·Brief Report·
Scleral
buckling combined with internal cyclopexy for severe traumatic cyclodialysis
cleft in open globe injuries
Bo
Chen1, Gao-Xiang Wang2, Xian Zhang1, Hong Yang1
1Department
of Ophthalmology, Tongji Hospital, Tongji Medical College, Huazhong University
of Science and Technology, Wuhan 430030, Hubei Province, China
2Department
of Hematology, Tongji Hospital, Tongji Medical College, Huazhong University of
Science and Technology, Wuhan 430030, Hubei Province, China
Correspondence to: Xian Zhang and Hong Yang. Department of Ophthalmology,
Tongji Hospital, Tongji Medical College, Huazhong University of Science and
Technology, Wuhan 430030, Hubei Province, China. zhangxiantjyk@163.com;
dr_yangh@aliyun.com
Received: 2018-10-06
Accepted: 2019-03-17
Abstract
This study aimed to evaluate the effect of scleral
buckling combined with internal cyclopexy on the treatment of severe traumatic
cyclodialysis cleft in open globe injuries (OGIS). This retrospective study
recruited 10 patients of 10 eyes. With our surgical intervention, all the 10
eyes achieved retinal and ciliary body anatomic re-attachment. The choroidal
ruptures in nine eyes were closed with complete choroidal reattachment.
Postoperative best-corrected visual acuity of nine eyes had various
improvements. The mean intraocular pressure was increased from 8.9±2.6 mm Hg to 13.4±4.4 mm Hg. Eventually, six eyes underwent silicone oil
(SO) removal without complications, two eyes still had SO tamponade and two
eyes became SO-dependent eyes. The result shows that internal direct cyclopexy
combined with scleral buckling is an effective treatment for severe traumatic
cyclodialysis cleft in OGIS.
KEYWORDS: cyclodialysis; ocular trauma; cyclopexy; scleral
buckling; pars plana vitrectomy
DOI:10.18240/ijo.2019.10.20
Citation:
Chen B, Wang GX, Zhang X, Yang H. Scleral buckling
combined with internal cyclopexy for severe traumatic cyclodialysis cleft in
open globe injuries. Int J Ophthalmol 2019;12(10):1649-1653
INTRODUCTION
Open globe injuries (OGIS) are a major cause of
blindness, causing approximately 203 000 such cases per year worldwide[1]. According to the different location of injuries, OGIS
can be divided into three zones by Ocular Trauma Classification Group (OTCG)[2]. Briefly, zones are defined as the cornea and limbus
(I); the anterior 5 mm of
the sclera (II) and posterior to zone II (III). Severe OGIS, especially the
zone II and/or zone III injuries which included cyclodialysis, vitreous
hemorrhage, choroidal detachment, retinal detachment and so on, may lead to
worse outcomes[3-4].
With the development of microsurgical techniques,
pars plana vitrectomy (PPV), has dramatically improved the outcome of OGIS
involving the posterior segment[5-6].
However, some problems of OGIS with severe intraocular damage still deserve
attention. After received primary emergency ocular injury debridement suture,
in these patients, cyclodialysis, choroidal detachment and unclosed choroidal
rupture, which were usually accompanied by severe intraocular structure
abnormality (lens extrusion, iris defect and so on), could be defined as
“severe traumatic cyclodialysis cleft”. This kind of traumatic cyclodialysis
cleft is much more serious than the common traumatic cyclodiaysis cleft, which
occurs almost exclusively as a result of blunt ocular trauma[7-8]. In these patients, the unclosed choroidal rupture will
lead to the suprachoroidal space collection of tamponading agents, such as
silicone oil (SO). SO may migrate through the choroidal rupture into the
suprachoroidal space, which can possibly lead to persisent hypotony after
surgery[9-10]. When
cyclodialysis and choroidal detachment combined with choroidal rupture, the
hypotony will be more serious and impact patients’ visual function and
appearance. Our search of Medline database failed to reveal a similar report on
managing this kind of traumatic cyclodialysis cleft during the primary PPV. In
this study, we introduced an effective technique using the scleral buckling
combined with internal cyclopexy to treat the severe traumatic cyclodialysis
cleft in OGIS.
SUBJECTS AND METHODS
Ethical Approval
This retrospective study
included patients who consecutively attended the Tongji Hospital
diagnosed with severe OGIS from November 2016 to June 2017. The review board of
the Tongji Hospital approved our study, and the
study followed the tenets of the Declaration of Helsinki. As it was a
retrospective assessment and all the data were obtained during routinely taking
care of patients, the necessity of an informed consent by the participants was
waived by the ethics committee.
The OGIS patients who had been diagnosed with severe
traumatic cyclodialysis cleft were included in our study. All these patients
had received an emergency ocular injury debridement suture in the Tongji Hospital.
Before the PPV, the preoperative examinations included best-corrected visual
acuity (BCVA), intraocular pressure (IOP) and slit lamp of the anterior
segment. Because of the corneal edema, cataract or severe vitreous hemorrhage,
ultrasound B scans were taken to confirm detachment of choroid. Cyclodialysis
was diagnosed during PPV process.
All the surgeries were carried out by the same
vitreoretinal ophthalmologist (Yang H) with 23G standard three-port PPV. Two transparent corneal
incisions were made for temporary infusion cannula and vitrector. After
lensectomy and anterior vitrectomy, the conventional three-port (infusion
cannula, light cannula and vitrector cannula) could be made and the
cyclodialysis could be located by the scleral depression. The infusion pressure
was maintained at 25 mm
Hg. The major internal cyclopexy procedures were as follow: a double-armed
straight needle was inserted through the patient’s opposite limbus incision
towards the location of the cyclodialysis. Meanwhile, two 30G needles at the proposed anatomical site, which
were located at the cyclodialysis area and 2 mm
posterior to the limbus, were used to guide the straight needles through the
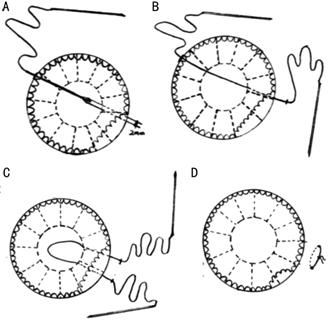
detached ciliary body and sclera to the outside of the eyeball (Figure 1A-1C,
Figure 2A). The free ends of the
polypropylene thread were then tied to re-attach the ciliary body (Figure 1D).
The knot of the suture was placed on the surface of the sclera and was covered
by conjunctiva. The extent of each paired suture was around 20°. In most of the
severe OGIS, the extent of cyclodialysis usually exceeded 20°, and some of them
were even close to 360°. So, several pairs of paired sutures were used
according to the extent of the cyclodialysis. After re-fixation of the ciliary
body, PPV was continued to remove the posterior vitreous body. Then, the
unclosed choroidal rupture and choroidal detachment could be marked by scleral
depression. The scleral buckling procedures were as follows: a 4.5-7 mm silicone sponge was sewn to the
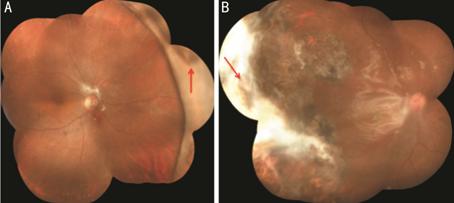
marked scleral area overlying the choroidal rupture (Figure 2B, 2C). To complete the routine PPV, the
suture was adjusted to ensure a high enough buckle to close the choroidal
rupture. After that, the SO tamponade was performed in all the cases.
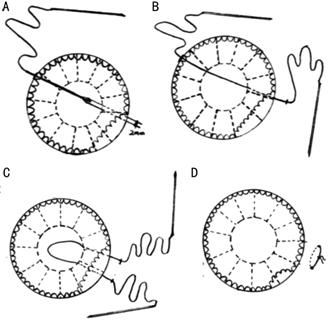
Figure 1 Diagrammatic
drawing of internal cyclopexy using double-armed straight needle A: A 30G syringe needle from ~2 mm posterior to the limbus at the cyclodialysis area
was used to guide the straight needle; B: One of the straight needles was
passed through the detached ciliary body and sclera to the outside of the
eyeball; C: The second straight needle was introduced to the detached area with
the same method as in Figure 1B, 2 mm
away from the first thread; D: The free ends of the polypropylene thread are
then tied and part of the ciliary body was re-attached.

Figure 2 The
surgical color photographs of patient two
A: The straight needle guided by 30G guide needle as same as that in Figure 1A; B: The outer view of scleral buckling
towards the choroidal rupture; C: The inner view of the choroidal rupture (red
asterisk) and detached retina (red arrowhead) on the ridge of scleral buckling.
Follow-up examinations including BCVA, IOP, slit lamp
and ultrasound biomicroscopy (UBM) of the anterior segment and fundus
examination were performed 1 and 2wk, 1, 3, 6 and 12mo after surgery. SO was
removed 6-12mo after surgery for patients with retinal attachment and stable
normal IOP.
RESULTS
Our study included 10 eyes of 10 patients (8 men)
with a mean age of 41.6±16.7y (range from 3 to 66y). The causes of OGIS
included being hit by metallic stick, fish, wood bar, the explosion of
firecrackers, car accidents, cutting injury, and so on. Before the surgery, the
BCVA of four eyes were no light perception (NLP), four eyes were light
perception (LP) and two eyes were hand motion (HM). The location of the wound
was zone II in three eyes and zone III in seven eyes. The length of the wound
was 12.9±2.8 mm (range from 9
to 17 mm). The unclosed
choroidal ruptures of eight eyes were located in front of the equator while the
other two were exceeded across the equator to the posterior choroid.
The clinic data of 10 cases are presented in Table 1.
Four eyes received retinotomy, three eyes received choroidotomy and all the
eyes received SO tamponade because of the complicated and severe retinal
detachment. Four eyes have partial iris defect. Six eyes have lens extrusion
during the injury; the other four eyes have lensectomy because of the severe
cataract or dislocation of the lens. The extent of the cyclodialysis was
170.5°±74.9° (range from 80° to 360°). The postoperative follow-up was
longitudinally performed up to 12mo. The average follow-up time was 8.9±1.79mo
(range from 7 to 12mo).
Postoperatively, the ciliary body was re-attached in
all the eyes, as confirmed by UBM at the end of follow-up. The choroidal
ruptures in nine eyes were closed with complete choroidal reattachment (Figure
3, Table 1). In the other one eye, although the choroidal rupture was not fully
closed, the choroidal detachment was less extensive than pre-operation. After
the SO tamponade for 6 to 12mo, all the eyes achieved retinal anatomic
re-attachment, which included one eye undergoing re-operation due to the
recurrence of retinal detachment in SO. Six eyes received SO removal without
complications, two eyes still had SO tamponade (Figure 3B, Table 1) and two
eyes became SO-dependent eyes due to the IOP<8 mm Hg with SO tamponade. The postoperative BCVA of
nine eyes was various improvements from HM to 20/80 except for one eye still
NLP (Table 1). Two eyes were performed temporary elevation of IOP after surgery
and were controlled with the topical anti-glaucoma applications. Finally, the
mean IOP was increased from 8.9±2.6
mm Hg (preoperative IOP, range from 5 to 12 mm Hg) to 13.4±4.4
mm Hg (postoperative IOP, range from 7 to 21 mm Hg).
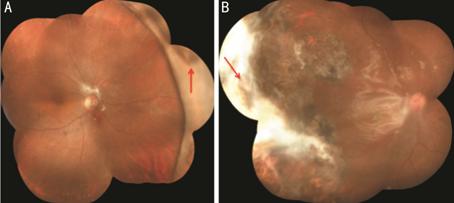
Figure 3 The fundus photographs of representative
patients at the last follow up visit
A: The fundus photograph
of patient five. Red arrow shows the choroidal rupture was tightly closed. SO
had already been removed. B: The fundus photograph of patient three. The
choroidal rupture (red arrow) was surrounded by white scars and was also
closed. SO was still in the vitreous cavity.
DISCUSSION
Severe OGIS, especially combined with severe traumatic
cyclodialysis cleft, is still a complicated challenge even for current PPV. In
our retrospective study, although the OGIS were complex and serious, the BCVA
was improved in most eyes. All the 10 patients who received internal cyclopexy
combined with scleral buckling successfully achieved ciliary body reattachment
and most of the choroidal ruptures were closed. Only two eyes became
SO-dependent eyes with hypotony. We speculate that there are some reasons
causing SO-dependence: 1) the extensive retinal defect caused by primary severe
and complicated injury may increase the exposure of the choroid which can lead
to hypotony; 2) the extensive detachment of ciliary body in these two cases may
reflect more severe ciliary damage causing irreversible reduction of aqueous
humor; 3) traumatic cyclitic membranes in child also may permanently inhibit
the formation of aqueous humor.
There are some differences between traditional
techniques in repairing the ciliary body detachment, most of which use scleral
flap for external direct cyclopexy to reattach ciliary body[7-8,11-12]. Briefly, a
scleral flap is made at the region of the cyclodialysis and the detached
ciliary body can be directly visualized. The ciliary body is sutured under
direct vision to the sclera, followed by suturing the scleral flap both using
10/0 nylon sutures. Compared to conventional external direct cyclopexy, our
techniques have some advantages: 1) There is no need to prepare scleral flap
which may interfere the three-port of scleral incision for vitrectomy. 2) Our
technique is suitable for patients with extensive cyclodialysis, which will
lead to instability or/and ischemia of the eyeball due to large extent of
scleral flap if treated by the traditional external cyclopexy. 3) This method
is especially suitable for aphakia, which allows us to directly observe and
suture the cyclodialysis without densely or inadequately suturing. Our method
of internal cyclopexy is similar with that Wang et al[13]
reported. However, we made some modifications due to the aphakia in most of the
patients. First, we used scleral depression to precisely locate the region of
the cyclodialysis. Meanwhile, the pars plana sclerotomy was replaced by limbus
as the location of piercing into the eye which did not cause iatrogenic cyclodialysis
and did not need suturing. Thus, with these modifications, our method is more
convenient and safe for the severe cyclodialysis.
There are some favorable surgical techniques to
repair traumatic cyclodialysis cleft that included capsular tension ring,
intraocular lens, cryotherapy or endolasercoagulation combined with cyclopexy
and PPV combined with vitreous cavity endotamponade[8,12,14-16]. However,
all of these techniques are not suitable for these OGIS patients who have
cyclodialysis, choroidal detachment and unclosed choroidal rupture. The
choroidal rupture may become rigid, and lead to SO migration into
suprachoroidal spaces which may cause long-term hypotony[10].
Thus, choroidal detachment will not recover unless we fix both choroidal rupture
and cyclodialysis in severe OGIS. In our technique, firstly we use internal
cyclopexy to reattach the ciliary body, which can block the communication from
the anterior chamber to suprachoroidal space and stabilize the detached
choroid. Secondly, the scleral buckling was followed with the internal
cyclopexy to close the choroidal rupture and enhance choroidal reattachment. As
we expected, our study data demonstrated that scleral buckling combined with
internal cyclopexy could effectively reattached ciliary body, close the
choroidal rupture, minimize choroidal detachment, and eventually prevent
hypotony. Our study also has some limitations. First, our study is
retrospective and the number of patients is relatively less, which may lead to
selection bias. Second, our investigation did not include a control group that
did not allow the comparison among different surgical techniques. Third, the
limited cases also restricted the statistical analysis, such as for
investigating the success rate of surgery and risk factors of SO-dependent.
However, the preliminary results of our study are encouraging.
In conclusion, our study shows the internal direct
cyclopexy combined with scleral buckling is an effective way for repairing the
severe traumatic cyclodialysis cleft in OGIS.
ACKNOWLEDGEMENTS
Conflicts of Interest: Chen B, None; Wang GX, None; Zhang X, None; Yang
H, None.
REFERENCES
|
1 Négrel AD, Thylefors B. The
global impact of eye injuries. Ophthalmic Epidemiol 1998;5(3):143-169.
https://doi.org/10.1076/opep.5.3.143.8364
PMid:9805347
|
|
|
|
2 Pieramici DJ, Sternberg P Jr,
Aaberg TM Sr, Bridges WZ Jr, Capone A Jr, Cardillo JA, de Juan E Jr, Kuhn F,
Meredith TA, Mieler WF, Olsen TW, Rubsamen P, Stout T. A system for
classifying mechanical injuries of the eye (globe). The Ocular Trauma Classification
Group. Am J Ophthalmol 1997;123(6):820-831.
https://doi.org/10.1016/S0002-9394(14)71132-8
|
|
|
|
|
3 Thakker MM, Ray S.
Vision-limiting complications in open-globe injuries. Can J Ophthalmol
2006;41(1):86-92.
https://doi.org/10.1016/S0008-4182(06)80074-8
|
|
|
|
|
4 Cruvinel Isaac DL, Ghanem VC,
Nascimento MA, Torigoe M, Kara-José N. Prognostic factors in open globe
injuries. Ophthalmologica 2003;217(6):431-435.
https://doi.org/10.1159/000073075
PMid:14573978
|
|
|
|
|
5 de Juan E Jr, Sternberg P Jr,
Michels RG, Auer C. Evaluation of vitrectomy in penetrating ocular trauma. A
case-control study. Arch Ophthalmol 1984;102(8):1160-1163.
https://doi.org/10.1001/archopht.1984.01040030938018
PMid:6466178
|
|
|
|
|
6 Spalding SC, Sternberg P Jr.
Controversies in the management of posterior segment ocular trauma. Retina
1990;10 Suppl 1:S76-S82.
https://doi.org/10.1097/00006982-199010001-00013
PMid:2191387
|
|
|
|
|
7 Ioannidis AS, Barton K.
Cyclodialysis cleft: causes and repair. Curr Opin Ophthalmol
2010;21(2):150-154.
https://doi.org/10.1097/ICU.0b013e3283366a4d
PMid:20051856
|
|
|
|
|
8 Agrawal P, Shah P. Long-term
outcomes following the surgical repair of traumatic cyclodialysis clefts. Eye
(Lond) 2013;27(12):1347-1352.
https://doi.org/10.1038/eye.2013.183
PMid:23989121 PMCid:PMC3869508
|
|
|
|
|
9 Gopal L, Mittal N, Verma A.
Suprachoroidal collection of internal tamponading agents through a choroidal
hole. Indian J Ophthalmol 2008;56(2):149-150.
https://doi.org/10.4103/0301-4738.39122
PMid:18292628
|
|
|
|
|
10 Feng X, Ma Z. Treatment for
suprachoroidal silicone oil migration following surgeries for open globe
injuries. Can J Ophthalmol 2013;48(4): 307-311.
https://doi.org/10.1016/j.jcjo.2013.03.005
PMid:23931471
|
|
|
|
|
11 Küchle M, Naumann GO. Direct
cyclopexy for traumatic cyclodialysis with persisting hypotony. Report in 29
consecutive patients. Ophthalmology 1995;102(2):322-333.
https://doi.org/10.1016/S0161-6420(95)31021-4
|
|
|
|
|
12 Kluś A, Kosatka M, Kozera M,
Rękas M. Surgical reconstruction of traumatic ciliary body dialysis: a case
report. J Med Case Rep 2017;11(1):22.
https://doi.org/10.1186/s13256-016-1170-6
PMid:28110637 PMCid:PMC5256542
|
|
|
|
|
13 Wang C, Peng XY, You QS, Liu Y,
Pang XQ, Zheng PF, Jonas JB. Internal cyclopexy for complicated traumatic
cyclodialysis cleft. Acta Ophthalmol 2017;95(6):639-642.
https://doi.org/10.1111/aos.13463
PMid:28631430
|
|
|
|
|
14 Gross JB, Davis GH, Bell NP,
Feldman RM, Blieden LS. Surgical repair of large cyclodialysis clefts. Eur J
Ophthalmol 2017;27(3):382-385.
https://doi.org/10.5301/ejo.5000868
PMid:27646330
|
|
|
|
|
15 Gupta S, Selvan H, Shakrawal J,
Gupta V. One-step management of post-traumatic triple dialysis using two
rings. Eur J Ophthalmol 2018;12(1):1120672118803520.
|
|
|
|
|
16 Sood G, Rajendran V, George R,
Sharma T, Raman R. Comparison of encirclage and cryotherapy with argon laser
in the management of traumatic cyclodialysis cleft. Int J Ophthalmol
2019;12(1):165-168.
https://doi.org/10.18240/ijo.2019.01.24
|
|