lntraocular lens optic capture in pediatric cataract surgery
Ying-Bin Xie, Mei-Yu Ren, Qi Wang, Li-Hua Wang
Department of Ophthalmology, Shandong Provincial Hospital Affiliated to Shandong University, Jinan 250021, Shandong Province, China
INTRODUCTION
O ver the past decade, the treatment of children’s cataracts has undergone rapid development[1-5]. However, due to the specific biological characteristics of children’s eyeballs,posterior capsule opacification (PCO) is still a serious complication of pediatric cataract surgery, and it seriously threatens the recovery of visual function after surgery. Current efforts to prevent PCO include primary posterior capsulotomy(PPC) with or without anterior vitrectomy[6-7], intraocular lens(IOL) optic capture[8-16], use of perfusate containing heparin and heparin-surface-modified (HSM) IOLs[15,17]. Chemical prevention of PCO by irrigation with antimetabolite has also been tested in animal models[18]. Despite these efforts, there is still no clear optimal treatment option for effective prevention and reduction of the occurrence of PCO.
In 1994, Gimbel and DeBroff[11]was the first to publish the IOL optic capture technique and use it to prevent PCO in pediatric patients with congenital cataracts. This technique has been featured in reports by many other researchers, but there is currently no professional consensus on the exact preventive effect of PCO, especially on the need for anterior vitrectomy at the same time. In 2017, Vasavada et al[19]reported 26 eyes with pediatric congenital cataracts that were subjected to IOL optic capture operation without anterior vitrectomy. After 12mo of follow-up, eyes were examined for visual transparency, which confirmed the clinical effect of the operation to prevent visual axis obscuration (VAO). Recently, Zhou et al[20]published a Meta-analysis of 282 eyes with pediatric cataracts that were subjected to IOL optic capture and showed that the technique can significantly reduce the VAO rate and eccentricity of IOL.In this report, we reviewed literatures related with optic capture technique since its first report by Gimbel and DeBroff[11]. We here discuss the topics including applications of optic capture in pediatric cataract management, complications after optic capture IOL, typical types and features of IOLs which have been used for optic capture technique.
HISTORY OF INTRAOCULAR LENS OPTIC CAPTURE
In 1991, Neuhann and Neuhann described a technique involving placing the IOL in the sulcus and then placing the optic of the IOL through the opening in the anterior capsulorhexis to achieve capture and stable fixation when the posterior capsule tears during adult cataract surgery[7]. In 1994,Gimbel and DeBroff[11]modified the technique and used it to prevent PCO in pediatric cataract surgery. This technique involves implantation of polymethylmethacrylate (PMMA)IOL in the capsular bag following anterior curvilinear capsulorhexis (ACCC) and posterior curvilinear capsulorhexis(PCCC), capturing the IOL optic through the PCCC opening,and placing of the anterior and posterior capsule leaflets in apposition. This maneuver seals the residual cortex within the bag and eliminates the need for an anterior vitrectomy.Since the initial report, this technique has been used for the prevention of PCO in pediatric cataract treatment (Table 1).
INTRAOCULAR LENS USED FOR OPTIC CAPTURE TECHNIQUE
IOLs, which have been used for optic capture in pediatric cataract, mainly include single-piece PMMA IOLs[9-10,17,21-23,25]and three-piece acrylic IOLs[12-14,16,19,24](Table 2).
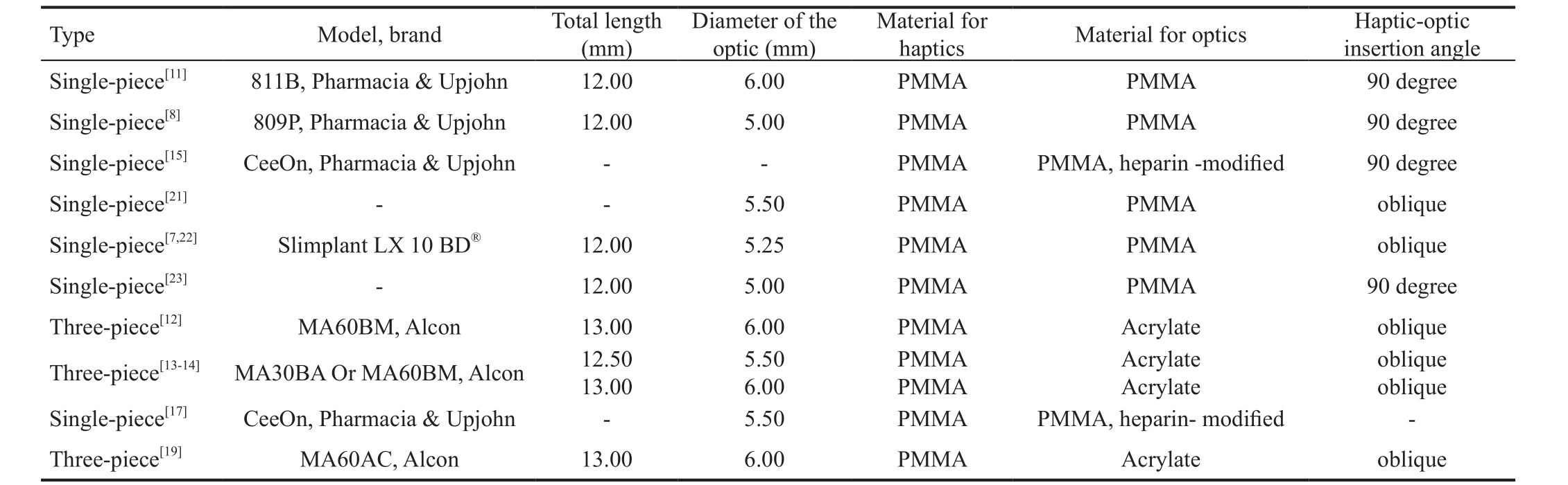
Table 1 Summary of peer-reviewed articles on the topic of intraocular lens capture with pediatric cataracts n (%)

BP: Behind the posterior curvilinear capsulorhexis; CS: Ciliary sulcus; PCO: Posterior capsule opacification; -: No available data.
Author, year capturing Incision Anterior vitrectomy Eyes of Mean age at surgery(y)Haptic placement placement PCO Pigment deposits Synechias Follow-up(mo)Optic Gimbel and DeBroff, 1994[11]2.5 1 Sclera No Bag BP 0 (0) 0 (0) 0 (0) 5 Gimbel, 1996[9]5.8 13 Sclera No Bag BP 0 (0) - - 19 Gimbel, 1997[15]2.5-12 16 Sclera No Bag BP 0 (0) - - 35.5 Koch and Kohnen, 1997[21]6.1 5 Sclera No Bag BP 4 (80) 0 (0) - 24 Koch and Kohnen, 1997[21]6.1 3 Sclera Yes Bag BP 0 (0) 0 (0) - 24 Vasavada and Desai, 1997[7]2.1 3 Sclera No Bag or CS BP - - - 13.3 Vasavada and Desai, 1997[7]2.5 5 Sclera Yes Bag or CS BP - - - 13.3 Vasavada and Trivedi, 2000[22]2.2 10 Sclera Yes Bag BP 0 (0) 10 (100) 6 (60) 15 Vasavada and Trivedi, 2000[22]2.2 4 Sclera Yes CS BP 0 (0) 4 (100) 4 (100) 15 Dada et al, 2000[17]4.2 14 Limbus No Bag BP 0 (0) - - 36 Vasavada et al, 2001[10]7 21 Sclera Yes Bag BP 0 (0) 4 (19) 3 (15) 21 Vasavada et al, 2001[10]7 20 Sclera No Bag BP 14 (70) 6 (30) 8 (40) 21 Argento et al, 2001[14]3.4 8 Sclera No Bag BP 0 (0) - - 28.9 Raina et al, 2002[8]6.4 16 Limbus No Bag BP 0 (0) 0 (0) 2 (13) 17.5 Müllner-Eidenböck et al, 2003[16]3.6 8 Cornea Yes Bag BP 0 (0) 0 (0) 2 (25) 20.7 Müllner-Eidenböck et al, 2003[16]11.4 7 Cornea No Bag BP 0 (0) 0 (0) 0 (0) 20.7 Raina et al, 2004[13]6.5 6 Sclera No Bag BP 0 (0) 1 (16) 0 (0) 13 Grieshaber et al, 2005[23]3 68 Limbus No Bag BP 0 (0) 0 (0) 6 (9) 109 Sharma et al, 2006[24]8.3 17 Cornea 2/17 Bag BP - - - -Sharma et al, 2006[24]7.9 11 Cornea 2/11 Bag BP - - - -Grieshaber et al, 2009[25]4.1 47 Cornea No Bag BP 0 (0) - 5 (11) 48 Faramarzi and Javadi, 2009[12]5.1 14 Cornea Yes CS BP 0 (0) 3 (21) 0 (0) 22.2 Vasavada et al, 2017[19]1.5 26 Limbus No Bag BP 0 (0) 4 (15) 2 (8) 12 Cicik et al, 2018[26]7 26 - No Bag BP 0 (0) - 0 (0) 30
Table 2 Comparison of commonly used IOLs suitable for optic capture techniques
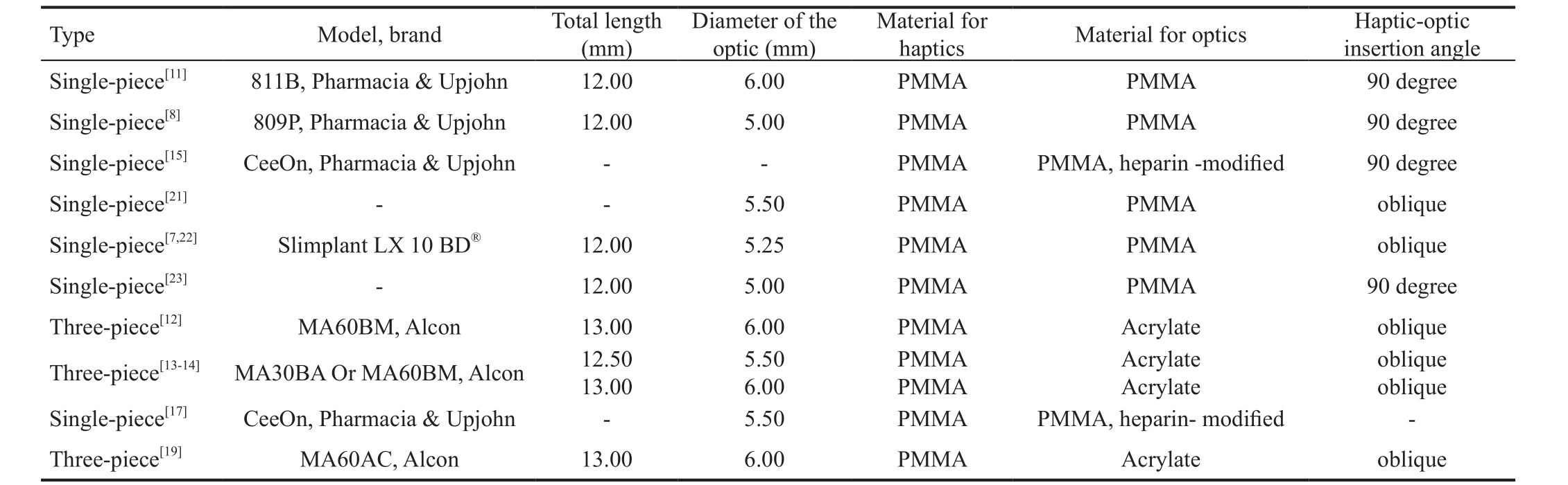
-: No available data; PMMA: Polymethylmethacrylate.
oblique oblique Single-piece[17]CeeOn, Pharmacia & Upjohn - 5.50 PMMA PMMA, heparin- modified -Three-piece[19]MA60AC, Alcon 13.00 6.00 PMMA Acrylate oblique haptics Material for optics Haptic-optic insertion angle Single-piece[11]811B, Pharmacia & Upjohn 12.00 6.00 PMMA PMMA 90 degree Single-piece[8]809P, Pharmacia & Upjohn 12.00 5.00 PMMA PMMA 90 degree Single-piece[15]CeeOn, Pharmacia & Upjohn - - PMMA PMMA, heparin -modified 90 degree Single-piece[21]- - 5.50 PMMA PMMA oblique Single-piece[7,22]Slimplant LX 10 BD®12.00 5.25 PMMA PMMA oblique Single-piece[23]- 12.00 5.00 PMMA PMMA 90 degree Three-piece[12]MA60BM, Alcon 13.00 6.00 PMMA Acrylate oblique Three-piece[13-14]MA30BA Or MA60BM, Alcon 12.50 13.00 Type Model, brand Total length(mm)Diameter of the optic (mm)Material for 5.50 6.00 PMMA PMMA Acrylate Acrylate
Polymethylmethacrylate Intraocular LensPMMA, also known by the trade name Plexiglas, is the first material used for IOL manufacture. It has the best optical quality among synthetic transparent materials. Before 2001, most of the IOLs used in optic capture have been made of PMMA. PMMA material has excellent biocompatibility, low tissue reactivity,a high refractive index, and excellent optical properties.However, PMMA material cannot endure high temperatures or pressures, and it is relatively rigid and unfoldable. As a result,PMMA IOL has been used less and less in pediatric cataract surgery[27].
Heparin-surface-modified Polymethylmethacrylate Intraocular LensHeparin-surface-modified (HSM) PMMA IOL has been reported to reduce the incidence of VAO and iris inflammation after cataract surgery[15,28]. Heparin is a naturally occurring anticoagulant produced in animals. It inhibits the formation of fibrin, outgrowth of fibroblasts, and polymerization of type I collagen. Pediatric eyes usually have stronger postoperative fibrinous reactions due to the immaturity of the blood-aqueous barrier and insufficient fibrinolytic activity[29-30]. HSM IOL has been used to reduce anterior chamber reaction. Basti et al[28]evaluated the performance of HSM IOLs in 90 pediatric eyes after cataract surgery. Cellular deposits on the IOL surface and postoperative inflammation were significantly less pronounced in HSM IOL implantation patients. Gimbel[15]reported PCCC with optic capture of the heparin-coated IOLs in 16 eyes. No VAO occurred at 35.5mo follow-up.
Acrylic Intraocular LensAcrylic IOL is less irriating to intraocular tissue than other substances, causes less inflammation than PMMA IOL[31]and offers excellent biocompatibility[16].Another advantage of acrylic IOL is foldable design, which makes implantation possible with an incision under 3 mm in length, rather than the traditional 5.5 mm incision required for PMMA IOL. Primary implantation of foldable acrylic IOLs in paediatric eyes may allow fewer rate of perioperative complications[32-33]. Moreover, hydrophobic acrylic IOL have a strong tendency to adhere to the lens capsule, which contributes to posterior and anterior capsule clarity and prevent lens decentration[34]. Acrylic IOL have been reported as having very low rates of PCO[31,35-37]. So far, almost all acrylic IOLs used for pediatric cataract IOL capture are three-piece design. Vasavada et al[19]concluded that this design of threepiece, in particular its optic-haptic junction, allowing almost 360 degrees of capsular fusion and might be better suited for optic capture. Faramarzi and Javadi[12]emphasized that for the approach of implantation of IOL haptics in the ciliary sulcus and optic capture through the capsule opening, only the threepiece IOL with PMMA haptics is applicable and one-piece AcrySof IOL is not indicated for sulcus fixation. Solebo et al[38]conducted national postal questionnaire surveys of consultant ophthalmologists in the UK and Ireland. All surgeons (100%)who performed primary IOL implantation used hydrophobic acrylic lenses in children ˂ or =2y, with 90% using an AcrySof model.
INTRAOCULAR LENS OPTIC-HAPTIC INSERTION ANGLE DESIGN
The design of the insertion angle between the haptic and optic is believed to affect the ability of optic capture to prevent postoperative PCO. For the Gimbel’ capturing mode[11], the site at which the haptics enter the capsular bag creates an area in which the posterior capsule is posterior to the optic, in which residual cortex may find their way into the posterior chamber and cause PCO. Some scholars believe that this gap at the optic-haptic junction may be reduce by the right-angle design of optic-haptic junction. Gimbel and DeBroff[11]and Raina et al[8]postulated that using an IOL with a distinct right-angle departure of the haptic from the optic may help in achieving a tighter seal than a traditional lens design. In their study, all eyes had a clear central visual axis during the follow-up period even in the absence of vitrectomy. In contrast, Vasavada and Desai[7]observed opacification of the anterior vitreous face in all 3 eyes that had optic capture without an anterior vitrectomy and a secondary pars plana anterior vitrectomy was required,in which the haptic-optic angulation of PMMA IOL of in their study is oblique. Koch and Kouhnen[21]also used a PMMA IOL that had an oblique haptic-optic junction. In their study, 4 of the 5 eyes that had optic capture without vitrectomy developed secondary cataracts.
LOCATION OF INTRAOCULAR LENS
Haptics in the Bag with the Optic Capture Through Posterior Curvilinear CapsulorhexisThis technique involves IOL implantation in the capsular bag following ACCC and PCCC,capturing the IOL optic through the PCCC opening. Gimbel and DeBroff[11]first reported this technique in children’s cataracts in 1994. After closure of posterior and anterior capsules, the migration of remnant cortex out of capsule is inhibited, which in turn inhibits PCO formation and eliminates the need for anterior vitrectomy. The IOL optics, together with continuous curvilinear capsulorhexis between posterior and anterior capsules, creates a stable barrier. After optic capture, both posterior and anterior capsules are located in the anterior surface of IOL. In this case, small amounts of migrating cortex were unable to reach the posterior of IOL to form PCO. Five months postoperatively, the anterior vitreous face was clear and no precipitates had formed on the anterior or posterior IOL surface. In 1996, Gimbel[9]conducted a study in 13 pediatric eyes using posterior capsulorhexis with optic capture technique, and no VAO occurred. In 1997, Gimbel[15]conducted PCCC with optic capture of the Heparin-coated IOLs in 16 pediatric eyes, the visual axis remained clear in all eyes.
Posterior Vertical Capsulotomy with Optic EntrapmentGrieshaber et al[23]reported a modified surgical technique,namely posterior vertical capsulotomy with optic entrapment,in 68 pediatric cataract eyes. In this technique, the anterior and posterior capsules were opened by capsulotomy with a diamond knife and straight Sutherland microscissors in a vertical direction with length comparable to that of IOL. A one-piece PMMA IOL was implanted in the bag and the optic was then entrapped centrally behind the bag. According to Grieshaber, this technique maximizes the contact area between anterior and posterior leaflets and offers an almost congruent fusion area. All 68 eyes maintained a clear visual axis for 5 to 12y postoperatively. In all eyes, the IOL remained well centered and entrapped. However, there is some disadvantage of this technique. Although vertical capsulotomy maximized contact of both leaflets and increase the barrier effect, there may be more encroachment on the visual axis than in the PCCC method developed by Gimbel, which may affect vision under dim illumination when the pupil is wider.
Haptics in the Ciliary Sulcus with the Optic Capture through Posterior Curvilinear CapsulorhexisAnother approach to preventing PCO is to implant the haptics of IOL in the ciliary sulcus, after which the optic is captured through the posterior capsulorhexis[12]. This technique is easier to perform than the optic capture technique developed by Gimbel and DeBroff[11].In addition, optic capture of the IOL through the PCCC provides complete fusion of the anterior and posterior capsule leaflets, which is beneficial to reduce PCO. Vasavada et al[10]suggested that this technique could also be applied to cases of incomplete anterior capsulorhexis because it could decrease the total area of optic contact with the iris, reducing the uveal inflammatory response. In 2009, Faramarzi and Javadi[12]applied this technique in 14 pediatric cataract surgeries and followed up the patients for 22.2mo. No PCO was noted in this series.
APPLICATION OF CAPSULAR DYES IN CAPTURE TECHNIQUE IN PEDIATRIC CATARACT
Capsular dyes have been successfully used to stain the anterior capsule in adult patients with an absence of a red fundus reflex[39], as well as to enhance visualization in cases of cataracts with corneal haze/opacification[40]. The pediatric capsule is thin, transparent, and elastic. As a result, capsule staining has been used to visualize anterior and posterior capsule flaps during pediatric cataract surgery and to facilitate capsule plaque removal[41-42]. In 2006, Sharma et al[24]evaluated the efficacy of trypan blue in posterior capsulorhexis with optic capture in pediatric cataracts. Optic capture was possible in 17 out of 18 eyes (94.4%) in the group that received trypan blue dye assisted procedures but in only 11 out of 17 (64.7%)in the group not given trypan blue assistant. Sharma et al[24]concluded that trypan blue facilitates visualization of posterior capsulorhexis and consequently increases the success rate of optic capture of IOL. Cicik et al[26]carried out a study of 52 eyes pediatric cataract with or without IOL optic capture and suggested that the anterior capsule was stained with trypan blue for better visibility when necessary.
DECISION TO UNDERGO SIMULTANEOUS ANTERIOR VITRECTOMY IN PEDIATRIC CATARACT CAPTURE SURGERY
Whether or not to perform anterior vitrectomy during cataract surgery in pediatric patients has been a controversial topic,and it has drawn attention from many scholars. So far, there is debate regarding whether to conduct anterior vitrectomy alongside IOL optic capture or not. Gimbel[9,15]conducted posterior capsulorhexis with optic capture without anterior vitrectomy using PMMA IOL in 13 eyes in 1996 and heparincoated IOL in 16 eyes in 1997, respectively. There was no PCO after surgery. Dada et al[17]suggested that lens aspiration using intracameral heparin, combined with primary posterior capsulorhexis and optic capture of a heparin-coated IOL, is a useful means of preventing secondary VAO in pediatric cataracts. Raina et al[8]supported the conclusion that IOL optic capture without anterior vitrectomy can effectively prevent PCO.
Koch and Kohnen[21]reported that PCCC with anterior vitrectomy was the only effective method of preventing or delaying secondary cataract formation in infants and children.Vasavada and Desai[7]suggested that anterior vitrectomy is desirable along with primary PCCC in children younger than 5y with congenital cataracts. In another study, Vasavada et al[10]concluded that anterior vitrectomy is necessary with optic capture in children with congenital cataract who are between 5 and 12 years old. However, Vasavada et al[19]recently published a report covering 26 eyes with pediatric cataracts that were subjected to IOL capture implantation without anterior vitrectomy. After 12mo of follow-up, all visual axis areas were found to have maintained their transparency,and no difference was found in the incidence or severity of synechiae or cell deposits between the capture group and capsule group.
COMPLICATION OF INTRAOCULAR LENS OPTIC CAPTURE
Posterior Capsule OpacificationPCO is the most common complication of pediatric cataract surgery[43-44]. The incidence of PCO approaches 100% if the posterior capsule is left intact during pediatric cataract surgery. Various options have been used to manage the PCO in pediatric cataracts, although the ideal procedure is still debated. However, it is well acknowledged that different surgical techniques affect the incidence of PCO[45]. IOL optic capture technique has come into widespread application since it was first introduced by Gimbel. For those implantation of haptics in the capsule and optic capture through the capsule opening, the incidence of postoperative PCO ranged from 0 to 80%, with an average of 5.71% (18/315)[8-11,13-17,19,21-23,25-26]. And for those implantation of haptics in the ciliary sulcus and optic capture through the capsule opening, the incidence of postoperative PCO was 0 (0/18)[12,22]. Raina et al[8]observed no PCO in 16 eyes underwent IOL optic capture procedure. Dada et al[17]used IOL optic capture in 14 eyes and followed up for 36mo. The visual axis remained clear in all the eyes in the IOL optic capture group, but 57.14% of the eyes in the non-capture group developed PCO. Argento et al[14]reported that eight eyes of 5 children had cataract extraction with AcrySof IOLs optic capture, the visual axis remained clear in all cases during the follow-up period. It was posited that the adhesive properties of AcrySof IOLs to the capsular bag played an important role in preventing PCO. Grieshaber et al[23]evaluated 68 eyes that underwent the IOL optic capture technique. The visual axis remained clear in all eyes during postoperative follow-up. In 2005, Zhou et al[20]conducted a Meta-analysis covering 282 eyes and found the IOL optic capture technique to be safe and to significantly reduce the incidence of PCO in pediatric cataract surgery. Vasavada et al[19]recently published a report of 26 eyes that were subjected to pediatric cataract surgery IOL capture, no anterior vitrectomy was performed, and all visual axes remain transparent. In a previous study, they found proliferation of lens epithelial cells (LECs) and projection onto the IOL 18mo after optic capture of a 1-piece PMMA IOL[22]. In the current study, they found that this phenomenon did not occur during the 12mo of follow-up. They concluded that this might be attributable to the design of the 3-piece IOL,allowing almost 360 degrees of capsular fusion and the fusion of the anterior and posterior capsules leads to sequestration of LECs within the capsular fornices and prevents their migration to the intact anterior vitreous face. Furthermore, with better techniques, ophthalmic viscosurgical devices (OVDs), and instrumentation there might be lesser iris manipulation, thus reducing postoperative inflammatory sequelae.
GlaucomaSecondary glaucoma is an important postoperative sight-threatening complication of pediatric cataract surgery[46-47].The incidence has been variably reported as between 10%and 21% in the literature[48-51]. Patients undergoing cataract surgery at an early age are at high risk for the development of glaucoma. According to IATS report[52-53], when operating on an infant younger than 7mo of age with a unilateral cataract,IOL implantation resulted in more actual and suspected glaucoma than leaving the eye aphakic, although the difference was not significant at 1y postoperative follow-up. However,there were no reports of glaucoma after IOL optic capture technique[10,19,25]. Grieshaber et al[23]used optic entrapment of the IOL in 68 eyes and followed the patients up for 9y.Vasavada et al[10]reported optic capture in 41 pediatric eyes and followed up for 21.04mo. Glaucoma was not observed in either study. In 2017, Vasavada et al[19]also published a report of 26 eyes of children under 4 years old who underwent cataract IOL capture. They were followed up for 12mo, and no glaucoma was observed. A recent Meta-analysis concluded that the risk of postoperative glaucoma after cataract surgery in infants less than 1 year of age may be influenced by the timing of surgery, primary IOL implantation, and additional intraocular surgery[46]. The mechanism underlying the relatively low incidence of glaucoma after IOL optic capture might involve backward movement of the optic part of IOL and an increase in the anterior space. This hypothesis will need further investigation.
Intraocular Lens DecentrationIOL decentration is not uncommon after IOL implantation after pediatric cataract surgery and can be caused by the rupture of or injury to the suspension ligaments. In some cases, abnormal IOL location, e.g. one haptic placed in the capsular bag while the other placed in the ciliary sulcus, which may also cause IOL decentration. Some IOL decentration may be caused by unsymmetrical shrinkage of the capsular bag. Since the introduction of IOL optic capture technique, the decentration of IOL has not been reported to be attributed to the satisfactory capsular fixation from ACCC and PCCC. Vasavada et al[10]performed IOL optic capture in 41 pediatric eyes. Excellent IOL centration was maintained in all the eyes. This study and others[12-14,19,22]demonstrated that the optic capture technique provides stability and long-term centration of the IOL.
Inflammation and Iris SynechiaPediatric eye usually has higher tissue reactivity, which pose a risk of severe inflammation response and formation of iris synechia or PCO after surgery[54-55]. The incidence of inflammation and iris synechia after pediatric cataract IOL capture ranged from 0 to 100%, with an average of 13.87% (38/274)[8,10-11,13,16,19,22-23,25-26].However, the effects of IOL optic capture on the risk and severity of iris inflammation are still debated. Some studies have proposed that since the IOL position is moved backward in IOL optic capture technique, the distance between the posterior surface of the iris and IOL increases. As a result, the chaffing and rubbing between iris and IOL decreases and so does the iris’ inflammatory reactions[12,56]. In 2005, Grieshaber et al[23]performed IOL entrapment procedure in 68 pediatric cataract eyes. The incidence of posterior synechia was 8.8%.Vasavada and Trivedi[22]reported a 71.4% incidence of uveal inflammation and posterior synechia in 14 eyes that underwent IOL optic capture. Most synechia formed at fixated haptics and at sites of optic capture through the posterior capsulorhexis.Based on this finding, Vasavada and Trivedi[22]concluded that IOL optic capture actually increases the post operational inflammatory reactions of the iris. However, Vasavada et al[19]recently published a report covering 26 eyes of children with cataracts who underwent capture implantation and 30 eyes that were subjected to conventional capsule implantation and there were no statistically significant differences in the incidence of posterior synechiae or cell deposits between the two groups.In 2018, Cicik et al[26]reported 26 eyes of pediatric cataract IOL optic capture, and there was no uveitic reaction, posterior synechiae occurred after operation. According to Zhou et al[20]Meta-analysis in 282 eyes, IOL optic capture has no significant effect on the incidence of posterior synechia after pediatric cataract surgery.
Pupillary CapturePupillary capture is a common complication after pediatric cataract surgery, which occurs most often in children under 2 years of age, when an optic size of less than 6 mm is used and the lens is placed in the ciliary sulcus[57]. The IOL optic capture technique involves drawing an IOL optic through a PCCC opening, and apposition of the anterior and posterior capsule leaflets. This maneuver ensures the anterior and posterior capsule leaflets are closely in contact and closed on the front surface of IOL. In this way, the risk for pupil capture is greatly reduced. This is one of important advantages of IOL optic capture. So far, complication of pupillary capture after IOL capture are rarely reported.
Intraocular Lens Surface DepositsThe typical IOL deposits that develop after cataract surgery include small cells, giant cells and erythrocytes, and pigment granules[58]. IOL deposits usually do not affect visual acuity significantly. Pediatric patients with darker irises or who are less compliant with postoperative medication regimens are more likely to develop IOL deposits. The small round-shaped cellular deposits that occurred soon after the operation are typically associated with impairments in the intraocular blood-aqueous barrier, while the giant cell deposits that develop later are associated with iris inflammatory responses[27]. The incidence of IOL surface deposits after pediatric cataract IOL capture ranged from 0 to 100%, with an average of 15.31% (32/209)[8,10-13,16,19,22-23].Vasavada and Trivedi[22]conducted a study covering 40 eyes and reported that deposits on the anterior IOL surface occurred in all eyes in the optic-capture group and in 61.5% in the nocapture group. The deposits in the optic-captured group were greater in number and persisted longer than those in the nocapture group. They proposed a possible explanation that the both anterior and posterior capsule openings were located at the front surface of IOL. The deposits may include pigments,inflammatory cells, or lens cortex. Grieshaber et al[23]performed IOL entrapment procedure in 68 pediatric cataract eyes, no pigment deposits were observed in all eyes. Zhou et al[20]conducted a Meta-analysis covering 282 eyes and found there to be significantly more deposits in the anterior IOL in the optic capture group early after surgery and at the last follow-up than in the control group. Some studies found that anti-inflammatory treatment significantly decreased the deposit at the last follow-up[8,10,12-13]. The use of heparin-modified IOLs also decreased the incidence of IOL surface deposits[28].
Cystoid Macular EdemaThere is no report of cystoid macular edema (CME) in children who underwent IOL optic capture with or without vitrectomy to date[10,12,23,25]. A few early works reported the occurrence of CME after pediatric cataract surgery. Hoyt and Nickel[59]reported 10 out of 27 eyes (37%)developed aphakic CME. However, later literature reposts contradicted these findings and attribute the uncommon CME to current fine microsurgical techniques, the lack of hypotony during surgery and postoperative apply of steroids,cycloplegics and non-steroidal antiinflammatory drugs(NSAIDs)[60-61].
Retinal DetachmentThe most common risk factors of retinal detachment (RD) include male, myopic, and intellectual disabled child. A recent review of the Agarkar et al[62]of 481 eyes showed that the risk of RD was expected to be 5.5% for the first 10y after cataract surgery in children with no known eye and systemic abnormalities. Rabiah[51]reported an overall 3.2% frequency of RD. Haargaard et al[63]reported following up 1043 pediatric patients after cataract surgery for 20y in Denmark. The frequency of RD was 7%, with 3% occurring in patients with simple cataracts. There is no report of RD in pediatric patients who underwent IOL optic capture to date[23,25].
CONCLUSION
Reducing or avoiding PCO, the most common complication occurs after pediatric cataract surgery, has been a serious goal for ophthalmologists. To date, the critical factors contributing to the initiation of PCO and the effective managements of PCO are debatable. Whether and when to perform anterior vitrectomy and how anterior vitrectomy will affect the development of PCO are the subject of much discussion.The IOL optic capture technique leaves the anterior and posterior capsules with more contact area and can be united more closely. Good centralization of the IOL is achieved and consequently the incidence of PCO is reduced. Meanwhile,IOL optic capture technique does not increase the incidence of other post-operative complications, which appears to be a promising alternative to the standard surgical technique for the treatment of pediatric cataracts and it might allow clinicians to avoid the additional step of anterior vitrectomy.
ACKNOWLEDGEMENTS
Authors’ contributions:Wang LH and Ren MY conceived of the review. Xie YB drafted the manuscript. Wang Q made the tables.
Conflicts of Interest:Xie YB, None; Ren MY, None; Wang Q, None; Wang LH, None.
REFERENCES
1 Magnusson G, Haargaard B, Basit S, Lundvall A, Nystrom A,Rosensvard A, Tornqvist K. The Paediatric Cataract Register (PECARE):an overview of operated childhood cataract in Sweden and Denmark. Acta Ophthalmol 2018;96(1):51-55.
2 Demirkılınç Biler E, Yıldırım Ş, Üretmen Ö, Köse S. Long-term results in pediatric developmental cataract surgery with primary intraocular lens implantation. Turk J Ophthalmol 2018;48(1):1-5.
3 Corredor-Ortega C, Gonzalez-Salinas R, Montero MJ, González-Flores R, Collura-Merlier A, Cervantes-Coste G. Femtosecond laser-assisted cataract surgery in pediatric patients. J AAPOS 2018;22(2):148-149.
4 Sukhija J, Ram J, Gupta N, Sawhney A, Kaur S. Long-term results after primary intraocular lens implantation in children operated less than 2 years of age for congenital cataract. Indian J Ophthalmol 2014;62(12):1132-1135.
5 Khokhar SK, Pillay G, Agarwal E, Mahabir M. Innovations in pediatric cataract surgery. Indian J Ophthalmol 2017;65(3):210-216.
6 Lim ME, Buckley EG, Prakalapakorn SG. Update on congenital cataract surgery management. Curr Opin Ophthalmol 2017;28(1):87-92.
7 Vasavada A, Desai J. Primary posterior capsulorhexis with and without anterior vitrectomy in congenital cataracts. J Cataract Refract Surg 1997;23(Suppl 1):645-651.
8 Raina UK, Gupta V, Arora R, Mehta DK. Posterior continuous curvilinear capsulorhexis with and without optic capture of the posterior chamber intraocular lens in the absence of vitrectomy. J Pediatr Ophthalmol Strabismus 2002;39(5):278-287.
9 Gimbel HV. Posterior capsulorhexis with optic capture in pediatric cataract and intraocular lens surgery. Ophthalmology 1996;103(11):1871-1875.
10 Vasavada AR, Trivedi RH, Singh R. Necessity of vitrectomy when optic capture is performed in children older than 5 years. J Cataract Refract Surg 2001;27(8):1185-1193.
11 Gimbel HV, DeBroff BM. Posterior capsulorhexis with optic capture:maintaining a clear visual axis after pediatric cataract surgery. J Cataract Refract Surg 1994;20(6):658-664.
12 Faramarzi A, Javadi MA. Comparison of 2 techniques of intraocular lens implantation in pediatric cataract surgery. J Cataract Refract Surg 2009;35(6):1040-1045.
13 Raina UK, Mehta DK, Monga S, Arora R. Functional outcomes of acrylic intraocular lenses in pediatric cataract surgery. J Cataract Refract Surg 2004;30(5):1082-1091.
14 Argento C, Badoza D, Ugrin C. Optic capture of the AcrySof intraocular lens in pediatric cataract surgery. J Cataract Refract Surg 2001;27(10):1638-1642.
15 Gimbel HV. Posterior continuous curvilinear capsulorhexis and optic capture of the intraocular lens to prevent secondary opacification in pediatric cataract surgery. J Cataract Refract Surg 1997;23(Suppl 1):652-656.
16 Müllner-Eidenböck A, Amon M, Moser E, Kruger A, Abela C,Schlemmer Y, Zidek T. Morphological and functional results of AcrySof intraocular lens implantation in children: prospective randomized study of age-related surgical management. J Cataract Refract Surg 2003;29(2):285-293.
17 Dada T, Dada VK, Sharma N, Vajpayee RB. Primary posterior capsulorhexis with optic capture and intracameral heparin in paediatric cataract surgery. Clin Exp Ophthalmol 2000;28(5):361-363.
18 Fernandez V, Fragoso MA, Billotte C, Lamar P, Orozco MA, Dubovy S, Willcox M, Parel JM. Efficacy of various drugs in the prevention of posterior capsule opacification: experimental study of rabbit eyes. J Cataract Refract Surg 2004;30(12):2598-2605.
19 Vasavada AR, Vasavada V, Shah SK, Trivedi RH, Vasavada VA,Vasavada SA, Srivastava S, Sudhalkar A. Postoperative outcomes of intraocular lens implantation in the bag versus posterior optic capture in pediatric cataract surgery. J Cataract Refract Surg 2017;43(9):1177-1183.
20 Zhou HW, Zhou F. A Meta-analysis on the clinical efficacy and safety of optic capture in pediatric cataract surgery. Int J Ophthalmol 2016;9(4):590-596.
21 Koch DD, Kohnen T. A retrospective comparison of techniques to prevent secondary cataract formation after posterior chamber intraocular lens implantation in infants and children. J Cataract Refract Surg 1997;23(Suppl 1):657-663.
22 Vasavada AR, Trivedi RH. Role of optic capture in congenital cataract and intraocular lens surgery in children. J Cataract Refract Surg 2000;26(6):824-831.
23 Grieshaber MC, Pienaar A, Stegmann R. Posterior vertical capsulotomy with optic entrapment of the intraocular lens in congenital cataracts-prevention of capsule opacification. J Cataract Refract Surg 2005;31(5):886-894.
24 Sharma N, Balasubramanya R, Dada VK, Vajpayee RB. Efficacy of trypan blue in posterior capsulorhexis with optic capture in pediatric cataracts. BMC Ophthalmol 2006;16(6):12.
25 Grieshaber MC, Olivier J, Pienaar A, Stegmann R. Capsular opacification after vitreous-sparing cataract surgery in children. Klin Monbl Augenheilkd 2009;226(4):258-263.
26 Cicik ME, Dogan C, Bolukbasi S, Cinhuseyinoglu MN, Arslan OS.Comparison of two intraocular lens implantation techniques in pediatric cataract surgery in terms of postoperative complications. Balkan Med J 2018;35(2):186-190.
27 Özyol P, Özyol E, Karel F. Biocompatibility of intraocular lenses. Turk J Ophthalmol 2017;47(4):221-225.
28 Basti S, Aasuri MK, Reddy MK, Preetam P, Reddy S, Gupta S,Naduvilath TJ. Heparin-surface-modified intraocular lenses in pediatric cataract surgery: prospective randomized study. J Cataract Refract Surg 1999;25(6):782-787.
29 Pandolfi M, Kwaan HC. Fibrinolysis in the anterior segment of the eye. Arch Ophthalmol 1967;77(1):99-104.
30 Johnson RN, Blankenship G. A prospective, randomized, clinical trial of heparin therapy for postoperative intraocular fibrin. Ophthalmology 1988;95(3):312-317.
31 Aasuri MK, Fernandes M, Pathan PP. Comparison of acrylic and polymethyl methacrylate lenses in a pediatric population. Indian J Ophthalmol 2006;54(2):105-109.
32 Rowe NA, Biswas S, Lloyd IC. Primary IOL implantation in children:a risk analysis of foldable acrylic v PMMA lenses. Br J Ophthalmol 2004;88(4):481-485.
33 Kleinmann G, Zaugg B, Apple DJ, Bleik J. Pediatric cataract surgery with hydrophilic acrylic intraocular lens. J AAPOS 2013;17(4):367-370.
34 Packer M, Rajan M, Ligabue E, Heiner P. Clinical properties of a novel, glistening-free, single-piece, hydrophobic acrylic IOL. Clin Ophthalmol 2014;21(8):421-427.
35 Baradaran-Rafii A, Shirzadeh E, Eslani M, Akbari M. Optical correction of aphakia in children. J Ophthalmic Vis Res 2014;9(1):71-82.
36 Sukhija J, Kaur S, Ram J. Outcome of a new acrylic intraocular lens implantation in pediatric cataract. J Pediatr Ophthalmol Strabismus 2015;52(6):371-376.
37 Tetz M, Jorgensen MR. New hydrophobic IOL materials and understanding the science of glistenings. Curr Eye Res 2015;40(10): 969-981.
38 Solebo AL, Russell-Eggitt I, Nischal KK, Moore AT, Cumberland P,Rahi JS. British Isles Congenital Cataract Interest Group. Cataract surgery and primary intraocular lens implantation in children ˂ or = 2 years old in the UK and Ireland: finding of national surveys. Br J Ophthalmol 2009;93(11):1495-1498.
39 Chéour M, Ben Brahim F, Zarrad A, Khémiri N, Mghaieth K, Kraiem A. Trypan blue capsule staining for phacoemulsification in white cataract.J Fr Ophtalmol 2007;30(9):914-917.
40 Bhartiya P, Sharma N, Ray M, Sinha R, Vajpayee RB. Trypan blue assisted phacoemulsification in corneal opacities. Br J Ophthalmol 2002;86(8):857-859.
41 Kiel AW, Butler T. A novel use for trypan blue to minimize epithelial cell proliferation in pediatric cataract surgery. J Pediatr Ophthalmol Strabismus 2003;40(2):96-97.
42 Lotfy A, Abdelrahman A. Trypan blue-assisted posterior capsulorhexis in pediatric cataract surgery. Clin Ophthalmol 2017;24(11):219-222.
43 Gasper C, Trivedi RH, Wilson ME. Complications of pediatric cataract surgery. Dev Ophthalmol 2016;57:69-84.
44 Vasavada V. Paradigms for pediatric cataract surgery. Asia Pac J Ophthalmol (Phila) 2018;7(2):123-127.
45 Bar-Sela SM, Har-Noy NB, Spierer A. Secondary membrane formation after cataract surgery with primary intraocular lens implantation in children. Int Ophthalmol 2014;34(4):767-772.
46 Mataftsi A, Haidich AB, Kokkali S, Rabiah PK, Birch E, Stager DR Jr, Cheong-Leen R, Singh V, Egbert JE, Astle WF, Lambert SR, Amitabh P, Khan AO, Grigg J, Arvanitidou M, Dimitrakos SA, Nischal KK.Postoperative glaucoma following infantile cataract surgery: an individual patient data Meta-analysis. JAMA Ophthalmol 2014;132(9):1059-1067.
47 Chen D, Gong XH, Xie H, Zhu XN, Li J, Zhao YE. The long-term anterior segment configuration after pediatric cataract surgery and the association with secondary glaucoma. Sci Rep 2017;7(1):43015.
48 Swamy BN, Billson F, Martin F, Donaldson C, Hing S, Jamieson R,Grigg J, Smith JE. Secondary glaucoma after paediatric cataract surgery.Br J Ophthalmol 2007;91(12):1627-1630.
49 Trivedi RH, Wilson E Jr, Golub RL. Incidence and risk factors for glaucoma after pediatric cataract surgery with and without intraocular lens implantation. J AAPOS 2006;10(2):117-123.
50 Egbert JE, Christiansen SP, Wright MM, Young TL, Summers CG.The natural history of glaucoma and ocular hypertension after pediatric cataract surgery. J AAPOS 2006;10(1):54-57.
51 Rabiah PK. Frequency and predictors of glaucoma after pediatric cataract surgery. Am J Ophthalmol 2004;137(1):30-37.
52 Infant Aphakia Treatment Study Group, Lambert SR, Buckley EG,Drews-Botsch C, DuBois L, Hartmann EE, Lynn MJ, Plager DA, Wilson ME. A randomized clinical trial comparing contact lens with intraocular lens correction of monocular aphakia during infancy: grating acuity and adverse events at age 1 year. Arch Ophthalmol 2010;128(7):810-818.
53 Beck AD, Freedman SF, Lynn MJ, Bothun E, Neely DE, Lambert SR,Infant Aphakia Treatment Study Group. Glaucoma-related adverse events in the Infant Aphakia Treatment Study: 1-year results. Arch Ophthalmol 2012;130(3):300-305.
54 Whitman MC, Vanderveen DK. Complications of pediatric cataract surgery. Semin Ophthalmol 2014;29(5-6):414-420.
55 Zetterström C, Kugelberg M. Paediatric cataract surgery. Acta Ophthalmol Scand 2007;85(7):698-710.
56 Gimbel HV, DeBroff BM. Intraocular lens optic capture. J Cataract Refract Surg 2004;30(1):200-206.
57 Pandey SK, Wilson ME, Trivedi RH, Izak AM, Macky TA, Werner L,Apple DJ. Pediatric cataract surgery and intraocular lens implantation:current techniques, complications, and management. Int Ophthalmol Clin 2001;41(3):175-196.
58 Ygge J, Wenzel M, Philipson B, Fagerholm P. Cellular reactions on heparin surface-modified versus regular PMMA lenses during the first postoperative month. A double-masked and randomized study using specular microphotography. Ophthalmology 1990;97(9):1216-1224.
59 Hoyt CS, Nickel B. Aphakic cystoid macular edema: occurrence in infants and children after transpupillary lensectomy and anterior vitrectomy. Arch Ophthalmol 1982;100(5):746-749.
60 Rao SK, Ravishankar K, Sitalakshmi G, Ng JS, Yu C, Lam DS.Cystoid macular edema after pediatric intraocular lens implantation:fluorescein angioscopy results and literature review. J Cataract Refract Surg 2001;27(3):432-436.
61 Kirwan C, O'Keeffe M. Cystoid macular oedema in paediatric aphakia and pseudophakia. Br J Ophthalmol 2006;90(1):37-39.
62 Agarkar S, Gokhale VV, Raman R, Bhende M, Swaminathan G, Jain M. Incidence, risk factors, and outcomes of retinal detachment after pediatric cataract surgery. Ophthalmology 2018;125(1):36-42.
63 Haargaard B, Andersen EW, Oudin A, Poulsen G, Wohlfahrt J, la Cour M, Melbye M. Risk of retinal detachment after pediatric cataract surgery.Invest Ophthalmol Vis Sci 2014;55(5):2947-2951.
Correspondenceto:Li-Hua Wang. Department of Ophthalmology, Shandong Provincial Hospital Affiliated to Shandong University, No.324, Jingwu Road, Jinan 250021, Shandong Province, China. wang_glasses@163.com
Received:2018-04-13 Accepted: 2018-06-27
Abstract
● Posterior capsule opacification (PCO) remains the most common complication of pediatric cataract surgery despite continuous efforts to reduce its incidence. For this reason,pediatric cataract surgeons have expended considerable effort into preventing and mitigating PCO. The intraocular lens (lOL) optic capture technique has been used for the prevention of PCO after pediatric cataract surgery for more than 20y, but there is still no professional consensus.However, recent research has shown encouraging results.The lOL optic capture technique can be performed without anterior vitrectomy to prevent PCO, even in younger children.The type and characteristics of lOLs used for optic capture technique, the location of lOL and the complications of lOL optic capture in children are here reviewed.
● KEYWORDS:cataract; pediatric; lens; intraocular; surgery
DOl:10.18240/ijo.2018.08.24
Citation:Xie YB, Ren MY, Wang Q, Wang LH. Intraocular lens optic capture in pediatric cataract surgery. Int J Ophthalmol 2018;11(8):1403-1410