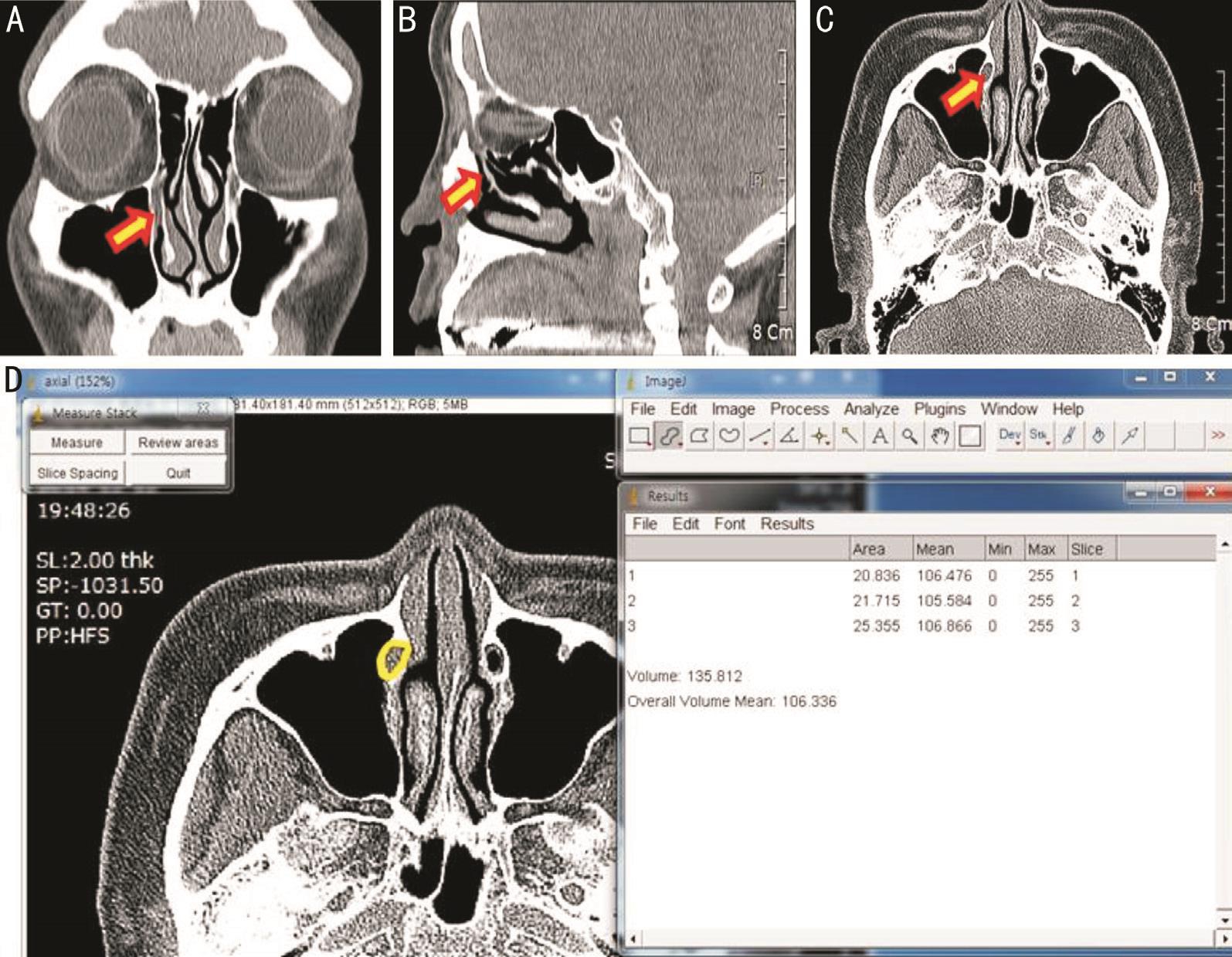
Figure 1 Coronal (A), sagittal (B), and axial (C) 2D computed tomography images were analyzed using Image J (D) for measurement of the nasolacrimal duct volume. Arrows indicate nasolacrimal duct.
Epiphora is a symptom very commonly experienced in ophthalmology, and nasolacrimal duct obstruction, dry eye, eyelid anomaly, the malfunction of the lacrimal pump,and many complex factors have been reported as causes[1-3].Partial and complete obstruction of the nasolacrimal duct is one of the most common causes of epiphora, and it has been reported that 31.8% of patients who complained of epiphora had nasolacrimal duct obstruction[4].
Nasolacrimal duct obstruction can be divided broadly into congenital and acquired types. Congenital nasolacrimal duct obstruction is a disease with a very clear cause, in which nasolacrimal duct obstruction occurs because the Hasner valve is not normally open even after birth. In contrast, various and complex causes for acquired nasolacrimal duct obstruction,such as primary factors (inflammation arising in the nose as ascending factors and in the eye as descending factors) and secondary factors [infection (bacteria, viruses and fungi),trauma, surgery, neoplasm, sarcoidosis and granulomatosis]have been reported[5-8], and no clear pathological physiology has yet been established.
Given that nasolacrimal duct obstruction is more common in women than in men, it has also been reported that nasolacrimal duct diameter may be a cause of obstruction[9]. A few studies on the structure of the nasolacrimal duct using computed tomography images have been reported, with a few studies that measured volume, all of which were in Westerners[10-12].We measured nasolacrimal duct volume using computed tomography images in Korean people to help understand the pathological physiology of nasolacrimal duct obstruction with complex causes of disease.
Ethical Approval The study was approved by the Institutional Review Board of Korea University Hospital, and it was carried out according to the tenets of the Declaration of Helsinki.
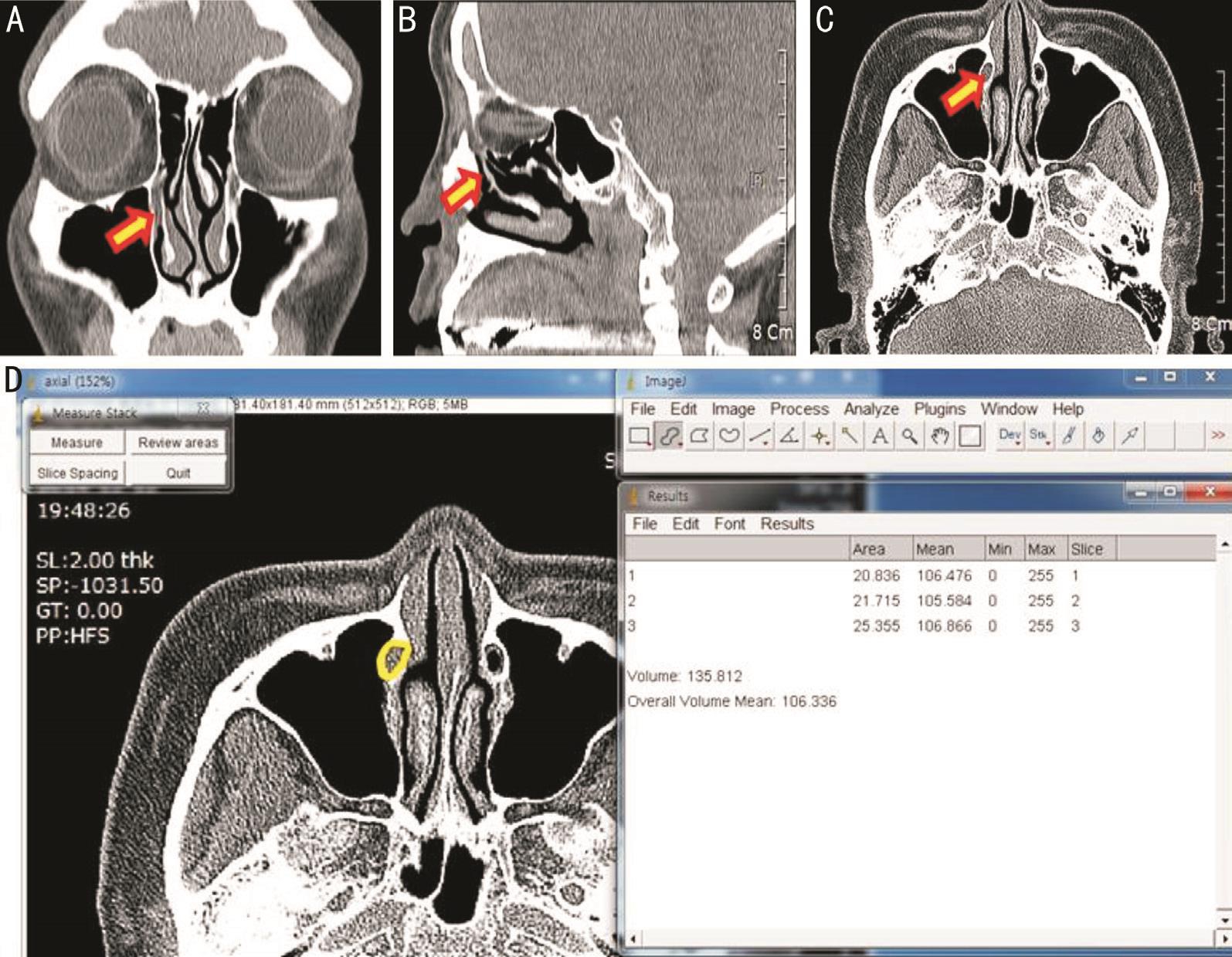
Figure 1 Coronal (A), sagittal (B), and axial (C) 2D computed tomography images were analyzed using Image J (D) for measurement of the nasolacrimal duct volume. Arrows indicate nasolacrimal duct.
We initially selected patients aged 30 to 80y who had visited Korea University Guro Hospital Oculoplastic Clinic and had undergone computed tomography from March 2013 through January 2016. We retrospectively analyzed medical records and classified a group of patients diagnosed with nasolacrimal duct obstruction into a patient group, and those who had computed tomography for the purpose of diagnosis on ophthalmological symptoms such as orbital contusion and eyelid edema into a control group. In order to exclude differences in nasolacrimal duct volume according to the difference in sex ratio between the two groups, the sex ratios of the two groups were matched.In order to exclude the symptom of reflexive epiphora by stimulus in the patient group, lacrimal punctum status, tear film break-up time, and keratoconjunctivitis degree were tested via a slit lamp microscopic test, nasolacrimal duct obstruction was evaluated with lacrimal syringing, and the obstruction region was judged with probing. In addition,if necessary, a dacryoscintigraphy was conducted to help diagnose nasolacrimal duct obstruction. If patients had a past history of facial nerve palsy and trauma, or other causes of epiphora, including scleroderma, eyelid stiffening by burn,intranasal surgery, punctal stenosis and malposition on slit lamp examination, laxity of the eyelid, and ectropion of the eyelid, they were excluded from the patient group. And patients with clinical or radiological evidence of acute or chronic dacryocystitis were also excluded from the patient group. If patients who had fractures due to orbital contusion or for whom there would be an impact on measurement of nasolacrimal duct volume by specific findings such as orbital tumor, idiopathic orbital in flammation, and thyroid eye disease observed in computed tomography images for the purpose of diagnosis, they were excluded from the control group.
Computed tomography was performed using Siemens Somatom Sensation 16 (Siemens, Erlangen, Germany) in three directions (axial, coronal, and sagittal) at an interval of 2 mm. Of the images obtained from axial, coronal, and sagittal directions, all images in which the nasolacrimal duct was seen were selected, and the range of the nasolacrimal duct was defined as the range from the junction between the lacrimal sac and the nasolacrimal duct to the Hasner valve.To determine the more accurate area of the nasolacrimal duct,an average of the volume measurements in three directions was used for statistical analysis. Selected 2 D images were reproduced into 3 D images with the Image J program, which is a public domain, Java-based image processing software package developed at the National Institutes of Health (NIH)[13] to measure nasolacrimal duct volume. The process of calculating the volume was as follows[14]: pixels are converted to the length unit; the distance between the images is set to 2 mm;the areas of the nasolacrimal duct seen from the axial, coronal,and sagittal images are marked as lines, using the Selection Brush Tool in Image J; 3 D images are produced; and volume is measured (unit: mm3) using the method of the Integral (Figure 1).In order to increase the reproducibility and accuracy of the volume measurement, one researcher (Park JH) measured the right and left three times each in a blind manner and then set the average value as the nasolacrimal duct volume.
Using an unpaired Student t-test, the average values for age and nasolacrimal duct volume of the patient group and control group were compared, and the nasolacrimal duct volumes of the obstructed eyes and normal eyes of subjects in the patient group were compared with the nasolacrimal duct volume of eyes of subjects in the control group. Using a paired t-test, for the patient group, the average value of the nasolacrimal duct volume of the obstructed eyes of patients with nasolacrimal duct obstruction only in one eye was compared with that of the normal eye on the opposite side. Men and women were differentiated in the patient group and the control group, and the average nasolacrimal duct volumes were compared by age groups using Kruskal-Wallis analysis. SPSS version 20.0(SPSS Inc. Chicago, IL, USA) was used, and a P-value lower than 0.05 was defined as statistically significant.
This study included 39 people in the patient group (78 eyes)and 39 people in the control group (78 eyes). The sex ratio of the patient group and the control group was the same (11 men and 28 women), and their average age was 55.72±14.51 years old in the patient group and 53.77±13.27 years old in the control group, which did not show any significant difference(P=0.412). In the patient group, the number of patients with nasolacrimal duct obstruction in one eye was 27 while 12 patients had nasolacrimal duct obstruction in both eyes (Table 1).The average bilateral nasolacrimal duct volume of the patient group was 236.28±79.80 mm3, while that of the control group was 217.61±82.04 mm3. The average nasolacrimal duct volume was higher in the patient group, but was not significantly difference (P=0.132). The average nasolacrimal duct volume of obstructed eyes (39 persons, 51 eyes) in all subjects in the patient group was 225.20±73.80 mm3, while that of the control group (39 persons, 78 eyes) was 217.61±82.04 mm3. On comparison of obstructed eyes and normal eyes in the patient group with those in the control group, both obstructed eyes and normal eyes of the patient group showed significantly higher average values of nasolacrimal duct volume than the control group (P<0.001, P<0.001). In patients with unilateral nasolacrimal duct obstruction in the patient group (27 persons,54 eyes), the average value of the nasolacrimal duct volume of the obstructed eyes (27 eyes) was 238.91±73.49 mm3 while that of normal eyes (27 eyes) on the opposite side was 225.20±73.80 mm3; further, the average nasolacrimal duct volume of the obstructed eyes was higher, but the result was not significant (P=0.092).
For all patients (78 persons, 156 eyes), the average right nasolacrimal duct volume was 226.62±80.49 mm3 while the left nasolacrimal duct volume was 227.28±82.37 mm3, without significant difference (P=0.445). On comparison of men (22 persons, 44 eyes) and women (56 persons, 112 eyes), the average men’s nasolacrimal duct volume was 265.33±90.57 mm3 while women’s nasolacrimal duct volume was 211.87±68.61 mm3,and the average men’s nasolacrimal duct volume was significantly higher than women’s nasolacrimal duct volume(P=0.009). The average nasolacrimal duct volume of obstructed eyes of men in the patient group (11 persons, 13 eyes) was 237.38±95.28 mm3, while the nasolacrimal duct volume of men in the control group (11 persons, 22 eyes) was 282.03±96.56 mm3. Additionally, the average nasolacrimal duct volume in men in the control group was higher, but the result was not significant (P=0.097). The average nasolacrimal duct volume of obstructed eyes of women in the patient group(28 persons, 38 eyes) was 244.29±79.52 mm3 while the control group (28 persons, 56 eyes) was 192.30±59.60 mm3, and the average nasolacrimal duct volume of women in the patient group was significantly higher (P<0.001; Table 2).
Table 1 Demographics of Subjects
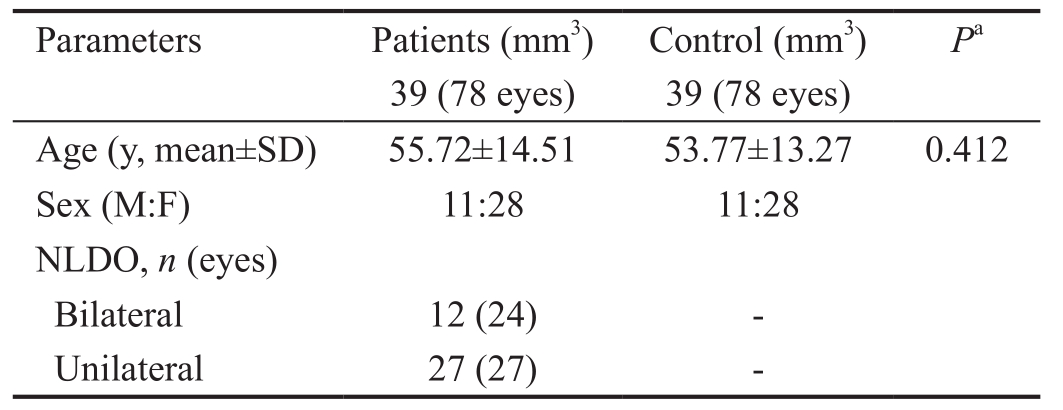
NLDO: Nasolacrimal duct obstruction; M: Male; F: Female; SD:Standard deviation.aUnpaired Student t-test.
?
In men in the patient group, nasolacrimal duct volume by age was 308.96±58.11 mm3 for subjects in their 30y; 192.79±79.72 mm3 for those in their 40y; 338.55±16.70 mm3 for those in their 50y; 203.93±144.11 mm3 for those in their 60y; and 215.48±65.48 mm3 for those in their 70y. There were no significant differences by age (P=0.073). For women in the patient group, it was 201.95±64.50 mm3 for subjects in their 30y; 187.49±64.06 mm3 for those in their 40y; 200.69±74.66 mm3 for those in their 50y; 183.88±38.36 mm3 for those in their 60y; and 189.04±58.27 mm3 for those in their 70y, also without any significant differences (P=0.938). For men in the control group, it was 298.17±64.50 mm3 for those in their 30y;131.69±16.66mm3 for those in their 40y; 358.87±14.04 mm3 for those in their 50y; 385.29±1.21 mm3 for those in their 60y; and 251.41±1.69 mm3 for those in their 70y. There were significant differences between the groups (P<0.001). For women, it was 162.96±30.67 mm3 for those in their 30y; 237.20±89.14 mm3 for those in their 40y; 245.48±71.96 mm3 for those in their 50y;229.02±81.98 mm3 for those in their 60y; and 268.85±47.32 mm3 for those in their 70y, without any significant differences(P=0.163; Table 3).
The most common cause of epiphora, nasolacrimal duct obstruction, occurs for idiopathic and congenital reasons,trauma, drugs, and irradiation. Inflammation of the nasolacrimal duct by these multiple causes can result inreconstruction of mucosal edema and connective tissue fibers,transient obstruction, and repetitive in flammation progress that in the end causes permanent obstruction of the nasolacrimal duct[10-11].
Table 2 Mean volume measurements of nasolacrimal ducts in patients and controls mm3, mean±SD

NLDO: Nasolacrimal duct obstruction; Rt.: Right eye; Lt.: Left eye; M: Male; F: Female; SD: Standard deviation.
aUnpaired Student’s t-test.
Mean volume of nasolacrimal duct Pa Rt. (78 eyes) vs Lt. (78 eyes) 226.62±80.49 vs 227.28±82.37 0.445 M (44 eyes) vs F (112 eyes) 265.33±90.57 vs 211.87±68.61 0.009 NLDO (+) M (n=11, 13 eyes) vs Control M (n=11, 22 eyes) 237.38±95.28 vs 282.03±96.56 0.097 NLDO (+) F (n=28, 38 eyes) vs Control F (n=28, 56 eyes) 244.29±79.52 vs 192.30±59.60 <0.001 Parameters
Table 3 Mean volume measurements of nasolacrimal ducts in patients and controls mm3, mean±SD
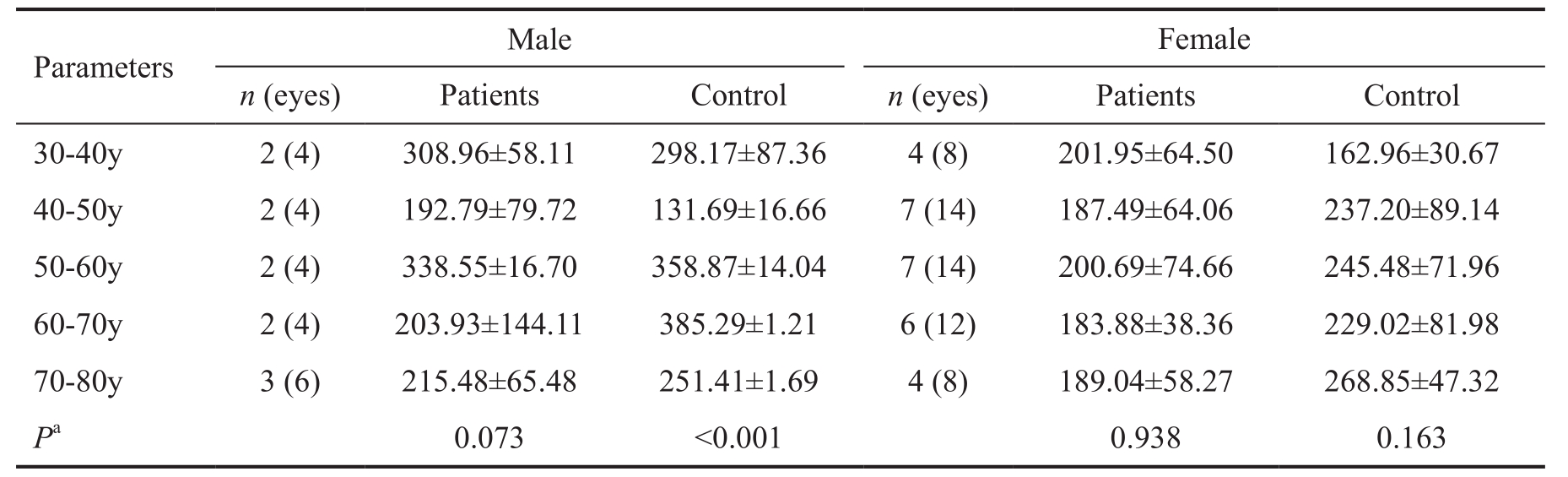
SD: Standard deviation.aKruskal-Wallis analysis.
?
With the development of image inspection equipment such as computed tomography, the structure of the nasolacrimal duct can be evaluated more clearly, and increased effort has been made to understand the causes of nasolacrimal duct obstruction from a structural perspective[12,15-18]. Ramey et al[10] compared nasolacrimal duct volume according to age, sex, and race, and they reported that young men had a significantly larger volume than young women. In contrast, Bulbul et al[12] divided subjects into a nasolacrimal duct obstruction group and a normal group to compare nasolacrimal duct volume, and they reported that there was no significant difference between the two groups.Estes et al[11] also divided subjects into a nasolacrimal duct obstruction group and a normal group and measured their nasolacrimal duct volume. There was no significant difference between the nasolacrimal duct obstruction group and the normal group, but they reported that men had a significantly larger volume than women. In addition, Estes et al[11] reported that nasolacrimal duct volume was smaller in men with nasolacrimal duct obstruction in a patient group than in those in a normal group, but it was not significant; on the other hand, women with nasolacrimal duct obstruction in a patient group had significantly larger nasolacrimal duct volume than those in a normal group. They predicted that nasolacrimal duct obstruction would become more common with smaller nasolacrimal duct volume, but the research result was different from their expectation and they concluded that there was no correlation between nasolacrimal duct volume and the occurrence of nasolacrimal duct obstruction.
In this study, similar to the results of Estes et al[11], the average bilateral nasolacrimal duct volume in the patient group was higher than that of the control group, but not significant;however, unlike the men, the average value of nasolacrimal duct volume of the obstructed eyes of women in the patient group was significantly larger than in the control group. This conflicts with the results of Jenssen et al[19] that there was a larger possibility of obstruction in nasolacrimal ducts with smaller diameter. The reason for this difference can be found first in the method of measuring nasolacrimal duct volume.Since this study used computed tomography images, it measured nasolacrimal duct volume based on clearly found bone. However, there is a limitation that the volume of the bone cannot accurately represent the volume of the nasolacrimal duct, which is soft tissue. Preceding studies reported that in children with congenital nasolacrimal duct obstruction, the size of the nasolacrimal duct increased in eyes with nasolacrimal duct obstruction compared to normal eyes, and this result has been explained by expansion of the nasolacrimal duct allowed by the plasticity of children’s bone structure[20-21]. Since this study was conducted with adults without bone structure plasticity, it was judged that large nasolacrimal duct volume is caused by degeneration of nasolacrimal duct bone tissue by repetitive inflammation. Another issue to be considered is the relationship between diameter and volume. Even if the diameter of the nasolacrimal duct is small, if the length is large, the measured nasolacrimal duct volume can still be large. Since a nasolacrimal duct with a small diameter and long length may be a factor that is likely to obstruct anatomically, it is necessary to investigate correlations among diameter, length,and volume of the nasolacrimal duct.
This study, like previous studies, could not clearly reveal the correlation between nasolacrimal duct volume and nasolacrimal duct obstruction[12,15-16]. However, this study demonstrated that women with nasolacrimal duct obstruction and smaller nasolacrimal duct volume less than men had larger nasolacrimal duct volume than that of the normal group. Since inflammation can easily occur in a smaller nasolacrimal duct volume, the possibility that this may cause degeneration of the bone cannot be excluded. The correlation between nasolacrimal duct volume and chronic in flammation should be considered together. In addition, in order to better reveal the correlation between nasolacrimal duct volume and nasolacrimal duct obstruction, it is necessary to utilize image devices that can directly measure soft tissue volume.
In this study, there was no significant difference in average nasolacrimal duct volumes of obstructed eyes and normal eyes of patients with unilateral nasolacrimal duct obstruction in the patient group. On comparison of the average nasolacrimal duct volumes of obstructed eyes and the normal eyes of patients with nasolacrimal duct obstruction in the patient group with that of the nasolacrimal duct volumes of the control group,the average value was significantly larger than the control group. Nasolacrimal duct obstruction usually occurs in one eye[22-23], but as time passes, there is a clinical aspect in which nasolacrimal duct obstruction occurs in the opposite normal eye as well. In other words, since non-obstructed eyes in patients with unilateral nasolacrimal duct obstruction show an anatomical difference in larger nasolacrimal duct volume, it is necessary to continuously observe possible clinical progression to nasolacrimal duct obstruction.
This study compared the average value of the left and right nasolacrimal duct volumes of the entire group, but there were no significant differences. Men’s nasolacrimal duct volume was significantly larger than that of women, and this result is similar to studies of Western populations[12]. In addition, this study divided subjects into men and women and compared nasolacrimal duct volume by age. There was no significant difference in all groups except for men in the control group.There have not been studies on the distribution of nasolacrimal duct volume by age, and Jenssen et al[19] reported that there was no significant difference between nasolacrimal duct diameter and age. In this study, the nasolacrimal duct volume of adults did not have any significant difference by age, similar to nasolacrimal duct diameter. Thus, the clinical aspect in which the prevalence rate of nasolacrimal duct obstruction increased with age could not be explained by nasolacrimal duct volume. In addition, it turned out that there was a difference in nasolacrimal duct volume by age only in men in the control group. In order to find clear statistical significance, it would be necessary to conduct a study with a larger number of patients.The average nasolacrimal duct volume of the patient group and the control group measured in this study was 236 mm3 and 218 mm3, respectively. These values are different from the study results in Westerners. The average nasolacrimal duct volume of men and women measured by Ramey et al[10]were 327 mm3 and 244 mm3, while the average values of the nasolacrimal duct volume of a patient group with nasolacrimal duct obstruction and a normal group measured by Estes et al[11] were 0.411 cm3 and 0.380 cm3, respectively. Both studies measured volumes using computed tomography images, but they differed in the method of measuring 3 D volumes using 2 D images. Therefore, differences in the nasolacrimal duct volume between Westerners and Korean people should not be asserted based on only these results. It is necessary to measure and analyze the nasolacrimal duct volume of Easterners and Westerners using the same method in the future.
This study has the following limitations. First, the sample size is small. Compared with previous studies, the number of subjects in this study is not small, but the sample is too small to compare the nasolacrimal duct volume by several age groups. In order to obtain higher statistical significance,the study of nasolacrimal duct volume by age including more subjects will be needed. Second, due to similar densities on computed tomography, the classification between the lacrimal drift and the surrounding tissue was not clearly differentiated.Third, since computed tomography was measured with a thickness of 2 mm, 3 D reproduction of the nasolacrimal duct using Image J could not be accurate. However, this study has profound significance because we measured and reported the nasolacrimal duct volume of Korean people for the first time using computed tomography images to understand the pathological physiology. To calculate the volume by advanced methods using 3 D reconstructed images, researchers should use specific devices such as laser scanning machines, camera,or the software packages that reconstruct images into a 3 D model or automatically calculate the volume based on computed tomography or magnetic resonance imaging. But these devices are too expensive and require specific volume-analysis software. We could confirm that volume measurement method using Image J software is a cost-effective, simple, and easily accessible.
Authors’ contributions: Park JH, study design, data acquisition and analysis, interpretation, drafting and revising manuscript, accountability for all aspects of the work, final approval; Huh JA, data acquisition and analysis, interpretation,drafting and revising manuscript, accountability for all aspects of the work, final approval; P JF, data acquisition and analysis, drafting and revising manuscript, accountability for all aspects of the work, final approval; Lee H, data acquisition and analysis, drafting and revising manuscript, accountability for all aspects of the work, final approval; Baek SH, study conception and design, drafting and revising manuscript,accountability for all aspects of the work, final approval.
Confiicts of Interest: Park JH, None; Huh JA, None; P JF,None; Lee H, None; Baek SH, None.
1 Tannenbaum M, McCord CD. The lacrimal drainage system. In: Tasman W, Jaeger EA, eds. Duane’s clinical ophthalmology. Vol 4. Philadelphia:J.B. Lippincott Co.; 1991:1-33.
2 Hirschbein MJ, Stasior GO. Lacrimal system. In: Chen WP-D, ed.Oculoplastic Surgery: The Essentials. New York: Thieme; 2001:263-288.
3 Vick VL, Holds JB, Hartstein ME, Massry GG. Tarsal strip procedure for the correction of tearing. Ophthal Plast Reconstr Surg 2004;20(1):37-39.
4 Sibley D, Norris JH, Malhotra R. Management and outcomes of patients with epiphora referred to a specialist ophthalmic plastic unit. Clin Exp Ophthalmol 2013;41(3):231-238.
5 Bartley GB. Acquired lacrimal drainage obstruction: an etiologic classification system, case reports, and a review of the literature. Part 3.Ophthal Plast Reconstr Surg 1993;9(1):11-26.
6 Hurwitz J. Diseases of the sac and duct. The Lacrimal System.Philadelphia: Lippincott-Raven 1996:117-122.
7 Seider N, Miller B, Beiran I. Topical glaucoma therapy as a risk factor for nasolacrimal duct obstruction. Am J Ophthalmol 2008;145(1):120-123.e1.
8 Woog JJ. The incidence of symptomatic acquired lacrimal outflow obstruction among residents of Olmsted County, Minnesota, 1976-2000.Trans Am Ophthalmol Soc 2007;105:649-666.
9 Linberg JV, McCormick SA. Primary acquired nasolacrimal duct obstruction a clinicopathologic report and biopsy technique. Ophthalmology 1986;93(8):1055-1063.
10 Ramey NA, Hoang JK, Richard MJ. Multidetector CT of nasolacrimal canal morphology: normal variation by age, gender, and race. Ophthal Plast Reconstr Surg 2013;29(6):475-480.
11 Estes JL, Tsiouris AJ, Christos PJ, Lelli GJ. Three-dimensional volumetric assessment of the nasolacrimal duct in patients with obstruction. Ophthal Plast Reconstr Surg 2015;31(3):211-214.
12 Bulbul E, Yazici A, Yanik B, Yazici H, Demirpolat G. Morphometric evaluation of bony nasolacrimal canal in a caucasian population with primary acquired nasolacrimal duct obstruction: a multidetector computed tomography study. Korean J Radiol 2016;17(2):271-276.
13 Schneider CA, Rasband WS, Eliceiri KW. NIH Image to Image J: 25 years of image analysis. Nat Methods 2012;9:671-675.
14 Rha EY, Kim MJ, Yoo G. Volume measurement of various tissues using the image J softwar. J Craniofac Surg 2015;26(6):505-506.
15 McCormick A, Sloan B. The diameter of the nasolacrimal canal measured by computed tomography: gender and racial differences. Clin Exp Ophthalmol 2009;37(4):357-361.
16 Fasina O, Ogbole GI. CT assessment of the nasolacrimal canal in a black African Population. Ophthal Plast Reconstr Surg 2013;29(3):231-233.
17 Lamping K, Levine MR. Jones’ tubes. How good are they? Arch Ophthalmol 1983;101(2):260-261.
18 Paulsen FP, Thale AB, Maune S, Tillmann BN. New insights into the pathophysiology of primary acquired dacryostenosis. Ophthalmology 2001;108(12):2329-2336.
19 Janssen AG, Mansour K, Bos JJ, Castelijns JA. Diameter of the bony lacrimal canal: normal values and values related to nasolacrimal duct obstruction:assessment with CT. AJNR Am J Neuroradiol 2001;22(5): 845-850.
20 Zhang CY, Wu Q, Cui YH, Yu G. Anatomy of nasolacrimal canal in congenital nasolacrimal duct obstruction-18 cases retrospective study.Acta Ophthalmol 2015;93(5):e404-e405.
21 Moscato EE, Kelly JP, Weiss A. Developmental anatomy of the nasolacrimal duct: implications for congenital obstruction. Ophthalmology 2010;117(12):2430-2434.
22 Zapala J, Bartkowski AM, Bartkowski SB. Lacrimal drainage system obstruction: management and results obtained in 70 patients. J Craniomaxillofac Surg 1992;20(4):178-183.
23 Vatansever M, Argin MA, Görür K. Effect of facial parameters in primary acquired nasolacrimal duct obstruction. J Craniofac Surg 2017;28(8):e752-e756.