
Citation: Yang J, Zhang H, Yang XT, Tian F, Zhao SZ. Accuracy of
corneal astigmatism correction with two Barrett Toric calculation methods. Int
J Ophthalmol
2019;12(10):1561-1566. DOI:10.18240/ijo.2019.10.07
·Clinical Research·
Accuracy
of corneal astigmatism correction with two Barrett Toric calculation methods
Jun Yang, Hong Zhang, Xiao-Tong Yang, Fang Tian,
Shao-Zhen Zhao
Tianjin Medical University Eye
Hospital, Tianjin Medical University Eye Institute & Tianjin Medical
University School of Optometry and Ophthalmology, Tianjin 300384, China
Correspondence to: Fang Tian and Shao-Zhen Zhao.
Tianjin Medical University Eye Hospital, Tianjin Medical University Eye
Institute & Tianjin Medical University School of Optometry and
Ophthalmology, Tianjin 300384, China. tianfang1216@126.com; zhaosz1997@sina.com
Received:
Abstract
AIM: To compare the prediction error between Barrett Toric calculator and the
new online AcrySof Toric calculator which incorporated Barrett astigmatism
algorithm in Chinese cataract eyes with normal axial length and anterior
chamber depth (ACD).
METHODS: Prospective case-control study. All the cases had
axial length (21
RESULTS: The |EM| obtained at 1mo after surgery were
0.21±0.12 D, 0.22±0.18 D in group 1 and group 2 respectively, and
correspondingly turned to be 0.19±0.13 D, 0.20±0.19 D at 3mo after surgery,
with no statistical difference (P=0.633, P=0.877). The vector
analysis showed that |EV| values in two groups at 1mo after surgery were
0.29±0.14@105 (D@angle) and 0.35±0.20@113 (D@angle), respectively, whereas |EV|
values 3mo after surgery were 0.27±0.16@86 (D@angle) and 0.32±0.23@102
(D@angle), respectively. The differences between the groups were not
statistically significant (P=0.119, P=0.261).
CONCLUSION: The clinical effect of Barrett Toric calculator has
a much more accurate tendency than that of new online AcrySof Toric calculator,
but is not evident in cases with normal axial length and normal anterior
posterior ratio.
KEYWORDS: Barrett Toric online calculator;
intraocular lens; vector analysis
DOI:10.18240/ijo.2019.10.07
Citation:
Yang J, Zhang H, Yang XT, Tian F, Zhao SZ. Accuracy of corneal astigmatism
correction with two Barrett Toric calculation methods. Int J Ophthalmol 2019;12(10):1561-1566
INTRODUCTION
Corneal astigmatism is one of the
important factors limiting uncorrected visual acuity after cataract surgery,
which can considerably affect visual quality. For astigmatic correction during
cataract surgery, toric intraocular lenses (IOLs) implantation has been shown
to be effective and predictable[1]. Several
clinical studies have shown that toric IOL has a wide range of astigmatism
correction spectrum, which can substantially reduce the residual astigmatism
after cataract surgery and improve the patient satisfaction and the distant
spectacle independence[2]. However, after the
toric IOL implantation, some patients still had residual astigmatism[3-4]. The underlying reasons for this
are a matter of some controversy. IOL tilt, IOL rotational misalignment, and
unexpected surgically induced astigmatism (SIA) all contribute to prediction
errors. However, correcting for these factors does not always explain the error
of the postoperative astigmatic outcome[4-5].
Moreover, successful correction of preexisting astigmatism requires accurate
calculation for the required toric IOL cylinder power and axis of alignment.
The original online toric calculator by Alcon uses a fixed ratio to calculate
the estimated IOL toric power at the corneal plane[5].
Barrett calculator is mounted in recent years, both in ASCRS and APACRS,
developed by Prof. Barrett’s team using a Universal II formula and adjusts the
cylindrical power and axis of alignment for the IOL with the employment of a
mathematic model to accommodate value of the posterior corneal surface. To
overcome the limitation of the initial calculator, Alcon Laboratories, Inc.
incorporates the astigmatic algorithms in Barrett Toric calculator. However,
the spherical power calculation is not recruited. Any formula can be used as
doctors used to. Whether the tiny difference between the two calculators could
deliver different outcome has not yet been clarified. To investigate it, the
Barrett Toric calculator and new online AcrySof Toric calculator were adopted
to decide the type and axis of toric IOL (Acrysof IQ), and then evaluate their
influences on the astigmatic correction effect.
SUBJECTS AND METHODS
Ethical Approval The study was conducted in
accordance with the Declaration of Helsinki and was approved by Tianjin Medical
University Eye Hospital (TMUEC; No.ChiCTR1800019682). All patients had been
fully informed of the purpose and methods of the present study and provided
written informed consent from themselves or their guardians.
Patient Population Patients who underwent cataract
removal by phacoemulsification were included. Preoperative measurements of
corneal astigmatism with LenSTAR 900 (HAAG-STREIT, USA) were performed, and
patients with corneal astigmatism greater than 0.75 D were enrolled. Corneal
topography (OCULUS PENTACAM, Germany) is used to evaluate the irregular corneal
astigmatism. Exclusion criteria were as followed: irregular astigmatism of
cornea, axial length (AL) >
Preoperative Examination All patients had full preoperative
ophthalmologic examinations, including uncorrected distance visual acuity and
corrected distance visual acuity using logMAR acuity charts at
In group 1, the toric IOL is
calculated by logging in APACRS and choosing Barratt Toric calculator. In group
2, the IOL spherical power was calculated using the SRK-T formula. The IOL
cylindrical power was calculated using the Alcon new online calculator and
automated keratometry (OLCR device). The A-constant was 119.2. The refractive
goal was emmetropia.
Surgical Technique Before surgery, limbus horizontal
meridian was marked by a special marker (copyright By professor Zhang H) after
topical anesthesia with the patient seated to prevent cyclotorsion. Then the
precalculated toric axis was marked on the basis of horizontal meridian when
the patient lay down. All surgeries were performed by an experienced cataract
specialist using topical anesthesia and a micro coaxial phacoemulsification
technique with a superior
Postoperative Examinations At 1 and 3mo after surgery, a subjective
optometry was performed by cross cylinder method, and the toric IOL axial
position was examined after mydriasis.
Postoperative Calculation The refractive power was converted from
the spectacle plane to the corneal plane in accordance with the vertex
distance. The conversion method is as follows[6]:
Ccorn=(Sspect+Cspect)/[1-V×(Sspect+Cspect)]-Sspect/(1-V×Sspect)
[Ccorn represents the
concave-cylinder diopter of the corneal surface, Sspect is the
spherical lens diopter of the glasses plane, Cspec denotes the concave-cylinder
diopter of the glasses plane, and V indicates the vertex distance (in mm)].
Error of refractive astigmatism
(ERA)=postoperative residual astigmatism (PRA; corneal surface)-predicted residual astigmatism
(corneal surface). Error vector (EV) is the vector deviation of ERA. Error
magnitude (EM) is the algebraic deviation of ERA.
Vector Analyses The PRA is decomposed into X and Y
components by vector transformation.
Xra=Cra×cos(2×Ara);
Yra=Cra×sin(2×Ara)
(1)
Xpra=Cpra×cos(2×Apra);
Yra=Cpra×sin(2×Apra)
(2)
(Ccorn represents the
diopter of the concave-cylinder, and A indicates the axial direction of the
concave-cylinder.)
YEV=Yra-Ypra,
XEV=Xra-Xpra;
(3)
|EV|=[(Xra-Xpra)²+(Yra-Ypra)²]1/2
(4)
θera=0.5×arctan (YEV/XEV)
(5)
Statistics Analysis The statistical analysis was undergone by
SPSS 22.0 software. The measurement data of normal distribution was expressed
as mean±standard deviation. After vector analysis, the ERA, EM, and EV values
between the two groups were compared using the independent sample t
test. P<0.05 was considered as statistically significant difference.
RESULTS
A total of 74 cases (74 eyes)
underwent phacoemulsification in Tianjin Medical University Eye Hospital were
randomized to two groups. Group 1 was Barrett Toric calculator including 36
cases (36 eyes), group 2 was new online AcrySof calculator with 38 cases (38
eyes). Five patients were lost to follow-up. The cases consisted of 33 males
(33 eyes) and 36 females (36 eyes) at the ages of 51-91y, with the average age
of 72±10y. The difference between two groups was not statistically significant
(χ2=0.357, P=0.473, t=-0.507, P=0.614),
as shown in Table 1. Among 69 eyes included in this study, 11 eyes (15.94%) had
with-the-rule (WTR) astigmatism, 47 eyes (68.12%) had against-the-rule (ATR)
astigmatism, and 11 eyes (15.94%) had oblique astigmatism. The implantation of
SN60T2, SN60T3, SN60T4, SN60T5, SN60T6, SN60T7, and SN60T8 were 1 eye (1.45%),
20 eyes (28.99%), 29 eyes (42.03%), 7 eyes (10.14%), 10 eyes (14.49%), 1 eye
(1.45%), and 1 eye (1.45%), respectively. No statistically significant
difference was found between the two groups in preoperative ocular biometry, such
as AL (P=0.099), ACD (P=0.556), and corneal astigmatism (P=0.599).
After surgery, IOL axis alignment in both groups were all <5° (Barrett group
1.89°±1.05°, New Alcon group 1.97°±0.97°), of which the difference has no
statistical significance (t=-0.349, P=0.729). Table 1 shows the
preoperative ocular parameter.
Table 1 Preoperative ocular
parameters of two groups
|
Groups |
Gender |
Age |
AL (mm) |
ACD (mm) |
Corneal astigmatism (D) |
IOL spherical equivalent (D) |
|
|
M |
F |
||||||
|
Total |
33 |
36 |
72±10 |
24.46±2.30 |
3.19±0.50 |
1.64±0.58 |
19.80±4.97 |
|
Barrett group |
15 |
20 |
71±11 |
23.81±2.20 |
3.12±0.49 |
1.60±0.63 |
20.14±5.22 |
|
New Alcon group |
18 |
16 |
73±9 |
24.67±2.06 |
3.18±0.45 |
1.67±0.52 |
19.51±4.69 |
|
t/χ2 |
0.357 |
-0.507 |
-1.674 |
-0.592 |
-0.529 |
0.525 |
|
|
P |
0.473 |
0.614 |
0.099 |
0.556 |
0.599 |
0.601 |
|
AL: axial length; ACD: Anterior
chamber depth.
The ERA Comparison
Comparison of |EM| obtained by the
two groups The |EM| obtained from the Barrett
calculator group 1mo and 3mo after surgery were 0.21±0.12 D and 0.19±0.13 D,
respectively. Simultaneously, |EM| in the new online AcrySof calculator group 1
and 3mo after surgery were 0.22±0.18 D and 0.20±0.19 D, respectively. The
difference between the groups was not statistically significant (t=-0.480,
-0.156, P=0.633, 0.877), as shown in Tables 2 and 3.
Table 2 Comparison of |EM|, EV, |XEV|,
and |YEV| of the two groups 1mo after surgery
|
Groups |
|EM| (D) |
EV (D@angle) |
|XEV| (D) |
|YEV| (D) |
|
Barrett group |
0.21±0.12 |
0.29±0.14@105 |
0.04±0.27 |
0.13±0.13 |
|
New Alcon group |
0.22±0.18 |
0.35±0.20@113 |
0.23±0.18 |
0.21±0.20 |
|
t |
-0.480 |
-1.581 |
-3.426 |
-2.157 |
|
P |
0.633 |
0.119 |
0.001 |
0.035 |
EM: Error magnitude; EV: The vector
deviation of ERA (error of refractive astigmatism); XEV: X components of EV by
vector transformation; YEV: Y components of EV by vector transformation.
Table 3 Comparison of |EM|, EV, |XEV|,
and |YEV| of the two groups 3mo after surgery
|
Groups |
|EM| (D) |
EV (D@angle) |
|XEV| (D) |
|YEV| (D) |
|
Barrett group |
0.19±0.13 |
0.27±0.16@86 |
0.22±0.13 |
0.13±0.13 |
|
New Alcon group |
0.20±0.19 |
0.32±0.23@102 |
0.22±0.22 |
0.18±0.17 |
|
t |
-0.156 |
-1.133 |
-0.052 |
-1.442 |
|
P |
0.877 |
0.261 |
0.959 |
0.154 |
EM: Error magnitude; EV: The vector
deviation of ERA (error of refractive astigmatism); XEV: X components of EV by
vector transformation; YEV: Y components of EV by vector transformation.
Comparison of |EV| obtained by the two
groups At 1mo after surgery,
the total |EV| obtained from group 1 was 0.29±0.14 D, whereas that of group 2
was 0.35±0.20 D, which showed no statistically significant difference (t=-1.581,
P=0.119). At 3mo after surgery, the total |EV| obtained by the two
groups were 0.27±0.16 D, 0.32±0.23 D, respectively, which has no statistically
significant difference (t=-1.133, P=0.261), as shown in Tables 2
and 3.
The EV of the two groups was
decomposed into two vectors and compared. At 1mo after surgery, the difference
in both X and Y was statistically significant (t=-3.426, P=0.001;
t= -2.157, P=0.035). At 3mo after surgery, the difference was not
statistically significant (t=-0.052, P=0.959; t=-1.442, P=0.154),
as shown in Tables 2 and 3.
Figure 1 presented the EV
distribution of the two groups in double angle plot. In group 1, patients with
|EV| less than 0.5 D at 1 and 3mo after surgery accounted for 88.57% (31 eyes)
and 88.57% (31 eyes), respectively. However, in group 2, patients with |EV| less
than 0.5 D at 1 and 3mo postoperatively occupied 76.47% (26 eyes) and 82.35%
(28 eyes), respectively.
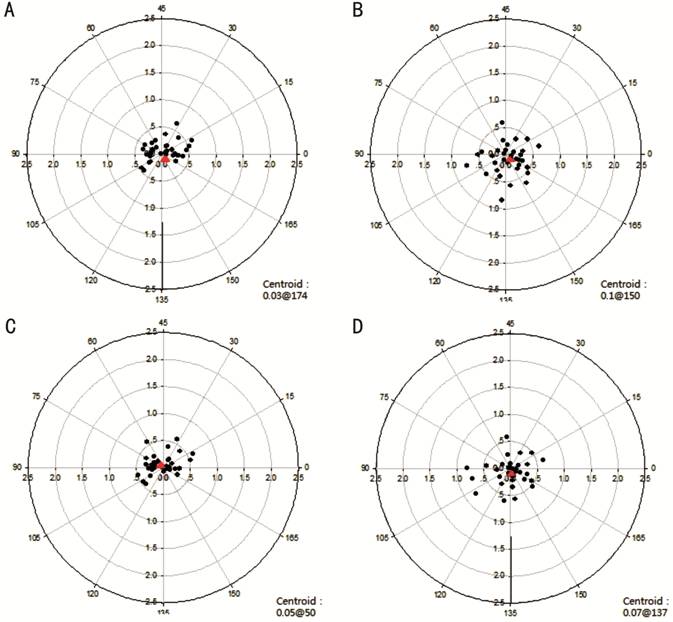
Figure 1 The EV distribution of both
groups A: Barrett calculator 1mo after surgery;
B: New online AcrySof calculator 1mo after surgery; C: Barret calculator group
3mo after surgery; D: New online AcrySof calculator 3mo after surgery (The
black dots represent the vector coordinates of EV of each eye, and the red dots
indicate the centroids).
DISCUSSION
Corneal astigmatism can
significantly impair the visual acuity in phakic and pseudophakic eyes[7]. Corneal astigmatism is not rare in cataract patients.
Between 15% and 29% of cataract patients have more than 1.5 D of keratometric
astigmatism[8-9]. Without proper
correction of corneal astigmatism, postoperative vision, and visual quality of
cataract patients will be considerably affected[10].
The results toric IOL are not always
predictable. Optimum correction of astigmatism requires accurate measurement,
meticulous alignment of the toric IOL, and appropriate calculations. Recent
studies support considering the predicted effective lens position (ELP),
spherical power of the IOL, and posterior corneal surface to achieve precise
results when implanting toric IOLs. To overcome the calculating pitfalls, the
Baylor nomogram and Barrett Toric calculator were introduced to adjust toric
IOL power to account for posterior corneal astigmatism by regression analysis
and theoretical model. The ASCRS and APACRS has introduced the Barrett Toric
calculator including astigmatism analysis and spherical power calculation. The
Alcon initial calculator is upgraded with Barrett astigmatism algorithm which
considers the posterior corneal astigmatism. The aim of our study was to
evaluate the accuracy of predicting toric IOL cylinder power by comparing the 2
toric IOL calculators.
In accordance with literature
reviews, patients with |EV| less than 0.5 D who used the old AcrySof online
calculator accounted for 31.3%-35.3%[11]. In the
Barrett Toric calculator group, patients with |EV| less than 0.5 D 1 and 3mo
after surgery accounted for 88.57% and 88.57%, respectively. In the new online
AcrySof Toric calculator group, patients with |EV| less than 0.5 D 1 and 3mo
after surgery accounted for 76.47% and 82.35%. Therefore, not only by Barrett
Toric calculator but also new online AcrySof calculator can achieve more
accuracy than that by the old AcrySof calculator.
Several studies have discovered that
the posterior corneal astigmatism is 0.26-0.78 D, with steeper curvature in
vertical meridian, which will have a negative power to the total corneal
astigmatism[12-14]. Therefore,
the inclusion of the posterior corneal surface in the calculation of these IOLs
is now considered relevant because ignoring it results in overcorrection in
eyes with WTR astigmatism and undercorrection in eyes with ATR astigmatism. The
old AcrySof calculator used simulated K values (simK) derived from assumption
that the cornea is 500 μm thick and the anterior/posterior radius is fixed to 0.82,
which cannot entirely reflect the overall corneal astigmatism[15-16]. The Barrett corneal
astigmatism algorithm is set up in a mathematical model based on big data. The
anterior corneal astigmatism is used to estimate the posterior corneal
astigmatism, so as to obtain the total corneal astigmatism, which is much more
reasonable than simK theoretically. It is definite from our result that the
algorithms increase the accuracy, with both centroid near to the origin, which
is consistent with the other studies[11,17].
The ray-tracing method implemented in the dual Scheimpflug analyzer uses the
Snell law to calculate total corneal power and total corneal astigmatism. This
approach, instead of assuming that parallel rays reach the posterior corneal
surface, accounts for the refraction of rays by the anterior corneal surface
and thereby more accurate in the calculation of the total corneal power and
total corneal astigmatism. There are some studies about using total corneal
refractive power (TCRP) from ray-tracing method in original
Alcon Toric calculator which can yield better results than before as well.
However, whether Barrett astigmatism algorithms is superior to the ray-tracing
measurement still needs further study.
Different ELP should have produced
different effect on the cylindrical power of corneal plane. AcrySof Toric IOL
has eight models (T2-T9), those are 1.0, 1.5, 2.25, 3.0, 3.75, 4.5, 5.25, and
6.0 D respectively at lens plane. The manufacturer, in fact, gives a single
corneal plane cylinder for each IOL cylinder power; this value is “based on the
average pseudophakic eye” and depends on a fixed ratio (1.46) between the
cylinder power in the IOL plane and the cylinder power in the corneal plane[18], which means the ACD is around
Moreover, the Barrett Toric
calculator carries formula Universal II, which is recognized to be more
reasonable and accurate in IOL power calculation. In this calculator, the
influence of spherical equivalent on astigmatic power was considered, while the
needed toric IOL is calculated only once including spherical and cylinder
power. As for the AcrySof Toric calculator, the old and new versions must use
the fourth-generation formula to calculate the IOL spherical power first. The
study showed that the toric IOL spherical power of the two groups have no
statistically significant difference. In the Barrett Toric calculator group,
patients with |EV| less than 0.5 D 1 and 3mo after surgery accounted for 88.57%
and 88.57%, respectively. In the new online AcrySof Toric calculator group,
patients with |EV| less than 0.5 D 1 and 3mo after surgery accounted for 76.47%
and 82.35%, respectively. It seemed that Barrett calculator group were slightly
better than those of the AcrySof calculator, however without significant
difference. Further study including more patients should be needed.
The ERA indicates the difference
between the expected residual astigmatism and the actual astigmatism after
surgery. The smaller the ERA, the higher the predictive precision is. In this
study, the ERA of both groups was calculated, and the EM and EV of ERA were
compared as well, which aimed to assess the prediction of the two calculators.
In addition, astigmatism, as a vector, has magnitude and direction. The
standard vector analysis method[21] recommended
by the American National Standards Institute was adopted in this study to
evaluate the effect of astigmatism correction. After the astigmatism was
converted to the corneal plane, the horizontal diameter line of 90°-180° was
used as a reference axis. The astigmatism was decomposed into two components of
X and Y, and the coordinate system was constructed to analyze the correction
effect of the two calculators. There is no statistically significant difference
between the |EV| values obtained by the two calculators at 1mo and 3mo after
surgery. In terms of the vector analysis the difference between X and Y was
statistically significant. However, at 3mo post operatively, the difference
between X and Y was not statistically significant, which is related to the
instability of the refraction 1mo after surgery. This outcome is similar to
that of Ferreira et al[1]. The EV in the
center of the standard circle in coordinate system is the centroid. The closer
the centroid is to the origin, the more accurate it is. At 3mo after surgery,
the centroids of Barrett Toric calculator and new online AcrySof Toric
calculator were 0.05 D@50, and 0.07 D@137 respectively, suggesting both of them
have good prediction.
The limitation of this study is the
definition of “normal” cataract eyes which included normal AL and not shallow
anterior chamber with definite range. However, the ratio of anterior/posterior
in normal eyes should have presented a wide change, which may result in
difference between the two methods. It will be reasonable to include more eyes
to reach a further conclusion.
In summary, incorporation of
Barrett’s astigmatism algorithm significantly improves the predictability of
new online AcrySof Toric calculator. In comparison with the Barrett Toric
calculator, the new online AcrySof calculator can provide the same stable and
accurate results in patients with normal eye axial length and ACD. However, the
Barrett Toric calculator with more variables taken into consideration still has
certain advantages over the new online AcrySof Toric calculator, especially in
those eyes with abnormal ACD and extremely short or long AL, which need further
study.
ACKNOWLEDGEMENTS
We are grateful to all those who
contributed to the discussion of this study, and in particularly to the
patients themselves for their willingness to undergo investigation and
operation. The data used to support the findings of this study are available
from the corresponding author upon request.
Foundation: Supported by Natural Science
Foundation of Tianjin Medical University (No.2016KYZM14).
Conflicts of Interest: Yang J, None; Zhang H, None; Yang
XT, None; Tian F, None; Zhao SZ, None.
REFERENCES