Prevalence and characteristics of peripheral myopic retinopathy in Guangzhou office workers
Ting Zhang1, Yan-Tao Wei1, Wen-Bin Huang1,2, Rong-Jiao Liu1, Ya-Jing Zuo1, Li-Wen He1, Li-Ting Zhong1,Shao-Chong Zhang1
1State Key Laboratory of Ophthalmology, Zhongshan Ophthalmic Center, Sun Yat-Sen University, Guangzhou 510060, Guangdong Province, China
2Department of Ophthalmology, the Second Affiliated Hospital of Guangzhou Medical University, Guangzhou 510260,Guangdong Province, China
INTRODUCTION
M yopia has become a major global public health concern especially in East Asian countries and regions, such as mainland China, Taiwan, Hong Kong, and Japan[1]. In urban areas of these countries and regions, 80%-90% of children completing high school are now myopic[2]. In the Beijing Eye Study (n=4439, aged 40-90y), the prevalence of myopia,defined as a spherical equivalent (SE) of ˂-0.50 D, was reported as 22.9%[3], whereas it was about 16.8% in adults aged 40y or older (n=5927) in the Los Angeles Latino Eye Study[4].
Individuals with myopia have an increased risk of myopic retinopathy, which involves the posterior pole and includes peripheral retinal changes, such as posterior staphyloma,lacquer cracks, Fuchs’ spot, chorioretinal atrophy, lattice, paving stone, white-without-pressure (WWOP), and pigmentary degenerations, as well as retinal tears[5]. Myopic retinopathy was reported as the second leading cause of visual impairment among Chinese individuals 40y or older[6-8]and the third leading cause of bilateral poor vision among Japanese individuals 40y or older[9]. The Danish Copenhagen City Eye Study reported that myopic retinopathy was the major contributor to low vision among subjects aged 20 to 64y[10].More recently, Tokoro[11]estimated a prevalence of myopic retinopathy of 1.0% in the Japanese general population. Hu[12]screened a large Chinese population and reported a prevalence of 1.0% for myopic retinopathy.
Although myopic retinopathy is one of the major causes of low vision in working-aged populations, the prevalence and characteristics of myopic degeneration has not been documented in work-based studies. The higher prevalence of myopia in east Asian countries seems to be associated with intensive near work (reading and writing), which has reduced the time workers spend outside[13]. However, the type of myopia associated with myopic retinopathy in office workers has not been established.
The aim of this study was to examine the pattern of myopiarelated peripheral changes in adult Guangzhou office workers with myopia and to correlate these findings with refractive error (RE) and axial length (AL). The ultimate goal of this research is to provide useful information for the public regarding this ocular health issue and to raise awareness among eye care professionals regarding risk factors in vulnerable myopic office workers.
SUBJECTS AND METHODS
SubjectsWe undertook a cross-sectional study of the office workers who operated the 955 office works in the 31 different departments of the Guangzhou Power Supply Bureau, Guangdong Province, China. A comprehensive ocular examination was performed. Visual acuity was assessed using a decimal visual acuity chart. Intraocular pressure (IOP) was measured by a noncontact tonometer (TX-20, Canon, Inc.,Tokyo, Japan). Slit-lamp anterior segment was examined by noncycloplegic, and an optical biometry-ray was traced by IOLMaster(Carl Zeiss Meditec AG, Jena, Germany).The findings of fundus examinations, including varied peripheral myopic retinopathy, were recorded. And before fundus examination, the pupils were dilated by tropicamide phenylephrine eye drops.
The study was approved by the Institutional Review Board of the Zhongshan Ophthalmic Center and adhered to the tenets of the Declaration of Helsinki. Written informed consent was obtained from all participants.
Assessment of Refractive Error and Axial LengthThe SE was defined as a sphere plus a half negative cylinder for any myopia (SE˂-0.5 D) and hyperopia (SE˃+0.5 D). Mild myopia was defined as -3.0 D≤SE˂-0.5 D; moderate myopia as -6.0 D≤SE˂-3.0 D; high myopia as SE˂-6.0 D. Each office worker’s RE was obtained under cyclo condition with an auto refractor instrument (AR-330A/310A, Nidek Co., Ltd.,Beautshire, Japan). Subsequently, subjective refraction was determined by trained and certified study optometrists to achieve BCVA. The final subjective refraction result was used in the analysis. AL was measured by optical biometry using the Zeiss IOLMaster (Meditec AG, Jena, Germany).
Assessment of Peripheral RetinopathyStandard digital fundus photography for the central fundus was performed for all subjects by the same observer. Furthermore all subjects were imaged with a scanning laser ophthalmoscope (SLO,Daytona®, Optos, United Kingdom). If any suspicious peripheral retinopathy was observed by SLO, the standard consisted of observation from the dilated fundus examination with slit-lamp microscopy, combined with the three mirror contact lens, and this was recorded on a pre-designed form.Before the three mirror contact lens examinations, the pupil size was dilated at least 6 mm, measured using a Haab’s pupillometer.
Statistical AnalysisData were expressed as the mean±standard deviation (SD). Demographic data, as well as clinical measurements, were tabulated for all REs. The significance of differences among SE groups was determined using the χ2test for categorical variables, analysis of variance (ANOVA)for normally distributed variables, and the Kruskal-Wallis test for continuous variables that were not normally distributed.The significant differences of eyes with and without peripheral retinal changes were determined using the χ2test for categorical variables, the independent sample t-test when the data were normally distributed, or the Mann-Whitney U test when the data showed a nonparametric distribution. Logistic regression was used to identify potential participant characteristics that were associated with retinal changes. The associated factors were evaluated using a generalized estimating equation model,taking into consideration the correlation structure between both eyes of the subjects. For all tests, P˂0.05 was considered statistically significant. The data were processed and analyzed statistically using STATA software, version 14.0 (STATA Corp., College Station, TX, USA).
RESULTS
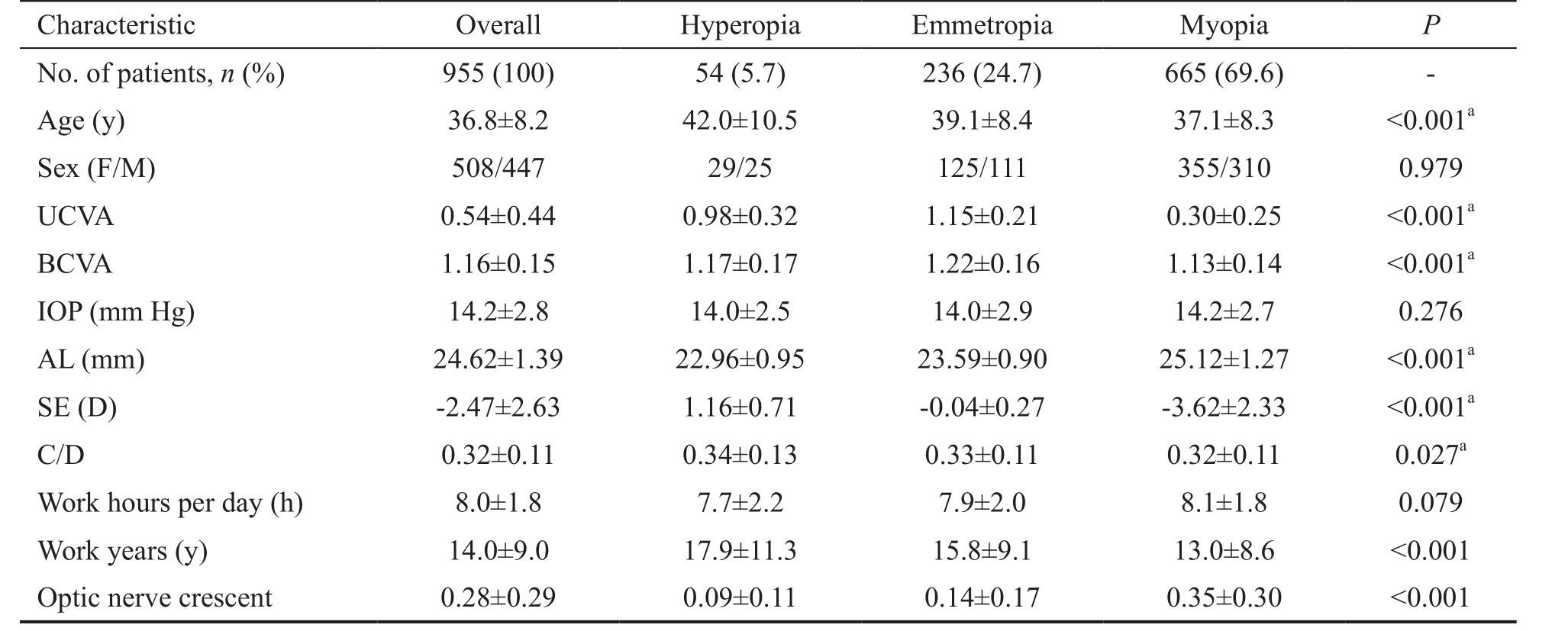
In this study, we included 1910 eyes of 955 subjects (508 females and 447 males) with a mean age of 36.8±8.2y (range,21 to 59y). Myopia was found in 69.6% of the eyes. The mean uncorrected visual acuity (UCVA) of all subjects was 0.54±0.44 (median, 0.40; range, 0.02 to 1.5), while the mean BCVA of all subjects was 1.16±0.15 (median, 1.2; range, 0.1 to 1.5). The mean AL was 24.62±1.39 mm, and the mean SE was-2.47±2.63 D (median, -1.75; range, -15.0 to 4.5). The mean work time was 8.0±1.8h. The myopia group had a younger age and worse UCVA and BCVA when compared with the other groups (P˂0.001). As expected, the AL was significantly longer, the SE was much higher, and the optic nerve crescent was significantly larger in subjects with myopia than with hyperopia and emmetropia. No significant gender, IOP, cupto-disc ratio (C/D), or work time differences were noted for subjects with myopia, hyperopia, or emmetropia. Details of the demographic and clinical data of the study population are shown in Table 1.
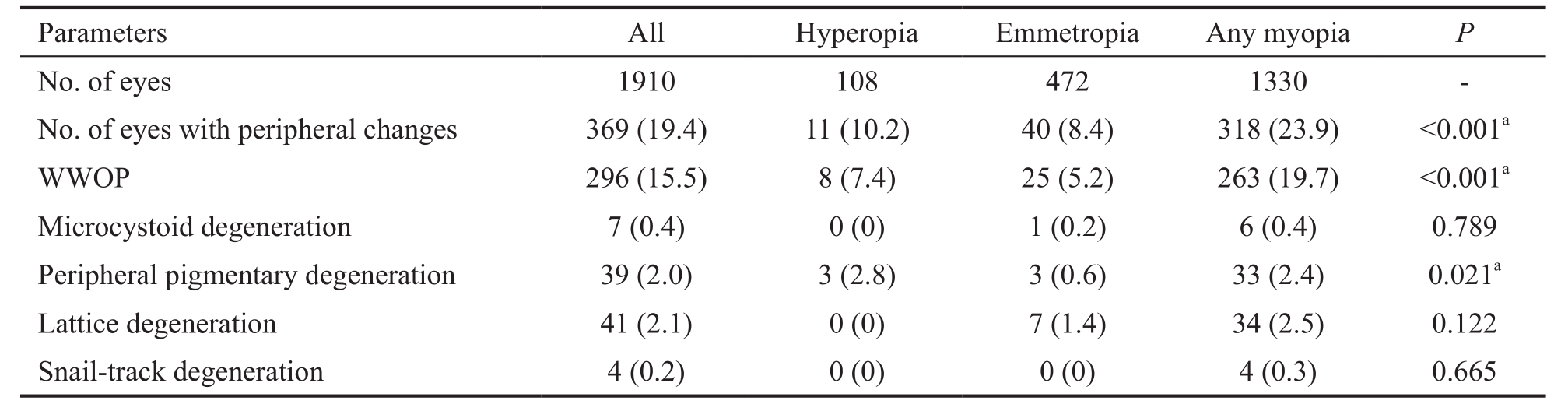
Frequencies of Myopia-related Retinal ChangesThe frequencies of myopia-related retinal changes among the different RE groups are shown in Table 2. Previous studies classified various changes as myopia-related retinal changes, and same classification was also adopted in this study[14-15]. Myopic eyes had more peripheral retinal changes (23.9%) [WWOP(19.7%, P˂0.001), peripheral pigmentary degeneration (2.4%,P=0.021)] when compared with the other two groups.
Table 1 Clinical characteristics of the study subjects
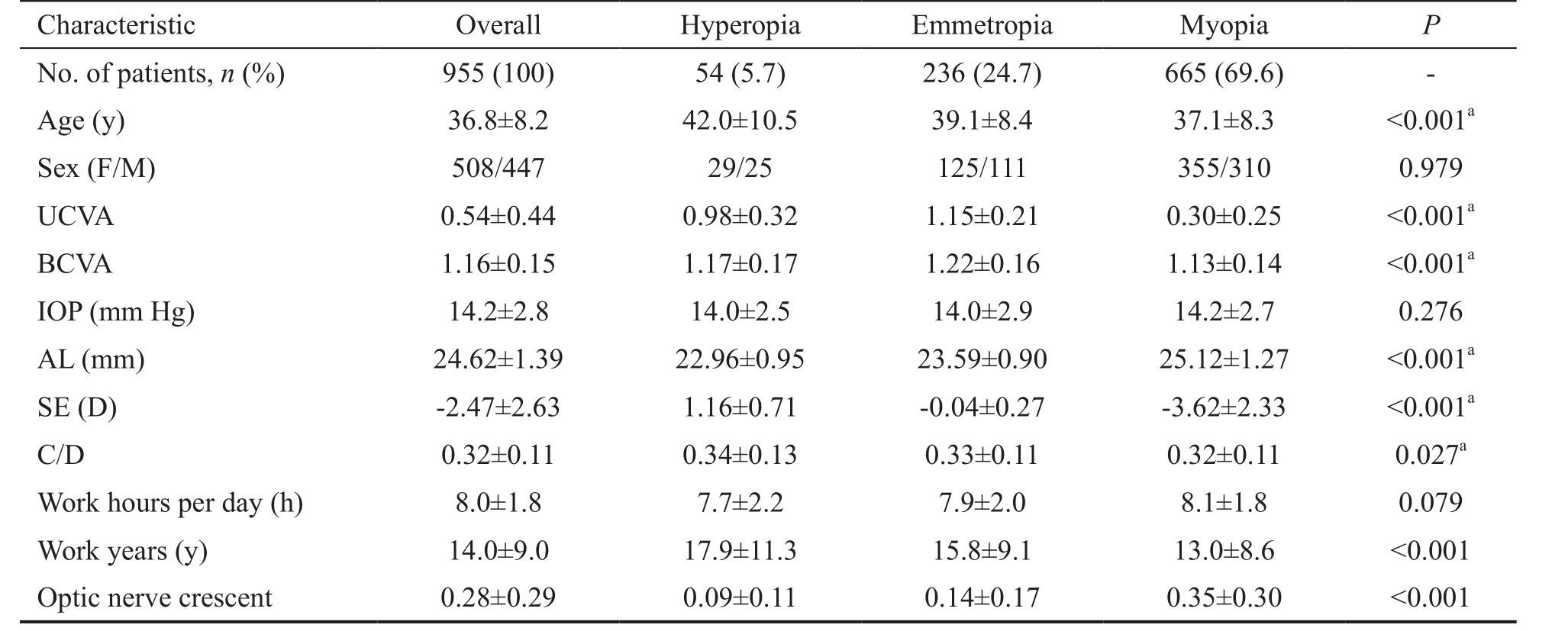
Data are expressed as the mean±SD. UCVA: Uncorrected visual acuity; BCVA: Best-corrected visual acuity; IOP: Intraocular pressure; AL: Axial length; SE: Spherical equivalent; D: Diopter; C/D: Cup/disc ratio.aSignificance.
Characteristic Overall Hyperopia Emmetropia Myopia P No. of patients, n (%) 955 (100) 54 (5.7) 236 (24.7) 665 (69.6) -Age (y) 36.8±8.2 42.0±10.5 39.1±8.4 37.1±8.3 ˂0.001aSex (F/M) 508/447 29/25 125/111 355/310 0.979 UCVA 0.54±0.44 0.98±0.32 1.15±0.21 0.30±0.25 ˂0.001aBCVA 1.16±0.15 1.17±0.17 1.22±0.16 1.13±0.14 ˂0.001aIOP (mm Hg) 14.2±2.8 14.0±2.5 14.0±2.9 14.2±2.7 0.276 AL (mm) 24.62±1.39 22.96±0.95 23.59±0.90 25.12±1.27 ˂0.001aSE (D) -2.47±2.63 1.16±0.71 -0.04±0.27 -3.62±2.33 ˂0.001aC/D 0.32±0.11 0.34±0.13 0.33±0.11 0.32±0.11 0.027aWork hours per day (h) 8.0±1.8 7.7±2.2 7.9±2.0 8.1±1.8 0.079 Work years (y) 14.0±9.0 17.9±11.3 15.8±9.1 13.0±8.6 ˂0.001 Optic nerve crescent 0.28±0.29 0.09±0.11 0.14±0.17 0.35±0.30 ˂0.001
Table 2 Frequencies of peripheral myopia-related retinal changes in the study subjects n (%)
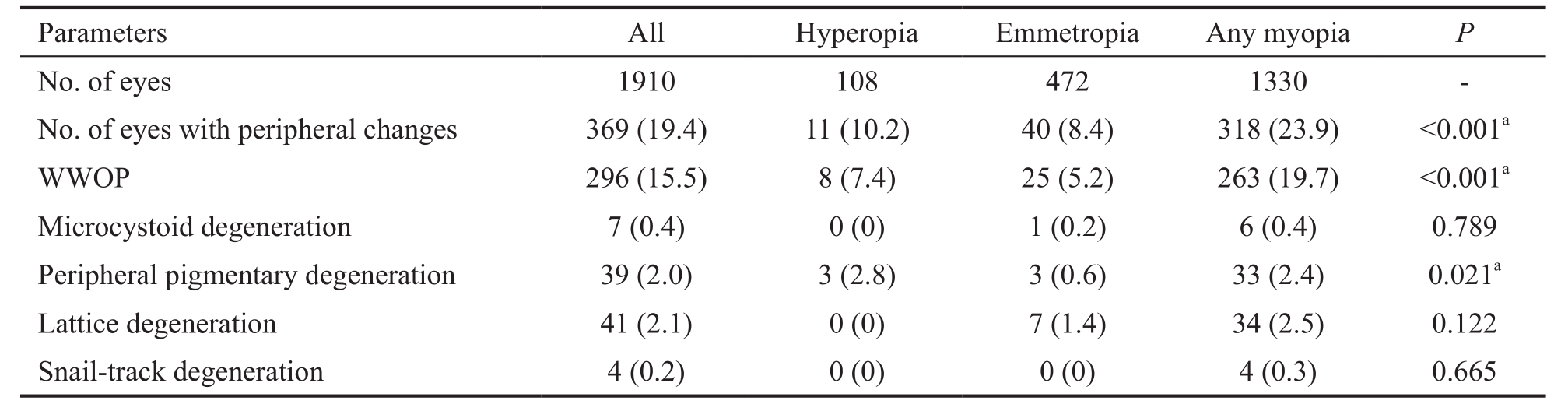
WWOP: White-without-pressure.aSignificance.
Parameters All Hyperopia Emmetropia Any myopia P No. of eyes 1910 108 472 1330 -No. of eyes with peripheral changes 369 (19.4) 11 (10.2) 40 (8.4) 318 (23.9) ˂0.001aWWOP 296 (15.5) 8 (7.4) 25 (5.2) 263 (19.7) ˂0.001aMicrocystoid degeneration 7 (0.4) 0 (0) 1 (0.2) 6 (0.4) 0.789 Peripheral pigmentary degeneration 39 (2.0) 3 (2.8) 3 (0.6) 33 (2.4) 0.021aLattice degeneration 41 (2.1) 0 (0) 7 (1.4) 34 (2.5) 0.122 Snail-track degeneration 4 (0.2) 0 (0) 0 (0) 4 (0.3) 0.665
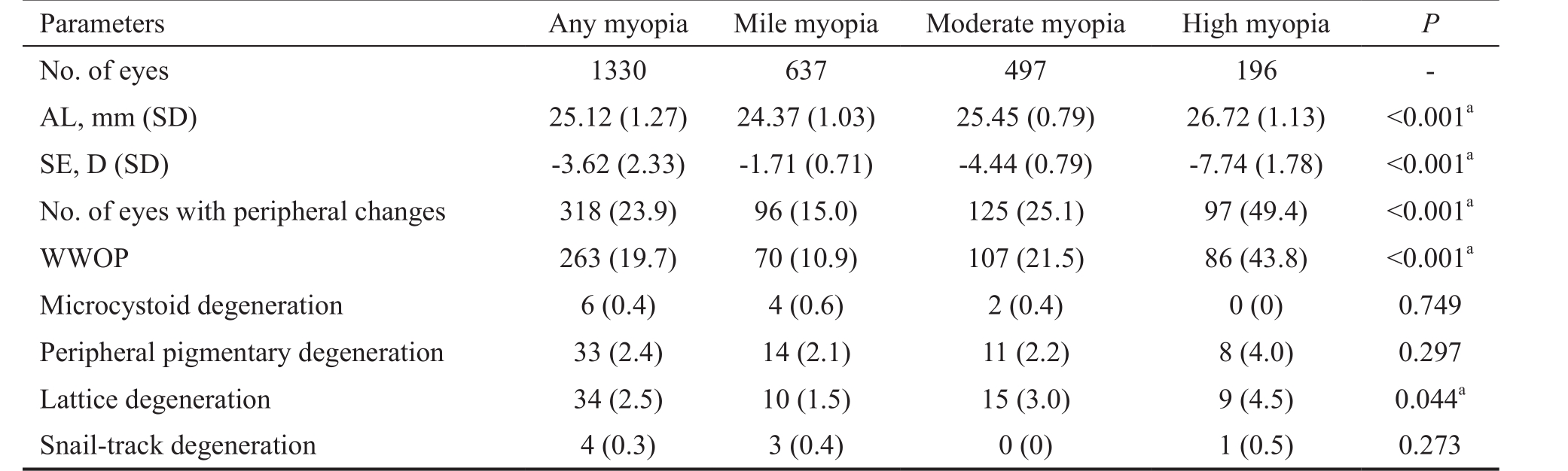
Table 3 Frequencies of peripheral myopia-related retinal changes in the myopia subjects n (%)
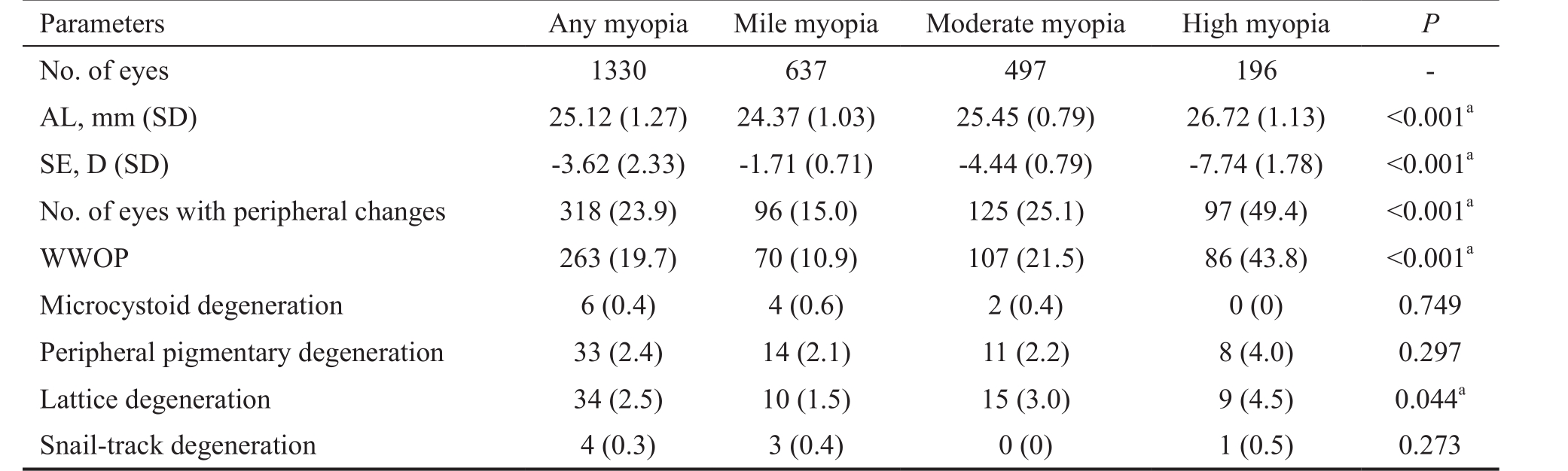
AL: Axial length; SE: Spherical equivalent; WWOP: White-without-pressure.aSignificance.
Parameters Any myopia Mile myopia Moderate myopia High myopia P No. of eyes 1330 637 497 196 -AL, mm (SD) 25.12 (1.27) 24.37 (1.03) 25.45 (0.79) 26.72 (1.13) ˂0.001aSE, D (SD) -3.62 (2.33) -1.71 (0.71) -4.44 (0.79) -7.74 (1.78) ˂0.001aNo. of eyes with peripheral changes 318 (23.9) 96 (15.0) 125 (25.1) 97 (49.4) ˂0.001aWWOP 263 (19.7) 70 (10.9) 107 (21.5) 86 (43.8) ˂0.001aMicrocystoid degeneration 6 (0.4) 4 (0.6) 2 (0.4) 0 (0) 0.749 Peripheral pigmentary degeneration 33 (2.4) 14 (2.1) 11 (2.2) 8 (4.0) 0.297 Lattice degeneration 34 (2.5) 10 (1.5) 15 (3.0) 9 (4.5) 0.044aSnail-track degeneration 4 (0.3) 3 (0.4) 0 (0) 1 (0.5) 0.273
Frequencies of Myopia-related Retinal Changes in the Myopia SubjectsWe further explored the myopia-related retinal changes in subjects with myopia by separating the myopia group into mild, moderate, and high myopia groups. Table 3 shows the comparison of the AL, SE and the frequencies of myopia-related retinal changes across these different degrees of myopia. Subjects with high myopia had the highest frequency of myopic retinal changes (49.4%,P˂0.001) [WWOP (43.8%, P˂0.001), lattice degeneration(4.5%, P=0.044)] among the three groups.
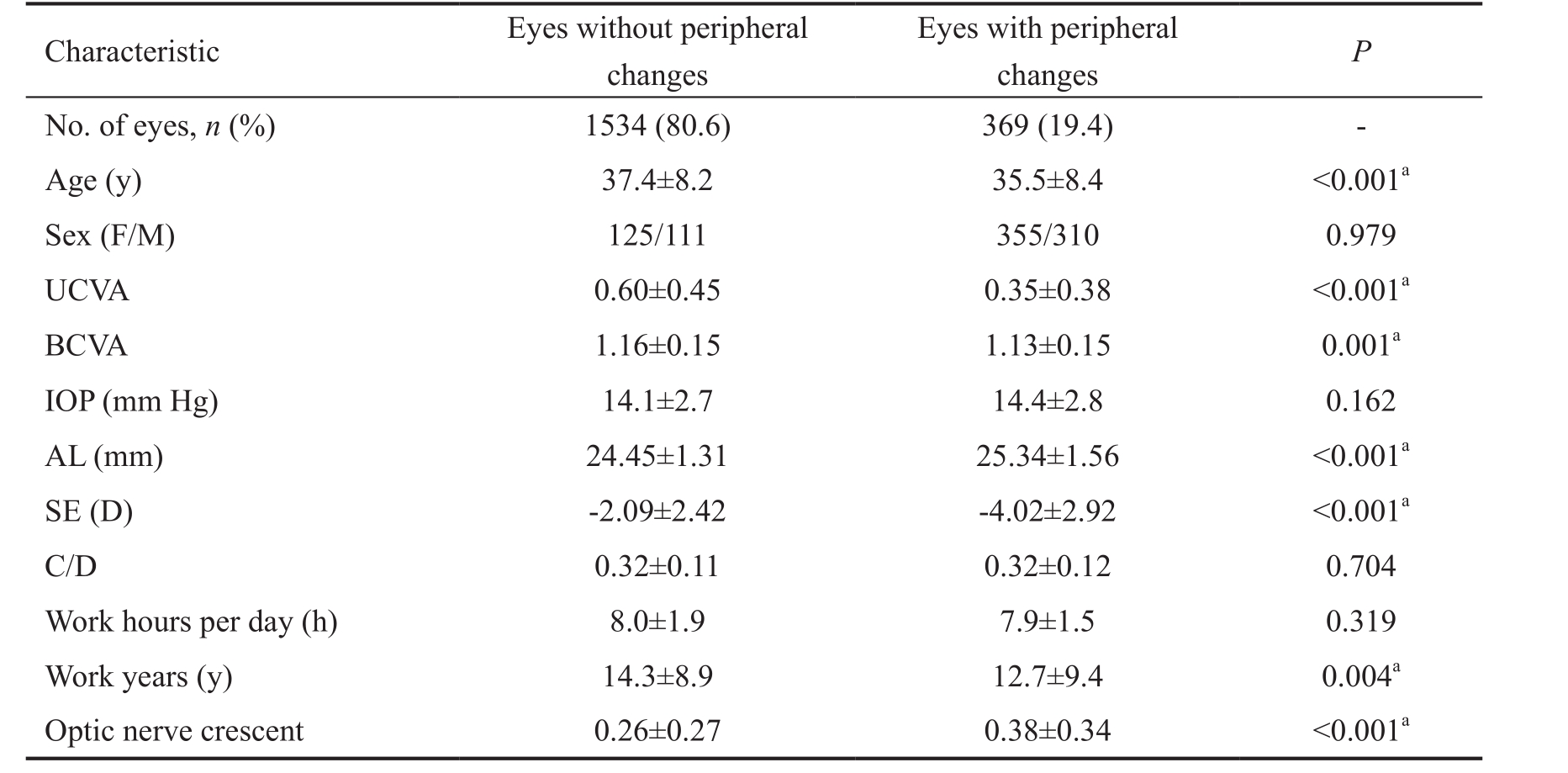
Mean Values of Parameters in Eyes with and Without Peripheral Retinal ChangesPeripheral retinal changes were found in 19.4% of the eyes. Eyes with peripheral retinal changes were younger and had significantly lower UCVA,longer AL, much higher SE, and a larger optic nerve crescent when compared to eyes without peripheral retinal changes (all P˂0.05). The differences in gender, BCVA,IOP, C/D, work hours per day, and work years between the two groups were not statistically significant are shown in Table 4.
Table 4 Mean values of parameters in eyes with and without peripheral retinal changes
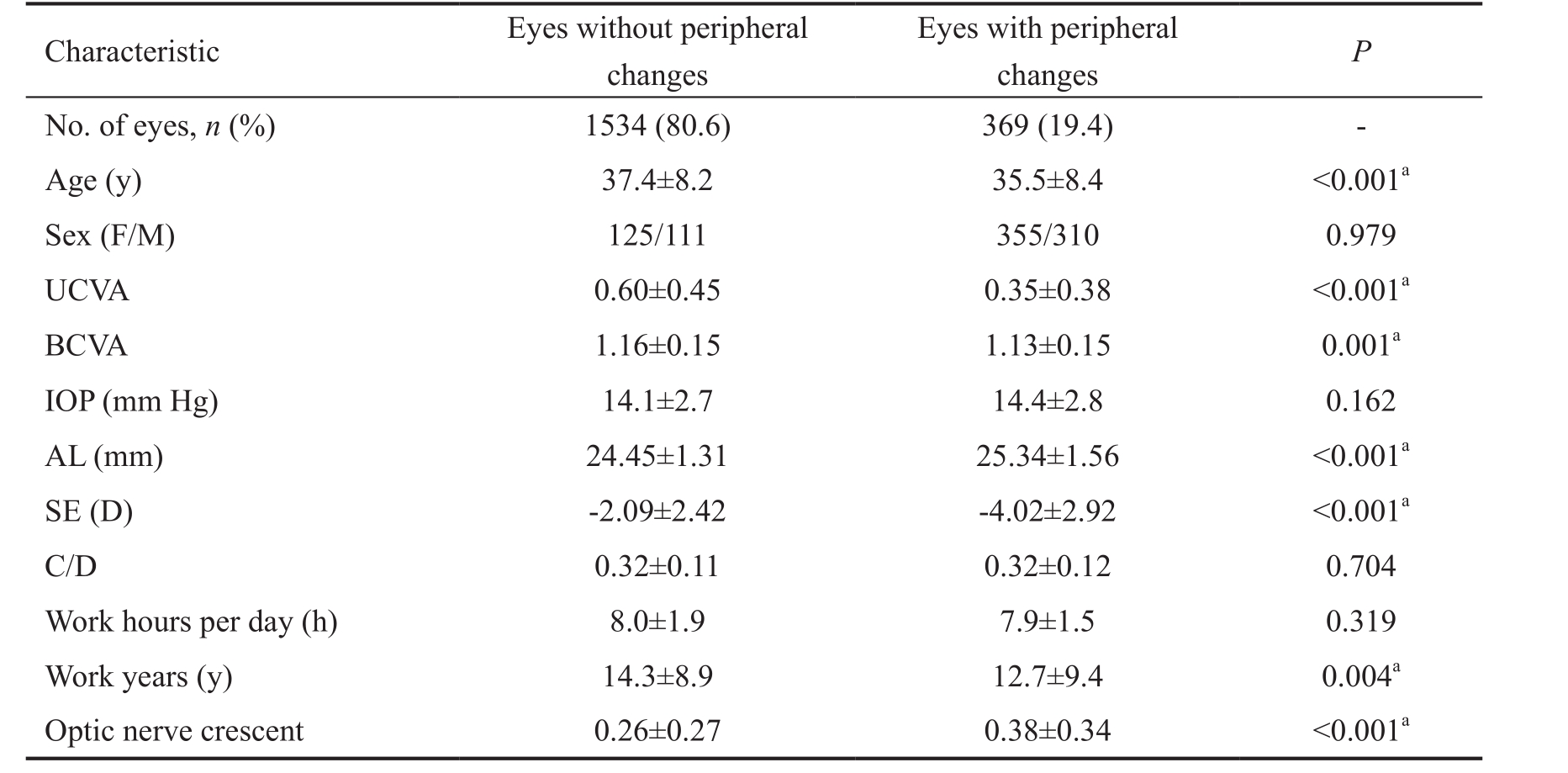
Data are expressed as the mean±SD. UCVA: Uncorrected visual acuity; BCVA: Best-corrected visual acuity; IOP:Intraocular pressure; AL: Axial length; SE: Spherical equivalent; D: Diopter; C/D: Cup/disc ratio.aSignificance.
Characteristic Eyes without peripheral changes Eyes with peripheral changes P No. of eyes, n (%) 1534 (80.6) 369 (19.4) -Age (y) 37.4±8.2 35.5±8.4 ˂0.001aSex (F/M) 125/111 355/310 0.979 UCVA 0.60±0.45 0.35±0.38 ˂0.001aBCVA 1.16±0.15 1.13±0.15 0.001aIOP (mm Hg) 14.1±2.7 14.4±2.8 0.162 AL (mm) 24.45±1.31 25.34±1.56 ˂0.001aSE (D) -2.09±2.42 -4.02±2.92 ˂0.001aC/D 0.32±0.11 0.32±0.12 0.704 Work hours per day (h) 8.0±1.9 7.9±1.5 0.319 Work years (y) 14.3±8.9 12.7±9.4 0.004aOptic nerve crescent 0.26±0.27 0.38±0.34 ˂0.001a
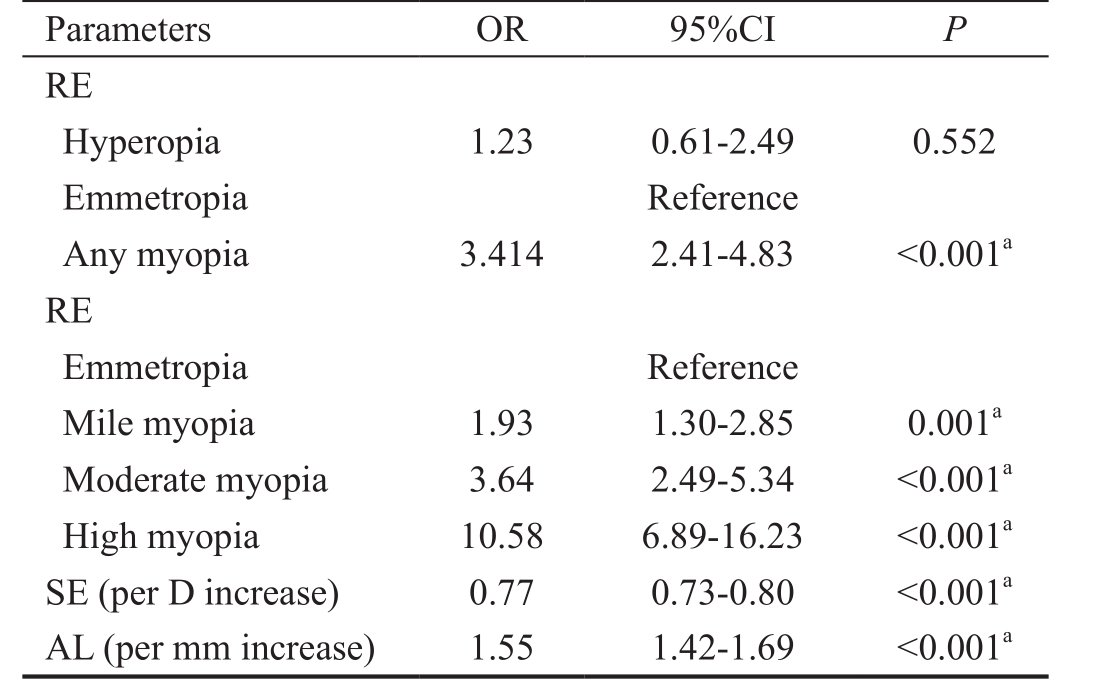
Associations of Refractive Error and Axial Length with Peripheral Retinal ChangesThe analysis of potential risk factors included the consideration of a possible relationship between different RE/AL ratios and peripheral retinal changes. Logistic regression was conducted to assess whether these factors significantly predicted the existence of any peripheral retinal changes. The odds ratios are summarized in Table 5. Any myopia (OR: 3.41, P˂0.001), mild myopia(OR: 1.93, P=0.001), moderate myopia (OR: 3.64, P˂0.001),and high myopia (OR: 10.58, P˂0.001), a greater AL (OR:1.55, P˂0.001), and a more serious SE (OR: 0.77, P˂0.001)increased the risk for peripheral retinal changes.
DISCUSSION
Myopic retinopathy was found in 19.4% of the eyes included in the study and was associated significantly with younger age,worse UCVA, greater AL, much higher SE, and a larger optic nerve crescent. Any myopia (OR: 3.41) [mild myopia (OR:1.93), moderate myopia (OR: 3.64), or high myopia(OR: 10.58)], a greater AL (OR: 1.55) and a much higher SE(OR: 0.77) increased the risk for peripheral retinal changes.
The prevalence of peripheral retinopathy in our study was considerably higher than the prevalence reported by Fuchs[16](0.3%-9.6%), Tokoro[11](2.16%), and Lai et al[17](11.3%).However, a possible reason is that this reflects the higher prevalence of myopia (69.6%) in our office workers (aged 21-59y), which was less than 2 fold higher than the rate seen in Singapore (38.7%; aged 40-79y)[18]and 2.5 fold higher than Poland (24.1%; aged 35y and older)[19]. As expected,the prevalence of peripheral myopic retinopathy in our study increased significantly (P˂0.001) with the level of myopia[5],from 15.0% in eyes with mild myopia to 25.1% and 49.4% in eyes with moderate and high myopia, respectively.
Table 5 Associations of RE and AL with peripheral retinal changes
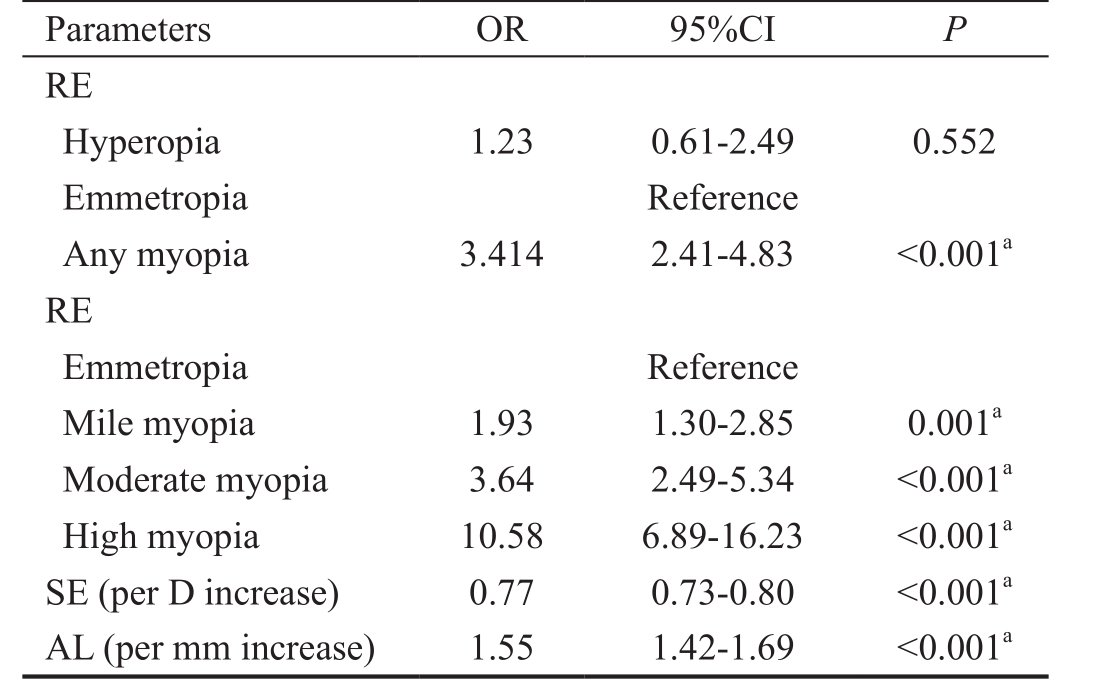
AL: Axial length; SE: Spherical equivalent; RE: Refractive error.aSignificance.
Parameters OR 95%CI P RE Hyperopia 1.23 0.61-2.49 0.552 Emmetropia Reference Any myopia 3.414 2.41-4.83 ˂0.001aRE Emmetropia Reference Mile myopia 1.93 1.30-2.85 0.001aModerate myopia 3.64 2.49-5.34 ˂0.001aHigh myopia 10.58 6.89-16.23 ˂0.001aSE (per D increase) 0.77 0.73-0.80 ˂0.001aAL (per mm increase) 1.55 1.42-1.69 ˂0.001a
We found that retinopathy was more common in the peripheral retina than in the posterior polar retina, and that the WWOP was the most common peripheral change, accounting for 19.7% of the changes. Interestingly, WWOP was more commonly seen in moderately myo pic eyes, in contrast to previous studies in Taiwan and Hong Kong studies that recruited highly myopic college students[17]. In our study,the eyes with moderate myopia had the highest incidence of peripheral retinal changes (39.3%) and WWOP (40.7%), which was similar with the findings of the study from Poland[19],which demonstrated a decrease in the prevalence of myopia and, simultaneously, an increase in the prevalence of hyperopia with increasing age[20-23]. Our findings were also similar to those of a previous studies[5,24], which reported that eyes with myopic retinal changes and WWOP were markedly younger than the remaining subjects without these changes. However,the possibility that WWOP is becoming more prevalent in younger high myopes is not confirmed and will require additional longitudinal studies.
UCVA was markedly worse in the group with myopic retinopathy than in the remaining subjects (Table 4). The main reasons for this may be myopia-associated changes in the macula and the myopic RE-associated reduction in the size of the image on the retina. No gender difference was detected in the prevalence of myopic retinopathy in the present study, in agreement with the Beijing Eye Study[6], whereas Lai et al[17]reported a higher prevalence of myopic retinopathy in women.Our results also demonstrated strong associations between AL and SE and various retinal lesions. Overall, 19.4% of the eyes with an AL of 25.34±1.56 mm, an SE of -4.02±2.92 D,and an optic nerve crescent of 0.38±0.34 had retinal lesions,whereas 80.6% of the eyes with an AL of 24.45 mm, SE of-2.09±2.42 D, and optic nerve crescent of 0.26±0.27 had no retinal lesions. This was consistent with previous studies by Jonas et al[25]and Pierro et al[26], who showed that eyes with posterior pole retinal changes, WWOP, paving stone degeneration, and lattice degeneration had significantly greater AL. After adjusted analysis for AL, our results also demonstrated that a higher magnitude of SE has an independent association with the presence of retinal lesions.Multivariate regression analysis identified moderate and high myopia as important risk factors for retinal lesions,suggesting that close follow-up of patients with moderate or higher myopia and with retinal changes might be warranted.Some studies have reported no significant association between myopic retinopathy and the level of education or rural versus urban regions of residence[27]. Nevertheless, our study provides the first evidence that myopia is becoming more common among urban Chinese office workers, with a clear trend toward a higher prevalence of myopia in participants with a more recent birth year. Possible environmental reasons include an apparent increase in formal education and more time spent on near work tasks by East Asians[28-29]. The subjects in our study had a higher level of education, as approximately 95%of them had a bachelor’s degree or above. Near work, such as reading and writing, may be a further factor associated with a higher prevalence of myopic retinopathy[30]. The subjects were also urban, and the Beijing Eye Study reported that the urban population was significantly more myopic than the rural population[3], suggesting that urbanization may be associated with increased myopia.
Limitations of the present study included the differences in study design and population sampling and the possible presence of selection bias. We cannot directly compare our data with other population-based studies. Patients enrolled in our study were solely from the Guangzhou Power Supply Bureau; thus, the prevalence of ocular disorders might be higher in our cohort than in the general population.
In conclusion, in our study population of Guangzhou Power Supply workers, myopia-related retinal changes were positively associated with younger age, greater AL, much higher SE,and moderate or high myopia. To the best of our knowledge,the distribution and characteristics of myopia-related retinal changes among office workers in Eastern Asia have not been previously reported. However, further investigations are needed on larger and randomly selected populations.
ACKNOWLEDGEMENTS
Foundations:Supported by the National Natural Science Foundation of China (No.81570865); the Guangdong Science and Technology Plan (No.2014A020212586); the Guangdong Natural Science Fund (No.2016A030310196;No.2017A030313543).
Conflicts of Interest:Zhang T, None; Wei YT, None; Huang WB, None; Liu RJ, None; Zuo YJ, None; He LW, None;Zhong LT, None; Zhang SC, None.
REFERENCES
1 Morgan IG, Ohno-Matsui K, Saw SM. Myopia. Lancet 2012;379(9827):1739-1748.
2 Jonas JB, Xu L, Wang YX, Bi HS, Wu JF, Jiang WJ, Nangia V, Sinha A,Zhu D, Tao Y, Guo Y, You QS, Wu LJ, Tao LX, Guo XH, Ohno-Matsui K, Panda-Jonas S. Education-related parameters in high myopia: adults versus school children. PLoS One 2016;11(5):e0154554.
3 You QS, Wu LJ, Duan JL, Luo YX, Liu L J, Li X, Gao Q, Wang W, Xu L, Jonas JB, Guo XH. Prevalence of myopia in school children in greater Beijing: the Beijing Childhood Eye Study. Acta Ophthalmol 2013;92(5):e398-e406.
4 Tarczy-Hornoch K, Ying-Lai M, Varma R; Los Angeles Latino Eye Study Group. Myopic refractive error in adult Latinos: the Los Angeles Latino Eye Study. Invest Ophthalmol Vis Sci 2006;47(5):1845-1852.
5 Gozum N, Cakir M, Gucukoglu A, Sezen F. Relationship between retinal lesions and axial length, age and sex in high myopia. Eur J Ophthalmol 1997;7(3):277-282.
6 Xu L, Wang Y, Li Y, Wang Y, Cui T, Li J, Jonas JB. Causes of blindness and visual impairment in urban and rural areas in Beijing: the Beijing Eye Study. Ophthalmology 2006;113(7):1134.e1-11.
7 Hsu WM, Cheng CY, Liu JH, Tsai SY, Chou P. Prevalence and causes of visual impairment in an elderly Chinese population in Taiwan: the Shihpai Eye Study. Ophthalmology 2004;111(1):62-69.
8 Liang YB, Friedman DS, Wong TY, Zhan SY, Sun LP, Wang JJ, Duan XR, Yang XH, Wang FH, Zhou Q, Wang NL. Prevalence and causes of low vision and blindness in a rural Chinese adult population: the Handan Eye Study. Ophthalmology 2008;115(11):1965-1972.
9 Iwase A, Araie M, Tomidokoro A, Yamamoto T, Shimizu H, Kitazawa Y; Tajimi Study Group. Prevalence and causes of low vision and blindness in a Japanese adult population: the Tajimi Study. Ophthalmology 2006;113(8):1354-1362.
10 Buch H, Vinding T, La Cour M, Appleyard M, Jensen GB, Nielsen NV.Prevalence and causes of visual impairment and blindness among 9980 Scandinavian adults: the Copenhagen City Eye Study. Ophthalmology 2004;111(1):53-61.
11 Tokoro T. On the definition of pathologic myopia in group studies.Acta Ophthalmol Suppl 1988;185:107-108.
12 Hu DN. Prevalence and mode of inheritance of major genetic eye diseases in China. J Med Genet 1987;24(10):584-588.
13 Saw SM, Chua WH, Hong CY, Wu HM, Chan WY, Chia KS, Stone RA, Tan D. Nearwork in early-onset myopia. Invest Ophthalmol Vis Sci 2002;43(2):332-339.
14 Cheng SC, Lam CS, Yap MK. Prevalence of myopia-related retinal changes among 12-18 year old Hong Kong Chinese high myopes.Ophthalmic Physiol Opt 2013;33(6):652-660.
15 Zhang T, Zuo Y, Wei Y, Huang W, Zhou X, Liu R, Zhong L, Peng M, Zhang S. The prevalence and associations of peripheral retinopathy:baseline study of guangzhou office computer workers. J Ophthalmol 2018:e2358690.
16 Fuchs A. Frequency of myopia gravis. Am J Ophthalmol 1960;49:1418-1419.
17 Lai TY, Fan DS, Lai WW, Lam DS. Peripheral and posterior pole retinal lesions in association with high myopia: a cross-sectional community-based study in Hong Kong. Eye (Lond) 2008;22(2):209-213.
18 Wong TY, Foster PJ, Hee J, Ng TP, Tielsch JM, Chew SJ, Johnson GJ,Seah SK. Prevalence and risk factors for refractive errors in adult Chinese in Singapore. Invest Ophthalmol Vis Sci 2000;41(9):2486-2494.
19 Nowak MS, Jurowski P, Grzybowski A, Smigielski J. Characteristics of refractive errors in a population of adults in the central region of Poland. Int J Environ Res Public Health 2018;5(1).pii:E90.
20 Rodriguez NM, Romero AF. The prevalence of refractive conditions in Puerto Rican adults attending an eye clinic system. J Optom 2014;7(3):161-167.
21 Hashemi H, Khabazkhoob M, Iribarren R, Emamian MH, Fotouhi A. Five-year change in refraction and its ocular components in the 40-to 64-year-old population of the Shahroud eye cohort study. Clin Exp Ophthalmol 2016;44(8):669-677.
22 Anton A, Andrada MT, Mayo A, Portela J, Merayo J. Epidemiology of refractive errors in an adult European population: the Segovia study.Ophthalmic Epidemiol 2009;16(4):231-237.
23 Katz J, Tielsch JM, Sommer A. Prevalence and risk factors for refractive errors in an adult inner city population. Invest Ophthalmol Vis Sci 1997;38(2):334-340.
24 Shukla M, Ahuja OP. White with pressure (WWP) and white without pressure (WWOP) lesions. Indian J Ophthalmol 1982;30(3):129-132.
25 Jonas JB, Nangia V, Gupta R, Bhojwani K, Nangia P, Panda-Jonas S.Prevalence of myopic retinopathy in rural Central India. Acta Ophthalmol 2017;95(5):e399-e404.
26 Pierro L, Camesasca FI, Mischi M, Brancato R. Peripheral retinal changes and axial myopia. Retina 1992;12(1):12-17.
27 Ohno-Matsui K, Kawasaki R, Jonas JB, Cheung CM, Saw SM,Verhoeven VJ, Klaver CC, Moriyama M, Shinohara K, Kawasaki Y,Yamazaki M, Meuer S, Ishibashi T, Yasuda M, Yamashita H, Sugano A,Wang JJ, Mitchell P, Wong TY; META-analysis for Pathologic Myopia(META-PM) Study Group. International photographic classification and grading system for myopic maculopathy. Am J Ophthalmol 2015;159(5):877-883.
28 Saw SM, Katz J, Schein OD, Chew SJ, Chan TK. Epidemiology of myopia. Epidemiol Rev 1996;18(2):175-187.
29 Xu C, Pan C, Zhao C, Bi M, Ma Q, Cheng J, Song E. Prevalence and risk factors for myopia in older adult east Chinese population. BMC Ophthalmol 2017;17(1):191-202.
30 Li SM, Liu LR, Li SY, Ji YZ, Fu J, Wang Y, Li H, Zhu BD, Yang Z, Li L, Chen W, Kang MT, Zhang FJ, Zhan SY, Wang NL, Mitchell P; Anyang Childhood Eye Study Group. Design, methodology and baseline data of a school-based cohort study in Central China: the Anyang Childhood Eye Study. Ophthalmic Epidemio 2013;20(6):348-359.
Co-first authors:Ting Zhang and Yan-Tao Wei
Correspondenceto:Shao-Chong Zhang. State Key Laboratory of Ophthalmology, Zhongshan Ophthalmic Center, Sun Yat-Sen University, Guangzhou 510060, Guangdong Province,China. Zhshaochong@163.com
Received:2018-04-14 Accepted: 2018-06-27
Abstract● AlM: To determine the prevalence and characteristics of peripheral myopic retinopathy among a sample of Guangzhou office workers.● METHODS: A cross-sectional study of Guangzhou Chinese office works in different departments and units of the Guangzhou Power Supply Bureau, China, in 2016. Myopic retinopathy was recorded and analyzed with a scanning laser ophthalmoscope and by slit-lamp microscopy combined with a three-mirror contact lens.● RESULTS: ln total, 1910 eyes of 955 subjects (508 females and 447 males) aged 21-59y were included; 69.6% of these eyes were myopic. The myopia group had a younger age and worse uncorrected visual acuity (UCVA) and bestcorrected visual acuity (BCVA) when compared with hyperopia and emmetropia groups (P<0.001). The axial length (AL) was significantly longer, the spherical equivalent(SE) was more serious, and the optic nerve crescent was significantly larger in subjects with myopia than with hyperopia and emmetropia. Subjects with myopia, and especially high myopia, had the highest frequency of myopic retinal 18 changes (49.4%, P<0.001) [white-without-pressure(43.8%, P<0.001), lattice degeneration (4.5%, P=0.044)] among the three groups. Logistic regression confirmed that any myopia (OR: 3.41, P<0.001) [mild myopia (OR: 1.93, P=0.001),moderate myopia (OR:3.64, P<0.001), and high myopia(OR:10.58, P<0.001)], a greater AL (OR: 1.55, P<0.001) and a much higher SE (OR: 0.77, P<0.001) increased the risk for peripheral retinal changes.● CONCLUSlON: Myopia-related retinal changes are positively associated with greater AL, higher SE, and myopia.
● KEYWORDS:peripheral myopic retinopathy; prevalence;characteristics; office workers
DOl:10.18240/ijo.2018.08.22
Citation:Zhang T, Wei YT, Huang WB, Liu RJ, Zuo YJ, He LW,Zhong LT, Zhang SC. Prevalence and characteristics of peripheral myopic retinopathy in Guangzhou office workers. Int J Ophthalmol 2018;11(8):1390-1395