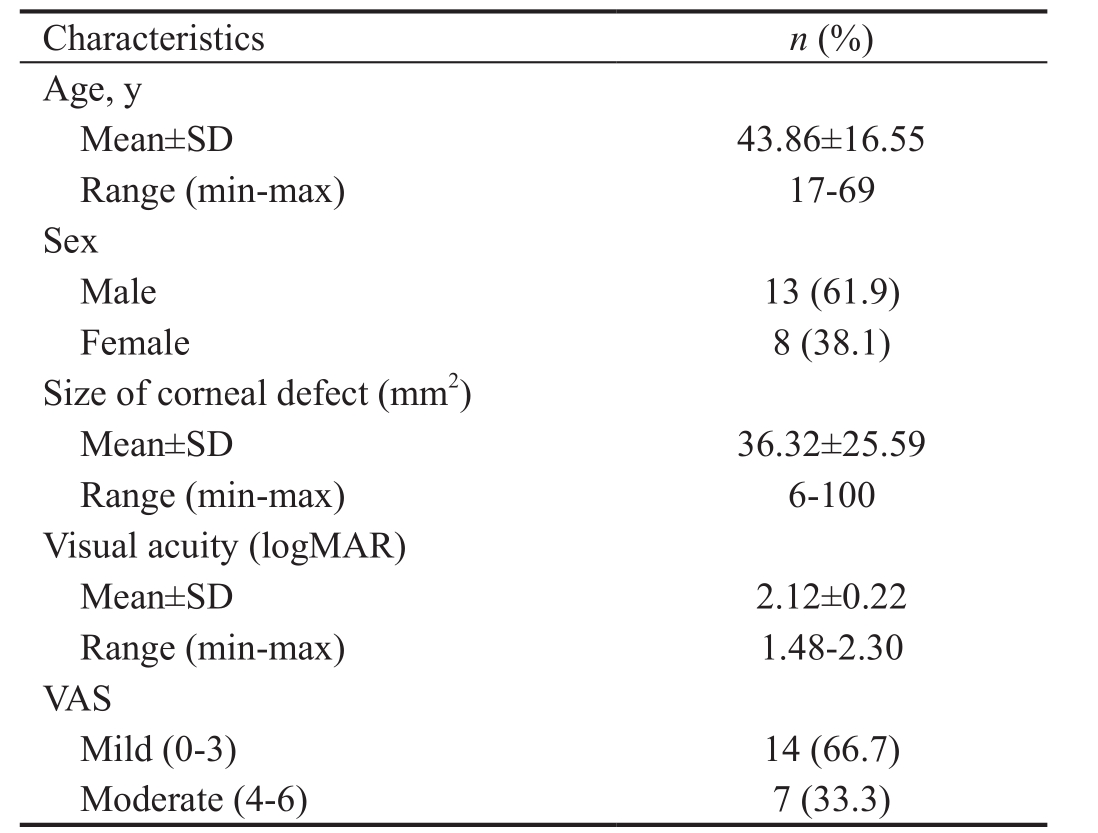
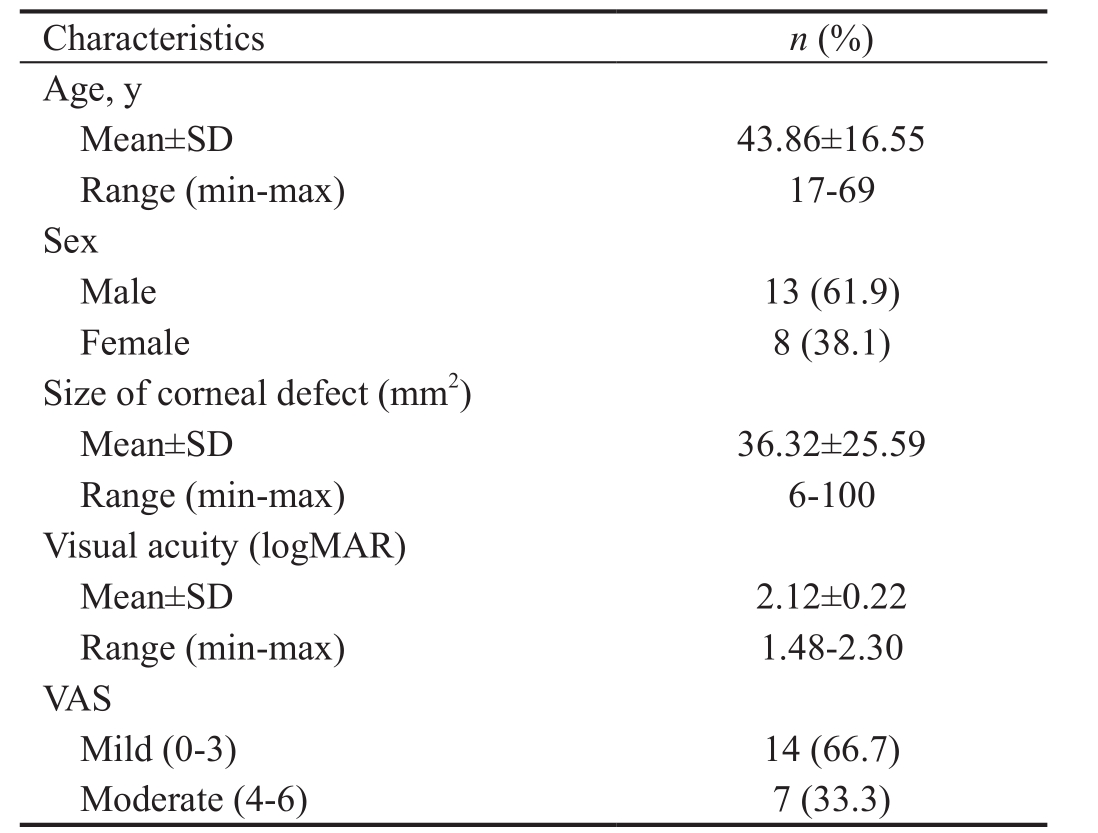
Table 1 Characteristics of the study subjects
IL-6: Interleukin-6; VAS: Visual analogue scale.
Marzarendra Dhion Erlangga1, Indra Tri Mahayana1, Jajah Fachiroh2, Angela Nurini Agni1, Agus Supartoto1,Suhardjo Pawiroranu1
1Department of Ophthalmology, Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada/Dr. Sardjito General Hospital, Yogyakarta 55284, Indonesia
2Department of Biomolecular and Cell Biology, Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada, Yogyakarta 55284, Indonesia
Corneal ulcer or ulcerative keratitis is an inflammatory condition involving disruption of the epithelial lining and corneal stroma. Characteristic of corneal ulcers is its rapid progression; delayed management can lead to blindness.Corneal destruction can occur completely within 24-48h in highly virulent bacterial infections[1-3].
The incidence of corneal ulcers in developed countries is 2-11/100 000 per year, and tends to increase due to the use of contact lenses. The incidence in developing countries is much higher. A retrospective study in South India showed that the incidence of corneal ulcers was 113/100 000 per year[4]. In
Nepal, the figure is estimated to reach 799/100 000 per year[5].
Bacterial keratitis is a vision-threatening and progressive condition; even with optimal management, the condition may still progress into ulceration, stromal abscess, even perforation.The difficulty in determining appropriate and effective antibiotic therapy leads to high rates of treatment failure.In cases of corneal ulcers that do not respond to antibiotic therapy, collagen cross-linking (CXL) is an adjuvant therapy option that promises good results[6-7].
In CXL, photoactivation of chromophores can have a disinfectant effect, resulting in reduced microbial counts. It is postulated that when light activates chromophore, there is intercalation between chromophore and nucleic acid from pathogens[8-10]. This leads to replication inhibition, thereby reducing the number of pathogens[7].
Immune responses and inflammatory processes in corneal ulcers are mediated by cytokines; interleukin-6 (IL-6) is one of the most common proinflamatory cytokines[11]. IL-6 is produced by corneal fibroblast cells around the site of injury.Increased IL-6 levels are associated with inflammatory processes, while decreased IL-6 levels are associated with improvements in inflammation and wound healing[12-13].
The purpose of this study was thus to investigate changes in IL-6 tear concentration and clinical conditions [such as size of corneal defect, descemetocele, logMAR visual acuity,visual analogue scale (VAS), blepharospasm, and conjunctival hyperemia] in patients with moderate-to-severe corneal ulcers which underwent CXL therapy.
SubjectsThis study used a pre-post design, involving 21 subjects with moderate-to-severe infectious bacterial corneal ulcers which underwent CXL during the study period at Dr. Sardjito General Hospital Yogyakarta; from January to June 2017. Patients with infectious corneal ulcer were given CXL therapy as adjunctive treatment after 5d broadspectrum antibiotic treatments (Ceftazidim and Vancomycin). The antibiotic treatment was then adjusted after the culture and antibiotic sensitivity test of corneal swab and scrapping was available (after 7d of treatment). The inclusion criteria in this study were all patients diagnosed wit moderate-to-severe bacterial corneal ulcers (moderate: 2-5 mm size and 20%-50%stromal depth; severe: size ˃5 mm and stromal depth ˃50%)indicated for CXL therapy; willing to do CXL therapy, willing to follow the research and signed the research informed consent sheet. Exclusion criteria in this study included patients who after CXL therapy refused to provide tear specimens as well as patients whose tear specimens were damaged or lost in the transport. Subjects who failed to follow the post CXL monitoring schedule were also excluded.
Data CollectionTear sampling was performed before (pre),1h after (peri) and 7d after (post) CXL therapy, using sterile Schimer paper, extracted from conjunctival inferior fornix. The primary outcome was IL-6 concentration in tears, obtained from ELISA results done at the Laboratory of Molecular Biology, Faculty of Medicine, Universitas Gadjah Mada,Indonesia. Clinical outcomes were size of corneal defects(clinically the ulcer size was observed 3 dimensionally,however for the objective data, the parameter was only 2 dimensional), presence of descemetocele, VAS, blepharospasm,and conjunctival hyperemia. The study followed the tenets of the Declaration of Helsinki. The Ethics Committee of the Faculty of Medicine, Universitas Gadjah Mada/Dr.Sardjito General Hospital approved the study protocol. After detailed explanation, informed consent was obtained from each patient prior to examination.
Table 1 Characteristics of the study subjects
IL-6: Interleukin-6; VAS: Visual analogue scale.
Statistical AnalysisStatistical analysis was performed using SPSS 22.0 for Windows software. Data were expressed as mean±standard deviation (SD) and range, normality of all data samples was first confirmed by the Kolmogorov-Smirnov test.Difference in subject research characteristics were analyzed using the Chi-square test for categorical data and unpaired t test for numerical data if the distribution was normal, or Mann-Whitney test if the distribution was not normal. Changes in IL-6 concentration, average size of corneal defects, and visual acuity after CXL were analyzed using Wilcoxon signedrank test. Changes in VAS, blepharospasm, and conjunctival hyperemia were analyzed using Chi-square test.
Characteristics of the study subjects are listed in Table 1.We found that there was a significant decrease in tear IL-6 concentration pre and post CXL therapy, with differences 2055.43±2396.61 pg/mL (P=0.001). There was no statistically significant decrease in IL-6 concentration pre and peri CXL therapy, with differences 93.08±1885.50 pg/mL (P=0.821;Table 2).
The mean size of corneal defects before and after CXL therapy also significantly reduced; pre CXL defect size was 36.32±25.59 mm2and post CXL was 26.42±20.32 mm2with differences is 9.90±14.37 mm2(P=0.007). The mean visual acuity (logMAR) before and after CXL therapy in this study was not found to change significantly (pre CXL: 2.12±0.22 vs post CXL: 2.06±0.26; P=0.277; Table 3). Similar results were also obtained in previous studies by Vajpayee et al[9], where the mean visual acuity (logMAR) of pre CXL and post CXL was not statistically significant (P=0.46). This might due to healing of the cornea that results in scarring, thus still obscuring the visual axis[14]. There was a significant decrease in VAS values pre CXL and post CXL (P=0.018; Table 4).
There was a statistically significant decrease in blepharospasm levels pre CXL and post CXL (P=0.011; Table 5).Blepharospasm and hyperemia levels reflect the general inflammatory sequelae of patients with corneal ulcers. Changes in conjunctival hyperemia inconsistent with the decreased IL-6 concentration post CXL may be attributed to the fact that IL-6 does not play a direct role in the mechanism of conjunctival hyperemia (Tables 6-7).
Table 2 Changes in IL-6 tears concentration after CXL
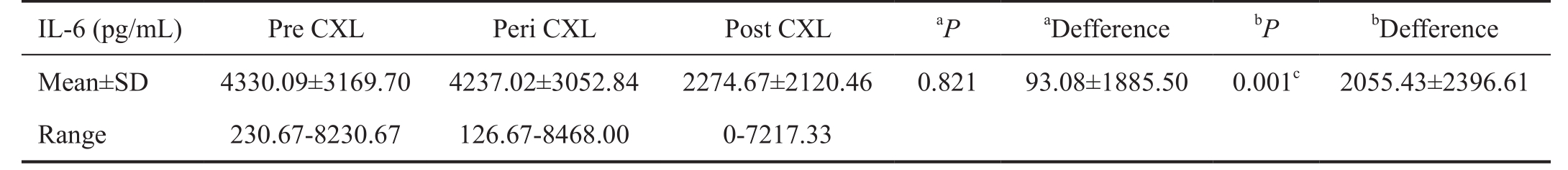
IL-6: Interleukin-6; CXL: Collagen cross-linking.aPre CXL vs Peri CXL;bPre CXL vs Post CXL;cP<0.05 (Mann-Whitney U test).
Table 3 Changes in average size of corneal defects and visual acuity, pre and post CXL
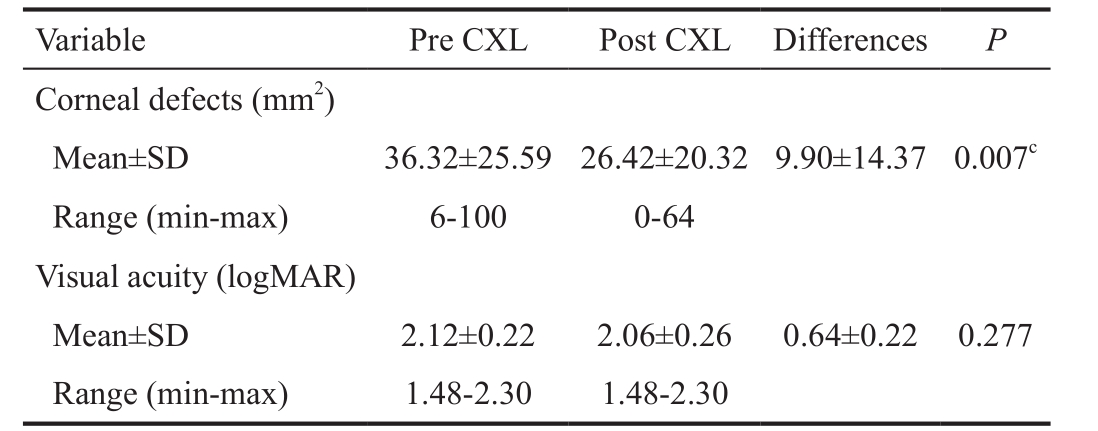
CXL: Collagen cross-linking.cP<0.05 (Mann-Whitney U test).
Table 4 Changes in VAS pre, peri, and post CXL n (%)
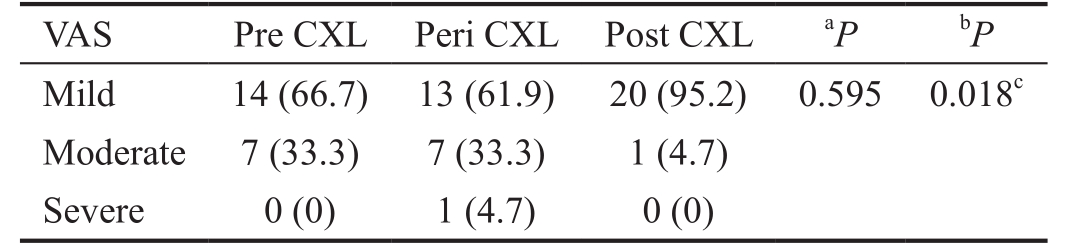
VAS: Visual analogue scale; CXL: Collagen cross-linking.aPre CXL vs Peri CXL;bPre CXL vs Post CXL;cP<0.05.
Table 5 Blefarospasm proportions pre and post CXL n (%)
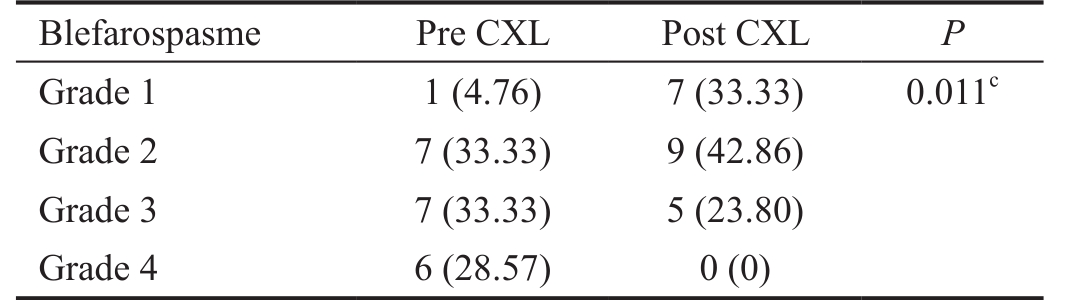
CXL: Collagen cross-linking.cP<0.05.
Table 6 Conjunctival hyperemia proportions pre and post CXL n (%)

CXL: Collagen cross-linking.
To our best knowledge, no previous studies have investigated tear IL-6 concentration differences pre and post CXL therapy.Our study demonstrates that CXL is accompanied by a significant reduction in IL-6 values. In a study assessing IL-6 concentration by Santacruz et al[15], the average IL-6 tearsconcentration in normal people was 25±17 pg/mL; whereas in subjects suffering from corneal ulcer, the concentration was 758±1166 pg/mL. Normal tears have very low concentration of IL-6[16]. Elevated concentration of IL-6 in tears are associated with its important role in the mechanism of inflammatory regulation[17-19].
Table 7 IL-6 tears concentration based on the presence of descemetocele condition

IL-6: Interleukin-6; CXL: Collagen cross-linking.aWith descemetocele vs no descemetocele;bStatistically significant; patients with descemetocele condition underwent transplantation of amnionic membrane after CXL.
In a report by Zamani et al[6], 8 eyes with bacterial keratitis underwent CXL, 2 (25%) of which required additional action in the form of penetrating keratoplasty and conjunctival flap.In a Meta-analysis of 12 CXL studies in infectious keratitis,with total number of 104 eyes, 90 experienced discontinuation of the corneal damaging process and the rest (n=14; 13.5%)had to undergo corneal transplantation[7]. Our study had a higher percentage of eyes experiencing descemetocele than in previous research results[6-7], likely due to the severity of the corneal ulcers included.
In the present study, the lower mean concentration of IL-6 post CXL were present in clinically improved end-conditions.A higher mean tear IL-6 concentration was present in patients with descemetocele. These results are consistent with the role of IL-6 in corneal infections; as cytokines that activate inflammatory cascades, they lead to inhibition of corneal stromal repair and corneal surface epithelialization[20].
Based on the results of this study it can be concluded that there is a significant reduction in tear IL-6 concentration in bacterial corneal ulcers which underwent CXL therapy. The exact mechanisms underlying these IL-6 changes remain unknown,this was paralled by clinical improvement in the corneal ulcer shown as decrease in size of corneal defects, VAS values, and blepharospasm levels in corneal ulcers which underwent CXL therapy.
Subsequent studies should better control the variables that may affect the results of IL-6 levels during the follow-up process. In addition, it is necessary to conduct an experimental study by including a control group not treated by CXL, to determine the magnitude of the change in IL-6 levels as a comparison. Subsequent studies should also observe other clinical parameters such as ulcer depth, infiltration degree, and other potential modulators of IL-6 levels. In addition, other inflammatory biomarkers such as IL-1, IL-8, and TNF-α may be examined for levels in CXL-treated corneal ulcers.
Conflicts of Interest:Erlangga MD, None; Mahayana IT,None; Fachiroh J, None; Agni AN, None; Supartoto A,None; Pawiroranu S, None.
REFERENCES
1 Tabibian D, Mazzotta C, Hafezi F. PACK-CXL: corneal cross-linking in infectious keratitis. Eye Vis (Lond) 2016;3:11.
2 Tabibian D, Richoz O, Hafezi F. PACK-CXL: corneal cross-linking for treatment of infectious keratitis. J Ophthalmic Vis Res 2015;10(1):77-80.
3 Micelli Ferrari T, Leozappa M, Lorusso M, Epifani E, Micelli Ferrari L. Escherichia coli keratitis treated with ultraviolet A/riboflavin corneal cross-linking: a case report. Eur J Ophthalmol 2009;19(2):295-297.
4 Gupta N, Tandon R, Gupta SK, Sreenivas V, Vashist P. Burden of corneal blindness in India. Indian J Community Med 2013;38(4):198-206.
5 Al-Mujaini A, Al-Kharusi N, Thakral A, Wali UK. Bacterial keratitis:perspective on epidemiology, clinico-pathogenesis, diagnosis and treatment. Sultan Qaboos Univ Med J 2009;9(2):184-195.
6 Zamani M, Panahi-Bazaz M, Assadi M. Corneal collagen crosslinking for treatment of non-healing corneal ulcers. J Ophthalmic Vis Res 2015;10(1):16-20.
7 Alio JL, Abbouda A, Valle D, del Castillo JM, Fernandez JA. Corneal cross linking and infectious keratitis: a systematic review with a metaanalysis of reported cases. J Ophthalmic Inflamm Infect 2013;3(1):47.
8 Tal K, Gal-Or O, Pillar S, Zahavi A, Rock O, Bahar I. Efficacy of primary collagen cross-linking with photoactivated chromophore (PACKCXL ) for the treatment of staphylococcus aureus-induced corneal ulcers.J Cornea Extern Dis 2015;34(10):1281-1286.
9 Vajpayee RB, Shafi SN, Maharana PK, Sharma N, Jhanji V. Evaluation of corneal collagen cross-linking as an additional therapy in mycotic keratitis. Clin Exp Ophthalmol 2015;43(2):103-107.
10 Mastropasqua L. Collagen cross-linking: when and how? A review of the state of the art of the technique and new perspectives. Eye Vis (Lond)2015;2(2015):19.
11 Hosseini RH. Evaluation of IL-6 and IL-8 in tear fluid of sulfur mustard gas-exposed patients with eye lesions. OALib 2014;1(5):1-6.
12 Higuchi A, Kawakita T, Tsubota K. IL-6 induction in desiccated corneal epithelium in vitro and in vivo. Mol Vis 2011;17:2400-2406.
13 Ebihara N, Matsuda A, Nakamura S, Matsuda H, Murakami A.Role of the IL-6 classic- and trans-signaling pathways in corneal sterile inflammation and wound healing. Invest Opthalmol Vis Sci 2011;52(12):8549-8557.
14 Eraslan M, Toker E. Mechanisms of corneal wound healing and its modulation following refractive surgery. Marmara Med J 2009;22(2):169-178.
15 Santacruz C, Linares M, Garfias Y, Loustaunau L, Pavon L, Perez-Tapia S, Jimenez-Martinez M. Expression of IL-8, IL-6 and IL-1β in tears as a main characteristic of the immune response in human microbial keratitis. Int J Mol Sci 2015;16(3):4850-4864.
16 Carreño E, Enríquez-de-Salamanca A, Tesón M, García-Vázquez C,Stern ME, Whitcup SM, Calonge M. Cytokine and chemokine levels in tears from healthy subjects. Acta Ophthalmol 2010;88(7):e250-e258.
17 Sugaya S, Sakimoto T, Shoji J, Sawa M. Regulation of soluble interleukin-6 (IL-6) receptor release from corneal epithelial cells and its role in the ocular surface. Jpn J Ophthalmol 2011;6(55):277-282.
18 Weiss TW, Arnesen H, Seljeflot I. Components of the interleukin-6 transsignalling system are associated with the metabolic syndrome,endothelial dysfunction and arterial stiffness. Metab Clin Exp 2013;62(7):1008-1013.
19 Velasco F, Vidaurri-leal J, Arce AY, Morales C, García-rojas M.Proinflammatory cytokines level in the tear film after corneal surface surgery. Med Univ 2012;14(54):3-10.
20 Yamaguchi T, Calvacanti BM, Cruzat A, Qazi Y, Ishikawa S, Osuka A,Lederer J, Hamrah P. Correlation between human tear cytokine levels and cellular corneal changes in patients with bacterial keratitis by in vivo confocal microscopy. Invest Ophthalmol Vis Sci 2014;55(11):7457-7466.
Correspondenceto:Agus Supartoto. Department of Ophthalmology, Faculty of Medicine, Universitas Gadjah Mada/Dr.Sardjito General Hospital, Jl. Farmako, Sekip Utara,Yogyakarta 55284, Indonesia. agus.supartoto2015@gmail.com;agus.supartoto@ugm.ac.id
Received:2017-07-20 Accepted: 2018-01-23
Abstract● We aimed to evaluate interleukin-6 (lL-6) tear concentration and clinical outcome in patients with moderate-to-severe bacterial corneal ulcers post corneal collagen cross-linking(CXL) therapy. This pre-post designed study involving 21 moderate-to-severe corneal ulcer patients who underwent CXL therapy. Patients with infectious corneal ulcer were given CXL therapy as adjunctive treatment after 5d of broadspectrum antibiotic treatment. Patients with moderate to severe infectious bacterial corneal ulcers were included in this study. Tear sampling was performed before CXL therapy, using sterile Schimer paper from conjunctival inferior fornix. CXL therapy was performed in accordance with the CXL Dresden protocol. Data recording and tear sampling were then performed at day 1 and day 7 after CXL therapy. Data recording included, presence of conjunctival hyperemia, visual analogue scale (VAS),size of corneal defects, and decemetocele. There was a decrease in lL-6 tear concentration by day 7 after CXL therapy (P=0.001). lL-6 concentration at 1h after therapy(2274.67±2120.46 pg/mL) tended to be lower than before therapy (4330.09±3169.70 pg/mL), but the difference was not statistically significant (P=0.821). The size of corneal defects decreased significantly post CXL (P=0.007). The logMAR visual acuity before and after CXL therapy was not found to be significantly different (P=0.277). There was a significant decrease in VAS values (P=0.018) and blepharospasm (P=0.011) pre and post CXL. There was no significant decrease in conjunctival hyperemia pre and post CXL (P=0.293). There was significant reduction in lL-6 tear concentration and clinical improvement in moderateto-severe bacterial corneal ulcers which underwent CXL therapy.
● KEYWORDS:corneal ulcers; bacterial keratitis; collagen cross-linking; interleukin-6
DOl:10.18240/ijo.2018.08.27
Citation:Erlangga MD, Mahayana IT, Fachiroh J, Agni AN, Supartoto A,Pawiroranu S. Changes in interleukin-6 tear concentration and clinical outcome in moderate-to-severe bacterial corneal ulcers after corneal collagen cross-linking. Int J Ophthalmol 2018;11(8):1421-1424