Visual and morphological outcomes of vitreomacular traction syndrome in retinitis pigmentosa treated by vitrectomy
Feng Yan1, Feng-Jie Xia2, Feng Jiang1, Hyeong Gon Yu3
1Department of Ophthalmology, Jinling Hospital, School of Medicine, Nanjing University, Nanjing 210002, Jiangsu Province, China
2Medical School of Nanjing University, Department of Ophthalmology, Jinling Hospital, Nanjing 210002, Jiangsu Province, China
3Department of Ophthalmology, Seoul National University Hospital, Seoul National University College of Medicine,Seoul 110-744, South Korea
INTRODUCTION
Retinitis pigmentosa (RP) is a heterogeneous group of genetic retinal disorders that primarily affect the rod and cone photoreceptors and the retinal pigment epithelial (RPE)cells. Macular complications can significantly reduce the visual acuity in patients with RP whose central vision is usually well preserved until the late stages of the disease. These macular abnormalities include cystoid macular edema (CME),epiretinal membranes (ERM), vitreomacular traction (VMT)syndrome and macular holes (MHs)[1]. In order to maintain the remnant central vision of RP patients, the vitrectomy is necessary in some cases.
Optical coherence tomography (OCT) is a noninvasive technique that can assess the morphology of the retina, especially the macula in vivo. This technique is especially useful in patients with RP, because OCT enables the investigator to evaluate the morphologic changes in each retinal layer and the overall retina. The recent introduction of spectral-domain optical coherence tomography (SD-OCT) has improved image resolution and has enabled the analysis of various macular morphologies quantitatively. SD-OCT can assess the photoreceptor cells in vivo, both retinal thinning caused by photoreceptor cell loss and retinal thickening due to macular edema appeared to be associated with a worse vision in RP patients[2-3]and the total macular volume was a significant correlation with the amplitudes of the a- and b-waves of the focal macular electroretinograms (fmERGs)[4]. In addition,the presence of ellipsoid zone (EZ) was associated with better visual acuity and the absence of an EZ may reflect a foveal dysfunction in RP patients[5]. The length of the EZ line generally correlated with the fmERG amplitude[3]and the width of the EZ seems to be a sensitive and reliable measure of progression in RP eyes[6]. Therefore, the EZ line and foveal thickness may be important parameters tomonitor macular abnormalities in RP patients.
Hyperreflective foci (HFs) or small dense particles are observed in pathological retinas and have been considered as macrophages,migrating RPE cells, or extravasated lipoproteins resulting from retinal inflammation or the breakdown of retinal vessel barriers. It has been reported that HFs might be indicative of changes in the retinal structure at each stage of RP[7].
To our knowledge, there are few reports on the anatomical and functional outcomes of vitreoretinal surgery for RP with macular abnormalities. In this study, we examined retinal morphologies by SD-OCT to assess the outcomes of vitreoretinal surgery for RP with macular abnormalities.
METHODS
In accordance with the Helsinki Declaration, the patients were informed about all relevant aspects of the surgery and of the use of their data. They signed an informed consent before enrolment. The study protocol was approved by the Ethical Committee of the Seoul National University Hospital.
The retrospective study comprised 13 eyes of 11 RP patients who underwent vitrectomy for VMT syndrome and who were followed up for at least 9mo after surgery. The mean postoperative follow-up time was 35.2±15.8mo (range, 9-60mo).All procedures took place at Seoul National University Hospital between January 2010 and February 2016. RP was diagnosed on the basis of a history of night blindness and ophthalmologic findings. To diagnose RP, each participant was subjected to a complete ophthalmologic examination, including a review of the participant’s medical and clinical history,measurement of best corrected visual acuity (BCVA), slitlamp biomicroscopy, dilated fundoscopic examination, visual field testing, and full-field electroretinography. BCVA was evaluated by examiners who were masked to the information obtained during previous determinations using the same Snellen projection chart at 5 m in decimal units. The decimal acuities were converted into a logarithm of the minimum angle of resolution (logMAR) for the statistical analysis.
Spectral Domain-optical Coherence Tomography Image AnalysisThe morphology of all patients’ macula was assessed by SD-OCT using Cirrus high-density OCT (HD-OCT;Carl Zeiss Meditec Inc., Dublin, CA, USA). The acquisition protocol consisted of an HD 5-line raster scan composed of 1024 A-scans at each 6 mm line and a macular cube with a 200×200 scan pattern in which a 6 mm×6 mm region of the retina was scanned. Each eye was pharmacologically dilated prior to OCT scanning. All scans were performed by the same certified OCT technician. A total of three “highquality” scans were obtained; these were defined as scans with a signal strength ≥6 which would exhibit correct delineation of the inner limiting membrane (ILM) and RPE as detected automatically by the intrinsic software segmentation algorithm.Macular thickness values were calculated automatically by the software included with the machine. The retinal thickness within the inner circle 1 mm in diameter was defined as the central subfield (CSF) thickness. Overall average macular thickness and overall macular volume over the entire grid area were also obtained from the computational software output.
The greyscale images were used for a more precise identification and measurement of the EZ and HFs distribution patterns.
The appearance of the EZ in the OCT images at the fovea was graded from 1 to 3: Grade 1, EZ not visible; Grade 2, abnormal EZ; and Grade 3, normal EZ. To grade the cases, we measured the length of the EZ, which extended from just beneath the fovea, and defined eyes as Grade 3 when the length of the continuous EZ line was ˃0.5 mm. The eyes with disruptions of the EZ just beneath the fovea were placed in Grade 2[4,6]. We observed the macular morphology, the grade of the EZ, central foveal thickness (CFT) and HF locations by SD-OCT.
Surgical MethodsVitreoretinal surgery was performed on seven patients with ERM, four patients with stage 4 MH.Vitrectomy combined with phacoemulsification and aspiration with intraocular lens implantation because all patients had cortical cataracts. All surgeries were performed by a single surgeon (Yu HG) under retrobulbar anesthesia. In each case, a Millennium 25-gauge transconjunctival sutureless vitrectomy system (Baush & Lomb., St. Louis, MO, USA) was used to perform 3-port pars plana vitrectomy (PPV). The ERM was peeled using end gripping forceps (Alcon Surgical, Fort Worth,Texas, USA) with assistance of triamicinolone acetonide or indocyanine green. During the surgeries, ILM peeling was performed in all cases. Sulphur hexafluoride (SF6) or octafluoropropane (C3F8) gas tamponade was used in the first operation of all the cases, but silicon oil was used in the repeat operations which occurred in one MH case.
Statistical AnalysisThe data were showed as the arithmetic mean±standard deviation (SD). All statistical analyses were performed using Wilcoxon signed rank test to compare the preoperation and post-operation examination. P values less than 0.05 were considered significant.
RESULTS AND DISCUSSION
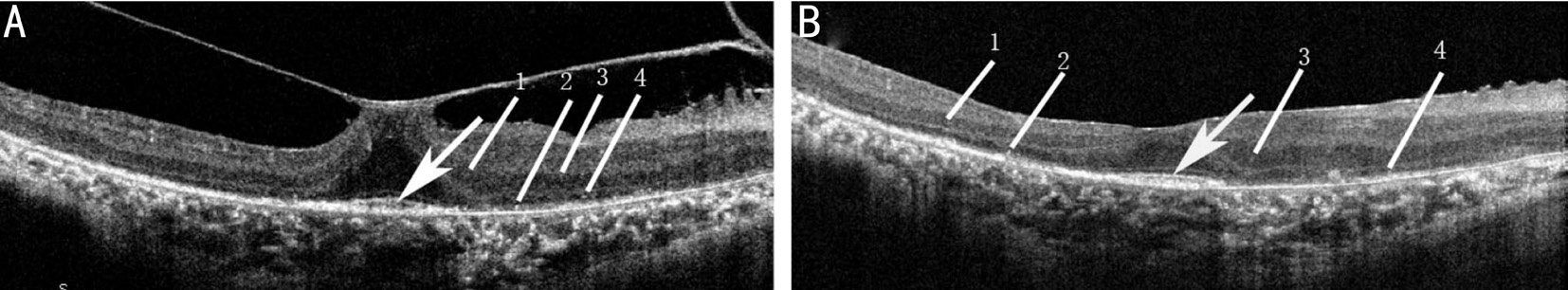
Visual AcuityThe mean±SD patient age was 56.62±7.77y(range, 38-67y) including 9 eyes with ERM and 4 eyes with MH. In the ERM cases, ERMs of 7 eyes (totally 9 eyes,77.8%) were well removed (Figure 1) and vitreous traction was released. Vision acuity of the 7 cases was improved in 6 eyes, unchanged in 1 eye. ERMs of 2 eyes (case No.3 and 5) was recurred. The visual acuity of case No.3 was reduced postoperatively, while the visual acuity of case No.5 was improved significantly.
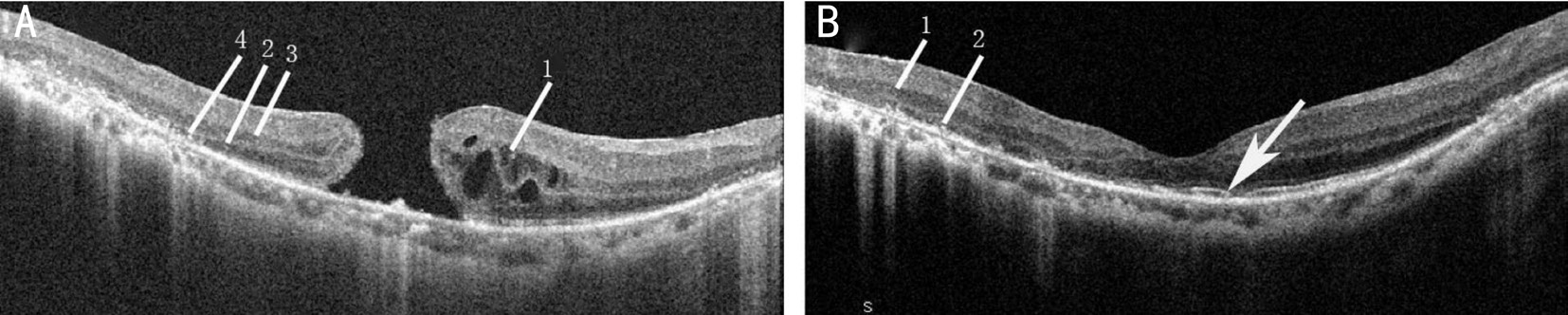
In the MH cases, 3 eyes (totally 4 eyes, 75%) obtained MH closure. In 2 eyes (cases No.10 and 11), the grade of EZ was increased from Grade 1 to Grade 2 after vitrectomy, in accordance with the morphological change, the BCVA of the 2 cases was improved (Figure 2). But vision unchanged in 1 eye (case No.12) probably because of long term damage and progress of photoreceptor or the RPE cells loss, leading to retinal thinning and atrophy of the RPE at the macula. One eye (case No.13) underwent 3 times of PPV for remained MH,but the MH kept unclosed and the visual acuity was reduced postoperatively.
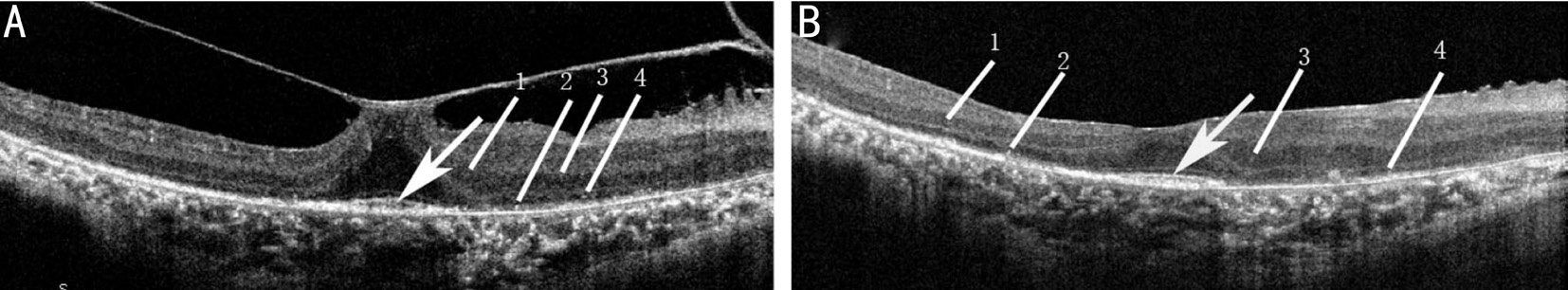
Figure 1 Greyscale SD-OCT images of a 6-mm horizontal macular scan from the case No.1 The images mainly show the ERM was well removed and the morphology of the macula was improved after the surgery. The visual acuity was improved by 0.19 logMAR. A: The baseline scan. The grade of EZ (arrow) was Grade 2 and HFs was located in the INL and ONL. The central subfield thickness was 269 μm; B: At approximately 9mo post-PPV. The grade of EZ (arrow) and the locations of HFs were both unchanged. The central subfield thickness reduced to 192 μm. 1, 3: HFs in the INL; 2, 4: HFs in the ONL.
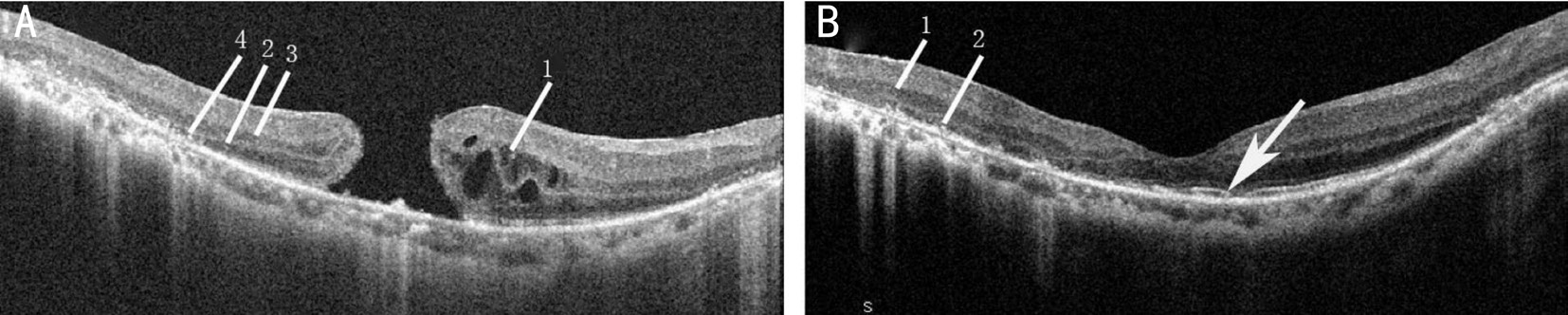
Figure 2 Greyscale SD-OCT images of a 6-mm horizontal macular scan from the case No.10 The images mainly showed that the MH was well closed and the morphology of the macula was improved after the surgery. The visual acuity was improved by 0.60 logMAR. A: The baseline scan. The grade of EZ was Grade 1 and the HFs were located in the INL and ONL. The central subfield thickness was 283 μm; B: At approximately 60mo post-PPV. The grade of EZ (arrow) recovered to Grade 2 and the locations of HFs were unchanged. The central subfield thickness was 191 μm. 1, 3: HFs in the INL; 2, 4: HFs in the ONL.
The mean baseline BCVA was 1.09±0.71 (range 0.40-2.30).The mean final BCVA was 0.86±0.85 (range 0.10-2.30). In the statistical analysis of the BCVA before and after the operation,there was no significant difference between the pre-operation and post-operation eyes (P=0.068).
But the visual acuity of cases No.3 and 13 decreased after the surgery and they were the only two cases whose visual acuity reduced significantly in all the 13 cases after the operation.
Macular MorphologyThe grade of EZ increased from Grade 1 to Grade 2 after vitrectomy in 2 cases (case No.10 and 11), in accordance with which, the BCVA of the 2 cases both increased significantly. The EZ of the other 11 cases were not changed after vitrectomy. HFs of one case (case No.13)located both in outer nuclear layer (ONL) and inner nuclear layer (INL) pre-operation, and only located in ONL postoperation. HFs of the other 12 cases located in both ONL and INL before operation, and the location of HFs did not changed after operation. HFs of one case (case No.3) located only in INL pre-operation and post-operation.
Before the vitrectomy, the mean CSF thickness was 376.46±63.63 µm, the mean cube volume was 10.19±1.08 mm3, and the mean cube average thickness was 285.31±31.23 µm. SDOCT showed a considerable reduction in CSF thickness from 376.46±63.63 to 241.77±94.71 µm after vitrectomy (P=0.002).And the mean cube volume and the mean cube average thickness also reduced significantly after the vitreoretinal surgery (P=0.014, 0.016).
RP is an inheritable blinding disease. The earliest histopathologic change is the shortening of outer segments in the rods. After that, the decay of rod photoreceptors occurs. Ultimately, the shortening of outer segments in the cone cells and the decay of cones lead to central vision loss. Macular abnormalities were more frequent in RP patients compared to the general population, ranging from mild ERM, cystoid maculopathy to full-thickness MH[8]. VMT might exert traction forces on the macula and VMT was associated with ERM formation and the development of MH[9]. Therefore, some ophthalmologists believe it is necessary to relieve VMT in RP patients by vitrectomy surgery as same in VMT patients without RP, ignoring both the degeneration of the vitreous body and the inflammation of retina might also result in the ERM and MH in RP patients.
SD-OCT can reveal the detailed structure of retinas in the progression of RP, including the inner/outer segment junction(IS/OS) of the photoreceptors. The presence of IS/OS line also known as EZ band most indicates that the normal function of the photoreceptors, while the absence of EZ band indicates the dysfunction of the fovea. Furthermore, HFs have been considered as macrophages, migrating RPE cells, or extravasated lipoproteins resulting from retinal inflammation or the breakdown of retinal vessel barriers. HFs in the OCT images can indicate the progression of RP[7]. Thus, EZ grade and the location of HFs in SD-OCT images are both the morphological indicators which can represent the progression of RP. In this retrospective study, we measured the EZ, HFs,CSF thickness, macular volume of RP patients with VMT in the SD-OCT images. The purpose of this study was to evaluate the functional and morphological outcomes of RP patients with VMT by vitrectomy surgery and whether it was necessary to treat VMT in RP by surgery.
In the study, morphological improvement, such as ERMs removed and MH closed, was obtained in 10 of 13 eyes.But the detailed structures which were closely related with functions, such as EZ grade or locations of HFs, were improved only in 2 (cases No.10 and 11) of 13 eyes, unchanged in 10 of 13 eyes, worse in 1 of 13 eyes based on SD-OCT. The MH patients (cases No.10, 11, 12 and 13) who had the same EZ grades before the operation had different EZ grade outcomes after the operation. The ERM patients (cases No.3 and 5)who had the recurred ERM had absolutely different visual outcomes. No matter the visual outcomes of post-operation was unchanged, decreased or improved, in most cases, EZ grades and the distribution of HFs were unchanged. Therefore,EZ grades and HFs are not the sensitive predictors for the visual outcomes after the operation in RP patients with VMT.In addition, the visual function was also only significantly improved in the 2 (cases No.10 and 11) eyes, slightly improved in 6 eyes, unchanged in 2 eyes, worse in 2 eyes. In statistical analysis, there was no significant improvement of visual function and also no significant decrease of visual function during the follow-up period (P=0.068). Our study suggested that the postoperative visual/functional outcomes were variable and unpredicted. However, PPV and ILM removal could maintain the remnant central vision and prevent the further degeneration of photoreceptors in most of RP patients with VMT over the long-term.
In idiopathic ERM or MH, early membrane removals might be benefit to prevent further progression of photoreceptor damage in macular abnormality patients with photoreceptor disruption[10]. Unlike idiopathic macular abnormalities, RP patients with macular abnormalities were a progressive process and eventually resulted in the death of the photoreceptors. In addition, decreased macular blood flow and sustained chronic inflammatory reaction occurred in RP patients which were also associated with central vision loss[11]. Several studies had reported that vitrectomy and ILM removal improved visual acuity in RP patients with macular abnormalities[4,12]. In our study, there were also some cases who had significantly improved visual outcomes after the operation, while there were some cases who had decreased visual outcomes. These facts made us think that the main causes of vision loss might differ among RP patients with VMT. We hypothesized that VMT might be the main reason for vision loss in some cases,while inflammation and the progression of RP might be the main reason for vision loss in other cases. It was obvious that vitrectomy and ILM removal could not save the decayed photoreceptors or inhibit the progression of RP. On the other hand, the baseline BCVA of our cases (1.09±0.71) was much worse than other similar studies[10]. And this might be another reason that lead to our poor surgical outcomes.
In our cases, there were two patients (cases No.3 and 13)who had decreased visual acuity during the follow-up. ERM recurred in case No.3. The recurrence of ERM might result in the postoperative vision loss because the contraction of ERM could lead to macular edema which might impair the normal alignment of photoreceptors and accelerate the death of photoreceptors in RP patients[13]. Furthermore, RP is a heterogeneous group of inherited diseases that cause degeneration of rod and cone photoreceptors in the retina.The degenerative changes occur at all times, including the postoperative period. Therefore, the ERM- and RP-related degeneration of photoreceptors might be both causes of vision loss in patient No.3 postoperatively. In addition, the MH of the 1 eye (case No.13) with vision loss was not closed finally and 3 times vitreoretinal surgeries were performed during the follow-up period. Ultimately, the retina of the eye got atrophy and thinning so that the HFs in the INL might be not distinct in the SD-OCT image, which might lead to the location changes of the HFs in the eye (case No.13)[7].Several times surgeries might not be tolerated by the RP patients,which would lead to retinal thinning and visual acuity worsening.It has been reported that the traction of ERM leaded to the disruption of photoreceptors. Once photoreceptor cells were impaired, they hardly recovered with time after surgery. On the one hand, prolonged macular traction caused irreversible photoreceptor cells impairment and a change in the alignments of cone cells in eyes with macular edema. On the other hand, the histopathological change of the retina in RP was the degeneration of the rods and cones. VMT generally tended to take place in the advanced RP patients. In addition,indocyanine green (ICG) might potentially be toxic to the optical nerve fibers, accelerate epithelial atrophy and cause unfavorable visual outcomes[14]. Besides that, the operative illumination and the surgical trauma should be considered to be other causes of unsatisfied visual performances. Therefore, the longstanding dysfunction of photoreceptors in RP would make the rods and cones be more likely to be impaired irreversibly by the prolonged ERM traction, the surgical trauma and the ocular toxicity of ICG. In this study, statistical analysis showed that there was no significant improvement between postoperative visual outcomes and preoperative ones. We believed that careful consideration should be necessary before vitrectomy in RP patients. The prognostic outcomes of vitrectomy were not always favorable in RP patients with VMT.
In this study, the CSF thickness was significantly decreased after the vitrectomy surgery (P=0.002). The removal of ILM could release the macular traction, and then the macular edema would be absorbed over time after surgery. However,the photoreceptors which were dead before the surgery could hardly recover after the surgery. Both retinal thinning (due to cell loss) and retinal thickening (due to presumed edema)appeared to be associated with lower visual acuity in patients with typical RP[2]. Although the CSF thickness was decreased,the visual function was improved limitedly.
In conclusion, although vitrectomy could improve the macular morphology in some RP patients with VMT, visual outcomes might be limited and unpredicted most likely because of the long-standing retinal dysfunction. However, the vitrectomy is necessary in order to remain or improve the central vision in some cases.
ACKNOWLEDGEMENTS
Foundation: Supported by the National Natural Science Foundation of China (No.81600754).
Conflicts of Interest:Yan F, None; Xia FJ, None; Jiang F,None; Yu HG, None.
REFERENCES
1 Hagiwara A, Yamamoto S, Ogata K, Sugawara T, Hiramatsu A, Shibata M, Mitamura Y. Macular abnormalities in patients with retinitis pigmentosa:prevalence on OCT examination and outcomes of vitreoretinal surgery.Acta Ophthalmol 2011;89(2):e122-e125.
2 Sandberg MA, Brockhurst RJ, Gaudio AR, Berson EL. The association between visual acuity and central retinal thickness in retinitis pigmentosa.Invest Ophthalmol Vis Sci 2005;46(9):3349-3354.
3 Kim YJ, Joe SG, Lee DH, Lee JY, Kim JG, Yoon YH. Correlations between spectral-domain OCT measurements and visual acuity in cystoid macular edema associated with retinitis pigmentosa. Invest Ophthalmol Vis Sci 2013;54(2):1303-1309.
4 Sugita T, Kondo M, Piao CH, Ito Y, Terasaki H. Correlation between macular volume and focal macular electroretinogram in patients with retinitis pigmentosa. Invest Ophthalmol Vis Sci 2008;49(8):3551-3558.
5 Aizawa S, Mitamura Y, Baba T, Hagiwara A, Ogata K, Yamamoto S. Correlation between visual function and photoreceptor inner/outer segment junction in patients with retinitis pigmentosa. Eye (Lond)2009;23(2):304-308.
6 Birch DG, Locke KG, Felius J, Klein M, Wheaton DK, Hoffman DR,Hood DC. Rates of decline in regions of the visual field defined by frequencydomain optical coherence tomography in patients with RPGR-mediated X-linked retinitis pigmentosa. Ophthalmology 2015;122(4): 833-839.
7 Kuroda M, Hirami Y, Hata M, Mandai M, Takahashi M, Kurimoto Y.Intraretinal hyperreflective foci on spectral-domain optical coherence tomographic images of patients with retinitis pigmentosa. Clin Ophthalmol 2014;8:435-440.
8 Triolo G, Pierro L, Parodi MB, De Benedetto U, Gagliardi M, Manitto MP, Bandello F. Spectral domain optical coherence tomography findings in patients with retinitis pigmentosa. Ophthalmic Res 2013;50(3):160-164.
9 Steel DH, Lotery AJ. Idiopathic vitreomacular traction and macular hole: a comprehensive review of pathophysiology, diagnosis, and treatment. Eye (Lond) 2013;27(Suppl 1):S1-S21.
10 Ikeda Y, Yoshida N, Murakami Y, Nakatake S, Notomi S, Hisatomi T, Enaida H, Ishibashi T. Long-term surgical outcomes of epiretinal membrane in patients with retinitis pigmentosa. Sci Rep 2015;5:13078.
11 Murakami Y, Ikeda Y, Akiyama M, Fujiwara K, Yoshida N, Nakatake S,Notomi S, Nabeshima T, Hisatomi T, Enaida H, Ishibashi T. Correlation between macular blood flow and central visual sensitivity in retinitis pigmentosa. Acta Ophthalmol 2015;93(8):e644-e648.
12 Vingolo EM, Gerace E, Valente S, Spadea L, Nebbioso M. Microincision vitrectomy surgery in vitreomacular traction syndrome of retinitis pigmentosa patients. Biomed Res Int 2014;2014:537081.
13 Odrobina D, Michalewska Z, Michalewski J, Dzięgielewski K,Nawrocki J. Long-term evaluation of vitreomacular traction disorder in spectral-domain optical coherence tomography. Retina 2011;31(2):324-331.
14 Ando F, Yasui O, Hirose H, Ohba N. Optic nerve atrophy after vitrectomy with indocyanine green-assisted internal limiting membrane peeling in diffuse diabetic macular edema. Adverse effect of ICG-assisted ILM peeling. Graefes Arch Clin Exp Ophthalmol 2004;242(12):995-999.
Correspondenceto:Hyeong Gon Yu. Department of Ophthalmology, Seoul National University Hospital, Seoul National University College of Medicine, 101, Daehak-ro,Jongno-gu, Seoul 110-744, South Korea. hgonyu@snu.ac.kr
Received:2017-09-29 Accepted: 2018-03-01
Abstract● Retrospective review of 13 eyes that had undergone pars plana vitrectomy (PPV) for vitreomacular traction(VMT) syndrome in retinitis pigmentosa (RP) and had a postoperative follow-up period ≥9mo in order to evaluate whether it is necessary to treat VMT in RP by vitrectomy.The 13 RP eyes suffering from VMT were evaluated by means of best corrected visual acuity (BCVA), anterior and posterior binocular examination, spectral-domain optical coherence tomography (SD-OCT) before and after operation. We detected that although vitrectomy could improve the macular morphology in some RP patients with VMT, visual outcomes might be limited and unpredicted most likely because of the long-standing retinal dysfunction,but the vitrectomy is necessary in order to remain or improve the central vision in some cases.
● KEYWORDS:macular abnormalities; spectral-domain optical coherence tomography; pars plana vitrectomy; retinitis pigmentosa
DOl:10.18240/ijo.2018.08.25
Citation:Yan F, Xia FJ, Jiang F, Yu HG. Visual and morphological outcomes of vitreomacular traction syndrome in retinitis pigmentosa treated by vitrectomy. Int J Ophthalmol 2018;11(8):1411-1415