Centre for Eye Research Australia receives Operational Infrastructure Support from the Victorian State Government.
Conflicts of Interest:Wang LL, None; Wang W, None; Han XT, None; He MG, None.
REFERENCES
1 Harvey EM. Development and treatment of astigmatism-related amblyopia. Optom Vis Sci 2009;86(6):634-639.
2 Gwiazda J, Grice K, Held R, McLellan J, Thorn F. Astigmatism and the development of myopia in children. Vision Res 2000;40(8):1019-1026.
3 Twelker JD, Miller JM, Sherrill DL, Harvey EM. Astigmatism and myopia in Tohono O’odham Native American children. Optom Vis Sci 2013;90(11):1267-1273.
4 Narayanasamy S, Vincent SJ, Sampson GP, Wood JM. Simulated astigmatism impairs academic-related performance in children.Ophthalmic Physiol Opt 2015;35(1):8-18.
5 Wills J, Gillett R, Eastwell E, Abraham R, Coffey K, Webber A, Wood J. Effect of simulated astigmatic refractive error on reading performance in the young. Optom Vis Sci 2012;89(3):271-276.
6 Harvey EM, Miller JM, Twelker JD, Davis AL. Reading fluency in school-aged children with bilateral astigmatism. Optom Vis Sci 2016;93(2):118-125.
7 He M, Zeng J, Liu Y, Xu J, Pokharel GP, Ellwein LB. Refractive error and visual impairment in urban children in southern China. Invest Ophthalmol Vis Sci 2004;45(3):793-799.
8 Xiao X, Liu WM, Ye YJ, Huang JZ, Luo WQ, Liu HT, Lin Q, Zhao WX, Lin EW. Prevalence of high astigmatism in children aged 3 to 6y in Guangxi, China. Optom Vis Sci 2014;91(4):390-396.
9 Chan SE, Kuo HK, Tsai CL, Wu PC. Astigmatism in Chinese primary school children: prevalence, change, and effect on myopic shift. Jpn J Ophthalmol 2018;62(3):321-326.
10 Li Z, Xu K, Wu S, Lv J, Jin D, Song Z, Wang Z, Liu P. Populationbased survey of refractive error among school-aged children in rural northern China: the Heilongjiang eye study. Clin Exp Ophthalmol 2014;42(4):379-384.
11 Wu JF, Bi HS, Wang SM, Hu YY, Wu H, Sun W, Lu TL, Wang XR,Jonas JB. Refractive error, visual acuity and causes of vision loss in children in Shandong, China. The Shandong Children Eye Study. PLoS One 2013;8(12):e82763.
12 Kleinstein RN, Jones LA, Hullett S, Kwon S, Lee RJ, Friedman NE,Manny RE, Mutti DO, Yu JA, Zadnik K; Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error Study Group. Refractive error and ethnicity in children. Arch Ophthalmol 2003;121(8):1141-1147.13 Fozailoff A, Tarczy-Hornoch K, Cotter S, Wen G, Lin J, Borchert M,Azen S, Varma R; Writing Committee for the MEPEDS Study Group.Prevalence of astigmatism in 6- to 72-month-old African American and Hispanic children: the Multi-ethnic Pediatric Eye Disease Study.Ophthalmology 2011;118(2):284-293.
14 Huang J, Maguire MG, Ciner E, Kulp MT, Cyert LA, Quinn GE, Orel-Bixler D, Moore B, Ying GS; Vision in Preschoolers (VIP) Study Group.Risk factors for astigmatism in the Vision in Preschoolers Study. Optom Vis Sci 2014;91(5):514-521.
15 Hashemi H, Nabovati P, Malekifar A, Yekta A, Ostadimoghaddam H, Jafarzadehpur E, Khabazkhoob M. Astigmatism in underserved rural areas: a population based study. Ophthalmic Physiol Opt 2016;36(6):671-679.
16 Huynh SC, Kifley A, Rose KA, Morgan I, Heller GZ, Mitchell P. Astigmatism and its components in 6-year-old children. Invest Ophthalmol Vis Sci 2006;47(1):55-64.
17 Huynh SC, Kifley A, Rose KA, Morgan IG, Mitchell P. Astigmatism in 12-year-old Australian children: comparisons with a 6-year-old population. Invest Ophthalmol Vis Sci 2007;48(1):73-82.
18 Dirani M, Chan YH, Gazzard G, Hornbeak DM, Leo SW, Selvaraj P,Zhou B, Young TL, Mitchell P, Varma R, Wong TY, Saw SM. Prevalence of refractive error in Singaporean Chinese children: the strabismus,amblyopia, and refractive error in young Singaporean Children (STARS)study. Invest Ophthalmol Vis Sci 2010;51(3):1348-1355.
19 Giordano L, Friedman DS, Repka MX, Katz J, Ibironke J, Hawes P, Tielsch JM. Prevalence of refractive error among preschool children in an urban population: the Baltimore Pediatric Eye Disease Study.Ophthalmology 2009;116(4):739-746,746.e1-e4.
20 Wen G, Tarczy-Hornoch K, McKean-Cowdin R, Cotter SA, Borchert M, Lin J, Kim J, Varma R; Multi-Ethnic Pediatric Eye Disease Study Group. Prevalence of myopia, hyperopia, and astigmatism in non-Hispanic white and Asian children: multi-ethnic pediatric eye disease study. Ophthalmology 2013;120(10):2109-2116.
21 He M, Huang W, Zheng Y, Huang L, Ellwein LB. Refractive error and visual impairment in school children in rural southern China.Ophthalmology 2007;114(2):374-382.
22 Negrel AD, Maul E, Pokharel GP, Zhao J, Ellwein LB. Refractive Error Study in Children: sampling and measurement methods for a multicountry survey. Am J Ophthalmol 2000;129(4):421-426.
23 Villegas EA, Alcón E, Artal P. Minimum amount of astigmatism that should be corrected. J Cataract Refract Surg 2014;40(1):13-19.
24 Guo H, Atchison DA. Subjective blur limits for cylinder. Optom Vis Sci 2010;87(8):E549-E559.
25 Dobson V, Miller JM, Harvey EM, Mohan KM. Amblyopia in astigmatic preschool children. Vision Res 2003;43(9):1081-1090.
26 Harvey EM, Dobson V, Miller JM. Prevalence of high astigmatism,eyeglass wear, and poor visual acuity among Native American grade school children. Optom Vis Sci 2006;83(4):206-212.
27 Read SA, Vincent SJ, Collins MJ. The visual and functional impacts of astigmatism and its clinical management. Ophthalmic Physiol Opt 2014;34(3):267-294.
28 Wolffsohn JS, Bhogal G, Shah S. Effect of uncorrected astigmatism on vision. J Cataract Refract Surg 2011;37(3):454-460.
29 Chen SI, Hove M, McCloskey CL, Kaye SB. The effect of monocularly and binocularly induced astigmatic blur on depth discrimination is orientation dependent. Optom Vis Sci 2005;82(2):101-113.
30 Remón L, Tornel M, Furlan WD. Visual acuity in simple myopic astigmatism: influence of cylinder axis. Optom Vis Sci 2006;83(5):311-315.
31 Remón L, Monsoriu JA, Furlan WD. Influence of different types of astigmatism on visual acuity. J Optom 2017;10(3):141-148.
32 Chou YS, Tai MC, Chen PL, Lu DW, Chien KH. Impact of cylinder axis on the treatment for astigmatic amblyopia. Am J Ophthalmol 2014;157(4):908-914.e1.
33 Fricke TR, Holden BA, Wilson DA, Schlenther G, Naidoo KS,Resnikoff S, Frick KD. Global cost of correcting vision impairment from uncorrected refractive error. Bull World Health Organ 2012;90(10):728-738.
34 Lim MC, Gazzard G, Sim EL, Tong L, Saw SM. Direct costs of myopia in Singapore. Eye (Lond) 2009;23(5):1086-1089.
35 Vitale S, Cotch MF, Sperduto R, Ellwein L. Costs of refractive correction of distance vision impairment in the United States, 1999-2002.Ophthalmology 2006;113(12):2163-2170.
Correspondenceto:Ming-Guang He. State Key Laboratory of Ophthalmology, Zhongshan Ophthalmic Center, Sun Yat-sen University, 54S. Xianlie Road, Guangzhou 510060, Guangdong Province, China. mingguang_he@yahoo.com
Received:2018-04-26 Accepted: 2018-05-28
Abstract● AlM: To investigate the influence of astigmatism on visual acuity in school-aged children, and to define a cutoff for clinically significant astigmatism.● METHODS: This is a population-based, cross-sectional study. Among 5053 enumerated children aged 5-15y in Guangzhou, 3729 (73.8%) children aged 7-15 with successful cycloplegic auto-refraction (1% cyclopentolate)and a reliable visual acuity measurement were included.Ocular measurement included external eye, anterior segment, media and fundus and cycloplegic auto-refraction.Primary outcome measures included the relationship between severity and subtypes of astigmatism and the prevalence of visual impairment. Three criteria for visual impairment were adopted: best-corrected visual acuity(BCVA) ≤0.7, uncorrected visual acuity (UCVA) ≤0.5 or <0.7 in the right eye.● RESULTS: lncreases of cylinder power was significantly associated with worse visual acuity (UCVA: β=0.051,P<0.01; BCVA: β=0.025, P<0.001). A substantial increase in UCVl and BCVl was seen with astigmatism of 1.00 diopter (D) or more. Astigmatism ≥1.00 D had a greater BCVl prevalence than cylinder power less than 1.00 D (OR=4.20,95%Cl: 3.08-5.74), and this was also true for hyperopic,emmetropic and myopic refraction categories. Oblique astigmatism was associated with a higher risk of BCVl relative to with the rule astigmatism in myopic refractive category (OR=12.87, 95%Cl: 2.20-75.38).● CONCLUSlON: Both magnitude and subtypes of astigmatism influence the prevalence of visual impairment in school children. Cylinder ≥1.00 D may be useful as a cutoff for clinically significant astigmatism.
● KEYWORDS:astigmatism; visual acuity; children;population-based study
DOl:10.18240/ijo.2018.08.20
Citation:Wang LL, Wang W, Han XT, He MG. Influence of severity and types of astigmatism on visual acuity in school-aged children in southern China. Int J Ophthalmol 2018;11(8):1377-1383