A challenging case of tuberculosis-associated uveitis after corticosteroid treatment for Vogt-Koyanagi-Harada disease
Tian-Wei Qian1,2, Su-Qin Yu1,2, Xun Xu1,2
1Department of Ophthalmology, Shanghai General Hospital,Shanghai 200080, China
2Shanghai Key Laboratory of Ocular Fundus Diseases,Shanghai 200080, China
Dear Editor,
I am Dr. Tian-Wei Qian, from Shanghai General Hospital,Shanghai, China. I write to present one case report of tuberculosis (TB)-associated uveitis after corticosteroid treatment for Vogt-Koyanagi-Harada (VKH) disease. VKH disease, caused by an autoimmune response, is a multisystemic disorder, often associated with neurologic and cutaneous manifestations in certain populations[1]. It is characterized by granulomatous panuveitis with iridocyclitis,exudative retinal detachments, diffuse choroidal swelling,and optic disc hyperemia[2]. Prognosis may be improved by the timely use of high-dose corticosteroids during the acute phase. TB, caused by mycobacterium TB, is another disease that can cause multi-systemic granulomatous inflammation,probably involving the eye, and requires anti-tubercular therapy. We report a challenging case of TB-associated uveitis after corticosteroid therapy for VKH disease. In this case,the diagnosis and treatment were challenging because VKH disease and TB can share the similar manifestation of uveitis but require different treatments.
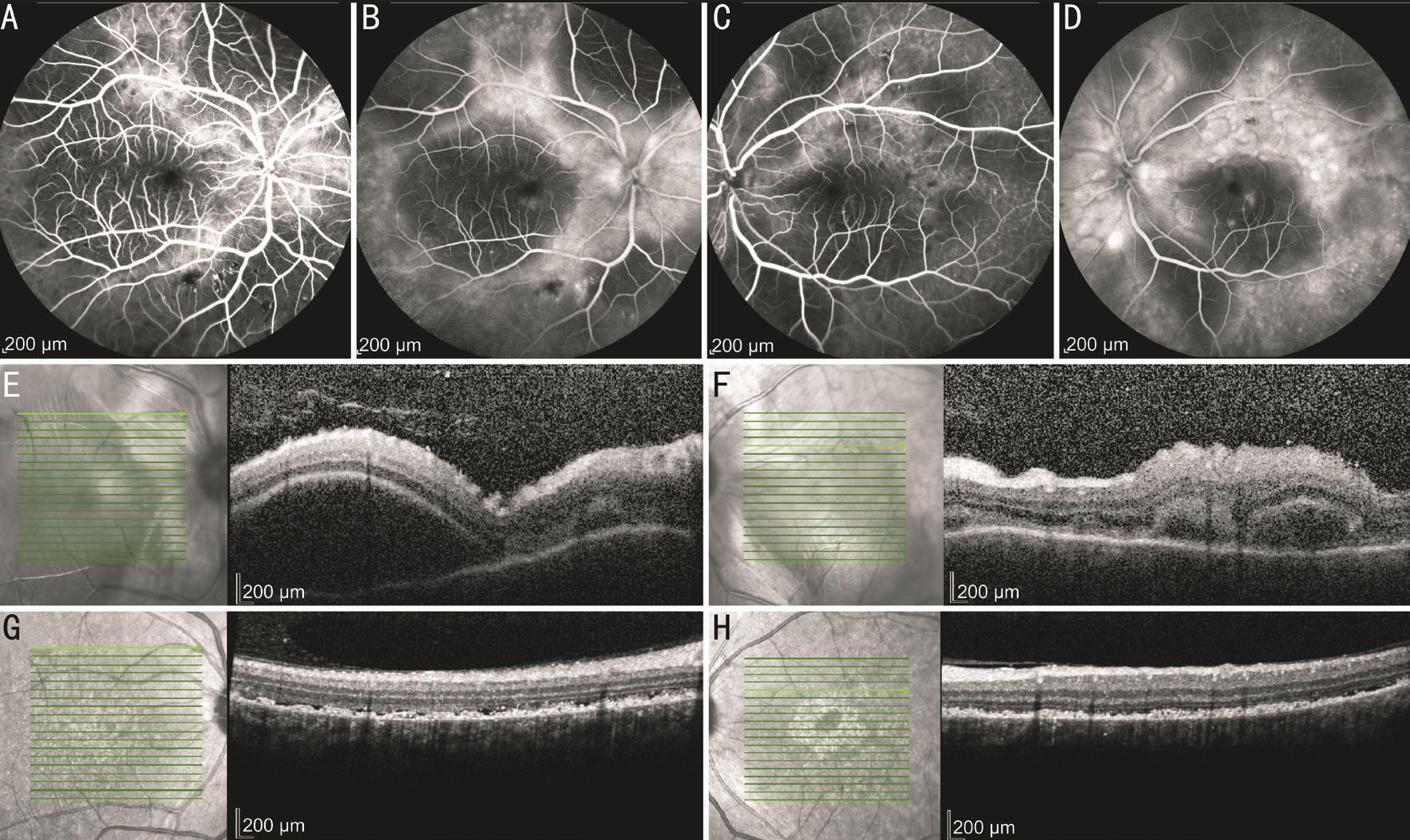
A 52-year-old man presented with sudden vision loss in both eyes for 1wk associated with frontal headache and occasional tinnitus on Nov. 25, 2014. The patient denied history of eye trauma or surgery. His best-corrected visual acuity (BCVA)was finger counting in both eyes. Anterior segments were normal at that time. Fundus fluorescein angiography (FFA)revealed angiographic features typical of VKH disease in both eyes (Figure 1A-1D): multifocal leakage in the early stage,pooling and dye leakage in the subretinal space in the late stage of the angiogram, and serous detachments with late pooling of dye. Optical coherence tomography (OCT) showed exudative retinal detachment with subretinal septa at the posterior pole(Figure 1E, 1F) in both eyes.
One week after administration of oral metacortandracin (initial dose of 1.2 mg/kg·d), his vision improved to 20/200 in the right eye and 20/100 in the left eye. The dosage was then tapered gradually (10 mg every week until 20 mg/d, then 5 mg every month) with continuous improvements in BCVA. At the 3-month visit post initial treatment, his BCVA returned to 20/30 in both eyes. In addition, subretinal fluid was obviously absorbed (Figure 1G, 1H).
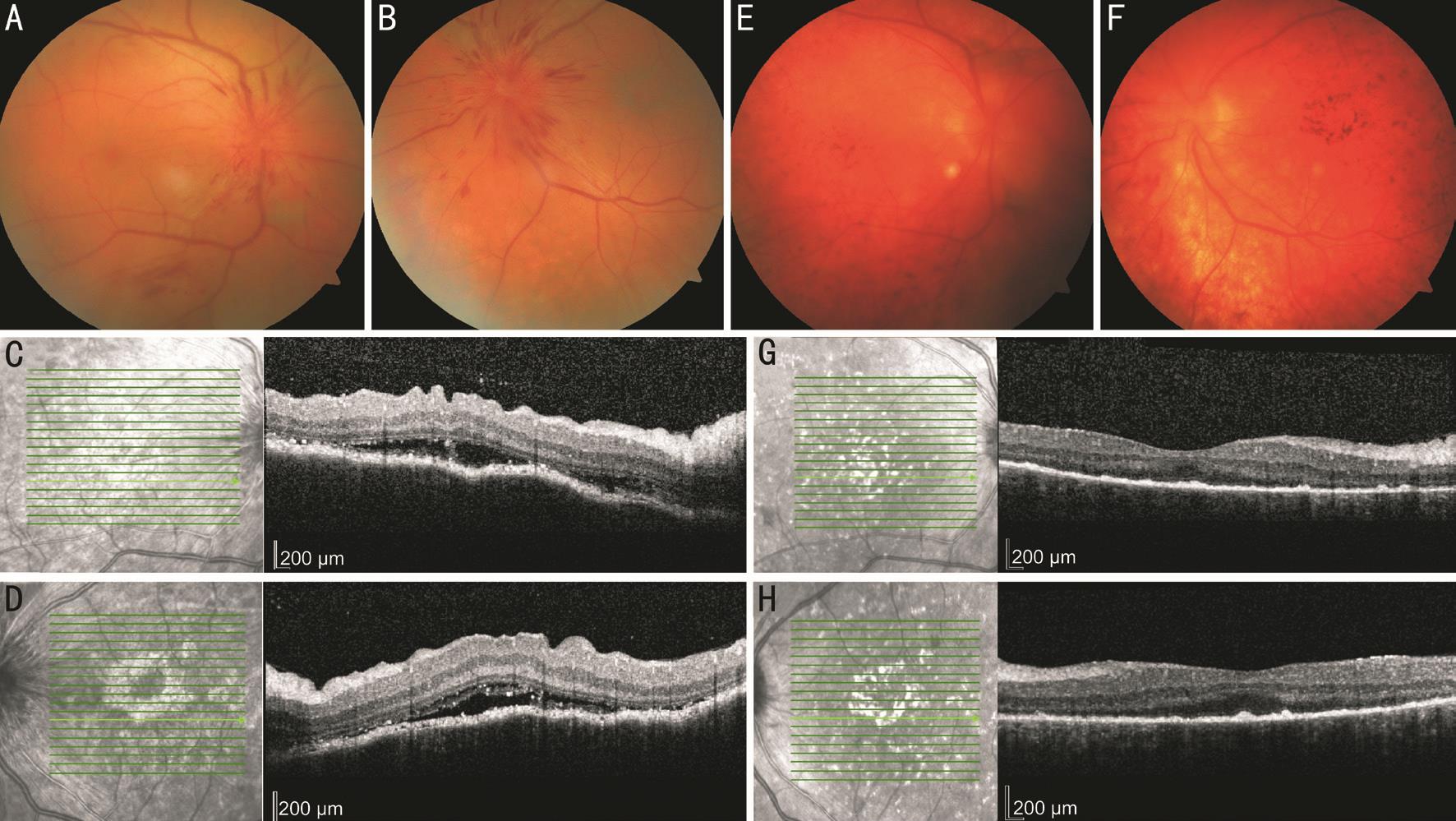
However, at the 105-day visit, the patient experienced another sudden decrease in vision to 20/60 with ciliary hyperemia and aqueous flare. Color fundus photography (FP) and OCT images showed papilledema with re-accumulation of subretinal fluid around the disc and radial linear hemorrhage in both eyes (Figure 2A-2D). Laboratory examinations for potential infectious diseases were also performed and showed positive T-SPOT®.TB results (ESAT-6 antigen was 23, CFP-10 antigen was 45). Chest radiograph revealed manifestation of pulmonary TB.
Therefore, the patient was suspected to have TB-associated uveitis and was administered anti-TB treatment (combined medication of isoniazid, rifampicin, and pyrazinamide).Anterior chamber inflammatory reaction occurred and his BCVA decreased to 20/150 in both eyes. Since the papilledema responded to anti-TB therapy relatively well, the treatment was continued. Various eye drops (prednisolone acetate ophthalmic suspension, diclofenac sodium eye drops, and tropicamide phenylephrine eye drops) were administered to control the anterior chamber reaction, which subsequently disappeared.
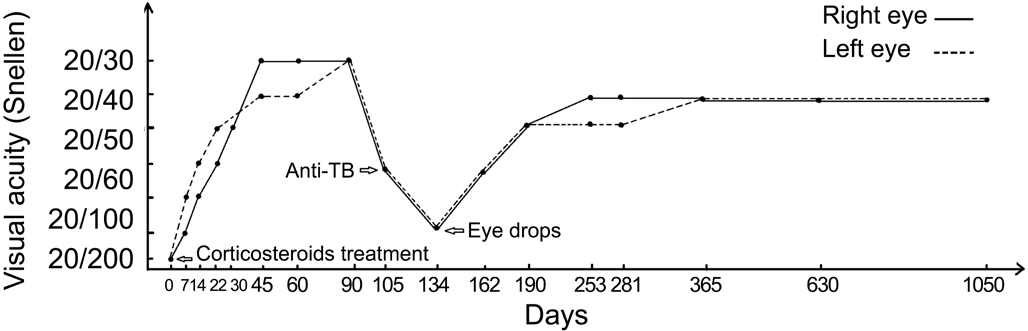
During 6mo of regular follow-up after the completion of anti-TB treatment, the patient developed “sunset glow” fundus(Figure 2E, 2F). OCT showed complete reabsorption of subretinal fluid as well as normal retinal thicknesses (Figure 2G, 2H). Binocular BCVA steadily increased to 20/50, and the immune index decreased to normal compared with the previous outcomes. However, 1y later, the patient experienced another anterior chamber reaction but with a flat retina. It was controlled again with local anti-inflammatory eye drops. The patient was followed-up for another 2y; his situation stabilized with a BCVA of 20/40 in both eyes. Visual acuity changes during the course of the disease in both eyes are shown in Figure 3.
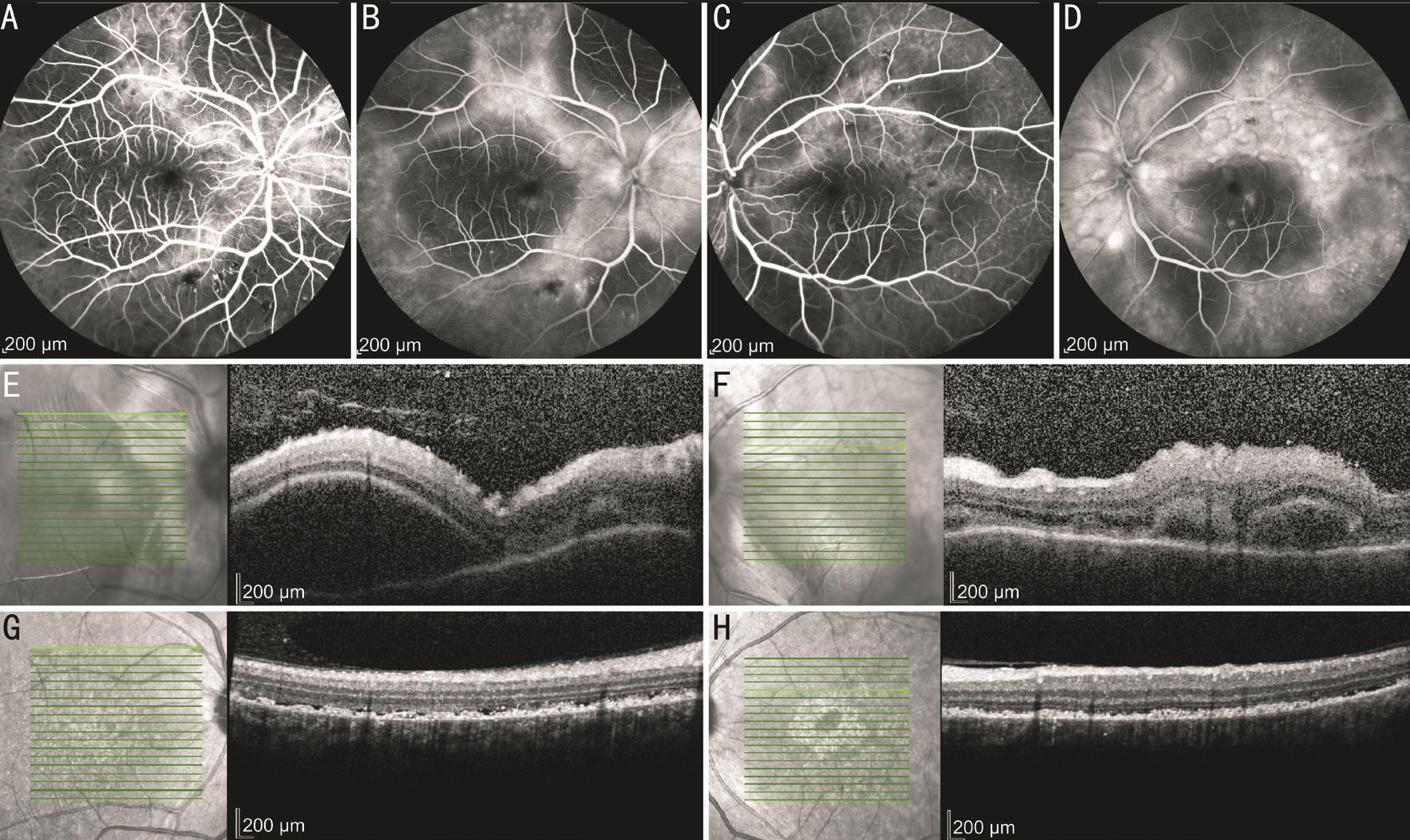
Figure 1 FFA and OCT examination results of the patient A, B, E, G: Right eye; C, D, F, H: Left eye. FFA showed multifocal leakage in the early phase (A, C), and pooling in the late phase (B, D) in both eyes at presentation. OCT showed neurosensory layer detachment with subretinal septae (E, F) and after corticosteroids treatment the subretinal fluid was completely absorbed in both eyes (G, H).
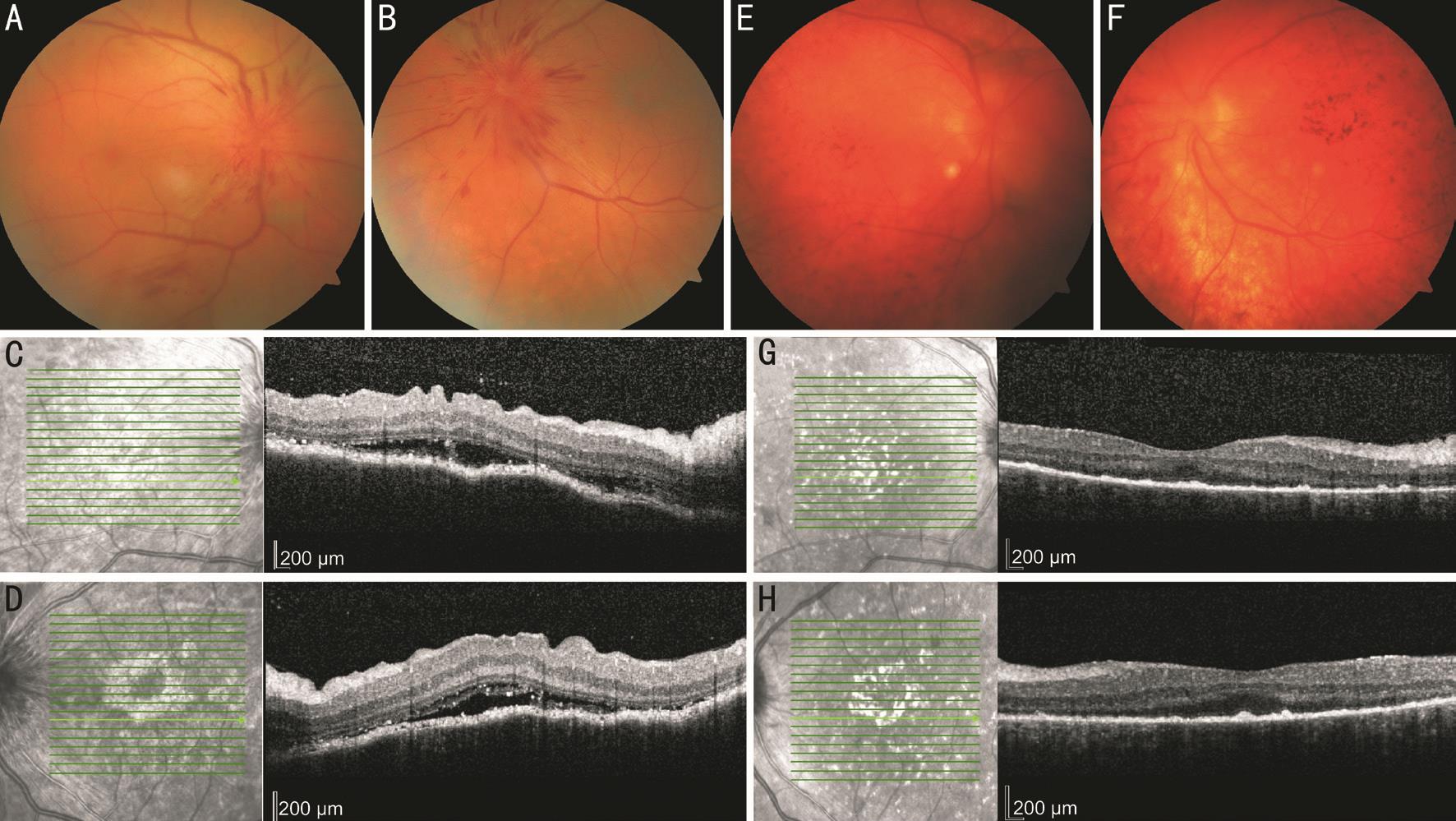
Figure 2 FP and OCT examination of the patient A, C, E, G: Right eye; B, D, F, H: Left eye. Color FP at the visit of the fifth month showed papilledema and radial linear hemorrhage bilateral (A, B) and re-accumulation of subretinal fluid around disc on OCT (C, D). After anti-TB treatment, papilledema and hemorrhage disappeared. The development of “sunset glow” fundus with pigmentation could be seen on photography(E, F) and flat retina was presented on OCT (G, H) in both eyes.
We presented a challenging case of TB-associated uveitis after corticosteroid therapy for VKH disease. The diagnosis and treatment were both challenging because VKH disease and TB can share the similar manifestation of uveitis but require different treatments. The patient was initially diagnosed with VKH disease on the basis of his clinical features and multimodal imaging according to the revised diagnostic criteria for VKH disease[3], which has also shown to be useful for the diagnosis of Chinese patients with VKH disease[4].It was reported that atypical manifestation of tuberculous uveitis could imitate VKH disease[5]; however, the diagnosis of our case was beyond doubt due to several reasons. First, the patient had typical precursory symptoms of VKH. Second, he did not have a history of penetrating ocular trauma or surgery,eliminating sympathetic ophthalmia. Third, he exhibited typical clinical features and characteristic images of VKH disease on FFA and OCT. Finally, the patient responded to oral steroid treatment very well with quick absorption of subretinal fluid and vision improvement.
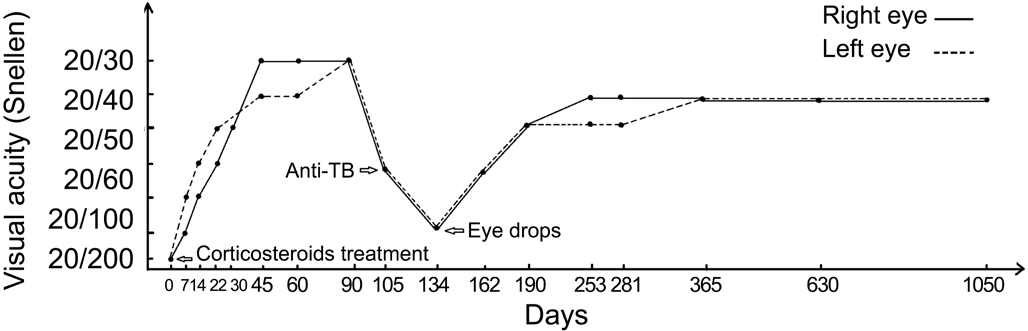
Figure 3 Visual acuity changes in both eyes during about 3y follow-up period The straight line represents visual changes in the right eye while the dotted line represents changes in the left eye.
Almost after 105d of steroid tapering, the patient developed another episode of optic disc swelling with re-decreased vision in both eyes. Treatment selection presented a dilemma because it was not clear if the patient had VKH disease recurrence.Positive T-SPOT®.TB test results and chest radiographs confirmed that the patient exhibited an active stage of TB infection and that eye condition deterioration was due to TB-associated uveitis. Moreover, the improvement of retinal condition after anti-TB treatments also corroborated the diagnostic accuracy.
Corticosteroid treatment has been the mainstay therapeutic strategy for VKH disease for several decades[6-8]. Systemic corticosteroids are considered to control active inflammation and prevent new inflammatory episodes, preventing recurrence of the disease, and minimizing the incidence and severity of extraocular manifestations[2]. However, corticosteroids drugs have the pharmacological effect of immunosuppression,resulting in decreased immune function of the patient. The patient may be a mycobacterium TB carrier, and decreased immunity may activate TB and induce TB-associated uveitis.Furthermore, the results of a case-control study of TB by Jick et al[9]indicated that patients treated with glucocorticoids had an increased risk of developing TB. Prolonged therapy with moderate- or high-dose corticosteroids could increase the risk of TB reactivation[10]. The Centers for Disease Control and Prevention and the American Thoracic Society identified prednisone 15 mg daily for 1mo as the threshold for increased risk of TB recurrence[11-12].
Corticosteroid drugs are considered to have many benefits in clinical practice; however, their immunosuppression effect and the fact that TB is still regarded as one of the main causes of uveitis must be considered, especially in patients using immunosuppressive agents.
In conclusion, we present a case of TB-associated uveitis induced by corticosteroid treatment for VKH disease. We meet two challenging choices in diagnosis and treatment in this case. Steroids are the mainstay treatment for VKH disease,but are disadvantaged by immunosuppression, and may induce infectious diseases such as TB. Multimodal imaging may assist in differential diagnosis, and blood tests may provide additional information regarding potential infection.Furthermore, it must be considered that TB is still regarded as one of the main causes of uveitis, especially in patients taking immunosuppressive agents.
ACKNOWLEDGEMENTS
Conflicts of Interest: Qian TW, None; Yu SQ, None; Xu X,None.
REFERENCES
1 Du L, Kijlstra A, Yang P. Vogt-Koyanagi-Harada disease: novel insights into pathophysiology, diagnosis and treatment. Prog Retin Eye Res 2016;52:84-111.
2 Neves A, Cardoso A, Almeida M, Campos J, Campos A, Castro Sousa JP. Unilateral Vogt-Koyanagi-Harada disease: a clinical case report. Case Rep Ophthalmol 2015;6(3):361-365.
3 Read RW, Holland GN, Rao NA, Tabbara KF, Ohno S, Arellanes-Garcia L, Pivetti-Pezzi P, Tessler HH, Usui M. Revised diagnostic criteria for Vogt-Koyanagi-Harada disease: report of an international committee on nomenclature. Am J Ophthalmol 2001;131(5):647-652.
4 Yang P, Ren Y, Li B, Fang W, Meng Q, Kijlstra A. Clinical characteristics of Vogt-Koyanagi-Harada syndrome in Chinese patients. Ophthalmology 2007;114(3):606-614.
5 Kalogeropoulos D, Kitsos G, Konstantinidis A, Gartzonika C, Svarna E, Malamos K, Katsanevakis E, Kalogeropoulos C. Tuberculous posterior sclero-uveitis with features of Vogt-Koyanagi-Harada uveitis: an unusual case. Am J Case Rep 2017;18:367-374.
6 Moorthy RS, Inomata H, Rao NA. Vogt-koyanagi-harada syndrome.Surv Ophthalmol 1995;39(4):265-292.
7 Read RW, Yu F, Accorinti M, et al. Evaluation of the effect on outcomes of the route of administration of corticosteroids in acute Vogt-Koyanagi-Harada disease. Am J Ophthalmol 2006;142(1):119-124.
8 Latronico ME, Rigante D, Caso F, Cantarini L, Costa L, Nieves-Martín L, Traversi C, Franceschini R. Bilateral dexamethasone intravitreal implant in a young patient with Vogt-Koyanagi-Harada disease and refractory uveitis. Clin Rheumatol 2015;34(6):1145-1148.
9 Jick SS, Lieberman ES, Rahman MU, Choi HK. Glucocorticoid use,other associated factors, and the risk of tuberculosis. Arthritis Rheum 2006;55(1):19-26.
10 Caplan A, Fett N, Rosenbach M, Werth VP, Micheletti RG. Prevention and management of glucocorticoid-induced side effects: a comprehensive review: infectious complications and vaccination recommendations. J Am Acad Dermatol 2017;76(2):191-198.
11 Bovornkitti S, Kangsadal P, Sathirapat P, Oonsombatti P. Reversion and reconversion rate of tuberculin skin reactions in correlation with the use of prednisone. Dis Chest 1960;38(1):51-55.
12 Schatz M, Patterson R, Kloner R, Falk J. The prevalence of tuberculosis and positive tuberculin skin tests in a steroid-treated asthmatic population.Ann Intern Med 1976;84(3):261-265.
Correspondenceto:Su-Qin Yu. Department of Ophthalmology,Shanghai General Hospital, No.100, Haining Road, Shanghai 200080, China. sq-yu@163.com
Received:2018-02-23 Accepted: 2018-05-25
DOl:10.18240/ijo.2018.08.29
Citation:Qian TW, Yu SQ, Xu X. A challenging case of tuberculosisassociated uveitis after corticosteroid treatment for Vogt-Koyanagi-Harada disease. Int J Ophthalmol 2018;11(8):1430-1432