Table 1 The comparison of baseline characteristics between two groups n (%)
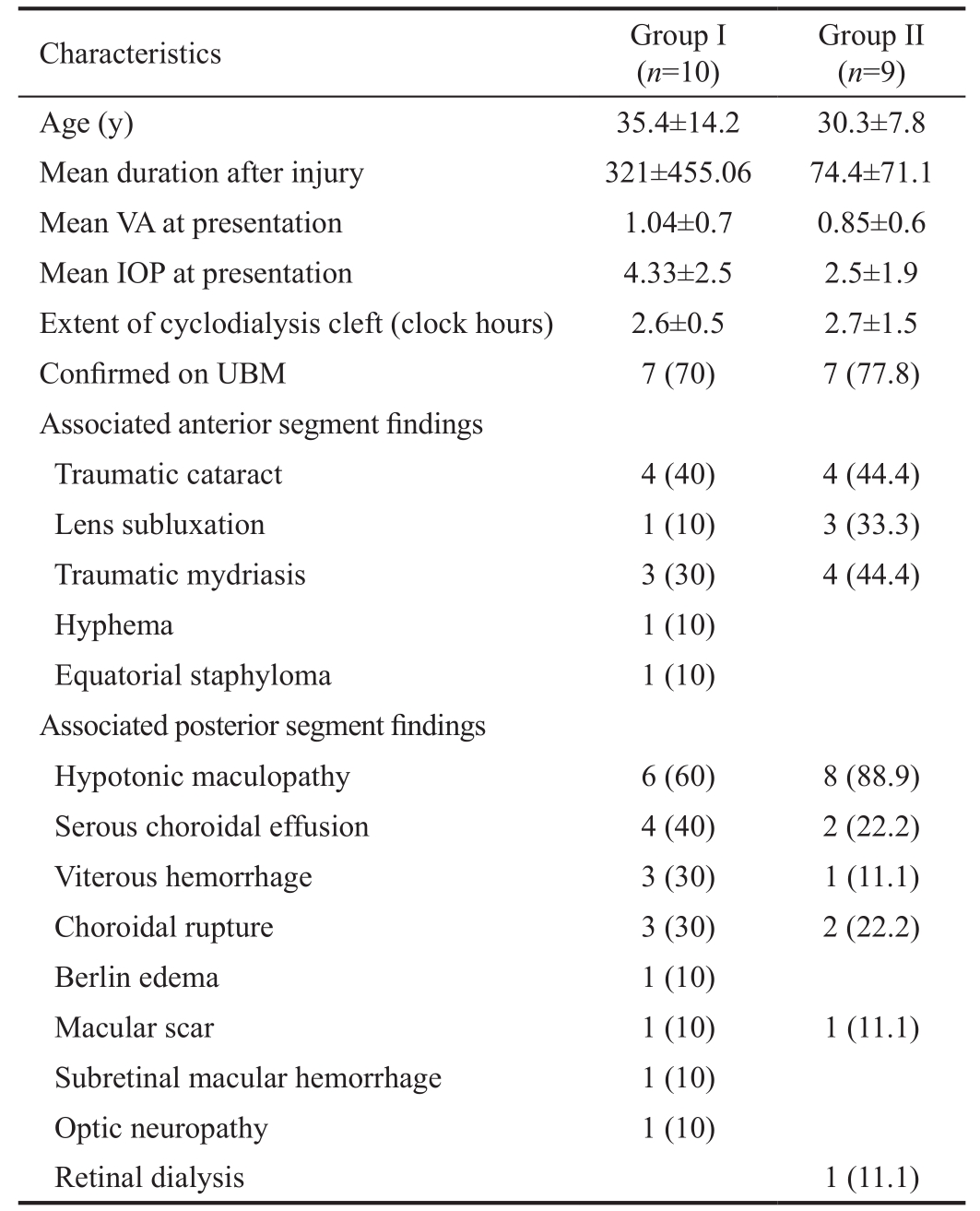
UBM: Ultrasound biomicroscopy; VA: Visual acuity; IOP: Intraocular Pressure; n: number. P>0.05 between baseline parameters in the two groups.
?
Post-traumatic cyclodialysis cleft is the separation of ciliary body from the sclera spur after a blunt trauma which results in an unrestricted flow of aqueous into the suprachoroidal space and decreased aqueous production by detached ciliary body; resulting in hypotony and its deleterious sequelae[1-3]. Spontaneous closure of the cleft is a rare occurrence and seems to occur only with smaller clefts[4].
Treatment options which have been tried in traumatic cyclodialysis cleft include mydriatics[5], ciliochoroidal diathermy[6], direct cyclopexy[7-8], indirect cyclopexy[9],anterior scleral buckling[10], cryoablation[11], argon laser photocoagulation[3,12], combined vitrectomy, cryotherapy and gas tamponade[13], trans-scleral YAG[14] or diode laser[15],microendoscopic endophotocoagulation, or transcleral diode photocoagulation under microendoscopic view[16]. However,all these techniques have been described as case reports or case series. The techniques have also not been compared in terms of anatomical and functional success rates.
Portney and Puncell[17] proposed the idea of anterior buckling to treat hypotony in cyclodialysis cleft. They had placed a segmental silicone rod under the partial thickness scleral flap over the entire extent of the cleft. Mandava et al[10] modified the technique by using a sponge which was removed after 3wk.The aim of the present study is to report a novel technique of using a 360 degree encirclage in combination with cryopexy to the extent of cleft for patients with hypotony due to traumatic cyclodialysis cleft and compare this technique with conventional laser photocoagulation.
Ethical Approval Institutional review board approval was obtained to analyze the hospital-based data and Declaration of Helsinki was followed. Patients had given written informed consent to be part of study or any clinical trial prior to intervention, and they received no stipend for that.
Study Design and Patient Eligibility Between March 1998 to March 2016, a retrospective chart review was done to identify cases with traumatic cyclodialysis cleft who had undergone either encirclage with trans-scleral cryopexy or argon laser treatment for the cleft; and fulfilled the eligibility criteria. Patients with history of blunt trauma who presented with hypotony and had been diagnosed with cyclodialysis cleft on gonioscopy +/- ultrasound biomicroscopy (UBM) were included in the study. Exclusion criterion was concomitant vitreoretinal surgery, spontaneous closure or closure by direct suturing of clef.
Collected data included detailed history of nature of trauma,demographic features, duration of trauma; best corrected visual acuity, intraocular pressure (IOP), and associated anterior and posterior segment abnormalities. During final follow-up,after the intervention, the end points that were considered for anatomical success included: a rise of IOP to ≥6 mm Hg, cleft closure on gonioscopy and cleft closure on UBM. Additionally,best corrected visual acuity and any additional procedures,which were done after the primary procedure, were noted.
Surgical Methodology Group I (belt buckle+trans scleral cryopexy): Under local anaesthesis, the conjunctival periotomy was done and all four recti were tagged using 4-0 silk.Sclera tunnels were made anteriorly, within 1 mm of muscle insertion and encircling band (#240, MIRA, USA) was placed.The region of cyclodialysis cleft was either localized using transillumination at the pupil or based on gonioscopy clock hours. Transsclerlal cryotherapy was performed about 1 mm from the limbus to cleft site (Frigitonic Cryoprobe). The encirclage was tightened to have a mild buckle indentation to mechanically appose the cleft and the conjunctiva was closed. One patient required an additional sclera patch graft for managing the staphyloma. In 2 patients at the end of the procedure, intraocular gas (0.3 mL) was injected (air and pure Arceole C3F8 one each).
Group II (argon laser): Under topical 0.05% proparacaine goniolens was placed on eye. No viscoelastic was injected to form the anterior chamber. Laser treatment was applied to both the edges and the depth of the cleft, blanching the tissue. Spot size used was 150-300 µm, duration 0.1-0.5s and power 300-1000 mW. After procedure topical atropine was prescribed to all patients to achieve a mechanical apposition for 2wk. If there was no significant apposition, the procedure was repeated after 1mo.
Outcome Measures We analyzed the anatomical and functional outcome of the patients. Anatomical outcome was build up in the IOP more than 6 mm Hg or the closure of cleft on gonioscopy or on UBM. Visual outcome was the change in visual acuity and analyzing the causes of decreased vision.
Statistical Analysis Categorical variables within groups were compared using Fisher’s exact test or the Chi-square test.Quantitative variables were summarized by means and other descriptive statistics. Groups were compared using Mann-Whitney test.
Of the 19 eyes, in 16 eyes gonioscopy could be done and cleft identifies, however, in 3 eyes gonioscopy was difficult due to hypotony and the diagnosis and extent of was ascertained on UBM. Of the 19 eyes, 10 were in Group I and 9 were in the Group II (Table 1).
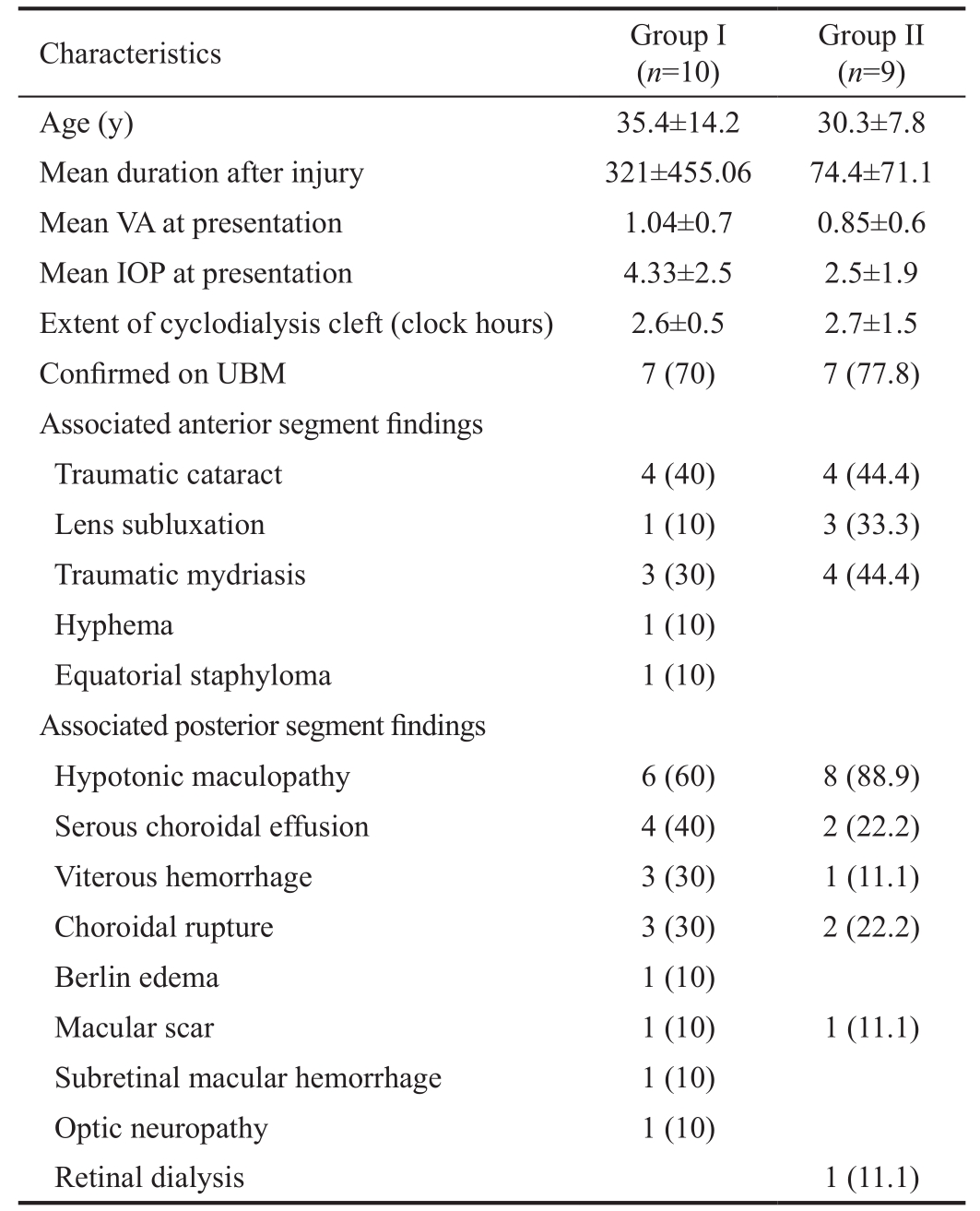
The two groups had no statistically significant difference between baseline characteristics like age, mean duration after injury, mean visual acuity at presentation, mean IOP at presentation and extent of cleft in clock-hours (P>0.05). Figure 1 shows the flowchart showing closure pattern of cleft of patients in Group I and Group II.
Table 1 The comparison of baseline characteristics between two groups n (%)
UBM: Ultrasound biomicroscopy; VA: Visual acuity; IOP: Intraocular Pressure; n: number. P>0.05 between baseline parameters in the two groups.
?
There was a statistically significant improvement in both groups, from 1.04 to 0.42 logMAR (P=0.01) in Group I and from 0.85 to 0.40 logMAR (P=0.03) in Group II. However,the visual results were comparable in between the groups(P=0.92). The diverse causes of reduced vision included macular scar, choroidal rupture, cataract and optic neuropathy.In Table 2 we mention the anatomical results in two groups along with any other intervention being contemplated.
This article describes a novel technique of encirclage with transscleral cryotherapy for the management of traumatic cyclodialysis cleft which was compared with the conventional Argon laser. The technique of encirclage with transscleral cryotherapy was found to result in anatomical closure in 90%of cases. There was a statistically significant improvement from 1.04 logMAR to 0.42 logMAR in this group of patients.The anatomical and visual success was comparable with the laser group.
In our study, the diagnosis of cleft was based on gonioscopy and in majority of cases was confirmed on UBM. However,Ioannidis et al[18] in their series used intracameral injection of 0.1-0.2 mL of viscoelastic, and then repeating the gonio in cases where the gonioscopy was difficult. Hwang et al[19]successfully identified all clefts in 32 cases in their series using UBM as the primary diagnostic modality. UBM and ASOCT are both non invasive procedures that can diagnose the cleft with certainity.
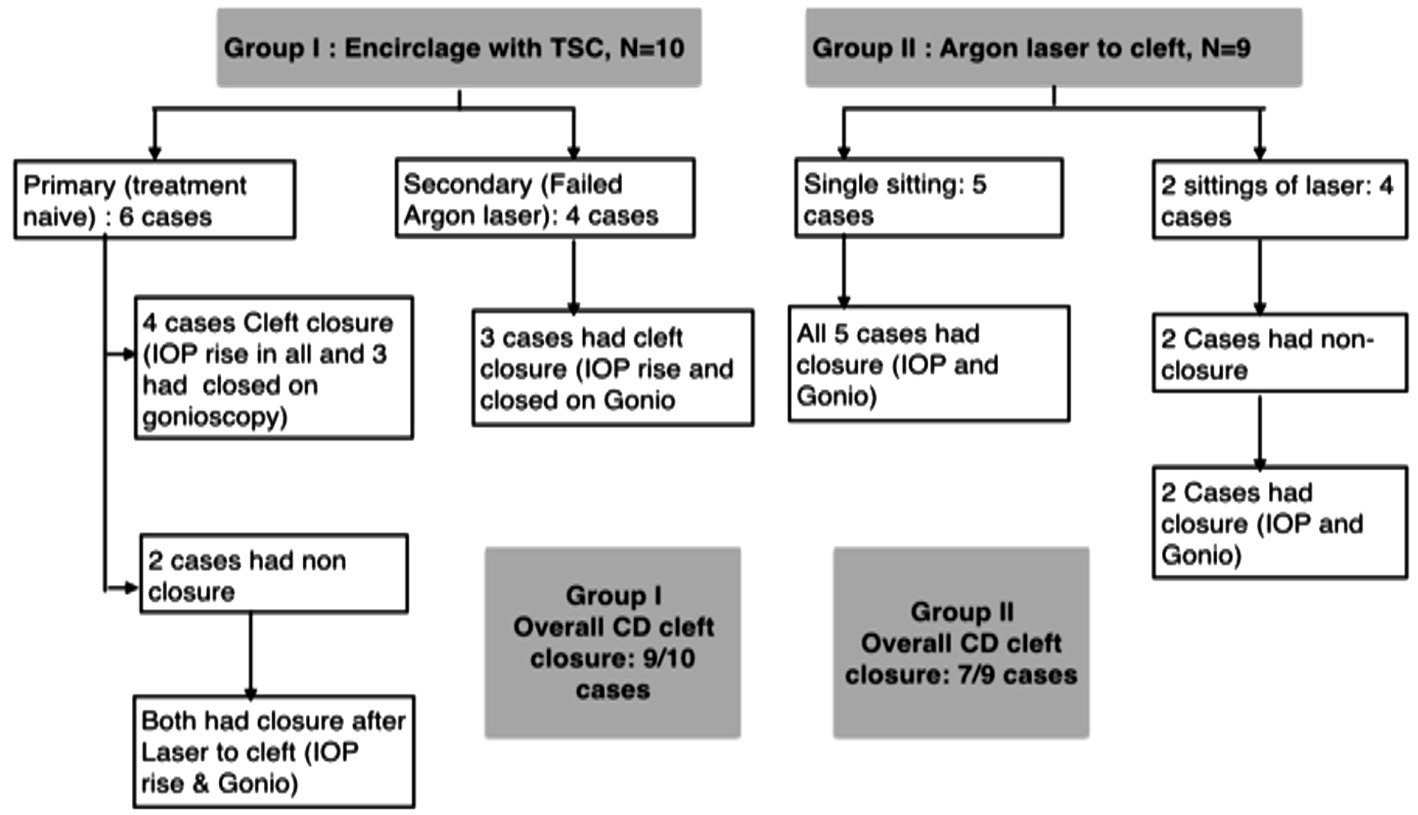
Figure 1 Flowchart showing closure pattern in Group I and II.
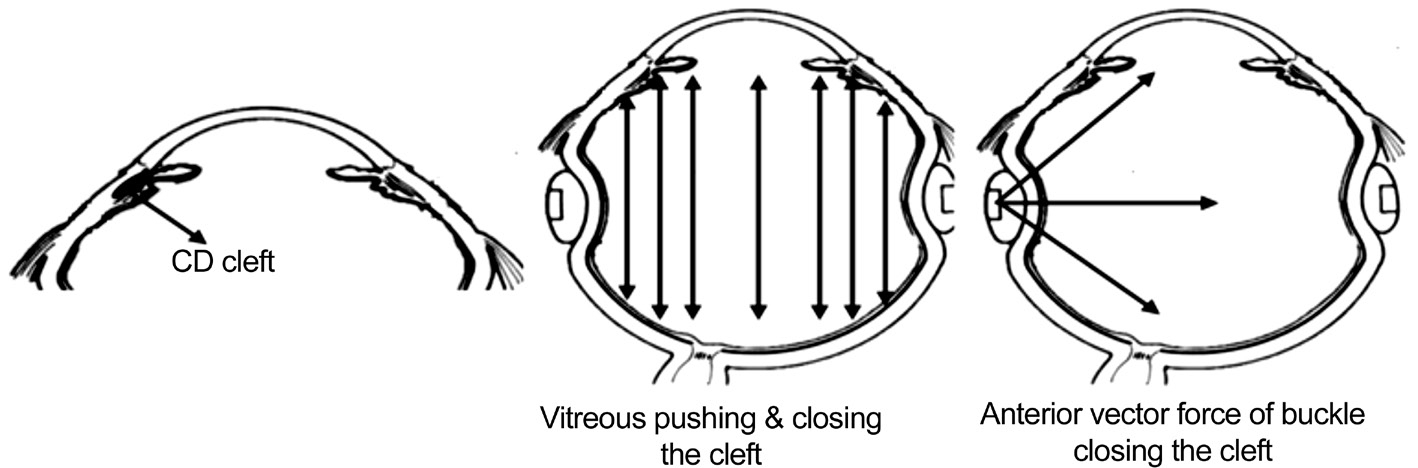
Figure 2 Possible mechanism of action of encirclage to close cyclodialysis cleft.
Table 2 The anatomical results of Group I and II and also shows the additional procedures done for cataract and subluxation of lens in both the groups n (%)
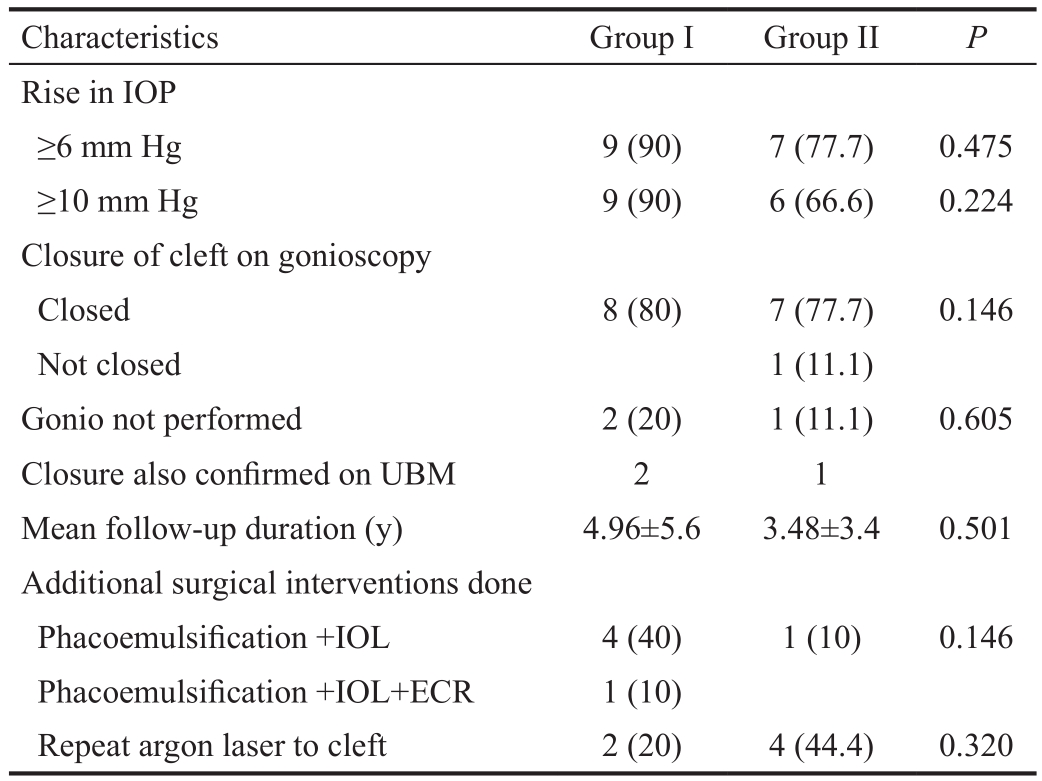
IOP: Intraocular pressure; UBM: Ultrasound biomicroscopy; IOL:Intraocular lens; ECR: Endocapsular ring.
Characteristics Group I Group II P Rise in IOP≥6 mm Hg 9 (90) 7 (77.7) 0.475≥10 mm Hg 9 (90) 6 (66.6) 0.224 Closure of cleft on gonioscopy Closed 8 (80) 7 (77.7) 0.146 Not closed 1 (11.1)Gonio not performed 2 (20) 1 (11.1) 0.605 Closure also confirmed on UBM 2 1 Mean follow-up duration (y) 4.96±5.6 3.48±3.4 0.501 Additional surgical interventions done Phacoemulsification +IOL 4 (40) 1 (10) 0.146 Phacoemulsification +IOL+ECR 1 (10)Repeat argon laser to cleft 2 (20) 4 (44.4) 0.320
Though various methods have been tried till date for management of cyclodialysis cleft, the success of these methods have been evaluated and presented as case reports to case series.
However, there are no studies comparing these methods.Portney and Puncell[17] have described use of segmental anterior buckling implant to treat hypotony in cyclodialysis cleft in a case report. A slight modification was proposed by Mandava et al[10], who used a temporary sponge explant, which was removed after 3wk.
Argon laser, a conventional treatment modality in management of small clefts (<4 clock hours), has been evaluated in many case series[5,18]. Ioannidis et al[18] have postulated the laser is unsuccessful unless apposition of the ciliary body band to sclera can be achieved. We found that the laser group had a functional success rate of 66.6% (rise in IOP) to 77.7%(closure of cleft). But in terms of visual outcome, there was no statistical difference in two groups.
Scleral buckle is being used in the retinal detachment surgery for achieving an anatomic approximation between the detached neurosensory retina and the retinal pigment epithelium choroid complex. There can be multiple factors responsible for approximation of the cleft. The indentation of the encirclage pushes the vitreous in the anteroposterior direction; the anterior force can thereby approximate the cleft. Likewise,the tangential vector force due to the encirclage could act in a way to approximate the cleft. Hammer[20] have described the forces which help in retinal reattachment after scleral buckling and suggested that the scleral buckle reverses the direction of the radial inward force on the retina to an outward force,thereby promoting retinal reattachment of a detached retina.Likewise, the outward force of the vitreous could have closed the cleft (Figure 2). Further adhesion between the two layers was augmented by using transcleral cryotherapy causing in flammatory reaction and in long term scarring at the site[13,21].In our series, in cases where encirclage was used as a primary procedure, 2 of the 6 had non-closure, which subsequently closed after laser. The extent of cleft was similar in the ones which closed and the ones which didn’t close; however, they were younger (mean age: 19y) as compared to others (mean age: 42.5y). It could probably be the inelastic vitreous in the younger age group, which could not exert the anterior force to allow approximation. Similarly in the patients who had failed laser, 3 of the 4 cases closed by encirclage. The one which didn’t close was similar to others in respect to age, duration of cleft, and extent of cleft.
Thus, this novel technique seems to have a role in the management of traumatic cyclodialysis cleft and is comparable in terms of anatomical and functional success with the conventional argon laser. However, encirclage seems to have a possible advantage of a single procedure (in the laser group,44% needed additional laser to close the cleft). Also encirclage can be used as second procedure, in patients where laser had failed.
The study has several strengths. It describes a novel and effective technique which is comparable to laser treatment.The comparison of techniques has not been previously done.However, the study has few limitations. The retrospective design and smaller sample in each group are important limitations. The two groups though comparable in baseline characteristics but all cases in Group I were not treatment naive cases and two received additional laser after encirclage thus the overall success in this group would have been lower if encirclage was used as isolated procedure. Also, it is difficult to ascertain whether cryopexy alone could have been equally effective. A larger randomized trial could probably give the answer to it and may help the treating ophthalmologists to make the best choice in cyclodialysis cleft.
Conflicts of Interest: Sood G, None; Rajendran V, None;George R, None; Sharma T, None; Raman R, None.
1 Shaffer RN, Weiss DI. Concerning cyclodialysis and hypotony. Arch Ophthalmol 1962;68(1):25-31.
2 Pederson JE, Gaasterland DE, MacLellan HM. Experimental ciliochoroidal detachment; effect of intraocular pressure andaqueous humor flow. Arch Ophthalmol 1979;97:536-541.
3 Ormerod LD, Baerveldt G, Green RL. Cyclodialysis clefts: natural history, assessment and management. In: WeinsteinGW (ed). Open Angle Glaucoma Churchill Linvingstone:New York,1986:pp201-225.
4 Gnanaraj L, Lam WC, Rootman DR, Levin AV. Endoscopic closure of a cyclodialysis cleft. J AAPOS 2005;9:592-594.
5 Ormerod LD, Baerveldt G, Sunalp MA, Riekhof FT. Management of the hypotonous cyclodialysis cleft. Ophthalmology 1991;98(9):1384-1393.
6 Edward Maumenee A, Stark WJ. Management of persistent hypotony after planned or inadvertent cyclodialysis. Am J Ophthalmol 1971;71(1):320-327.
7 Metrikin DC, Allinson RW, Snyder RW. Transcleral repair of recalcitrant, inadvertent, postoperative cyclodialysis cleft. Ophthalmic Surg 1994;25:406-408.
8 Küchle M, Naumann GOH. Direct cyclopexy for traumatic cyclodialysis with persisting hypotony report in 29 consecutive patients. Ophthalmology 1995;102(2):322-333.
9 McCannel MA. A retrievable suture idea for anterior uvea problems.Ophthalmic Surg 1976;7:98-103.
10 Mandava N, Kahook MY, Mackenzie DL, Olson JL. Anterior scleral buckling procedure for cyclodialysis cleft with chronic hypotony.Ophthalmic Surgery, Lasers & Imaging 2006;37(2):151-153.
11 Krohn J. Cryotherapy in the treatment of cyclodialysis cleft induced hypotony. Acta Ophthalmol Scand 2009;75(1):96-98.
12 Harbin TS. Treatment of cyclodialysis clefts with argon laser photocoagulation. Ophthalmology 1982;89(9):1082-1083.
13 Hoerauf H, Roider J, Laqua H. Treatment of traumatic cyclodialysis with vitrectomy, cryotherapy, and gas endotamponade. J Cataract Refract Surg 1999;25:1299-1301.
14 Brooks AMV, Troski M, Gillies WE. Noninvasive closure of a persistent cyclodialysis cleft. Ophthalmology 1996;103(11):1943-1945.
15 Amini H, Razeghinejad M. Transscleral diode laser therapy for cyclodialysis cleft induced hypotony. Clin Exp Ophthalmol 2005;33(4):348-350.
16 Saha N, MacNaught AI, Gale RP. Closure of cyclodialysis cleft using diode laser. Eye (Lond) 2003;17(4):527-528.
17 Portney GL, Purcell TW. Surgical repair of cyclodialysis induced hypotony. Ophthalmic Surg 1974;5:30-32.
18 Ioannidis AS, Bunce C, Barton K. The evaluation and surgical management of cyclodialysis clefts that have failed to respond to conservative management. Br J Ophthalmol 2014;98(4):544-549.
19 Hwang JM, Ahn K, Kim C, Park KA, Kee C. Ultrasonic biomicroscopic evaluation of cyclodialysis before and after direct cyclopexy. Arch Ophthalmol 2008;126(9):1222-1225.
20 Hammer ME. Retinal reattachment forces created by absorption of subretinal fluid. Doc Ophthalmol Proc Ser 1981;25:61-75.
21 Krohn J. Cryotherapy in the treatment of cyclodialysis cleft induced hypotony. Acta Ophthalmol Scand 1997;75(1):96-98.