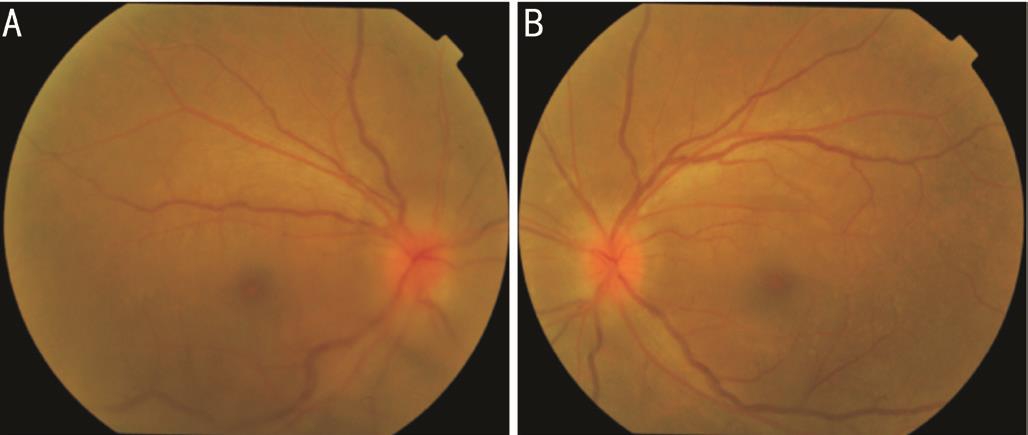
Figure 1 Bilateral hyperaemic and swollen optic disc with mild vitritis.
Mushawiahti Mustapha, Zakaria Abdollah, Amin Ahem, Hazlita Mohd Isa, Mae-Lynn Catherine Bastion,Norshamsiah Md Din
Department of Ophthalmology, Pusat Perubatan Universiti,Jalan Yaacob Latiff, Cheras 56000, Malaysia
Syphilis is a spirochaetal bacterial sexually transmitted disease (STD) caused by Treponema pallidum . Outbreaks of syphilis have been described in Western communities,especially in men who have sex with men (MSM) and people infected with human immunodeficiency virus (HIV) [1] . Reports of the condition from Asian countries remains limited, this is partly due to the topic of STD being still somehow taboo to a conservative Asian community, much to its detriment.
The resurgence of syphilis has resulted in an increase in the number of reported cases of ocular syphilis [2] . Known as the“Great Masquerader”, ocular syphilis has the potential to mimic a variety of ocular diseases, most commonly uveitis,but also interstitial keratitis, chorioretinitis, retinitis, retinal vasculitis and optic and cranial neuropathies [1] .
Syphilis is an important facilitator of HIV transmission with reported co-infection rates of 50%-70%. The presence of HIV may alter the presentation of syphilis, with possibly a more rapid progression to neurosyphilis [3] . Both conditions not surprisingly co-exist given both are STDs. Syphilis being a curable disease, awareness of its presentation and a high index of suspicion are paramount as prompt treatment can halt disease progression and prevent permanent visual loss.
Unfortunately, the data for syphilis in Malaysia was rather limited as under-reporting was prevalent and the general lack of local scientific literature in this field. Available reports indicated that the rate of notification of syphilis fluctuated between 9% and 11% from 1990 to 1999 and the prevalence was higher in sex workers [4] . There was also a reported decline in the rate of syphilis from 7.68 per 100 000 people in 2000 to 2.76 per 100 000 in 2006 [5] . Cultural trends may be contributing to an increase in the number of high-risk sexual behaviours,including MSM, which are subsequently increasing the rate of STD’s, particularly HIV and syphilis.
We report 4 cases of ocular syphilis with HIV co-infection in y oung adult males, who reported previous MSM behaviour that we encountered during the period between February to May 2017. The informed consents were obtained from all of patients and the treatment was conducted in accordance with the tenets of the Declaration of Helsinki.
A 27-year-old male presented to a private ophthalmologist complaining of bilateral blurring of vision for 1mo duration,worse on the right. It was associated with floaters, glare and reduced night vision. He was referred to our center for further management after treatment with topical steroids failed to alleviate his signs and symptoms. His visual acuity was 6/18 OD and 6/9 OS. Slit lamp biomicroscopy revealed bilateral anterior chamber cells of 2+ and fine white keratic precipitates (KPs) inferiorly. There was anterior vitreous cells of 2+ bilaterally. Fundus examination revealed bilateral vitritis 1+, hyperemic, swollen optic discs and dilated vessels.There were multiple areas of small vitreous condensations inferiorly in his right eye. No retinitis and choroiditis was seen(Figure 1). Confrontation visual field revealed enlarged blind spot. However, there was no relative afferent pupillary defect(RAPD). Other comprehensive, systemic physical examination revealed cervical lymphadenopathy and a painless penile ulcer.No skin rashes were observed. No neurological abnormalities elicited.
CT brain was done to rule out intracranial space occupying lesion and it was normal. An infectious panel revealed serum rapid plasma reagin (RPR) titre of 1:1024, as well as positive Treponema pallidum IgG and IgM. He also consented to HIV Western blot confirmatory test which was positive. Human immunodeficiency virus viral load was 81 234 copies/mm 3 ,and CD4 count was 178 cells/mm 3 . Other abnormal laboratory results include erythrocyte sedimentation rate (ESR) 130 mm/h and C-reactiomprotein (CRP) 32.7. Lumbar puncture was not performed. Epstein-Barr virus (EBV), cytomegalovirus (CMV)and toxoplasmosis serologies were negative.
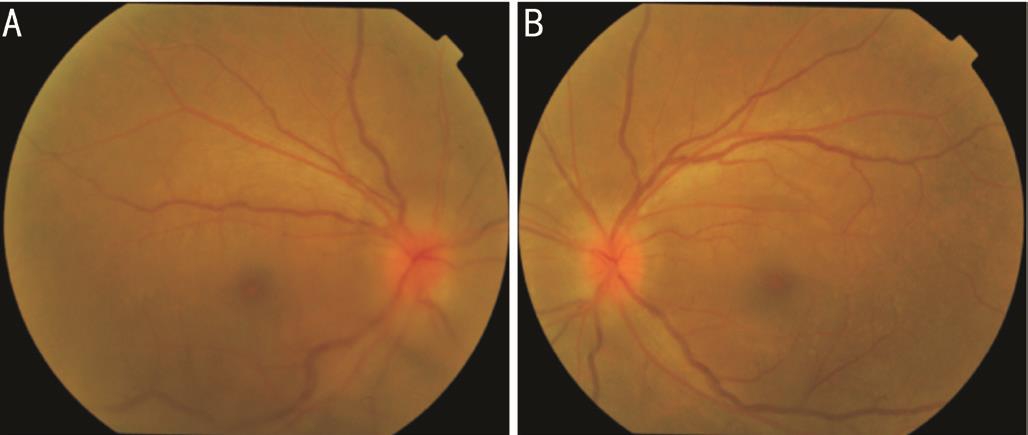
Figure 1 Bilateral hyperaemic and swollen optic disc with mild vitritis.
A diagnosis of ocular syphilis with HIV co-infection was made. Patient was co-managed with an infectious disease (ID)physician. He was admitted and treated with 24 million units(MU) of aqueous crystal penicillin G per day, administered as 4 MU intravenously over 4h for 14d. Oral prednisolone therapy was also prescribed at 50 mg per day for 2wk followed by tapering dose. One day after starting the penicillin treatment, he developed a fever, presumed secondary to a Jarisch-Herxheimer reaction but it resolved spontaneously.
Sexual history enquiries made revealed previous MSM behavior with multiple male sexual partners for the last 1y.After a 14-day course of intravenously penicillin therapy,his vision improved to 6/6 OU and continued to be the same at last follow-up 2mo later. He also received intramuscular benzathine penicillin 2.4 MU weekly for 3wk and highly active antiretroviral therapy (HAART) was started later by the ID physician during his subsequent outpatient follow-up.
A 24-year-old male presented with 2wk history of floaters and acute painless progressive loss of central vision in his right eye 5d prior to presentation to a private ophthalmologist. He denied metamorphopsia or seeing curtain over his field of vision. He had myopia corrected with spectacles since the age of 12y. He was diagnosed to have right eye rhegmatogenous retinal detachment and left eye retinal tear. Laser retinopexy of the retinal tear was performed in the left eye and he was subsequently referred to our center for the management of right retinal detachment.
Upon referral to our ophthalmology clinic, his visual acuity was 2/60 OD and 6/12 OS with positive RAPD OD. Slit lamp biomicroscopy revealed anterior chamber activity of 1+OD and occasional cells OS. Right eye fundus examination revealed a horseshoe tear at 11 o’clock, inferior retinal break at 6 o’clock and inferior bullous retinal detachment with macula off. Left eye fundus examination revealed inferior lattice degeneration and barricaded retinal tear. He subsequently underwent right trans pars plana vitrectomy with silicon oil tamponade on the following day.
Three months later, he underwent removal of silicon oil and insertion of Densiron-68 ® (Fluoron GmbH, Neu-Ulm,Germany) for retro-oil proliferative vitreoretinopathy (PVR).His best corrected visual acuity was 6/18 OD, 6/12 OS.
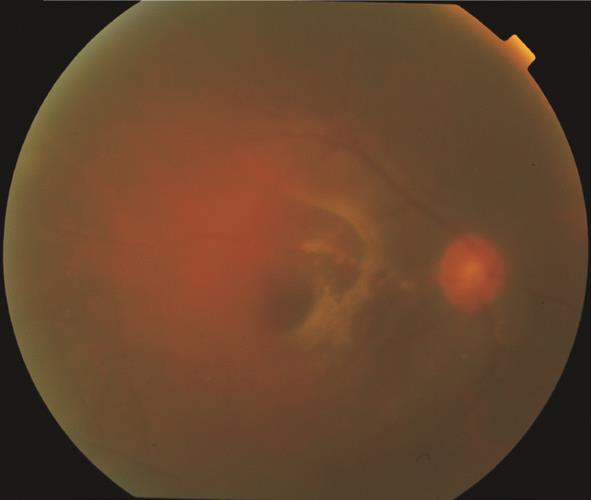
Figure 2 Right fundus showing mild vitritis and retinal fibrosis at posterior pole.
However, during subsequent follow-up, slit lamp examination revealed persistent anterior chamber activity of 2-3+ in both eyes. There were no KPs, or iris nodules seen. Fundus examination revealed bilateral hyperemic optic discs, vitritis and vascular sheathing. On repeated questioning, he revealed MSM behavior with 1 male partner.
Uveitic and infectious screening was performed. Infectious panel revealed serum RPR titer of 1:128. However, the patient was lost to follow up before commencement of any treatment. Three months later he returned with the intention to remove the Densiron. His vision was 6/24 OD and 6/9 OS.Fundus examination revealed right vitritis and retinal fibrosis(Figure 2). Further enquiries revealed that he had been treated for ocular syphilis by a private center with intramuscular benzylpenicillin weekly for 3wk. Repeat syphilis screening revealed serum RPR titer of 1:64, as well as positive Treponema pallidum IgG and IgM. HIV test was positive with CD4 count of 320 cells/mm 3 and HIV viral load of 16 989 copies/mm 3 .Lumbar puncture was not performed. The ID physician was consulted and he was treated for bilateral partially treated ocular syphilis with 24 MU of aqueous crystal penicillin G per day, administered as 4 MU intravenously over 4h for 14d. Oral prednisolone therapy was also prescribed at 50 mg per day.He was planned for subsequent treatment with intramuscular benzathine penicillin 2.4 MU weekly for 3wk. His latest visual acuity remained stable at 6/24 OD and 6/9 OS. He was planned to start on HAART later by the ID physician.
A 22-year-old man presented to us with 1wk history of eye itchiness followed by progressive blurring of vision in right eye. It was associated with redness. There was no history of fever,skin rashes, oral or genital ulcer. He has no known medical illness and his general condition was healthy. He is involved in MSM with a single partner who was diagnosed to have gonorrhoea. Ocular examination revealed visual acuity of 6/60 OD, corrected with pinhole to 6/24 and 6/6 OS. There was no relative afferent pupillary defect. The right eye revealed ciliary injection with fine white KPs, anterior chamber cell of 4+,and anterior vitreous cell of 4+. Fundus examination revealed dense vitritis, retinitis and hyperaemic optic disc (Figure 3).

Figure 3 Colored fundus photos of both eyes A: Right fundus showing dense vitritis and hyperaemic optic disc. B: Normal left fundus.
Chest X-ray (CXR) was normal. Full blood count did not show any sign of infection with white cell count of 7.9×10 9 /L.However, ESR was raised at 79 mm/h. Varicella zoster and herpes simplex 1 and 2 IgM were negative. Further blood investigation revealed positive venereal disease research laboratory (VDRL) of 1:128 titre and positive Treponema pallidum IgG (ELISA) and IgM (Western blot). Screening test for HIV by ELLIA method was reactive and supplementary test by Particle Agglutination method was positive for HIV-1.Unfortunately, patient requested for further follow up at different hospital.
A 30-year-old man, deaf and mute, with ambiguous genitalia,admitted to a medical ward with 2-week history of meningism,abnormal behavior, left sided weakness and left eye progressive blurring of vision. He was treated for bacterial meningitis and septicaemia. He was referred to us for eye assessment. Further enquiries revealed that he has engaged in MSM behavior with a male partner. Ocular examination revealed visual acuity of 6/12 OD and hand movement OS. No eye redness. No RAPD was observed but pupillary reflexes were sluggish. There was no cell in the anterior chamber but anterior vitreous cell was present (2+) in both eyes. Fundus examination showed vitritis,swollen and hyperaemic optic disc in the left eye. No retinitis or vasculitis was seen. (Figure 4). There was no maculopapular rashes and no oral or genital ulcer.
He was recently diagnosed with AIDS with CD4 count of 3, CD8 count of 76. His ESR was 95 mm/h and CRP 8.81.Syphilitic screening revealed positive RPR of 1:1024 titre and positive Treponema pallidum IgG. His head CT showed multifocal infarct. Lumbar puncture was performed and the results were negative for cryptococus, tuberculosis,CMV and toxoplasmosis. He was commenced on 24 MU of aqueous crystal penicillin G per day, administered as 4 MU intravenously over 4h for 14d and oral prednisolone 50mg per day for 1wk followed by tapering dose. HAART was also started during his admission in the ward. His left vision improves to 6/36 after 2wk of commencement of the therapy.
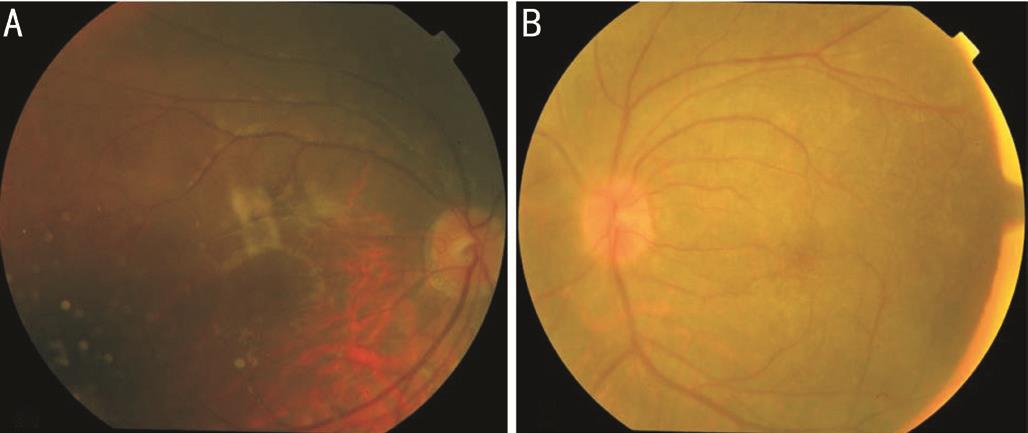
Figure 4 Colored fundus photos of both eye A: Normal right fundus.B: Left fundus showing vitritis, hyperaemic and swollen optic disc.
Syphilis is a multisystem, chronic bacterial infection caused by the spirochete Treponema pallidum . Treponema pallidum has the ability to infect multiple organ systems including skin, heart, blood vessels, bones, nervous system and eye leading to various clinical manifestations [1] . Its natural history progresses through well-characterised stages with devastating consequences if left untreated. Transmission occurs most often during sexual contact and may also occur transplacentally.
Syphilis is one of the great masqueraders of medicine and should always be considered in the differential diagnosis of any intraocular inflammatory disease even it is thought to be responsible for less than 2% of all uveitis cases. Ocular syphilis is considered to be a type of neurosyphilis, but it is not always accompanied by syphilitic meningitis. In the setting of normal lumbar puncture, the clinician should still consider this diagnosis.
Syphilis has been documented to affect almost every structure of the eye. Panuveitis and posterior uveitis are the most common type of ocular inflammation though optic neuropathy,interstitial keratitis, anterior uveitis and retinal vasculitis may all occur. Inflammation can be unilateral or bilateral,granulomatous or non-granulomatous [6] . Syphilis may affect the eye at both early and late stages regardless of the HIV status [1] . Patients may complain of eye pain, vision loss,floaters, flashes of lights, eye pressure and photophobia.
Diagnosis is centered around a high level of clinical suspicion and includes treponemal specific and non-treponemal serologic tests. All patients with newly diagnosed syphilis should be tested for co-infection with human immunodeficiency virus, as the risk factors are similar for both diseases. Current guidelines recommend that any ocular manifestation of syphilis (iritis,uveitis, choroiditis, retinitis) now be treated as neurosyphilis [1] .Parenterally administered penicillin G is the preferred drug for treatment of all stages of syphilis. Treatment of ocular syphilis consists of 18 to 24 MU of aqueous crystalline penicillin G per day, administered as 3 to 4 MU intravenously every 4h or as continuous infusion for 10 to 14d. Alternatively, it can be treated with 2.4 MU of intramuscular procaine penicillin once daily and probenecid 500 milligrams four times a day, both for 10 to 14d [7] .
In our first case, the patient presented with bilateral optic disc swelling and hyperaemia. Optic disc swelling has been reported in 13% of syphilis cases with posterior segment involvement [8] . With the availability of the antibiotics, the condition has become rare. While ocular syphilis is not a new phenomenon, recent reports from a growing number of countries indicate that syphilis rates among MSM, and in HIV-infected persons are on the rise and in some cases, reached levels not seen for more than 20y [9] . This has sparked a new interest in this old disease. A report by Tran et al [10] in 2005 in France found that all 12 HIV-infected patients with syphilitic uveitis were male and engaged in MSM.
The resurgence of syphilis has suggested to some that advances in HIV therapy has led to a disinhibition of MSM behaviors among men who no longer fear AIDS infection given the longer life expectancy afforded by HAART therapy. Among gay men, positive beliefs about the effectiveness of therapy were associated with increased rates of unprotected sex.Syphilitic ulcers facilitate HIV transmission and syphilis has been associated with increased viral load in HIV patient and decrease CD4 count. This explains the rapid progression among patients with syphilis co-infected with HIV [11] .
Early detection is important for the success of the treatment.A case series from Selayang Hospital, Malaysia reported a successful treatment of syphilitic uveitis with HIV positive patients. All were young aged from 23 to 35 years old [12] .Ocular syphilis co-infected with HIV is normally seen in young patient. When compared to HIV positive patient, HIV negative patient with ocular syphilis were older, were more likely to be female, and had poorer visual acuity at presentation [13] .
Prevention and control of sexually transmitted illness (STI)should be an integral part of comprehensive sexual and reproductive health services. This strategy deals with methods to promote healthy sexual behaviour, protective barrier methods, effective and accessible care for STIs. In patient already infected with syphilis and HIV, continuous moral support from family members or counsellors is important to prevent further dissemination of the disease. Contact tracing and regular communication with sufferers will also hopefully curb the rise in the disease.
In our case series, 3 patients showed good clinical responses to treatment. However, their treatment is far from over. All 4 patients were offered counselling on reproductive health services including their family members and their partners.This case series is likely to reflect a rise in cases of syphilitic ophthalmic disease. Ophthalmologist and ID physicians should be aware of the complexity of the diagnosis, the range of presenting symptoms and the fact that mild symptoms may mask potentially serious ocular disease. Prompt diagnosis,correct staging of syphilis and appropriate treatment and follow-up of the patient is important to reduce the ocular morbidity caused by this disease.
ACKNOWLEDGEMENTS
Conflicts of Interest: Mustapha M, None; Abdollah Z, None; Ahem A, None; Mohd Isa H, None; Bastion M-LC, None; Din NM, None.
REFERENCES
1 Woolston SL, Dhanireddy S, Marrazzo J. Ocular syphilis: a clinical review. Curr Infect Dis Rep 2016;18(11):36.
2 Marx GE, Dhanireddy S, Marrazzo JM, Tuddenham SA, Rompalo AM,Leone PA, Gaydos CA, Rietmeijer CA. Variations in clinical presentation of ocular syphilis: case series reported from a growing epidemic in the united states. Sex Transm Dis 2016;43(8):519-523.
3 Røttingen JA, Cameron DW, Garnett GP. A systematic review of the epidemiologic interactions between classic sexually transmitted diseases and HIV: how much really is known? Sex Transm Dis 2001;28(10):579-597.
4 Consensus report on STI, HIV and AIDS epidemiology Malaysia by MOH Malaysia. Apr., 2001.
5 Malaysian Guidelines in the Treatment of Sexually Transmitted Infections, Ministry of Health Malaysia 2008.
6 Rescigno RJ, Glatman M, Patel SN. A complicated case of sarcoidosis.Neurosyphilis. JAMA Ophthalmol 2014;132(5):649-650.
7 Kiss S, Damico FM, Young LH. Ocular manifestations and treatment of syphilis. Semin Ophthalmol 2005;20(3):161-167.
8 Northey LC, Skalicky SE, Gurbaxani A, McCluskey PJ. Syphilitic uveitis and optic neuritis in Sydney, Australia. Br J Ophthalmol 2015;99(9):1215-1219.
9 Read P, Fairley CK, Chow EP. Increasing trends of syphilis among men who have sex with men in high income countries. Sex Health 2015;12(2):155-163.
10 Tran TH, Cassoux N, Bodaghi B, Fardeau C, Caumes E, Lehoang P. Syphilitic uveitis in patients infected with human immunodeficiency virus. Graefes Arch Clin Exp Ophthalmol 2005;243(9):863-869.
11 Peterman TA, Furness BW. The resurgence of syphilis among men who have sex with men. Curr Opin Infect Dis 2007;20(1):54-59.
12 Nurfahzura MJ, Hanizasurana H, Zunaina E, Adil H. Successful treatment of syphilitic uveitis in HIV-positive patients. Clin Ophthalmol 2013;7:1651-1654.
13 Moradi A, Salek S, Daniel E, Gangaputra S, Ostheimer TA, Burkholder BM, Leung TG, Butler NJ, Dunn JP, Thorne JE. Clinical features and incidence rates of ocular complications in patients with ocular syphilis. Am J Ophthalmol 2015;159(2):334-343.
Citation: Mustapha M, Abdollah Z, Ahem A, Mohd Isa H, Bastion M-LC, Din NM. Ocular syphilis: resurgence of an old disease in modern Malaysian society. Int J Ophthalmol 2018;11(9):1573-1576
DOl: 10.18240/ijo.2018.09.25
Correspondence to: Mushawiahti Mustapha. Department of Ophthalmology, Pusat Perubatan Universiti, Jalan Yaacob Latiff, Cheras 56000, Malaysia. drmusha@gmail.com Received: 2017-08-14 Accepted: 2017-12-06