
Figure 1 Releasing of the ORL using blunt scissors.
The tear trough, named also nasojugal groove, extends inferolaterally from the medial canthus to the medial pupillary line, laterally the palpebromalar groove continues.With aging, both grooves connect to become a single groove that demarcates the protruding orbital fat above[1-2].
The tear trough may be found in young people, however it becomes more prominent with age. Despite being of an important cosmetic concern, the exact anatomical origin of the tear trough was not well defined. Tear trough dissection studies showed that the accurate location of tear trough corresponds to an obvious demarcation between the palpebral and orbital parts of the orbicularis oculi origin[3-6].
In 2011, tear trough dissection study was done by Wong et al[3].Their dissection through the soft-tissue spaces of the face revealed a true strong osteocutaneous ligament; the tear trough ligament. This ligament lied between the attachments of the palpebral and orbital parts of the orbicularis oculi to the maxilla, then inserts firmly into the skin at the site of the tear trough.
Multiple surgical and non surgical techniques have been described to correct the tear trough deformity, but unfortunately most techniques do not fully correct this deformity, and some even accentuate it[7-9]. Recent studies[7-12] have addressed management of tear trough deformity through fat repositioning,suborbicularis oculi fat lifting, filler (fat or artificial)injections or septal resetting but no studies have considered the disinsertion of orbicularis retaining ligament (ORL) for improving the tear trough deformity.
Rohrich et al[7] in 2011 described a five steps blepharoplasty technique which included: step 1, in which fat injection was done to augment the deep malar fat; step 2, transconjunctival fat excision; step 3, release of the trough ligament; step 4,lateral canthopexy; and step 5, skin was removed by pinching technique or skin flap.
The aim of our study was to evaluate the importance of adding the release of tear trough ligament to the transconjunctival fat excision in patients with tear trough deformity.
Ethical Approval The research adhered to the tenets of the Declaration of Helsinki and was conducted after the approval of the Ethical Review Committee of Cairo University, Faculty of Medicine. All patients signed an informed consent for intervention including: advantages, disadvantages and risks of possible complications.
A surgical trial which included 50 patients (100 eyes) with bilateral visible tear trough deformity and lower eyelid fat bulging were enrolled from July 2015 to January 2017.Patients were randomized (by closed envelope technique) into two groups (A&B): group A included 50 eyes of 25 patients who had a transconjunctival blepharoplasty surgery for fat excision; Group B included 50 eyes of 25 patients who had blepharoplasty surgery with releasing the ORL.
Inclusion Criteria Lower eyelid fat bulging with visible tear trough deformity.
Exclusion Criteria 1) Patients with fat bulging without tear trough; 2) Previous lower eyelid surgery; 3) History of abnormal bleeding or coagulopathy, renal failure, and edema of the extremities; 4) Combined conditions (i.e. Graves ophthalmopathy); 5) History of previous surgical fillers in tear trough area; 6) Patients with Sunken globe with lacrimal crest bone prominence; 7) Marked eyelid laxity with redundant skin.Qualitative evaluation of the tear trough deformity was done pre and postoperatively, using the grading system, Barton’s classification (the most common used grading system of tear trough deformity based on anatomic analysis:
Grade 0: Smooth contour of the orbit-cheek junction with no medial or lateral lines demarcating the arcus marginalis or the orbital rim.
Grade I: Mild, faint medial line or shadow with smooth transition of lid-cheek junction laterally.
Grade II: Moderate deepening of the demarcation line of the lid-cheek junction from medial to lateral.
Grade III: Severe well defined grooving of the orbit-cheek junction.
In an effort to objectively analyze the postoperative results,data was summarized using frequencies (number of cases) and relative frequencies (percentages).
Quantitative Outcome Assessment of Tear Trough Deformity Quantitative assessments by evaluating some preoperative and postoperative measurements in the form of:1) Distance from center of the pupil to tear trough (C-TT); 2)Distance from the center of lid margin to tear trough (Lid-TT);3) Distance from center of the pupil to lid margin (C-Lid); 4)Thickness of tear trough (Thick-TT).

Figure 1 Releasing of the ORL using blunt scissors.
Data were presented using mean, standard deviation, median minimum and maximum for quantitative variables.
Standardized photographic documentation of each patient was done pre- and postoperatively, also assessment of the patients’satisfaction postoperatively from (excellent-very goodgood-fair) according to the improvement in the peri-orbital rejuvenation.
Surgical Technique A traction suture is placed through the lower lids at the level of the meibomian gland orifices using 4-0 silk. A transconjunctival incision is made from the punctum medially to the lateral canthus laterally. Dissection is then performed to the inferior orbital rim between the orbital septum and the orbicularis muscle. A 4-0 silk suture is then taken through the cut end of the conjunctiva. Dissection is continued below the inferior orbital rim in the pre-periosteal plane with a blunt scissors to detach the ORL in group B as shown in Figure 1. The septum is then opened to identify the medial, central and lateral fat compartments which are excised only without transposition. The transconjunctival incision is then closed using 7-0 vicryl sutures. Topical antibiotic ointment is applied.
Follow-up Final results were documented at 1, 3 and 6mo postoperatively. The patient returned back at postoperative day 5 to 7. The second visit was at 1mo to detect any possible complications as lid retraction or ectropion, success rate was defined by achieving grade 0: smooth contour of the orbitcheek junction with no medial or lateral lines demarcating the arcus marginalis or the orbital rim or grade1: mild, medial line or shadow with smooth transition of the lid-cheek junction laterally of Barton classification after 6mo postoperatively.
Statistical Analysis Statistical analysis was done by SPSS 16.0 statistical software package. Results were presented in the form of frequencies, percentage for qualitative data, mean and standard deviation in case of quantitative variables. Statistical analysis for pre- and postoperative findings was performed using paired t-test. The results were considered statistically significant if P value was below 0.05.
Group A had a bilateral lower eye lid transconjunctival blepharoplasty surgery. Number of females was 23 (92%) and males 2 (8%) and mean age 42 years old with (range 25-58y). Group B had bilateral lower eyelid transconjunctival blepharoplasty surgery combined with release of the ORL, this group had 21 (84%) females and 4 (16%) males and mean age 47 years old (range 39-50y).
Table 1 Comparison between the two groups (A&B) regarding the four measurements pre- and postoperatively
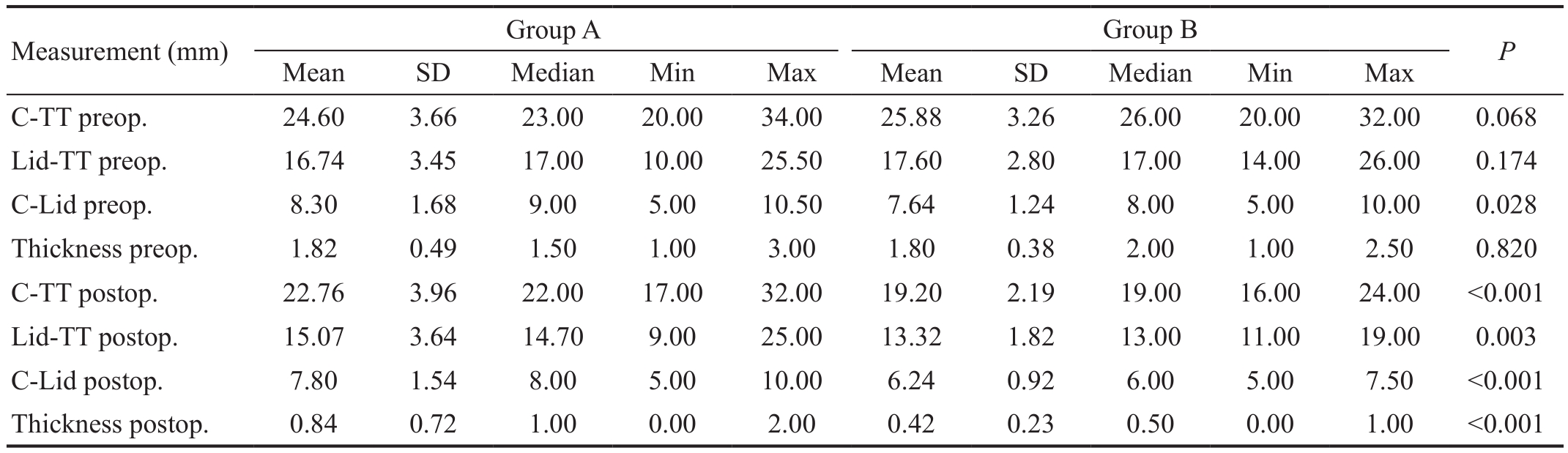
Lid-TT: Lid margin to tear trough; C-Lid: Distance from center of the pupil to lid margin; Thick-TT: Thickness of tear trough.
Measurement (mm) Group A Group B P Mean SD Median Min Max Mean SD Median Min Max C-TT preop. 24.60 3.66 23.00 20.00 34.00 25.88 3.26 26.00 20.00 32.00 0.068 Lid-TT preop. 16.74 3.45 17.00 10.00 25.50 17.60 2.80 17.00 14.00 26.00 0.174 C-Lid preop. 8.30 1.68 9.00 5.00 10.50 7.64 1.24 8.00 5.00 10.00 0.028 Thickness preop. 1.82 0.49 1.50 1.00 3.00 1.80 0.38 2.00 1.00 2.50 0.820 C-TT postop. 22.76 3.96 22.00 17.00 32.00 19.20 2.19 19.00 16.00 24.00 <0.001 Lid-TT postop. 15.07 3.64 14.70 9.00 25.00 13.32 1.82 13.00 11.00 19.00 0.003 C-Lid postop. 7.80 1.54 8.00 5.00 10.00 6.24 0.92 6.00 5.00 7.50 <0.001 Thickness postop. 0.84 0.72 1.00 0.00 2.00 0.42 0.23 0.50 0.00 1.00 <0.001
Comparison Between the Two Groups Regarding the Four Measurements Pre- and Postoperatively (Quantitative Analysis of Tear Trough) When comparing postoperative C-TT, Lid-TT, Thick-TT between groups A and B, P value was statistically significant as shown in Table 1.
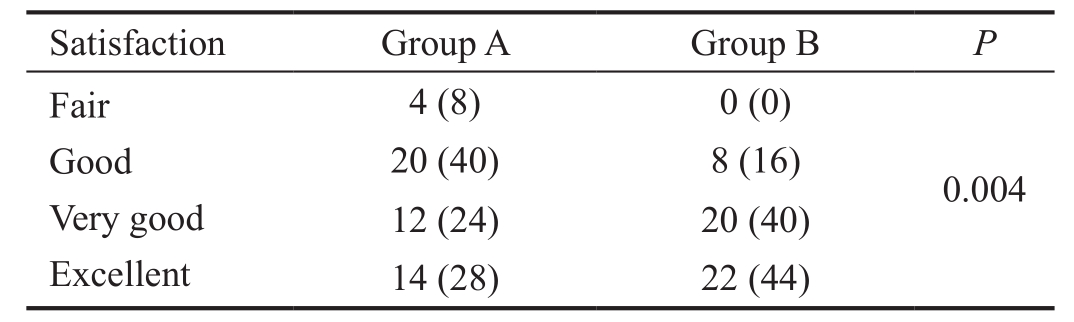
Comparison Between the Two Groups Regarding the Grades of Tear Trough Deformity Postoperatively (Qualitative Analysis of Tear Trough) When comparing grades of the tear trough in both groups postoperatively, we found that in group A most of patients had grade 0 (40%) followed by grade 2 (36%) and the least had grade 1 (24%; Figure 2), while in group B most of the patients had grade 1 (52%; Figure 3)followed by grade 0 (40%; Figure 4) and least had grade 2 (8%).Patient Satisfaction Patients’ questionnaire (from fair to excellent) was done at 6mo postoperatively to testify patients’satisfaction from the surgery in both groups regarding the aesthetic results depending on their expectations and postoperative complications as shown in Table 2.
Complications In group B (where release of ORL was combined with blepharoplasty surgery) the surgeon experienced difficulty while releasing the ORL in 6 eyes, as scissors manipulation caused severe bleeding that stopped by diathermy and compression, those 6 (3%) eyes had hematoma postoperatively which resolved by the fourth week follow up.Lower eyelid malposition was not seen in any of the patients.
Rejuvenation of the lower eyelid is an important issue in aesthetic plastic surgery. To quote Glaser and Patel[13], “The aesthetically attractive lower eyelid should display a relatively smooth transition between the pre-septal and orbital portions of the orbicularis oculi muscle and continue into the upper malar region without a definable transition point.
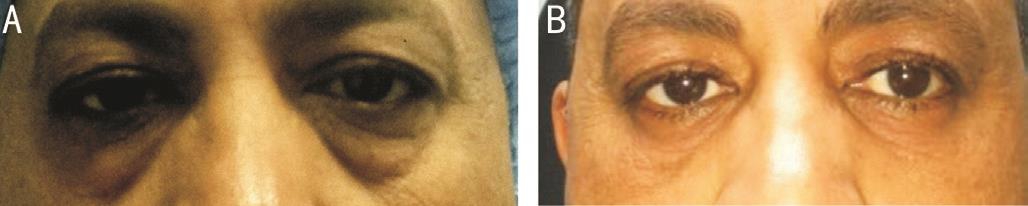
Figure 2 Example of group A (conventional blepharoplasty) A:Preoperative photo of a patient with grade 3 tear trough; B: After 6mo follow up, grade 1 tear trough. This patient evaluated this surgery as good.
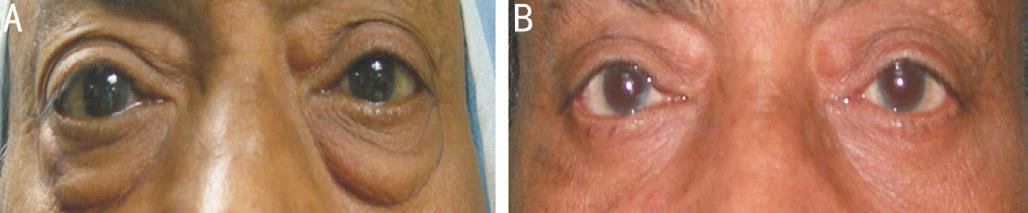
Figure 3 Example of group B (conventional blepharoplasty with release of ORL A: Preoperative photos of a patient was grade 3;B: After 6mo follow up, grade of tear trough became 1. The patient evaluated the outcome as excellent.
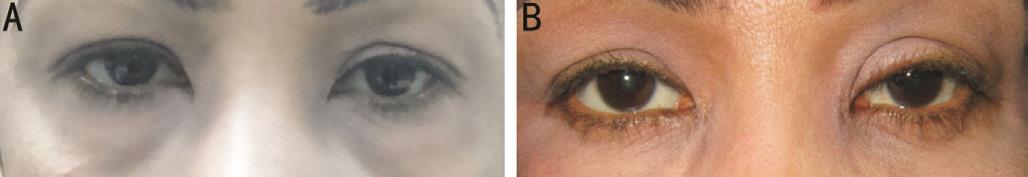
Figure 4 Example of group B (conventional blepharoplasty with release of ORL) A: Preoperative photos of a patient with grade 2;B: After 6mo follow up, grade of tear trough became 0. This patient evaluated the new technique as very good.
Table 2 Comparison between groups A and B regarding patient satisfaction n (%)
?
In the last years fat transposition in transconjunctival blepharoplasty was widely used in management of fat bulging with tear trough deformity as it decreases the drawbacks of skin-muscle flap methods[14]. However there are several factors that affect fat transposition outcomes, mainly determining the adequate amount of fat to resect. Too much resection leaves too little fat to transpose and inadequate fat resection causes undercorrection of fat herniation[15].
A second variable is the time needed for transposed fat to become stable. Fat may be retracted again into the orbit, also fat atrophy may develop postoperatively[16-17]. Fat transposition also results in postoperative edema and ecchymosis due to subperiosteal dissection of the orbital rim with possible longterm visibility of the transposed fat and septum[18].
The idea of our study was based upon the fact that a true osteocutaneous ligament, the tear trough ligament, originates from the maxillary bone and attaches to the skin at the site of the tear trough. The tethering effect of the tear trough ligament is the main etiology of the prominence of the tear trough deformity[3,19]. Secondary factors are the different tissue characteristics above and below the trough[20]. The tear trough ligament needs to be detached totally to soften the tear trough deformity. To make sure that the ligament is completely detached, the attachment of the palpebral and orbital parts of the orbicularis oculi should be cut completely from the maxilla.This should be done close to its insertion to the bone to avoid injury of the motor nerves and vessels[21]. Rohrich et al[7] in 2011, performed five step blepharoplasty; in the form of fat injection in the deep malar fat, transconjunctival fat excision,ORL release, lateral retinacular canthopexy and skin removal by pinching technique or skin flap. Their study included 50 patients (100) with bilateral tear trough deformity, their results showed an 80 percent decrease in pupil to tear trough distance together with a 79 percent narrowing of tear trough width in cases of ORL release. Our results were consistent with theirs,however, we only did fat resection together with the release of the ligament without lateral canthal support or skin flaps,only pinch technique in some selected cases, as we believe that these steps help in softening tear trough deformity.
In 2017, Wong and Mendelson[22] showed the results of their work in which they adopted similar procedure to ours. From 2012 to 2015, 54 subjects had transconjunctival blepharoplasty with fat excision. Medially, the attachments of both the palpebral and orbital parts of the orbicularis oculi together with the tear trough ligament were released. More laterally, the ORL was detached. Excised fat was grafted beneath the released ligament to fill the tear trough groove. The mean follow-up was 10mo. High satisfaction was found among the patients.The revision rate was 2 percent[22].
As the primary concern in any aesthetic surgery is subjects’satisfaction, we used a questionnaire to evaluate it (from fair to excellent) and more patient’s satisfaction was in favor of the group with tear trough ligament release. This was consistent with a retrospective study by Kashkouli et al[23] who reported that patients’ satisfaction is improved when transconjunctival blepharoplasty was associated with other procedures addressing facial functional and aesthetic issues. This may signify the importance of periocular status, as tear trough deformity, on self-image and satisfaction.
No complications were encountered while releasing the ORL except for intraoperative bleeding in 6 patients, which might be due to being a new technique with a learning curve. Hematoma persisted postoperatively for four weeks, however this didn’t affect patients’ satisfaction.
In conclusion, fat resection through conventional blepharoplasty shouldn’t be done alone especially in severe tear trough deformity. ORL release should be done in order to release the tethering effect of this ligament which leads to the prominence of the naso-jugal groove. Our study proved that both the aesthetic results and patient satisfaction was higher in patients who had the new combined technique compared to those who had conventional blepharoplasty alone, this highlights the importance of the ORL and the significance of its release in the new trends for management of tear trough.
We would like to thank our patients who gave us the right to carry out this work.
Confiicts of Interest: Gawdat TI, None; Elsherif EA, None;Alahmadawy YA, None; Mostafa YS, None.
1 Mendelson BC, Jacobson SR. Surgical anatomy of the midcheek:facial layers, spaces, and the midcheek segments. Clin Plast Surg 2008;35(3):395-404; discussion 393.
2 Ghavami A, Pessa JE, Janis J, Khosla R, Reece EM, Rohrich RJ. The orbicularis retaining ligament of the medial orbit: closing the circle. Plast Reconstr Surg 2008;121(3):994-1001.
3 Wong CH, Hsieh MK, Mendelson B. The tear trough ligament:anatomical basis for the tear trough deformity. Plast Reconstr Surg 2012;129(6):1392-1402.
4 Mendelson BC. Anatomic study of the retaining ligaments of the face and applications for facial rejuvenation. Aesth Plast Surg 2013;37(3):513-515.
5 Alghoul M, Codner MA. Retaining ligaments of the face: review of anatomy and clinical applications. Aesthet Surg J 2013;33(6):769-782.
6 Haddock NT, Saadeh PB, Boutros S, Thorne CH. The tear trough and lid/cheek junction: anatomy and implications for surgical correction. Plast Reconstr Surg 2009;123(4):1332-1340; discussion 1341-1342.
7 Rohrich RJ, Ghavami A, Mojallal A. The five-step lower blepharoplasty:blending the eyelid-cheek junction. Plast Reconstr Surg 2011;128(3):775-783.
8 Stutman RL, Codner MA. Tear trough deformity: review of anatomy and treatment options. Aesthetic Surgery Journal 2012;32(4):426-440.
9 Codner MA, Hirmand H. Lid-cheek blending: the tear trough deformity.In: Aston S, Steinbrech D, Walden J, eds. Aesthetic Plastic Surgery.Philadelphia, PA: Saunders Elsevier; 2009.
10 Spector JA, Draper L, Aston SJ. Lower lid deformity secondary to autogenous fat transfer: a cautionary tale. Aesthetic Plast Surg 2008;32(3):411-414.
11 Chang YC. Tear trough-anatomy and treatment by autologous fat grafting. J Surg Dermatol 2016;1(2).
12 Donath AS, Glasgold RA, Meier J, Glasgol MJ. Quantitative evaluation of volume augmentation in the tear trough with a hyaluronic acid-based filler: a three dimensional analysis. Plast Reconstr Surg 2010;125(5):1515-1522.
13 Glaser DA, Patel U. Enhancing the eyes: use of minimally invasive techniques for periorbital rejuvenation. J Drugs Dermatol 2010;9(8 Suppl ODAC Conf Pt 2):s118-s128.
14 Grant JR, Laferriere KA. Periocular rejuvenation: lower eyelid blepharoplasty with fat repositioning and the suborbicularis oculi fat.Facial Plast Surg Clin North Am 2010;18(3):399-409.
15 Hidalgo DA. An integrated approach to lower blepharoplasty. Plast Reconstr Surg 2011;127(1):386-395.
16 Darcy SJ, Miller TA, Goldberg RA, Villablanca JP, Demer JL, Rudkin GH. Magnetic resonance imaging characterization of orbital changes with age and associated contributions to lower eyelid prominence. Plast Reconstr Surg 2008;122(3):921-929; discussion 930-931.
17 Wattanakrai K, Chiemchaisri N, Wattanakrai P. The periosteal pulley technique for orbital fat realignment and correction of nasojugal groove in lower lid blepharoplasty. J Plast Reconstr Aesthet Surg 2014;67(4):513-519.
18 Pepper JP, Baker SR. Transcutaneous lower blepharoplasty with fat transposition. Clin Plast Surg 2015;42(1):57-62.
19 Wong CH, Mendelson B. Facial soft-tissue spaces and retaining ligaments of the midcheek: defining the premaxillary space. Plast Reconstr Surg 2013;132(1):49-56.
20 Hirmand H. Anatomy and nonsurgical correction of the tear trough deformity. Plast Reconstr Surg 2010;125(2):699-708.
21 Yoo DB, Peng GL, Massry GG. Transconjunctival lower blepharoplasty with fat repositioning. JAMA Facial Plastic Surgery 2013;15(3):176-181.
22 Wong CH, Mendelson BC. Reply: extended transconjunctival lower eyelid blepharoplasty with release of the tear trough ligament and fat redistribution. Plast Reconstr Surg 2018;142(2):236e-237e.
23 Kashkouli MB, Pakdel F, Kiavash V, Ghiasian L, Heirati A,Jamshidian-Tehrani M. Transconjunctival lower blepharoplasty: a 2-sided assessment of results and subjects’ satisfaction. Ophthalmic Plast Reconstr Surg 2013;29(4):249-255.